Abstract
Healthy lifestyle reduces the risk of inflammation-related diseases. This study assessed how lifestyle changes affect inflammatory cytokines over 2 months. Involving 179 apparently healthy participants recruited from community, collecting data on lifestyles (smoking, alcohol, BMI, daily activity, sleep, diet) and measured inflammatory cytokines (TNF-α, IL-1β, IL-17A, CRP, IL-8, IL-18, IFN-γ) plus pepsinogens (PG I, PG II) at the baseline and 2-month follow-up. The combined adverse lifestyle score is the sum of scores across six lifestyles, with higher scores indicating more adverse lifestyle factors. Use multiple linear regression and mixed linear models to analyze the relationship between the changes in lifestyle and inflammatory cytokines (follow-up values minus baseline values). For every 1-point increase in combined adverse lifestyle score, IL-17A increased by 0.98 (95% CI 0.23, 1.73) pg/mL, IFN-γ increased by 1.79 (95% CI 0.39, 3.18) pg/mL. Decreased changes in daily activity were associated with higher IL-17A (β = 1.83, 95% CI 0.53, 3.13) and IFN-γ (β = 2.59, 95% CI 0.9, 4.98). Excluding daily activity, changes in combined adverse lifestyle scores were not associated with changes in inflammatory cytokines. Lifestyle improvements at 2-month intervals may reduce TNF-α, IL-17A and IFN-γ, with daily activity making the greatest contribution.
Similar content being viewed by others
Introduction
The inflammatory response is essential for the immune system to address harmful stimuli and maintain balance in the body1. While acute inflammation provides immediate protection, failure to resolve the harmful stimulus can lead to chronic inflammation, contributing to diseases such as cardiovascular disease, chronic kidney disease, non-alcoholic fatty liver disease, and even gastric cancer2,3.
Adopting a healthy lifestyle can prevent the development of many inflammatory diseases4,5,6. For instance, a healthy lifestyle score based on factors like smoking, alcohol consumption, exercise, and BMI shows that lifestyle improvements over ten years can reduce chronic low-grade inflammation in patients with stable cardiovascular disease7. Different lifestyle choices offer varying anti-inflammatory benefits. For example, quitting smoking and alcohol can impact the inflammatory process and reduce levels of inflammatory cytokines such as IFN-γ, IL-12, and TNF-α8,9,10. Regular exercise reduces inflammation by decreasing fat tissue and increasing anti-inflammatory cytokines through muscle activity11,12. Maintaining good sleep can reduce systemic inflammation and subsequently lower mortality rates13,14,15. Therefore, improving lifestyle habits is crucial for preventing inflammation.
However, the connection between lifestyle changes and chronic inflammation is not well understood, and some factors like alcohol consumption and obesity have controversial links to inflammation16,17. And most studies rely on cross-sectional surveys or long-term cohort studies7,17,18, leaving a gap in understanding the short-term effects of lifestyle changes on inflammatory cytokine levels. Understanding the short-term effects of lifestyle changes on inflammatory cytokines is crucial as it provides insights into the initial biological responses to lifestyle modifications, informs public health recommendations by highlighting immediate benefits, motivates individuals to adopt healthier habits, offers evidence-based guidance for healthcare professionals on effective interventions, sets measurable goals for patient progress, and bridges the gap between short-term changes and long-term health outcomes, ultimately aiding in the prevention and management of chronic inflammatory diseases. Therefore, this study aims to explore the relationship between lifestyle modifications (including smoking, alcohol consumption, BMI, daily activity, sleep, and fruit and vegetable intake) and inflammatory cytokines over two-month intervals.
Material and methods
Subjects and study design
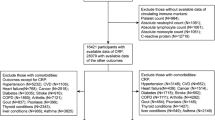
A total of 533 volunteers, without sex restrictions, were recruited from the Third People’s Hospital of Baiyin City and the Jingyuan County Hospital of Traditional Chinese Medicine nearby community. Of these, 179 participants were selected for the study, including 12 hospital administrative staff, 102 healthcare professionals, 20 unemployed or retired persons, 13 migrant workers, and 32 individuals from other occupations, and all signed written informed consent forms. Baseline surveys (F0) were conducted at both hospitals in June 2021 and September 2021, with follow-up visits (F2) in August 2021 and November 2021. The study adhered to medical ethics standards and was reviewed and approved by the Ethics Committee of the School of Public Health of Lanzhou University (Approval No. IRB19122001). Inclusion criteria were as follows: (1) age 20–70 years, voluntary participation. Exclusion criteria included: (1) refusal to sign the informed consent form; (2) pregnant or lactating women, allergic; (3) patients with serious diseases of the heart, liver, kidney, haematopoietic system and psychiatric patients; (4) use of drugs that severely impair gastrointestinal function within 3 months; (5) patients using e.g. NSAIDs or anticoagulants; (6) patients with severe ulcers of the peptic system; (7) self-reported patients with atrophic gastritis; (8) patients who are unable to cooperate with the completion of investigations or tests.
Laboratory tests
After fasting for at least 8 h, 5 ml of venous blood was collected. The levels of inflammatory cytokines IFN-γ, TNF-α, CRP, IL-17A, IL-1β, IL-8 and IL-18 were measured by ELISA kit (Human ELISA Kit; Elabscience, Wuhan, Hubei, CHN). The coefficient of variation of inflammatory cytokines above was 11.25, 9.37%, 12.89, 5.34, 10.53, 9.34 and 9.32% respectively. Plasma levels of PG I and PG II were tested with a time-resolved fluorescence immunoassay (Pepsinogen Quantitative Determination Kit; Jiangyuan industrial Technology, Wuxi, Jiangsu, CHN), and the ratio of PG I to PG II (PGR) was calculated. The coefficient of variation of PG I and PG II was 10.90 and 9.24%, respectively. The change in inflammatory cytokines is defined as the difference between the inflammatory cytokines levels at follow-up and the baseline levels (F2-F0).
Changes in lifestyle components and combined adverse lifestyle scores
Data on lifestyle factors were collected using a self-administered questionnaire and a face-to-face survey conducted by uniformly trained investigators. The combined adverse lifestyle score was calculated by summing the lifestyle scores across six dimensions7,19 (Table 1), with a maximum possible score of 8. A higher score indicated a more adverse lifestyle.
The lifestyle factor change score was determined by subtracting the baseline lifestyle score from the follow-up lifestyle score. A positive value indicated a worsening lifestyle, while a negative value indicated an improvement (e.g. + 1 for a change from normal to abnormal BMI and – 1 for a change from abnormal to normal). The change in the combined adverse lifestyle score was calculated similarly, ranging from − 8 to + 8. A higher positive score indicated a deterioration in lifestyle. For further details, please refer to the eMethods in the Supplements.
Covariates
Our analysis included several key covariates to ensure a comprehensive understanding of the factors influencing inflammation: sex (male/female), age, education level (junior high school and below, high school and polytechnic school, junior college, bachelor or above), annual household income (less than or equal to 20,000 yuan, over 20,000 to 60,000 yuan, over 60,000 to 100,000 yuan, over 100,000 yuan), monthly alcohol intake, prevalence of 20 common diseases (including gastric ulcer, acute gastritis, chronic gastritis, duodenal ulcer, cholecystitis, hepatitis, fatty or alcoholic liver, enteritis, pancreatitis, reflux oesophagitis, kidney disease, prostate disease, rhinitis, pharyngitis, asthma, rash or urticaria, lupus erythematosus, cardiovascular disease, hyperthyroidism, gout), use of Bacillus licheniformis and other probiotics (e.g. bifidobacterium, lactobacillus capsules) in the last month, use of medications damaging to the stomach (e.g. dexamethasone, erythromycin, aspirin, phenylbutazone) in the last month, use of cold or painkillers in the last month, use of vitamin and plant antioxidant-based nutritional supplements, use of anti-inflammatory drugs (e.g. omeprazole, amoxicillin, clarithromycin, levofloxacin, metronidazole, tetracycline, furazolidone, citric acid, bismuth gum, ranitidine) in the last month, and changes in blood pressure, blood glucose, HDL-C, and LDL-C in the last month at the time of follow-up.
Statistical analysis
The sample size for this study was calculated using CRP levels as the primary indicator, based on previous research showing CRP levels of 1.2 ± 2.7 pg/mL and 2.5 ± 2.5 pg/mL in different lifestyle groups7. With a test power of 95%, a two-sided α of 0.05, and accounting for a 20% follow-up loss rate, the required sample size was determined to be 174 participants.
Continuous variables were described using means and standard deviations or medians and interquartile ranges, while categorical variables were described using frequencies and composition ratios. Histograms and Q-Q plots were used to assess the approximate normality of all measures. CRP indicators with a right-skewed distribution were LN-transformed to improve normality. Levels of inflammatory cytokines in different lifestyle groups at baseline were compared using independent samples t-tests, ANOVA, and LSD-t tests (see Table S2 in the Supplements).
The relationship between changes in lifestyle and changes in seven inflammatory cytokines over time was analyzed using multiple linear regression. Changes in the inflammatory cytokines served as the dependent variables, while changes in lifestyle factors and combined adverse lifestyle changes were the independent variables. Model 1 adjusted for sex and age, and also included baseline levels of each variable to account for their impact on observed changes. Model 2 further adjusted for all covariates. When analyzing changes in single lifestyle factors, adjustments were made for changes in other lifestyle factors. Since smoking status did not change at follow-up, the total number of previous smoking packs was included as a covariate. Additionally, a mixed-effects linear model in Model 2 evaluated the relationship between independent variables and cytokines progression, with time included as a covariate. Random intercepts for study participants were included to reflect differences in cytokine levels associated with varying lifestyle levels and changes. Continuous variables such as metabolic equivalent (MET) of daily activity, BMI, sleep time, alcohol intake, and smoking (packs) were used to fit restricted cubic spline (RCS) curves.
Several sensitivity analyses were conducted. First, weighted lifestyle scores were calculated based on the standardized β effect values for each lifestyle factor in multiple linear regression Model 2, using the formula: i = [βi/(∑βi)] × 5; (2) Each lifestyle component of the combined adverse lifestyle score was excluded in turn from the analysis. (3) Subjects with potential atrophic gastritis lesions (pepsinogen PG I ≤ 60 ng/mL or PGR ≤ 6, based on the normal reference range provided in the kit) and those using anti-inflammatory medications were excluded separately. Multiple linear regression model 2 also examined interactions between changes in different lifestyle factors. All statistical tests were two-tailed, with a significance level set at P ≤ 0.05, using IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the School of Public Health of Lanzhou University (Approval No. IRB19122001).
Consent to participate
Informed consent was obtained from all individual participants included in the study. Details that might disclose the identity of the subjects under study have been omitted.
Results
Basic characteristics of subjects
The study included 179 participants, with 77 (43.02%) being male and an average age of 43.59 ± 12.42 years. At baseline, 40 participants (22.35%) had a history of alcohol consumption, and this number slightly increased to 43 (24.00%) at follow-up. The daily activity levels of participants remained largely unchanged from baseline to follow-up (36.23 ± 6.13 vs. 36.20 ± 5.50 MET-h/day).
There was a decrease in the number of participants with a normal BMI, from 74 (41.34%) at baseline to 63 (35.20%) at follow-up. The most common score for vegetable and fruit intake was 1, with 72 participants (40.22%) achieving this score. In terms of sleep duration, there was an improvement, with the number of healthy sleepers increasing from 98 (54.75%) at baseline to 114 (63.69%) at follow-up (Table 2).
Lifestyle changes from baseline to follow-up
There was no change in the smoking status of the study participants. Regarding BMI, the majority of 165 (92.18%) participants maintained their BMI health status. At follow-up, the highest number of participants (48, 26.82%) showed no change in their combined adverse lifestyle score. However, more 80 (44.69%) participants experienced a decrease in their combined adverse lifestyle score compared to 51 (28.49%) who had an increase. For detailed data, refer to Table 3 and Fig. 1.
Relation between lifestyle changes (F2-F0) and changes in inflammatory cytokines (F2-F0)
In model 2, a 1-point increase in daily activity was associated with a 1.83 pg/mL increase in IL-17A (95% CI 0.53, 3.13) and a 2.59 pg/mL increase in IFN-γ (95% CI 0.19, 4.98). The study did not find any association between changes in alcohol consumption, sleep duration, or vegetable and fruit intake and changes in inflammatory cytokine levels (Table 4).
The linear mixed model results indicated that individuals with higher BMI experienced a greater increase in IL-1β over time (β = 0.09; 95% CI 0.00, 0.19). Those with insufficient daily activity had higher levels of IL-17A (β = 0.16; 95% CI 0.07, 0.25), although this association did not change over time. Alcohol consumers had higher levels of IFN-γ (β = 0.11; 95% CI 0.01, 0.20) and lower levels of CRP (β = − 0.12; 95% CI − 0.23, − 0.01) (eTables S9-S15 in supplements).
Restricted cubic spline (RCS) curves revealed a linear inverse relationship between increased daily activity and levels of IFN-γ (P for overall = 0.035; P for non-linear = 0.882) and IL-17A (P for overall = 0.004; P for non-linear = 0.004). Additionally, increased sleep duration was positively correlated with increased IL-8 levels (P for overall = 0.026; P for non-linear = 0.095), as detailed in Fig. 2.
Relation between changes in combined adverse lifestyle score and changes in inflammatory cytokines
Each 1-point increase in the combined adverse lifestyle score was associated with a 0.98 pg/mL increase in IL-17A (95% CI 0.23, 1.73) and a 1.79 pg/mL increase in IFN-γ (95% CI 0.39, 3.18) in model 2 (Table 5 and Fig. 3).
The linear mixed model results indicated that individuals with higher comprehensive adverse lifestyle scores had elevated levels of IL-17A (β = 0.15, 95% CI 0.05, 0.26) and IFN-γ (β = 0.12, 95% CI 0.03, 0.22). Furthermore, an increase in the combined adverse lifestyle score was associated with a rise in IL-17A levels (β = 0.09, 95% CI 0.01, 0.16) (eTables S9–S15 in supplements).
Sensitivity and interaction analysis
Weighted changes in the combined adverse lifestyle score were positively correlated with TNF-α in model 1 (see eTables S2 and S3 in Supplements). When daily activity factors were excluded, the association between changes in the combined adverse lifestyle score and changes in inflammatory cytokines disappeared (eTable S4 in Supplements). The relative contribution of daily activity changes to the relationship between IL-17A and IFN-γ was highest, with weights of 2.36 and 2.04, respectively (eTable S2).
After excluding subjects who may have atrophic gastritis and those using anti-inflammatory drugs, the research results did not change significantly (eTables S5–S8 in Supplements). Interaction analysis revealed that changes in daily activities and alcohol consumption, as well as changes in daily activities and BMI, were associated with changes in IL-17A levels. Additionally, the interaction between changes in vegetable and fruit intake and alcohol consumption was associated with changes in IFN-γ levels.
Discussion
In this longitudinal observational study conducted over two-month intervals, an increase in the combined adverse lifestyle score was positively correlated with higher levels of IL-17A and IFN-γ. Decreased daily activity was associated with increased levels of both IL-17A and IFN-γ, with changes in daily activity having the most significant impact on these levels. Additionally, a change in BMI from normal to abnormal was linked to elevated IL-17A levels. Alcohol consumers exhibited higher levels of IFN-γ and lower levels of CRP. Increased sleep duration was associated with higher levels of IL-8.
Our findings align with previous observational studies. For instance, R. Millar et al. demonstrated that healthier lifestyles—such as quitting smoking, moderate alcohol consumption, regular physical activity, a balanced diet, and maintaining a normal BMI—were linked to lower TNF-α levels in a middle-aged and 2045 elderly population. Our study builds on this by showing that changes in combined lifestyle factors over just two months are associated with alterations in TNF-α levels (plays a crucial role in regulating various immune responses, such as activating immune cells, producing other cytokines, and accumulating inflammatory cells at infection or injury sites)17,20. The short-term nature of our study offers valuable insights into the immediate biological effects of lifestyle changes. While Millar et al. focused on long-term adherence, our results indicate that even brief modifications can significantly impact inflammatory markers. This is consistent with findings from C.C. van 't Klooster et al., who reported that increased daily activity and weight loss notably affected the relationship between changes in lifestyle factors (smoking, weight, daily activity, and alcohol intake) and CRP levels7. We identified daily activity as a crucial factor; without it, the combined adverse lifestyle score did not correlate with IL-17A and IFN-γ levels.
Moreover, the synergistic effects of daily activity in conjunction with other lifestyle factors are important. A study by Miriam Adoyo Muga et al. in Taiwan found that the interaction between smoking, alcohol consumption, physical activity, and diet was linked to lipid and blood glucose levels, which can promote inflammation19. Our findings revealed that the relationship between changes in the combined adverse lifestyle score and IL-17A and IFN-γ was stronger and more stable than the association with daily activities alone, suggesting a synergistic effect among various lifestyle factors. This highlights that improving overall lifestyle may lower chronic inflammation and reduce the risk of malignant lesions in epithelial cells21,22,23.
Additionally, we found that changes in the weighted combined adverse lifestyle score correlated with TNF-α across all subjects. This suggests that the varying effects of each lifestyle factor on inflammatory cytokines should be considered when calculating the combined adverse lifestyle score. This comprehensive approach underscores the importance of a holistic lifestyle modification strategy rather than focusing on individual factors in isolation. In conclusion, our study illustrates that short-term lifestyle changes can lead to significant biological impacts, particularly in reducing inflammatory cytokines such as TNF-α, IL-17A, and IFN-γ.
The relationship between IL-17A and BMI is complex and debated. While some mouse experiments suggest IL-17A has anti-fat effects24, Dalmas et al. found elevated IL-17A levels in the adipose tissue of obese patients compared to normal-weight individuals25. Our study aligns with this, showing a positive association between two-month changes in BMI and IL-17A levels, supporting findings from a previous cross-sectional study16. This suggests that short-term BMI changes can influence IL-17A levels, potentially due to obesity-associated impaired immune function and increased susceptibility to infections26.
Alcohol consumption's impact on inflammation is multifaceted. It can lead to pro-inflammatory cytokines production and liver damage27, and long-term drinking affects both type 1 (IFN-γ, IL-12, TNF-α) and type 2 (IL-4, IL-10, IgE) immune responses10. Our study found higher baseline IFN-γ levels in drinkers compared to non-drinkers, consistent with previous research28,29. Interestingly, drinkers had lower CRP levels, likely due to alcohol's influence on metabolic pathways that reduce inflammation30, aligning with earlier longitudinal findings31. However, despite these short-term anti-inflammatory effects, alcohol should not be considered a treatment, as the ideal amount and frequency of moderate drinking remain debated17,32, and excessive consumption poses serious health risks, particularly cardiovascular diseases32.
Sleep significantly affects the hypothalamic–pituitary–adrenal axis and sympathetic nervous system, both of which can promote inflammation33. Insufficient or excessive sleep can elevate inflammatory cytokines and disrupt sleep patterns34,35. Our analysis indicated that longer sleep duration was associated with higher IL-8 levels, supported by findings from a prior Japanese study36. This highlights the short-term impact of sleep duration on inflammation, though the causal relationship requires further exploration.
The anti-inflammatory effects of exercise are well-documented11,37, with evidence suggesting exercise may reduce pro-inflammatory cyclooxygenase-2 (COX-2) activity, thus lowering cancer risk38. However, the relationship between daily non-exercise physical activity and inflammatory cytokines is less explored. Given that many individuals cannot maintain regular physical exercise due to various constraints, our study focuses on daily non-exercise physical activity. A cross-sectional study by Israel S. Ribeiro et al. suggested IL-17A and IFN-γ are key cytokines in the inflammatory process in middle-aged and older men39. Our findings support this, showing that changes in daily activity are consistently associated with changes in IL-17A and IFN-γ levels. This underscores the short-term beneficial effects of increased daily activity on inflammation.
Previous studies have indicated that obesity is a chronic inflammatory state, with adipose tissue secreting cytokines that increase CRP and IL-1β levels7,40. However, other study concluded that the protective effect of a healthy lifestyle on systemic inflammation in middle-aged and older adults was independent of maintaining a healthy weight17. Our study also did not find a relationship between changes in BMI status and changes in CRP levels. This may be due to the short two-month interval being insufficient to produce significant changes in CRP levels, or the small number of participants experiencing a change in BMI status during the follow-up, which limited our ability to detect statistical differences. A retrospective cohort study found that individuals who smoked were at a significantly higher risk of developing gastric cancer41. However, our study did not find a direct association between smoking and inflammatory cytokines, even though smokers had higher levels of all seven inflammatory cytokines compared to non-smokers (eTable S1 in Supplements). This unexpected finding may suggest that while smoking is known to influence cancer risk, its effects on inflammatory cytokines could be influenced by other confounding factors, such as overall health status or coexisting conditions. Additionally, while vegetables and fruits are known for their anti-inflammatory and antioxidant properties due to their rich content of vitamins, glucosinolates, flavonoids, and phenolic compounds42, our study did not find a link between fruit and vegetable intake and the seven inflammatory cytokines. This lack of association may be attributed to the small number of participants who changed their fruit and vegetable intake during the follow-up period. Furthermore, it is possible that the duration and amount of intake were insufficient to elicit measurable changes in cytokine levels.
Strengths and limitations
The strengths of our study include: (1) Providing robust population-based evidence on the relationship between lifestyle changes and inflammatory cytokines over a two-month interval; And (2) extensively analyzing seven common inflammatory cytokines closely linked to many chronic diseases, offering meaningful insights for further research. However, the study has several limitations: (1) The sleep duration survey was conducted via questionnaire, limiting the accuracy of sleep duration assessment, although previous studies have shown a high correlation between activity loggers, polysomnography, and subjective sleep estimates43,44; (2) There was no change in smoking status reported in the last month at the time of follow-up and no information on alcohol consumption was obtained, preventing analysis of the relationship between changes in smoking status and alcohol consumption as continuous variable and changes in inflammatory cytokines; (3) Lifestyle data were collected via questionnaires at baseline and follow-up, which may not represent the entire follow-up period, although lifestyle data were obtained simultaneously with blood samples, making inflammatory cytokines levels representative of lifestyle in the preceding weeks; (4) Detailed dietary information was not collected, which may be an important confounder in the relationship between lifestyle and inflammatory cytokines, and future studies should consider dietary patterns or nutrient intake more comprehensively; (5) There is an unavoidable Nyman bias in this study, as participants may have improved their lifestyle autonomously under observation; (6) Since the majority of our study participants were hospital employees, this inevitably introduced selection bias, limiting the generalizability of our findings.
Conclusion
(1) Increases in the combined adverse lifestyle score were associated with higher levels of TNF-α, IL-17A, and IFN-γ, with daily activity making the greatest contribution. (2) Increased levels of daily activity are associated with lower levels of IL-17A and IFN-γ. These findings highlight the importance of combined lifestyle interventions and their potential for immediate health benefits, which are crucial for preventing inflammatory diseases and reducing the risk of malignant lesions in epithelial cells.
Data availability
The data generated in this study are available upon request from the corresponding author.
Abbreviations
- IFN-γ:
-
Interferon-γ
- TNF-α:
-
Tumour necrosis factor-α
- CRP:
-
C-reactive protein
- IL-17A:
-
Interleukin-17 A
- IL-1β:
-
Interleukin-1β
- IL-8:
-
Interleukin-8
- IL-18:
-
Interleukin-18
- PG I:
-
Pepsinogen I
- PG II:
-
Pepsinogen II
References
Franceschi, C. & Campisi, J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J. Gerontol. A Biol. Sci. Med. Sci. 69(Suppl 1), S4-9. https://doi.org/10.1093/gerona/glu057 (2014).
Hodel, F. et al. The combined impact of persistent infections and human genetic variation on C-reactive protein levels. BMC Med. 20, 416. https://doi.org/10.1186/s12916-022-02607-7 (2022).
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832. https://doi.org/10.1038/s41591-019-0675-0 (2019).
Rutten-Jacobs, L. C. et al. Genetic risk, incident stroke, and the benefits of adhering to a healthy lifestyle: Cohort study of 306 473 UK Biobank participants. BMJ 363, k4168. https://doi.org/10.1136/bmj.k4168 (2018).
Lourida, I. et al. Association of lifestyle and genetic risk with incidence of dementia. JAMA 322, 430–437. https://doi.org/10.1001/jama.2019.9879 (2019).
Zhang, X. L., Wang, T. Y., Targher, G., Byrne, C. D. & Zheng, M. H. Lifestyle interventions for non-obese patients both with, and at risk, of non-alcoholic fatty liver disease. Diabetes Metab. J. 46, 391–401. https://doi.org/10.4093/dmj.2022.0048 (2022).
Van’t Klooster, C. C. et al. The relation between healthy lifestyle changes and decrease in systemic inflammation in patients with stable cardiovascular disease. Atherosclerosis 301, 37–43. https://doi.org/10.1016/j.atherosclerosis.2020.03.022 (2020).
Strzelak, A., Ratajczak, A., Adamiec, A. & Feleszko, W. Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: A mechanistic review. Int. J. Environ. Res. Public Health 15, 1033. https://doi.org/10.3390/ijerph15051033 (2018).
Lu, Z. et al. Necroptosis signaling promotes inflammation, airway remodeling, and emphysema in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 204, 667–681. https://doi.org/10.1164/rccm.202009-3442OC (2021).
Domínguez-Santalla, M. J., Vidal, C., Viñuela, J., Pérez, L. F. & González-Quintela, A. Increased serum IgE in alcoholics: Relationship with Th1/Th2 cytokine production by stimulated blood mononuclear cells. Alcohol. Clin. Exp. Res. 25, 1198–1205. https://doi.org/10.1111/j.1530-0277.2001.tb02336.x (2001).
Metsios, G. S., Moe, R. H. & Kitas, G. D. Exercise and inflammation. Best Pract. Res. Clin. Rheumatol. 34, 101504. https://doi.org/10.1016/j.berh.2020.101504 (2020).
Gleeson, M. et al. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 11, 607–615. https://doi.org/10.1038/nri3041 (2011).
Jin, Q. et al. Association of sleep duration with all-cause and cardiovascular mortality: A prospective cohort Study. Front. Public Health 10, 880276. https://doi.org/10.3389/fpubh.2022.880276 (2022).
Ni, J. et al. Evidence for causal effects of sleep disturbances on risk for osteoarthritis: A univariable and multivariable Mendelian randomization study. Osteoarthr. Cartil. 30, 443–450. https://doi.org/10.1016/j.joca.2021.11.021 (2022).
Mc Carthy, C. E. et al. Sleep patterns and the risk of acute stroke: Results from the INTERSTROKE international case-control study. Neurology 100, e2191–e2203. https://doi.org/10.1212/wnl.0000000000207249 (2023).
Siddiqui, B. et al. Distribution of Helicobacter pylori infection and abnormal body mass index (BMI) in a developing country. J. Infect. Dev. Ctries. 12, 342–346. https://doi.org/10.3855/jidc.10051 (2018).
Millar, S. R., Harrington, J. M., Perry, I. J. & Phillips, C. M. Associations between a protective lifestyle behaviour score and biomarkers of chronic low-grade inflammation: A cross-sectional analysis in middle-to-older aged adults. Int. J. Obes. (Lond.) 46, 476–485. https://doi.org/10.1038/s41366-021-01012-z (2022).
Jin, G. et al. Genetic risk, incident gastric cancer, and healthy lifestyle: A meta-analysis of genome-wide association studies and prospective cohort study. Lancet Oncol. 21, 1378–1386. https://doi.org/10.1016/s1470-2045(20)30460-5 (2020).
Muga, M. A., Owili, P. O., Hsu, C. Y. & Chao, J. C. Association of lifestyle factors with blood lipids and inflammation in adults aged 40 years and above: A population-based cross-sectional study in Taiwan. BMC Public Health 19, 1346. https://doi.org/10.1186/s12889-019-7686-0 (2019).
Waters, J. P., Pober, J. S. & Bradley, J. R. Tumour necrosis factor in infectious disease. J. Pathol. 230, 132–147. https://doi.org/10.1002/path.4187 (2013).
Kong, H. et al. Helicobacter pylori-induced adrenomedullin modulates IFN-γ-producing T-cell responses and contributes to gastritis. Cell Death Dis. 11, 189. https://doi.org/10.1038/s41419-020-2391-6 (2020).
Dewayani, A. et al. The roles of IL-17, IL-21, and IL-23 in the Helicobacter pylori infection and gastrointestinal inflammation: A review. Toxins 13, 315. https://doi.org/10.3390/toxins13050315 (2021).
Korn, T., Bettelli, E., Oukka, M. & Kuchroo, V. K. IL-17 and Th17 Cells. Annu. Rev. Immunol. 27, 485–517. https://doi.org/10.1146/annurev.immunol.021908.132710 (2009).
Ahmed, M. & Gaffen, S. L. IL-17 in obesity and adipogenesis. Cytokine Growth Fact. Rev. 21, 449–453. https://doi.org/10.1016/j.cytogfr.2010.10.005 (2010).
Dalmas, E. et al. T cell-derived IL-22 amplifies IL-1β-driven inflammation in human adipose tissue: Relevance to obesity and type 2 diabetes. Diabetes 63, 1966–1977. https://doi.org/10.2337/db13-1511 (2014).
Hegde, V. & Dhurandhar, N. V. Microbes and obesity–interrelationship between infection, adipose tissue and the immune system. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 19, 314–320. https://doi.org/10.1111/1469-0691.12157 (2013).
Tilg, H. & Diehl, A. M. Cytokines in alcoholic and nonalcoholic steatohepatitis. N. Engl. J. Med. 343, 1467–1476. https://doi.org/10.1056/nejm200011163432007 (2000).
Frank, K. et al. Alcohol dependence promotes systemic IFN-γ and IL-17 responses in mice. PLoS One 15, e0239246. https://doi.org/10.1371/journal.pone.0239246 (2020).
Wilkinson, A. N. et al. Effects of binge alcohol consumption on sleep and inflammation in healthy volunteers. J. Int. Med. Res. 46, 3938–3947. https://doi.org/10.1177/0300060518782020 (2018).
Albert, M. A., Glynn, R. J. & Ridker, P. M. Alcohol consumption and plasma concentration of C-reactive protein. Circulation 107, 443–447. https://doi.org/10.1161/01.cir.0000045669.16499.ec (2003).
Paulson, D. et al. The relationship between moderate alcohol consumption, depressive symptomatology, and C-reactive protein: The Health and Retirement Study. Int. J. Geriatr. Psychiatry 33, 316–324. https://doi.org/10.1002/gps.4746 (2018).
Millwood, I. Y. et al. Alcohol intake and cause-specific mortality: Conventional and genetic evidence in a prospective cohort study of 512 000 adults in China. Lancet Public Health 8, e956–e967. https://doi.org/10.1016/s2468-2667(23)00217-7 (2023).
Irwin, M. R., Olmstead, R. & Carroll, J. E. Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol. Psychiatry 80, 40–52. https://doi.org/10.1016/j.biopsych.2015.05.014 (2016).
Zhai, S. et al. Associations of sleep insufficiency and chronotype with inflammatory cytokines in college students. Nat. Sci. Sleep 13, 1675–1685. https://doi.org/10.2147/nss.S329894 (2021).
Gozal, D. et al. Sleep measures and morning plasma TNF-alpha levels in children with sleep-disordered breathing. Sleep 33, 319–325. https://doi.org/10.1093/sleep/33.3.319 (2010).
Tanaka, S., Honda, M., Toyoda, H. & Kodama, T. Increased plasma IL-6, IL-8, TNF-alpha, and G-CSF in Japanese narcolepsy. Hum. Immunol. 75, 940–944. https://doi.org/10.1016/j.humimm.2014.06.023 (2014).
El Assar, M., Álvarez-Bustos, A., Sosa, P., Angulo, J. & Rodríguez-Mañas, L. Effect of physical activity/exercise on oxidative stress and inflammation in muscle and vascular aging. Int. J. Mol. Sci. 23, 8713. https://doi.org/10.3390/ijms23158713 (2022).
Keum, N. et al. Association of physical activity by type and intensity with digestive system cancer risk. JAMA Oncol. 2, 1146–1153. https://doi.org/10.1001/jamaoncol.2016.0740 (2016).
Ribeiro, I. S. et al. Regular physical activity reduces the effects of inflammaging in diabetic and hypertensive men. Exp. Gerontol. 155, 111558. https://doi.org/10.1016/j.exger.2021.111558 (2021).
Khanna, D., Welch, B. S. & Rehman, A. StatPearls (StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC., 2022).
Kumar, S., Metz, D. C., Ellenberg, S., Kaplan, D. E. & Goldberg, D. S. Risk factors and incidence of gastric cancer after detection of helicobacter pylori infection: A large cohort study. Gastroenterology 158, 527-536.e527. https://doi.org/10.1053/j.gastro.2019.10.019 (2020).
Guo, K. et al. Effect of aqueous extract of seed of broccoli on inflammatory cytokines and Helicobacter pylori infection: A randomized, double-blind, controlled trial in patients without atrophic gastritis. Inflammopharmacology 30, 1659–1668. https://doi.org/10.1007/s10787-022-01030-x (2022).
Signal, T. L., Gale, J. & Gander, P. H. Sleep measurement in flight crew: Comparing actigraphic and subjective estimates to polysomnography. Aviat. Space Environ. Med. 76, 1058–1063 (2005).
Patel, S. R. et al. A prospective study of sleep duration and mortality risk in women. Sleep 27, 440–444. https://doi.org/10.1093/sleep/27.3.440 (2004).
Acknowledgements
We thank all study participants of this study, and the hospital for allowing the recruitment procedure.
Funding
This research was supported by the National Natural Science Foundation of China (No. 82003525), the Fundamental Research Funds for the Central Universities (lzujbky-2023-40), Gansu Province Science Foundation for Youths (No.21JR7RA507).
Author information
Authors and Affiliations
Contributions
L-P. J and L.W conceived and designed the research; K. G, X-J. Z, L. W, X-M. L collected the data; K.G performed the statistical analysis; K. G and L-P. J wrote the manuscript; X-J. Z, X-M. L, P-P. H, Z-W. Z, Q-W. Y contributed to the discussion; All authors read, revised and approved the final manuscript. L-P. J acts as guarantor for this study and publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, K., Zeng, X., Liu, X. et al. Lifestyle deterioration linked to elevated inflammatory cytokines over a two-month follow-up. Sci Rep 14, 21381 (2024). https://doi.org/10.1038/s41598-024-69967-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69967-3
- Springer Nature Limited