Abstract
This study investigated the frailty change patterns among Korean older adults during 2006–2020 and the effect of activity limitations induced by the fear of falling (FOF) on these patterns. We employed a descriptive longitudinal design utilizing data from Waves 1 to 8 of the Korean Longitudinal Study of Aging. The exclusion criteria were a baseline age < 65 years, frailty index (FI) captured only at baseline, and death or unknown survival status. Multilevel modeling, combining regression equations at two levels, was used to examine the effect of activity limitations due to FOF on frailty, adjusting for other confounding factors. An increase in FI (1.97; p < .001) was demonstrated in participants who had experienced falls versus those who had not in the past 2 years. Notably, those facing activity limitations due to FOF exhibited a more significant increase in FI (4.62; p < .001) compared with those without; frailty progression intensified over time in the former (0.54, p < .001). Activity limitations due to FOF had a more pronounced impact on frailty than falls; moreover, these activity limitations accelerated the progression of frailty. Healthcare providers must prioritize addressing FOF by employing both physical and psychological interventions to mitigate activity limitations and ultimately decelerate frailty.
Similar content being viewed by others
Introduction
Many countries have become super-aged societies, with 20% of their populations being over 65 years old1; South Korea is expected to become a super-aged society by 20252. As the global older population increases, frailty is becoming an important concept for understanding the process of aging. Frailty is defined as an age-related condition with increased functional vulnerability across multiple systems, including physical, psychological, and social aspects3,4,5. In previous studies, the frailty trajectory was found to increase linearly over time6,7,8. Transitions to frailty are preceded by falls, hospitalization, or a decline in grip strength or cognition8.
Falls are significant health threats to older adults and reduce their ability to remain independent9. The global prevalence of falls among older adults is 26.5%10, and the likelihood of falls increases with age owing to the progressive age-related loss of muscle strength, neuromuscular control, and sensation11,12. Additionally, one in five falls causes fractures or head injuries13, which can lead to more serious health problems and long-term disability14. Falls and frailty have a reciprocal relationship—older adults who have experienced more falls are more frail, and those who are highly frail have an increased likelihood of future falls15,16,17.
The fear of falling (FOF) is a common issue among older adults and is related to limitations in daily activities18. Approximately 70% of community-dwelling older adults have reported FOF, among whom 38% had fear-related activity restrictions19. As older adults experience a greater FOF, they are less active in daily life, even when they have relatively high levels of physical function20. Previous fall experiences and FOF are more likely to restrict daily activities, and FOF is a greater risk factor for activity dependence than fall experiences and related injuries21. Older adults with FOF and fear-related activity restrictions have shown increased odds ratios for sarcopenia and depression19. Physical inactivity in older adults leads to decreased muscle mass and strength22, which can accelerate frailty progression over time.
Few longitudinal studies have investigated the relationships among falls, FOF, fear-related activity restriction, and frailty, especially in the older Korean population. Many previous studies conducted among older adults have examined these relationships using cross-sectional designs. Therefore, we aimed to explore the patterns of change in frailty over time (during 2006–2020) in the older Korean population and to examine the effect of activity limitations due to FOF on these patterns. We hypothesized that activity limitations due to FOF will accelerate the progression of frailty over time.
Methods
Study design, setting, and sample
We employed a descriptive longitudinal design using data from the first to eighth wave of the Korean Longitudinal Study of Aging (KLoSA). The KLoSA survey aims to boost an understanding of South Korea’s aging population, predict individual behavior, and establish and implement effective social and economic policies. Since 2006, biennial KLoSA surveys have been conducted across the nation (excluding Jeju Island), surveying 10,254 adults aged ≥ 45 years. Using the national household register at the time the survey began in 2006, a sample was obtained using a multilevel stratified sampling method based on region and housing type.
Trained investigators conducted the survey through face-to-face interviews using computers. The survey encompassed a range of elements, including self-reported information (demographics, social relationships, health conditions, and cognitive capabilities) and objective data (such as measurements of physical functioning). In the initial baseline survey, 10,254 individuals were enrolled. From the second to fourth survey waves, the sample retention rate remained at approximately 80%; from the fifth wave, the survey was administered to both the previously enrolled and 920 new participants.
In the present study, we examined changes in frailty index (FI) over 14 years; therefore, our analysis excluded the data of new participants, concentrating solely on those who had been a part of the survey since its inception. The sample retention rate in the eighth wave was 77.1%. Only those who participated more than twice were enrolled to confirm the changes in frailty. The exclusion criteria were a baseline age < 65 years, FI recorded only at baseline, and death or unknown survival status.
Measures
Baseline demographic characteristics
We examined age, sex, marital status, and highest education level at baseline; therefore, the demographic characteristics were time-independent variables.
Fall experience and activity limitations due to FOF
In accordance with previous studies23,24, fall experience was defined as a dichotomous variable (yes, no) based on the answer to the question, “Have you experienced a fall since the last interview?” Activity limitations due to FOF was defined as a dichotomous variable (yes, no) based on the answer to the question, “Are there any things or activities you would like to do that you cannot do because you are afraid of falling?” which has been used25,26 and validated in previous studies27. Fall experience and activity limitations due to FOF were treated as time-dependent variables as the participants provided different answers in each survey wave.
FI
FI measures the degree of frailty by estimating the proportion of an individual’s accumulated deficits (symptoms, signs, and dysfunction). Since it can assess the multidimensional nature of frailty and the degree of its severity, the tool has been used widely to screen for frailty in various countries by demonstrating multiple aspects related to health-related outcomes and mortality3,5,6,7,8. In this study, frailty was assessed using the FI developed in a previous Korean study using the KLoSA data28. In the KLoSA study, 41 deficits closely associated with age were selected. The calculation involved summing the scores for each deficit and the count of the measured deficit, and subsequently dividing these sums. Scores for individual deficits were recorded as follows: 0 points (no deficit), 1 point (deficit), or fractional points such as 0.25, 0.5, and 0.75. The FI was calculated using the following formula:
The constituents of the FI include self-rated health, physical condition (e.g., impaired vision, sleep disturbance), mental status (e.g., loneliness), cognitive function (e.g., orientation time, registration), activities of daily living (e.g., needing assistance with dressing, bathing), instrumental activities of daily living (e.g., requiring assistance with grooming, housework), and chronic conditions (e.g., hypertension, diabetes). The details are described in Supplementary Table S1. The FI ranged from 0 to 1, with greater scores indicating increased frailty. We used the FI continuous variables as dependent variables to confirm the frailty changes; for input into our final model, we created a new variable for frailty status. Based on previous studies28, frailty status was classified into three categories at baseline: robust (FI ≤ 0.10), prefrail (0.10 < FI < 0.25), and frail (FI ≥ 0.25).
Statistical analysis
The baseline participant characteristics were presented as means, standard deviations, and percentages. The pattern of a participant’s FI over 14 years was presented as a spaghetti plot. We confirmed that the intercept of the FI at baseline and the slope of the FI from 2006 to 2020 differed according to the individual, and that the frailty pattern exhibited significant fluctuations among individuals. We assumed that the variations in the intercept and slope of the FI and frailty patterns would differ depending on the baseline frailty status. Therefore, according to the baseline frailty status, the frailty pattern until 2020 is presented as a spaghetti plot and a mean plot. Since the baseline frailty status was based on the baseline FI, the frailty pattern was confirmed using the data from the second to eighth waves.
Given the interdependence among the 14-years FI values of the individual participants, a multilevel modeling approach was followed to address the research objectives of this study. In this model, the regression equation was combined at two levels: the lower level, corresponding with the repeated measurement time points, and the upper level, representing the individual respondent characteristics. Only the intercept effect was considered a random effect of the integrated regression model. The null model refers to the basic model without a fixed-effects term, and the random intercept model refers to the model in which a fixed-effects term was added to the basic model to confirm our hypothesis. For the seven time variables between 2008 and 2020, mean-centered variables were inputted (− 5, − 3, − 1, 1, 3, 5, and 7). Time, baseline age, sex, marital status, highest education level, baseline frailty status, fall experience, and activity limitations due to FOF were entered as fixed-effects terms. An interaction term was added to ascertain whether activity limitations due to FOF accelerated frailty over time (time × activity limitations due to FOF). To estimate the random intercept model, restricted maximum likelihood estimation was used. The Akaike information criterion (AIC) and Bayesian information criterion (BIC) were used to compare the suitability of the null and random intercept models.
Statistical analyses were performed using R software, version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set at p < 0.001.
Ethical considerations
The study was exempted from review by the Institutional Review Board of the Gyeongsang National University owing to the use of secondary data (approval no. GIRB-G22-X-0065).
Patient consent
Informed consent was waived owing to the retrospective nature of the study.
Results
Figure 1 depicts the participant selection process. Of the 10,245 participants recruited at baseline, those aged < 65 years (n = 6081) and those with only baseline FI measurements (n = 548) were excluded; the data of 1601 participants were finally analyzed, excluding 1638 people who had died and 377 whose survival status was unknown. After excluding participants with only baseline FI measurements for 2006, the number of participants with missing data across the study period was determined as follows: 55 (3.4%) in 2008, 56 (3.5%) in 2010, 46 (2.9%) in 2012, 52 (3.2%) in 2014, 45 (2.8%) in 2016, 50 (3.1%) in 2018, and 0 (0%) in 2020.
Participant characteristics and frailty patterns
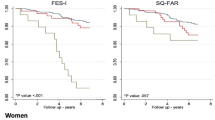
Table 1 presents the participant characteristics at baseline. The average age of the participants was 70.1 ± 4.3 (range 65–88) years, and 61.5% were female (n = 985). Most were married (71.6%, n = 1147) and had a middle-school education level or lower (80.2%, n = 1284). The frailty status at baseline was robust in 24.9% (n = 398), prefrail in 59.8% (n = 958), and frail in 15.3% (n = 245) of the participants. The frailty patterns of all participants from 2006 to 2020 are presented in Fig. 2, and the frailty patterns from 2008 to 2020 according to the baseline frailty status are presented in Fig. 3. Frailty has increased with time, and FI fluctuations in the frail group were more severe than in the robust and prefrail groups.
Linear mixed-effects model
Table 2 shows the results of the linear mixed-effects model. In the null model, assuming that no fixed effect of time exists, the intercept of the random effects was 72.53, the residual was 67.60, and the intraclass correlation was 51.8%. Of the total variance, 51.8% was caused by individual differences, and 48.2% changed over time; the AIC and BIC values of the null model were 91,754 and 91,777, respectively. The AIC and BIC values of the random-intercept model with additional fixed-effects administration were 87,579 and 87,675, respectively. FI increased over time (β = 0.54; p < 0.001) and as the baseline age increased (β = 0.48; p < 0.001). When comparing prefrail and robust statuses at baseline, the FI increased by 6.06 (p < 0.001); when comparing robust and frail statuses, the FI decreased by 15.36 (p < 0.001). Those who had experienced falls exhibited an increase in FI (β = 1.97; p < 0.001) compared with those without fall experience in the previous 2 years. Individuals with activity limitations due to FOF experienced an FI increase of 4.62 (p < 0.001) compared with those without such limitations. Additionally, frailty progression accelerated over time among participants with activity limitations due to FOF (β = 0.42, p < 0.001).
Subgroup analysis according to the baseline frail status
Table 3 shows the results of the linear mixed-effects model according to the baseline frail status. In the baseline robust group, FI increased over time (β = 0.75; p < 0.001) by activity limitations due to FOF (β = 3.50; p < 0.001). In the baseline prefrail group, FI increased over time (β = 0.50; p < 0.001) by fall experience (β = 1.93; p < 0.001) and activity limitations due to FOF (β = 4.79; p < 0.001). In the baseline frail group, FI increased by fall experience (β = 2.00; p < 0.05) and activity limitations due to FOF (β = 4.41; p < 0.001). In all the groups, frailty progression accelerated over time among participants with activity limitations due to FOF (robust [β = 0.30; p < 0.001], prefrail [β = 0.64; p < 0.001], and frail [β = 0.49; p < 0.001]).
Discussion
The major findings of this study are that an increasing frailty trend has been observed over a span of 14 years (2006–2020) in the older Korean population and that activity limitations due to FOF had more negative effects on frailty progression than fall experiences. Notably, fear-related activity restriction significantly accelerated frailty progression over time.
Consistent with previous studies conducted in other countries6,7,8, we found increasing patterns of frailty over time among older Koreans. A review of frailty trajectories reported that frailty levels increase with age; however, the rate and shape of the changes vary across studies29. Likewise, in our study, while the overall FI appeared to increase, the increasing pattern of FI for each subject was different when compared on the spaghetti plot. In addition, the increasing patterns were more visible after subgroup analysis by the frailty status at baseline (robust, prefrail, and frail) than across the entire cohort. We therefore performed additional regression analyses by each subgroup according to the baseline frailty status. Interestingly, time was not a significant factor in increasing the FI in the baseline frail group. Further, fall experience did not have a significant effect on frailty progression in the baseline robust group. This suggests that the frailty status at baseline plays an important role in determining the patterns of frailty change and that the affecting factors and their influence differ by the baseline frailty status. Additionally, we found that the fluctuation in frailty over time was more severe in the frail at baseline group than other groups. In practice, frailty assessment or screening at an early stage is important to identify individuals who may require active interventions to prevent the progression of frailty.
Both fall experiences and activity limitations due to FOF increased frailty progression in our study. A meta-analysis provided evidence for the association between falls and frailty syndrome in older adults30. Falls are common events preceding frailty transitions8; a history of falls is associated with a greater FOF31, and a greater FOF is associated with reduced physical activity20. Falls resulting in severe injuries also increase the likelihood of dependence in daily activities of living21. Hence, fall experiences and FOF often lead to a restriction in physical activity in older populations, which may negatively affect physical function and lead to increased physical frailty. Furthermore, physical frailty (e.g., reduced gait speed and muscle strength) is associated with the development of social frailty32. Frailty is also a well-known risk factor or predictor of future and recurrent falls in older adults, making this a vicious cycle15,33.
Importantly, the impact of activity limitations due to FOF on frailty progression was about 2.35 times greater than that of fall experiences. We also found that activity limitations due to FOF significantly accelerated the progression of frailty over time regardless of the baseline frailty status. While some older adults may not have experienced falls, most tend to restrict their activity due to FOF19. In a study conducted among older Korean adults (n = 4254), 15.2% had experienced falls, and 24.8% exhibited activity limitations due to FOF34. Physical activity can be an effective strategy to reduce the prevalence or severity of frailty, as higher physical activity levels have been associated with lower frailty levels35,36. However, activity avoidance due to FOF can cause sedentary behaviors37, and these behaviors have been associated with a high prevalence and level of frailty38. Older adults with insufficient physical activity levels who spend extended periods engaging in sedentary behaviors exhibit a higher prevalence of frailty39. Moreover, fear-related activity restriction was found to be associated with a decline in physical function (e.g., decreased muscle mass and strength), as well as depression, cognitive impairment, and social isolation, which accelerate frailty and worsen chronic health problems among older populations19,22.
To preclude or delay frailty progression, preventing older adults from falling and encouraging physical activity by reducing their FOF are important. Based on our results, targeting the issues of activity restriction due to FOF would be an effective intervention. A review of interventions aimed at FOF reported that various types of exercises aimed at improving strength, balance, agility, and flexibility could effectively reduce FOF among community-dwelling older adults40. Regarding non-exercise interventions, the cognitive behavioral therapy program aims to implant adaptive views about falls through cognitive reconstruction, and increase activity via goal setting and action planning, reducing concerns about falls, and decreasing related activity avoidance in frail older adults41. Additionally, guided relaxation and imagery can effectively increase fall self-efficacy and exercise during leisure time among older adults42. Early assessment of fall experiences, FOF, and fear-related activity limitation is necessary for older adults, and healthcare workers should provide exercise and/or non-exercise programs to prevent future falls and increase physical activity by reducing FOF.
This study has some limitations. As we used secondary public data, the study variables were limited to those included in the original KLoSA. Certain factors, such as nutritional status and social isolation, may affect frailty status; however, these and other possible relevant factors that were unmeasured in the original survey were not considered. Nonetheless, this study used the FI to accurately estimate frailty status based on various substantial factors that account for the physical, mental, and cognitive aspects of frailty. Moreover, the KLoSA data were collected through face-to-face interviews depending on self-reported information, such that recall bias or social desirability could potentially have affected the participants’ answers and, consequently, the results of the study. For example, it may be difficult for older adults to accurately account their fall experiences over the previous 2 years.
In conclusion, this is the first study to explore the frailty trajectory in the older Korean population. Frailty change patterns were found to increase with time, and activity limitations due to FOF were found to accelerate frailty progression. Fall prevention has long been considered an important strategy for improving the health of older adults. Additionally, more attention should be paid to interventions targeting fear-related activity restrictions to prevent or delay frailty in older adults. A psychological approach to reduce FOF and boost physical exercise may be helpful to resolve activity restriction and ultimately defer frailty.
Data availability
KLoSA data are available from the Korea Employment Information Service (KEIS) and can be accessed by anyone at http://survey.keis.or.kr/eng/klosa/databoard/List.jsp.
References
Grinin, L., Grinin, A. & Korotayev, A. Global aging: An integral problem of the future. How to turn a problem into a development driver? In Reconsidering the Limits to Growth: A Report to the Russian Association of the Club of Rome (eds Sadovnichy, V. et al.) 117–135 (Springer International Publishing, 2023). https://doi.org/10.1007/978-3-031-34999-7_7.
Economic Information and Education Center, Korea Development Institute. 2022 Elderly People Statistics. https://eiec.kdi.re.kr/policy/materialView.do?num=230699 (2022).
Clegg, A., Young, J., Iliffe, S., Rikkert, M. O. & Rockwood, K. Frailty in elderly people. Lancet 381, 752–762. https://doi.org/10.1016/S0140-6736(12)62167-9 (2013).
Fried, L. P. et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146–M157. https://doi.org/10.1093/gerona/56.3.m146 (2001).
Ye, L. et al. Factors associated with physical, psychological and social frailty among community-dwelling older persons in Europe: A cross-sectional study of Urban Health Centres Europe (UHCE). BMC Geriatr. 21, 422. https://doi.org/10.1186/s12877-021-02364-x (2021).
Hoogendijk, E. O. et al. Tracking changes in frailty throughout later life: Results from a 17-year longitudinal study in the Netherlands. Age Ageing 47, 727–733. https://doi.org/10.1093/ageing/afy081 (2018).
Jenkins, N. D. et al. Trajectories of frailty with aging: Coordinated analysis of five longitudinal studies. Innov. Aging 6, iga059. https://doi.org/10.1093/geroni/igab059 (2022).
Lim, R. et al. Frailty trajectory over one year among residential aged care (nursing home) residents. Front. Med. 9, 1010444. https://doi.org/10.3389/fmed.2022.1010444 (2022).
Centers for Disease Control and Prevention. About Older Adult Fall Prevention. https://www.cdc.gov/falls/index.html (2024).
Salari, N., Darvishi, N., Ahmadipanah, M., Shohaimi, S. & Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. 17, 334. https://doi.org/10.1186/s13018-022-03222-1 (2022).
Lord, S. R. & Sturnieks, D. L. The physiology of falling: Assessment and prevention strategies for older people. J. Sci. Med. Sport. 8, 35–42. https://doi.org/10.1016/s1440-2440(05)80022-2 (2005).
Terroso, M., Rosa, N., Torres Marques, A. & Simoes, R. Physical consequences of falls in the elderly: A literature review from 1995 to 2010. Eur. Rev. Aging Phys. Act. 11, 51–59. https://doi.org/10.1007/s11556-013-0134-8 (2013).
Centers for Disease Control and Prevention. Keep on Your Feet. https://www.cdc.gov/injury/features/older-adult-falls/index.html (2023, cited 2024 Jan 3).
National Institute on Aging. Falls and Fractures in Older Adults: Causes and Prevention. https://www.nia.nih.gov/health/falls-and-falls-prevention/falls-and-fractures-older-adults-causes-and-prevention (2022).
Bartosch, P. S., Kristensson, J., McGuigan, F. E. & Akesson, K. E. Frailty and prediction of recurrent falls over 10 years in a community cohort of 75-year-old women. Aging Clin. Exp. Res. 32, 2241–2250. https://doi.org/10.1007/s40520-019-01467-1 (2020).
Chittrakul, J., Siviroj, P., Sungkarat, S. & Sapbamrer, R. Physical frailty and fall risk in community-dwelling older adults: A cross-sectional study. J. Aging Res. 2020, 3964973. https://doi.org/10.1155/2020/3964973 (2020).
Makino, K. et al. Prospective associations of physical frailty with future falls and fear of falling: A 48-month cohort study. Phys. Ther. 101, pzab059. https://doi.org/10.1093/ptj/pzab059 (2021).
Auais, M. et al. Fear of falling as a risk factor of mobility disability in older people at five diverse sites of the IMIAS study. Arch. Gerontol. Geriatr. 66, 147–153. https://doi.org/10.1016/j.archger.2016.05.012 (2016).
Merchant, R. A. et al. Relationship between fear of falling, fear-related activity restriction, frailty, and sarcopenia. J. Am. Geriatr. Soc. 68, 2602–2608. https://doi.org/10.1111/jgs.16719 (2020).
Sawa, R. et al. The association between physical activity, including physical activity intensity, and fear of falling differs by fear severity in older adults living in the community. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 953–960. https://doi.org/10.1093/geronb/gby103 (2020).
Pereira, C. et al. Risk for physical dependence in community-dwelling older adults: The role of fear of falling, falls and fall-related injuries. Int. J. Older People Nurs. 15, e12310. https://doi.org/10.1111/opn.12310 (2020).
Merchant, R. A., Morley, J. E. & Izquierdo, M. Editorial: Exercise, aging and frailty: Guidelines for increasing function. J. Nutr. Health Aging 25, 405–409. https://doi.org/10.1007/s12603-021-1590-x (2021).
Kim, J. H. Experiences of falling and depression: Results from the Korean Longitudinal Study of Ageing. J. Affect. Disord. 281, 174–182. https://doi.org/10.1016/j.jad.2020.12.026 (2021).
Kim, Y. S. et al. Association of frailty with fall events in older adults: A 12-year longitudinal study in Korea. Arch. Gerontol. Geriatr. 102, 104747. https://doi.org/10.1016/j.archger.2022.104747 (2022).
Yang, J. M. & Kim, J. H. Association between activity restriction due to fear of falling and mortality: Results from the Korean longitudinal study of aging. Geriatr. Gerontol. Int. 22, 168–174. https://doi.org/10.1111/ggi.14336 (2022).
Jun, S. S. & Lee, E. A longitudinal study of disability in activities of daily living and activity restriction-induced fear of falling among Korean older people. Nurs. Open. 10, 2946–2959. https://doi.org/10.1002/nop2.1538 (2023).
Belloni, G., Büla, C., Santos-Eggimann, B., Henchoz, Y. & Seematter-Bagnoud, L. A single question as a screening tool to assess fear of falling in young-old community-dwelling persons. J. Am. Med. Dir. Assoc. 21, 1295–1301. https://doi.org/10.1016/j.jamda.2020.01.101 (2020).
Baek, W. & Min, A. Frailty index and gender-specific mortality in Korean adults: Findings from the Korean Longitudinal Study of Aging (2006–2018). J. Adv. Nurs. 78, 2397–2407. https://doi.org/10.1111/jan.15168 (2022).
Hoogendijk, E. O. & Dent, E. Trajectories, transitions, and trends in frailty among older adults: A review. Ann. Geriatr. Med. Res. 26, 289–295. https://doi.org/10.4235/agmr.22.0148 (2022).
Fhon, J. R. S., Rodrigues, R. A. P., Neira, W. F., Huayta, V. M. R. & Robazzi, M. L. Fall and its association with the frailty syndrome in the elderly: Systematic review with meta-analysis. Rev. Esc. Enferm. USP. 50, 1005–1113. https://doi.org/10.1590/S0080-623420160000700018 (2016).
Martínez-Arnau, F. M., Prieto-Contreras, L. & Pérez-Ros, P. Factors associated with fear of falling among frail older adults. Geriatr. Nurs. 42, 1035–1041. https://doi.org/10.1016/j.gerinurse.2021.06.007 (2021).
Nagai, K. et al. Physical frailty predicts the development of social frailty: A prospective cohort study. BMC Geriatr. 20, 403. https://doi.org/10.1186/s12877-020-01814-2 (2020).
Cheng, M. H. & Chang, S. F. Frailty as a risk factor for falls among community dwelling people: Evidence from a meta-analysis. J. Nurs. Scholarsh. 49, 529–536. https://doi.org/10.1111/jnu.12322 (2017).
Ji, Y. & Baek, W. The effects of fall experience, fear of fall, and activity limitations due to fear of fall on frailty. J. Korean Data Anal. Soc. 25, 1961–1975 (2023).
Kehler, D. S. & Theou, O. The impact of physical activity and sedentary behaviors on frailty levels. Mech. Ageing Dev. 180, 29–41. https://doi.org/10.1016/j.mad.2019.03.004 (2019).
Tolley, A. P. L., Ramsey, K. A., Rojer, A. G. M., Reijnierse, E. M. & Maier, A. B. Objectively measured physical activity is associated with frailty in community-dwelling older adults: A systematic review. J. Clin. Epidemiol. 137, 218–230. https://doi.org/10.1016/j.jclinepi.2021.04.009 (2021).
Stubbs, B., Patchay, S., Soundy, A. & Schofield, P. The avoidance of activities due to fear of falling contributes to sedentary behavior among community-dwelling older adults with chronic musculoskeletal pain: A multisite observational study. Pain Med. 15, 1861–1871. https://doi.org/10.1111/pme.12570 (2014).
Kehler, D. S. et al. A systematic review of the association between sedentary behaviors with frailty. Exp. Gerontol. 114, 1–12. https://doi.org/10.1016/j.exger.2018.10.010 (2018).
da Silva, V. D. et al. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health 19, 709. https://doi.org/10.1186/s12889-019-7062-0 (2019).
Whipple, M. O., Hamel, A. V. & Talley, K. M. C. Fear of falling among community-dwelling older adults: A scoping review to identify effective evidence-based interventions. Geriatr. Nurs. 39, 170–177. https://doi.org/10.1016/j.gerinurse.2017.08.005 (2018).
Dorresteijn, T. A. C. et al. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: Results of a randomized controlled trial. BMC Geriatr. 16, 2. https://doi.org/10.1186/s12877-015-0177-y (2016).
Kim, B. H., Newton, R. A., Sachs, M. L., Glutting, J. J. & Glanz, K. Effect of guided relaxation and imagery on falls self-efficacy: A randomized controlled trial. J. Am. Geriatr. Soc. 60, 1109–1114. https://doi.org/10.1111/j.1532-5415.2012.03959.x (2012).
Funding
This study was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MIST) (RS-2024-00350086). However, the opinions, analysis, results, and conclusions of this study are those of the authors and not those of the Korean government. Further, this research was made possible using data from the Korean Longitudinal Study of Aging (KLoSA). The KLoSA is a survey designed and implemented by the Korea Employment Information Service (KEIS) and is available to anyone with the link. The Korean government had no role in the design, methods, analysis, or preparation of the article.
Author information
Authors and Affiliations
Contributions
W.B., A.M., C.P., and M.K. conceptualized and planned the design of the study. WB handled the data. W.B., C.P., and M.K. analyzed and interpreted the data. W.B., A.M., Y.J., and M.P. drafted the manuscript. All authors reviewed the manuscript and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Baek, W., Min, A., Ji, Y. et al. Impact of activity limitations due to fear of falling on changes in frailty in Korean older adults: a longitudinal study. Sci Rep 14, 19121 (2024). https://doi.org/10.1038/s41598-024-69930-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69930-2
- Springer Nature Limited