Abstract
Air insoles have provided insights for reducing the risk of diabetic foot ulcers (DFU). The pressure time integral (PTI) is an effective assessment that considers the time effect in various physical activities. We investigated the interactions between three different insole inner pressures (80, 160, and 240 mmHg) and two walking durations (10 and 20 min). The big toe (T1), first metatarsal head (M1), and second metatarsal head (M2) were investigated in 13 healthy participants. One-way analysis of variance (ANOVA) showed that the effects of each insole inner pressure significantly differed (P < 0.05) with a 10 min walking duration. The PTI values resulting from 80 mmHg in M2 (38.4 ± 3.8, P = 0.002) and 160 mmHg in M1 (44.3 ± 4.3, P = 0.027) were lower than those from 240 mmHg. Additionally, the paired t test showed that the effects of each walking duration were also considerably different at 160 mmHg. The PTI at 10 min was lower than that at 20 min in M1 (44.31 ± 4.31, P = 0.015) and M2 (47.14 ± 5.27, P = 0.047). Thus, we suggest that walking with a pressure of 160 mmHg for 10 min has a lower risk of DFU.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by elevated blood glucose levels resulting from either insufficient insulin production or inability of the body to effectively use insulin1. In 2022, the cost of treating diabetes in the US was estimated to be $412.9 billion annually. The cost is projected to increase to $494 billion by 2030, driven by the growing number of diabetes cases and associated healthcare expenditures2. DM is predicted to affect 783 million individuals by 20453. Hence, policymakers must take urgent action to prepare health and social security systems to mitigate the impact of DM. One preventive intervention for DM is exercise, which may promote health and reduce the risk of chronic complications in patients with DM4. Walking is the most common exercise among individuals with DM5,6. Walking in individuals with diabetes mellitus may increase the risk of plantar skin breakdown due to repetitive high vertical and shear pressures on the plantar tissue, which can increase the risk of ulcers7. Previous studies have reported that wearing an inappropriate insole can increase the peak pressure and thus lead to the risk of diabetic foot ulcers (DFU)8,9,10,11.
Recent advances in the development of air insoles have demonstrated important improvements in mitigating discomfort and decreasing the risk of DFU12. Air insoles enclose air within a flexible bag in the shoe, increasing the shock absorption capacity and providing superior stability and comfort during ground contact13. This evidence points to the multifaceted benefits of air insoles, emphasizing their importance in promoting foot health and facilitating more effective exercise routines, particularly in people with DFU.
The hardness of the insoles is a crucial factor in foot health and injury prevention. Different hardness levels can significantly affect plantar pressure distribution, comfort, and muscle activity, thereby affecting the overall effectiveness of insoles in reducing foot injuries14. Suitable insole hardness plays a vital role in reducing the risk of DFU10,15. This is because variable hardness levels in insoles are instrumental in effectively redistributing pressure, as highlighted by Haris et al.9. Furthermore, the optimal insole hardness was greater than that obtained with softer insoles. The effectiveness of softer insoles in reducing peak plantar pressure (PPP) has been noted for their significance in preventing injuries, such as metatarsal problems and blisters16. In addition, longer walking durations have been associated with an increased complexity index of plantar soft tissues, suggesting potential alterations in their structure and function17. This heightened complexity may render tissues more susceptible to damage, thereby elevating the risk of developing DFUs.
Many studies have commonly used PPP to predict the risk of DFU based on the experience of the highest pressures during walking or weight-bearing activities9,18,19,20. Compared with PPP, the pressure time integral (PTI) is a more effective assessment tool for evaluating injuries or damage that considers time factors, such as tissue breakdown or ulceration7. Soames21 conducted the first study on PTI, integrating pressure over the entire stance phase, and concluded that combining information on pressure distribution and contact time provided a more comprehensive understanding of plantar mechanical loading21. The amount of pressure applied and duration of sustained pressure on the foot are crucial factors in assessing the load that causes prolonged pressure. This refers to the extended duration during which pressure is exerted on a particular area, potentially leading to increased strain or discomfort22.
Prolonged pressure, as quantified by PTI, can exacerbate these risks by causing damage to the skin and underlying tissues, potentially leading to ulcers23. Individuals with DM are at a higher risk of foot ulcers due to neuropathy and altered foot biomechanics, leading to abnormal plantar pressure distribution during walking20. Thus, studying PTI offers valuable insights into preventive strategies to reduce the risk of ulceration. This can be achieved by identifying and modifying the factors that contribute to excessive mechanical stress on the foot.
This study investigated the effects of different insole pressures and walking durations on PTI. The results of this study can be employed to optimize the air insole design for redistributing the plantar PTI in healthy patients. In addition, the results can also provide a foundation for understanding the effect of insole inner pressure and walking duration on PTI in individuals with DM and peripheral vascular disease. The use of healthy subjects in this study is justified, as it aims to establish baseline data and control conditions that are free from the confounding variables associated with DFUs. Research has shown that interventions aimed at preventing foot ulcers benefit from a robust understanding of plantar biomechanics and pressure distribution, which can be effectively studied in healthy populations before being applied to those at risk for DFUs24. Furthermore, studies have shown that biomechanical analyses do not always require non-insole baseline data, as interventions can be effectively evaluated under controlled, comparative conditions25.
We hypothesized that different interactions between the insole inner pressure and walking duration would influence the risk of DFU. Accordingly, various combinations of insole inner pressure and walking duration may generate distinct PTI values characterized by altered patterns of plantar pressure distribution over time and space. It has been recognized that such alterations have the potential to initiate biomechanical adaptations within the foot, which are conducive to reducing the negative effects caused by prolonged pressure exposure, an underlying cause of DFU. Therefore, a comprehensive examination of how various insole inner pressures and walking durations intricately interact to obtain PTI values could provide invaluable insights into the mechanisms underlying preventive strategies aimed at alleviating the risk of DFU occurrence. Therefore, this study aimed to determine which walking condition is suitable based on the effects of the insole inner pressure and walking duration on PTI to reduce the risk of DFU.
Results
The effects of different insole inner pressures and walking durations, both individually and in combination, on PTI were analyzed using a (3 × 2) factorial multivariate analysis of variance (MANOVA). The results revealed no significant differences between individual and combination factors.
Effect of insole inner pressures
The results of the one-way analysis of variance (ANOVA) showed that the impacts of each insole inner pressure on the PTI were significantly different (Table 1 and Fig. 1). It demonstrated that, with a walking duration of 10 min, the PTI obtained with the insole inner pressure of 80 mmHg was considerably lower than that attained with 240 mmHg in M2 (38.4 ± 3.8 vs. 59.9 ± 4.7 kPa·s, P = 0.002). Meanwhile, the insole inner pressure of 160 mmHg obtained lower PTI than 240 mmHg in M1 (44.3 ± 4.3 vs. 58.2 ± 4.6 kPa·s, P = 0.027).
Comparisons of the effect of the insole inner pressures on the PTI at two walking durations. (A) Effect of the insole inner pressures on the PTI in T1; (B) Effect of the insole inner pressures on the PTI in M1; (C) Effect of the insole inner pressures on the PTI in M2. Data are shown as mean ± standard errors. PTI, pressure time integral; T1, first toe; M1, first metatarsal head; M2, second metatarsal head. *a significant difference (P < 0.05); **a significant difference (P < 0.01).
Effect of walking duration
The paired t test showed that with an insole inner pressure of 160 mmHg, the PTI obtained with two varied durations was also significantly different (Table 2 and Fig. 2). It revealed that the PTI exhibited with a walking duration of 10 min was considerably lower compared to 20 min in M1 (44.31 ± 4.31 vs. 58.24 ± 5.51 kPa·s, P = 0.015). Meanwhile, the PTI obtained at 10 min was also considerably lower compared to 20 min in M2 (47.14 ± 5.27 vs. 65.42 ± 10.30 kPa·s, P = 0.047).
Comparisons of the effect of walking durations on the PTI at three insole inner pressure. (A) Effect of walking durations on the PTI in T1; (B) Effect of walking durations on the PTI in M1; (C) Effect of walking durations on the PTI in M2. Data are shown as mean ± standard errors. PTI, pressure time integral; T1, first toe; M1, first metatarsal head; M2, second metatarsal head. *, a significant difference (P < 0.05).
Reliability test
The reliability test of the PTI value based on the three insole inner pressures showed that the intraclass coefficient correlation (ICC) values at all locations with a 20 min walking speed were in moderate agreement (0.5 < ICC < 0.75); otherwise, the PTI value at 10 min walking speed were poor moderate (ICC < 0.5), as shown in Table 3.
Discussion
This study aimed to investigate the effects of insole inner pressure and walking duration on PTI. The results demonstrated that with 10 min of walking duration, the insole inner pressure of 80 mmHg significantly reduced PTI compared to 240 mmHg in M1. In addition, the pressure of 160 mmHg also considerably decreased PTI compared to 240 mmHg in M2.
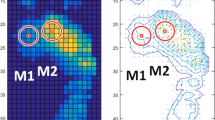
Thus, the study revealed that the effect of the insole inner pressure on the plantar region was significant, indicating that a pressure of 80 mmHg had a more pronounced effect on reducing PTI in M2. In comparison, 160 mmHg demonstrated a more pronounced effect on reducing PTI in M1 (Table 1 and Fig. 2B). The density and thickness of the insole materials prominently influence the plantar pressure26. This means that wearing insoles with a higher density results in an elevated PTI owing to the difficulty of effectively redistributing plantar pressure27. PTI and PPP are highly correlated across all areas of the foot sole, suggesting that minimizing PTI can substantially increase the ability of the foot to distribute plantar pressure28. Specifically, an insole inner pressure of 240 mmHg was not identified as the optimal condition for achieving the highest mesh density after walking (Fig. 3A). This suggests that the combined effect of the adjustment of insole inner pressure and physical activity can significantly contribute to a higher PTI.
Illustration effect of insole inner pressures and walking durations on the foot regions. (A) Effect of the insole inner pressures showed 80 mmHg was lower PTI than 240 mmHg in M2 and 160 mmHg was lower PTI than 240 mmHg in M1 at 10 min. (B) effect of the walking durations showed 10 min was lower PTI than 20 min in M1 and M2 with 160 mmHg. M1, first metatarsal head; M2, second metatarsal.
Different inner pressures of the insole appear to have different mesh-density properties. An appropriate mesh density in footwear design is pivotal for optimizing the pressure distribution and shock absorption in the foot sole. The inability to disperse and redistribute excessive plantar pressure during walking results in foot pain and increased PTI29. Furthermore, an enhanced distribution is important, considering that absorbing and dispersing the forces generated during walking is essential30.
Individuals with poor skin properties often experience a reduction in their shock-absorption capacity. This occurs because of the heightened stiffness of the plantar soft tissue, which is characteristic of diabetes31. The decline in shock absorption among individuals with compromised skin properties aligns with the findings for high-pressure air insoles. Moreover, deterioration in skin properties, attributed to DFU mostly in the plantar region near the metatarsal heads, contributes to the poor ability of DFU individuals to redistribute plantar pressure on the forefoot18. Plantar tissues play a crucial role in absorbing the mechanical loading and redistributing forces during walking. However, increased stiffness in the plantar tissue significantly reduces its ability to tolerate mechanical stresses while bearing weight, thereby increasing the potential for DFUs32. These can be considered intrinsic to footwear design aimed at optimizing pressure management and shock absorption while accommodating specific conditions contingent on skin properties. Consequently, it is not recommended for individuals with good skin properties to walk by employing an insole inner pressure set at 240 mmHg.
Additionally, the results also showed that with an insole inner pressure of 160 mmHg, the effects of walking durations of 10 and 20 min on PTI in M1 and M2 also demonstrated considerable differences (Fig. 3B). This indicates that at a medium insole inner pressure with a longer walking duration, the foot's initial shock absorption was less effective, resulting in higher PTI values at the outset. With longer walking duration, the neuromuscular response is affected by sensorimotor adaptation to foot pressure, leading to decreased PTI in M1 and M233. Additionally, longer walking durations allow for more stable and consistent biomechanical patterns, reducing variability, and increasing reliability34. Longer walking durations also provide a more comprehensive assessment of the subject's endurance and gait mechanics, leading to a more reliable measurement of walking ability35. This finding highlights the nuanced impact that approximately 25% of foot ulcers are located at M136. Similarly, M2, situated between the medial and lateral aspects of the foot, has emerged as a noteworthy site prone to exercise-induced injuries37. Meanwhile, air insole material with a pressure of 160 mmHg can also possibly undergo a series of compressions, which can alter its shock-absorbing properties over time.
This investigation highlighted the significant role of insole inner pressure and walking duration on the PTI values. The critical insight from these findings is that walking with an insole inner pressure of 160 mmHg for 10 min can offer a lower risk of foot ulcers. Conversely, walking with an inner insole pressure of 240 mmHg for all durations may increase the risk of foot ulcers. Furthermore, this research contributes to evidence supporting the need for selecting appropriate insole inner pressures to reduce the risk of DFU. Based on the observed variables, it is possible to determine suitable air insole inner pressure for individuals with diabetes, thereby enhancing foot health and preventing the risk of ulcerations.
Nevertheless, this study has several limitations. First, the investigation only involved insole inner pressures ranging from 80 to 240 mmHg, ignoring the potential benefits of lower pressure ranges achievable with softer insoles, which could reduce the PTI during walking. The air in the insole inner pressure density mesh affects the PTI owing to its ability to redistribute plantar pressure. This is because the insole receives different pressure distributions depending on the hardness of the inner insole26. A lower hardness insole inner pressure may significantly reduce PPP and PTI16. Hence, future studies should extend the tested pressures by examining the effects of pressures lower than 80 and higher than 240 mmHg. This will provide a more detailed understanding of the relationship between insole inner pressure and its impact on PTI, thereby contributing to the development of more effective insole designs for foot health. Second, the PTI measurement only considers PPP in terms of time per frame based on the device frequency. A previous study used alternative methods to calculate the PTI, which could consider peak and submaximal pressures38. This is a special consideration when calculating PTI because the alternative method contains information on the mechanical loading of the foot sole, which PTI and PPP do not provide. Thus, additional research is needed to compare the different PTI calculation techniques with predetermined factors to assess these results. Finally, this study did not consider the foot posture index (FPI) as a foot type to determine plantar pressure. Variations in foot posture, such as planus or cavus feet, are associated with specific pressure distributions that impact lower limb biomechanics and injury risks39. Therefore, additional research is required to compare and understand the differences in FPI in each foot type.
Methods
This study employed a repeated-measures design to examine the effects of two walking durations (10 and 20 min) and three air insole inner pressures (80, 160, and 240 mmHg) on PTI, as shown in Fig. 4A. The hardness values of the air insoles at different pressures were determined using a GS-701N Shore durometer (Teclock Co., Ltd., Nagano, Japan)40. The yields exhibited shore values of 51.7 ± 1.5, 54.7 ± 0.6, and 57.7 ± 0.6 at 80, 160, and 240 mmHg, respectively, as shown in Fig. 4B. In addition, this study selected three inner insole pressures to ensure appropriate stiffness for walking9. Based on the American Guidelines and the American Diabetes Association, a walking speed of 3.6 mph was chosen, as it is commonly used41,42. This study was part of a larger project investigating the effects of different insole inner pressures and walking durations on plantar soft tissue properties9.
Participants
The study involved 13 healthy participants (seven men and six women) aged 21–39 years. Participant characteristics (mean ± SD) included age of 27.0 ± 7.3 years, body weight of 56.0 ± 7.9 kg, body height of 165.8 ± 8.4 cm, and Body Mass Index of 20.3 ± 1.7 kg/m2. The required criteria were shoe size for men (41–43) and women (36–38) with body weights less than 80 kg and right-leg dominance. The Central Regional Research Ethics Committee approved this study at the China Medical University, Taichung, Taiwan (CRREC-111-017). All participants received information about the study's purpose and procedures, as a prerequisite for their involvement in the research. All the participants provided written informed consent. The participants were assured that their data would be kept confidential. The responses were anonymized, and a confidentiality agreement was established, allowing respondents to withdraw from the study at any point, based on the Declaration of Helsinki.
Experimental procedure
The participants were instructed to remove their socks and shoes and lie down for 20 min to minimize the impact of prior weight-bearing activities on muscle fatigue and plantar pressure. The specific walking procedure was as follows:
-
An insole inner pressure of 80 mmHg and a walking duration of 10 min
-
An insole inner pressure of 80 mmHg and a walking duration of 20 min
-
An insole inner pressure of 160 mmHg and a walking duration of 10 min
-
An insole inner pressure of 160 mmHg and a walking duration of 20 min
-
An insole inner pressure of 240 mmHg and a walking duration of 10 min
-
An insole inner pressure of 240 mmHg and a walking duration of 20 min
The participants randomly selected the insole inner pressure and walking duration each week. They were asked to wear commercial shoes (Hsin He Hsin Co., Ltd., Taichung, Taiwan) and walk on a treadmill (Cybex DE-20427 A, Cybex, Taoyuan, Taiwan), as shown in Fig. 4C. The inner pressure insole was made of a thermoplastic polyurethane material. It is located inside shoes to cover the forefoot area to specifically target and alleviate the high plantar pressures and shear forces concentrated in this region. This is crucial because high plantar pressure and shear force are critical factors for the development of metatarsalgia and other forefoot-related conditions. By focusing on the forefoot, air insoles can provide localized pressure relief and improve shock absorption8. It further effectively reduces the strain on this vulnerable area while also enhancing overall gait stability and comfort.
PTI was determined using an F-Scan plantar pressure measurement system (Tekscan Inc., South Boston, MA, USA). This system has a sensor with 960 sensing elements, where the dimensions of each element are 5.08 × 5.08 mm. Before walking on a treadmill, the participants walked for 3–5 min to familiarize themselves with the shoes43. The sensor was calibrated according to the manufacturer's guidelines to minimize measurement errors43. Herbert-Copley et al.44 performed an extensive analysis of the F-scan system to evaluate its performance over extended periods. Despite variations in the total force values over time, the F-Scan system consistently provided accurate evaluations of the pressure profiles and center-of-pressure trajectories. This indicates that the sensor's ability to measure the relative pressure distribution remains reliable, even over extended periods44.
Data analysis
PTI values were obtained from three intermediate steps from the last minute of each trial. All data were analyzed using MATLAB 2022b (The MathWorks, Natick, MA, USA). Data were filtered using a 2nd Butterworth low pass filter applied backward and forward, with a cut-off frequency of 150 Hz. This study focused on selecting three regions of the forefoot with a heightened risk of developing DFU: the first toe (T1), first metatarsal head (M1), and second metatarsal head (M2). The PTI data were determined from the plantar pressure in the contact area of a particular foot sole (5 × 5) F-Scan sensor pixels (645.2 mm2)45. This approach calculates the PTI by summing the peak pressures per sample (Fig. 5). The PTI for the plantar area was determined by adding the products of the peak pressure and duration of the sample, using Eq. 138:
where PPi is the peak pressure at the i-th time, N is the total number of frames, and \(\Delta t\) is the time sample duration.
Statistical analysis
The PTI values are presented as the mean ± standard error. A multivariate analysis of variance (MANOVA) test was used to analyze the main effects of the insole inner pressure and walking duration, as well as the interaction effect between the insole inner pressure and walking duration. One-way analysis of variance (ANOVA) with a least significant difference (LSD) post-hoc test was used for pairwise comparisons of the PTI between the three insole inner pressures and two walking durations9,46. The differences in PTI between the insole inner pressure and walking duration were examined using a paired t test. All statistical analyses were performed using SPSS version 22 (IBM, NY, USA) with a significance level of 0.05. Additionally, the intraclass correlation coefficient (ICC) was calculated, assuming separate data classes, and the three different insole inner pressures were instructed to perform the relative tests.
Ethical experimentation
Studies involving humans were approved by the Central Regional Research Ethics Committee of China Medical University, Taichung, Taiwan (CRREC-111-017). The studies were conducted in accordance with local legislation and institutional requirements. All participants provided written informed consent to participate in the study.
Data availability
Research data supporting this publication are available from the corresponding author upon request.
References
Alam, S. et al. Diabetes mellitus: Insights from epidemiology, biochemistry, risk factors, diagnosis, complications and comprehensive management. Diabetology 2(2), 36–50 (2021).
Parker, E. D. et al. Economic costs of diabetes in the U.S. in 2022. Diabetes Care 47(1), 26–43 (2023).
Sun, H. et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Wu, F. L. et al. Microvascular control mechanism of the plantar foot in response to different walking speeds and durations: Implication for the prevention of foot ulcers. Int. J. Low Extrem. Wounds 20(4), 327–336 (2021).
Wu, F. L. et al. Effects of walking speeds and durations on plantar skin blood flow responses. Microvasc. Res. 128, 103936 (2020).
Lung, C. W. et al. Effects of various walking intensities on leg muscle fatigue and plantar pressure distributions. BMC Musculoskel. Disord. https://doi.org/10.1186/s12891-021-04705-8 (2021).
Duan, Y. et al. The effects of different accumulated pressure-time integral stimuli on plantar blood flow in people with diabetes mellitus. BMC Musculoskel. Disorders 22(1), 554 (2021).
Ahmed, S., Barwick, A., Butterworth, P. & Nancarrow, S. Footwear and insole design features that reduce neuropathic plantar forefoot ulcer risk in people with diabetes: A systematic literature review. J. Foot Ankle Res. 13(1), 30 (2020).
Haris, F. et al. The effects of different inner pressures of air insoles and walking durations on peak plantar pressure. Medicine 102(43), e35704 (2023).
Haris, F. et al. A review of the plantar pressure distribution effects from insole materials and at different walking speeds. Appl. Sci. 11(24), 11851 (2021).
Zwaferink, J. B. J., Custers, W., Paardekooper, I., Berendsen, H. A. & Bus, S. A. Effect of a carbon reinforcement for maximizing shoe outsole bending stiffness on plantar pressure and walking comfort in people with diabetes at high risk of foot ulceration. Gait Posture 86, 341–345 (2021).
Teixeira, R. et al. Towards customized footwear with improved comfort. Materials 14(7), 1738 (2021).
Jankaew, A. et al. Impact of bilateral motion control shoes with outsole adjustment on gait asymmetry in individuals with mild leg length discrepancy. Gait Posture 103, 80–85 (2023).
Casado-Hernández, I. et al. The effectiveness of hard insoles for plantar pressure in cycling: A crossover study. Bioengineering 10(7), 816 (2023).
Korada, H., Maiya, A., Rao, S. K. & Hande, M. Effectiveness of customized insoles on maximum plantar pressure in diabetic foot syndrome: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 14(5), 1093–1099 (2020).
Melia, G., Siegkas, P., Levick, J. & Apps, C. Insoles of uniform softer material reduced plantar pressure compared to dual-material insoles during regular and loaded gait. Appl. Ergon. 91, 103298 (2021).
Liau, B. Y. et al. Using Bidimensional multiscale entropy analysis of ultrasound images to assess the effect of various walking intensities on plantar soft tissues. Entropy (Basel) 23(3), 264 (2021).
Abbott, C. A. et al. Site-specific, critical threshold barefoot peak plantar pressure associated with diabetic foot ulcer history: A novel approach to determine DFU risk in the clinical setting. Medicina 58(2), 166 (2022).
de Castro, J. P. W. et al. Accuracy of foot pressure measurement on predicting the development of foot ulcer in patients with diabetes: A systematic review and meta-analysis. J. Diabetes Sci. Technol. 17(1), 70–78 (2023).
Gnanasundaram, S., Ramalingam, P., Das, B. N. & Viswanathan, V. Gait changes in persons with diabetes: Early risk marker for diabetic foot ulcer. Foot Ankle Surg. 26(2), 163–168 (2020).
Soames, R. W. Foot pressure patterns during gait. J. Biomed. Eng. 7(2), 120–126 (1985).
Niemann, U. et al. Plantar temperatures in stance position: A comparative study with healthy volunteers and diabetes patients diagnosed with sensoric neuropathy. eBioMedicine 54, 102712 (2020).
Mervis, J. S. & Phillips, T. J. Pressure ulcers: Pathophysiology, epidemiology, risk factors, and presentation. J. Am. Acad. Dermatol. 81(4), 881–890 (2019).
Bus, S. A. et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2023 update). Diabetes/Metab. Res. Rev. 40(3), e3651 (2024).
Koska, D., Oriwol, D. & Maiwald, C. Comparison of statistical models for characterizing continuous differences between two biomechanical measurement systems. J. Biomech. 149, 111506 (2023).
Tafti, N. et al. Effect of wearing insole with different density on standing and walking plantar pressure distribution. J. Mech. Med. Biol. 19, 1950006 (2018).
Peng, H.-T., Liu, L.-W., Chen, C.-J. & Chen, Z.-R. The soft prefabricated orthopedic insole decreases plantar pressure during uphill walking with heavy load carriage. Bioengineering 10(3), 353 (2023).
Fellas, A. et al. POS0283 Effect of customised foot orthoses on peak pressure and pressure time integrals in children with juvenile idiopathic arthritis: A randomised clinical trial. Ann. Rheum. Dis. 82(Suppl 1), 382 (2023).
Chen, H.-Y. et al. Immediate effect of customized foot orthosis on plantar pressure and contact area in patients with symptomatic Hallux Valgus. Appl. Sci. 12(15), 7593 (2022).
Huang, Y.-P., Peng, H.-T., Wang, X., Chen, Z.-R. & Song, C.-Y. The arch support insoles show benefits to people with flatfoot on stance time, cadence, plantar pressure and contact area. PLOS ONE 15(8), e0237382 (2020).
Naemi, R. et al. Diabetes status is associated with plantar soft tissue stiffness measured using ultrasound reverberant shear wave elastography approach. J. Diabetes Sci. Technol. 16(2), 478–490 (2022).
Kwak, Y., Kim, J., Lee, K. M. & Koo, S. Increase of stiffness in plantar fat tissue in diabetic patients. J. Biomech. 107, 109857 (2020).
Claret, C. R. et al. Neuromuscular adaptations and sensorimotor integration following a unilateral transfemoral amputation. J. Neuroeng. Rehabil. 16(1), 115 (2019).
Shah, V. V. et al. Effect of bout length on gait measures in people with and without parkinson’s disease during daily life. Sensors 20(20), 5769 (2020).
Baudendistel, S. T. et al. Faster or longer steps: Maintaining fast walking in older adults at risk for mobility disability. Gait Posture 89, 86–91 (2021).
Tamir, E. et al. Mini invasive floating metatarsal osteotomy for diabetic foot ulcers under the first metatarsal head: A case series. Int. J. Lower Extrem. Wounds 21(2), 131–136 (2022).
Ellison, M. A., Fulford, J., Javadi, A. & Rice, H. M. Do non-rearfoot runners experience greater second metatarsal stresses than rearfoot runners?. J. Biomech. 126, 110647 (2021).
Melai, T. et al. Calculation of plantar pressure time integral, an alternative approach. Gait Posture 34(3), 379–383 (2011).
Chow, T.-H., Chen, Y.-S., Hsu, C.-C. & Hsu, C.-H. Characteristics of plantar pressure with foot postures and lower limb pain profiles in Taiwanese college elite rugby league athletes. Int. J. Environ. Res. Public Health 19(3), 1158 (2022).
Helili, M. et al. An investigation of regional plantar soft tissue hardness and its potential correlation with plantar pressure distribution in healthy adults. Appl. Bionics Biomech. 2021, 5566036 (2021).
Colberg, S. R. et al. Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care 39(11), 2065–2079 (2016).
Piercy, K. L. et al. The physical activity guidelines for Americans. JAMA 320(19), 2020–2028 (2018).
Lung, C. W., Hsiao-Wecksler, E. T., Burns, S., Lin, F. & Jan, Y. K. Quantifying dynamic changes in plantar pressure gradient in diabetics with peripheral neuropathy. Front. Bioeng. Biotechnol. https://doi.org/10.3389/fbioe.2016.00054 (2016).
Herbert-Copley, A. G., Sinitski, E. H., , Lemaire, E. D. & Baddour, N. Temperature and measurement changes over time for F-Scan sensors. In 2013 IEEE International Symposium on Medical Measurements and Applications (MeMeA) (2013).
Lung, C. W. et al. Effects of walking speeds and durations on the plantar pressure gradient and pressure gradient angle. BMC Musculoskel. Disord. 23(1), 823 (2022).
Lung, C. W. et al. Using elastographic ultrasound to assess plantar tissue stiffness after waking at different speeds and durations. Appl. Sci. (Switzerland) 10(21), 1–10 (2020).
Acknowledgements
The authors wish to express gratitude to Dr. Wei-Cheng Shen, Ms. Yori Pusparani, Ms. Ardha Ardhea Prisilla, Ms. Maftuhah Rahimah Rum, and Ms. Sylvatera Ayu Puspitasari for their assistance.
Funding
This study was supported by a Grant from the National Science and Technology Council of Taiwan (NSTC 113-2221-E-035-014). The funding agency did not involve data collection, analysis, or interpretation.
Author information
Authors and Affiliations
Contributions
Conceptualization, Y.-K.J. and C.-W.L.; Methodology, G.T.R., F.H. and C.-W.L.; Writing—original draft, G.T.R.; Writing—review and editing, Y.-K.J., C.-W.L. and F.H.; Supervision, B.-Y.L., W.-T.C., and C.-C.T.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramadhan, G.T., Haris, F., Jan, YK. et al. Effect of different inner pressures of air insoles and walking durations on plantar pressure time integral. Sci Rep 14, 19272 (2024). https://doi.org/10.1038/s41598-024-70312-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70312-x
- Springer Nature Limited








