Abstract
This study aims to evaluate the biomechanical performance of the Gamma 3 nail with an anti-rotation screw (GNS) and compare it to two established gold-standard methods for treating unstable femoral neck fractures (UFNFs). Synthetic bone models were prepared with Pauwels’ type III osteotomy and an additional posterior wedge. Three different implant configurations were tested: three cannulated crews (3CS) in an inverted triangle configuration, a dynamic hip screw with an anti-rotation screw (DHSS), and GNS. Non-destructive cyclic axial loading was applied at 7° adduction, with 1000 cycles ranging from 100 to 1000 N. Subsequently, a construct failure test was conducted using progressive axial compression, and fracture reduction loss was recorded. The average axial stiffness was 321 ± 52 N/mm for 3CS, 430 ± 71 N/mm for DHSS, and 519 ± 104 N/mm for GNS. The average ultimate failure loads were 2699.3 N for 3CS, 3427.1 N for DHSS, and 3758.9 N for GNS. GNS demonstrated significantly greater axial stiffness compared to the other two groups (P < 0.05). Both DHSS and GNS exhibited similar failure loading, which were greater than those of 3CS (P < 0.05). GNS offers the advantages of a minimally invasive and intramedullary implant with comparable stability to the DHSS system. Moreover, GNS demonstrated superior biomechanical performance compared to 3 CS configuration.
Similar content being viewed by others
Introduction
Hip fractures are the most common type of fractures; and it is estimated that their global incidence will reach 2.6 million by 20251. Among these fractures, femoral neck fractures account for approximately 50%2. While these fractures primarily affect older patients with osteoporosis, they can also occur due to a high-energy trauma in younger population3,4. Although hip replacement is the main choice for the elderly, internal fixation is still the common treatment for most young patients with femoral neck fractures. The current fixation implants still need to be improved, because complications in fracture healing, such as femoral head necrosis, fracture displacement, and nonunion, occur in up to 23% of all patients after they had been used5. These complications lead to postoperative functional decline caused by shortening and varus collapse of femoral neck, particularly impacting younger patients6.
At present, the treatment of femoral neck fractures mainly depends on several extramedullary fixation devices, for example multiple cannulated screws, the dynamic hip screw with an anti-rotation screw, and femoral neck system. Although multiple CSs is less traumatic and easy to insert7, it is prone to femoral neck shortening, screw withdrawal, cutting out, etc. The conventional treatment for vertical femoral neck fractures involves using a sliding hip screw (SHS) supported by an additional anti-rotation screw, which offers superior biomechanics compared to a configuration of three cannulated screws in an inverted triangle and is considered as the gold standard8,9,10. Yet, the use of DHSS brings greater trauma11. In recent years, femoral neck system has been used to fix femoral neck fractures, but its clinical efficacy still needs to be observed12. In summary, the above implants cannot meet clinical application requirements due to their inherent drawbacks.
Compared to extramedullary fixation, intramedullary nails offer the advantage of being minimally invasive, thereby reducing the risk of complications by avoiding damage to the periosteal circulation13. In addition, extramedullary fixation implants have a long moment, which is prone to implant fatigue and eventually fixation failure. As far as our knowledge extends, although intramedullary implants exhibited stronger biomechanics than extramedullary implants, there are few studies involving intramedullary implants for treating UFNFs. The use of intramedullary nails to fix femoral neck fractures has mainly been used as an optimal alternative for treating ipsilateral femoral neck and shaft fractures together in order to minimize trauma14,15,16,17,18,19,20,21,22,23. A significant contributing factor to this preference may be the challenging nature of implanting an anti-rotation screw due to the thickening of the proximal end of the main intramedullary nail.
The anatomical characteristics of the cross-section of the femoral neck isthmus play a crucial role in determining the spatial configuration and type of cannulated screw implantation24. Previous studies have indicated that the cross-section of the femoral neck resembles an oblique oval shape with a torsion angle25,26,27. These findings suggest that when using intramedullary fixation for femoral neck fractures, there may be sufficient space to position an anti-rotation screw in the anterosuperior region of the femoral neck if the lag screw is implanted at a lower position (Fig. 1). Therefore, considering the anatomical structure of the femoral neck, it becomes feasible to place an anti-rotation screw in the anterosuperior position of the lag screw within the intramedullary nail for the treatment of femoral neck fractures.
This study had two main objectives. The first was to verify the feasibility of placing an anti-rotation screw in the anterosuperior position of the lag screw after the implantation of the Gamma 3 nail. The second objective was to assess the biomechanical performance of a Gamma 3 nail with an anti-rotation screw (GNS) through initial compressive loading, cyclic compressive loading, and failure tests. These tests were conducted to compare the GNS construct with two widely accepted gold standard treatment methods for unstable femoral neck fractures, with a focus on improved survival and fracture reduction in treating unstable femoral neck fractures (UFNFs) (Fig. 2).
Representative X-ray fluoroscopy images of different fixation methods in Sawbones specimens. (a) Three cannulated screws arranged in an inverted triangle configuration (3CS). (b) Dynamic hip screw and anti-rotation screw (DHSS). (c) Gamma 3 nail with an anti-rotation screw (GNS). These images are for demonstration purposes only.
We hypothesized that GNS represented similar biomechanical stability to the DHSS and superior to cannulated screws in the treatment of UFNFs.
Materials and methods
Specimens and preparation
For this study, a synthetic tissue surrogate with uniform material properties and identical geometry was utilized. A total of thirty fourth-generation composite Sawbones left femurs, incorporating solid cancellous foam (Model 3403; Pacific Research Laboratories, Vashon, WA, USA), were evenly divided into three groups: GNS, 3CS (three cannulated screws in an inverted triangle configuration), and DHSS (dynamic hip screw with an anti-rotation screw). To create consistent fractures, each specimen was cut following the OTA/AO 31B2 osteotomy guidelines28, resulting in a triangular calcar defect29. All fracture models were classified as Pauwels type III fractures, inclined at a 70° angle to the horizontal plane30, and produced using a custom-made sawing guide.
The GNS group was stabilized using the Gamma 3 nail system (Stryker Trauma Gmbh, SchÖnkirchen, Germany), which included a 130° 90 mm sliding lag screw, along with an additional 7.3 mm cannulated screw (IRENE, Tianjin, China) placed in the anterosuperior position to function as an anti-rotation screw. In the 3CS group, three 7.3 mm cannulated screws (IRENE, Tianjin, China) were employed in an inverted triangle arrangement to secure the fracture models. The DHS group comprised a 130° 2-slot 90 mm sliding hip screw, accompanied by an extra 7.3 mm cannulated screw (IRENE, Tianjin, China) implanted superiorly to serve as an anti-rotation screw. To minimize variations in implant placement, all surgical procedures were conducted by the same experienced surgeon following the manufacturer's guidelines. Radiographic examinations were performed to verify the implant positions (Fig. 2). Subsequently, all specimens were cut proximally to a length of 25 cm and embedded in polymethylmethacrylate (PMMA; Heraeus Medical GmbH, Wehrhelm, Germany). The femoral shaft was inclined at a 7° angle when embedded in a 5 cm high Polyvinyl chloride (PVC) pipe (Fig. 3).
Biomechanical protocols
Biomechanical testing was conducted using a Bionix 880 servo-hydraulic test system (MTS Systems, Eden Prairie, MN, USA). The test setup and loading protocol were adopted from a previous study. To ensure the perpendicularity of the PVC pipe to the horizontal plane, a custom-made, adjustable metal clamp was used to secure the cement portion of each sample (Fig. 3). This embedding technique and metal clamping provided stability to the distal portion of each specimen throughout the testing process. A flat stainless-steel plate was vertically positioned on the femoral head and connected to a 5000 N load cell. This setup aimed to replicate a normal two-leg stance. Initially, all specimens underwent a nondestructive vertical compression force at a 7° valgus angle to simulate normal loading. Following a preloading phase where each specimen was subjected to a force of 200 N at a speed of 2 mm/min, the load was further increased to 600 N. This allowed the determination of the initial axial construct stiffness, which was calculated based on the linearly elastic region of the load-deformation curve. The entire preloading process adhered to the methodology outlined by Kuan et al.31. Subsequently, the specimens were subjected to cyclic loading, involving a force ranging from 100 to 1000 N (valley to peak), at a frequency of 1 Hz for 1000 cycles. At the conclusion of the cyclic loading test, the interfragmental displacement between the femoral head and shaft was measured and recorded. Finally, each sample was loaded until failure at a displacement rate of 5 mm/min. Failure was defined as a structural breakage occurring when the vertical compression height reached 15 mm29. The maximum load achieved during this process represented the failure load, indicating structural collapse. The appearance of model construct failure was visually documented and recorded (Fig. 4). All biomechanical measurements are presented in Table 1 as means and standard deviations.
Different failure patterns observed after applying destructive load. (a) Descent of the femoral head and fracture along the axis of the cannulated screws in the 3CS construct. (b) Collapse and splitting of the femoral head in the DHSS construct. (c) Collapse of the femoral head in the GNS construct.
Statistical analysis
Statistical analyses were performed using the SPSS software (SPSS Version 19; SPSS Inc., Chicago, IL, USA). The Shapiro–Wilk statistical test was used to check the normality distribution for all data. One-way Analysis of Variance (ANOVA) (two-tailed) and a least significant difference (LSD) correction post-hoc test was used to compare significant differences with respect to axial stiffness, interfragmental displacement, and load to failure. P < 0.05 was considered to be a significantly statistical difference.
Results
All biomechanical measurements are presented in Table 1 as means and standard deviations.
Axial stiffness
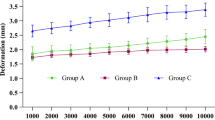
The average axial stiffness in each group was 321 ± 52 N/mm for 3CS, 430 ± 71 N/mm for DHSS, and 519 ± 104 N/mm for GNS (Fig. 5). Compared to the 3CS group, the DHSS group showed an increase in axial stiffness of 33.9% (P < 0.05), and the GNS group showed an increase of 61.7% (P < 0.001). In addition, the construct with Gamma 3 and an anti-rotation screw exhibited significantly higher axial stiffness than the DHSS group (P < 0.05). The GNS group exhibited the highest axial stiffness.
Interfragmental displacement
All specimens in the three groups survived all the cyclic loading tests. The mean depth of the inter-fragmentary displacement in each group was 2.61 mm for 3CS, 1.30 mm for DHS, and 1.15 mm for GNS. The fracture displacement of the GNS group was not significantly different from that of the DHSS group (P = 0.277), which indicated that the GNS construct had a cyclic compressive loading resistance similar to that of DHSS. Group 3CS exhibited the largest interfragmentary displacement compared to that of the other two groups (P < 0.001). In the case of intramedullary fixation with an anti-rotation screw, the interfragmental displacements were comparable to those of the standard fixation of the DHSS.
Load to failure
The corresponding failure load values were 2699.3 ± 950.2 N for 3CS, 3427.1 ± 759.3 N for DHSS, and 3758.9 ± 672.1 N for GNS (Fig. 5). GNS and DHSS had significantly higher values than the 3CS (P < 0.05). In contrast, no significant differences were observed between the GNS and DHSS groups (P = 0.052).
Type of failure
The maximal loading of all the samples was reached before the vertical compression height of the structure got to 15 mm. Catastrophic fractures were observed in seven samples: two 3CS, three DHSS, and two GNS samples. The other samples in the three groups mainly exhibited femoral leg shortening, which was derived from movements of the superior femoral head along the vertical direction.
Representative photographs captured after the onset of failure are shown in Fig. 3. The catastrophic fracture type of the 3CS was proximal femoral fracture through the cannulated screw axis. However, the catastrophic fracture types of DHSS and GNS were viewed as splitting and rotation of the femoral head (Fig. 4).
Discussion
To most young patients with femoral neck fractures, preserving the femoral head and internal fixation are still the first choice up to the present time. Unstable fixation of the femoral head is one of the main reasons for non-union and necrosis of the femoral head after operation2,32. Extramedullary fixation for treating UFNFs is primary method, for example CSs, DHS, and FNS8,9,10. To increase further stability of fixation for treating UFNFs, some surgeons have tried to use some modified techniques. Ye et al. used a medial buttress plate to enhance mechanical stability of three CSs in the fixation of such fractures33. Yet, this fixation method will increase local trauma and further decrease the remaining blood supply of the femoral head. Satish et al. tried to use four CSs to increase the whole stability for treating UFNFs. However, planning an ideal configuration of four CSs in cross section of femoral neck is very difficult, especially when there is no computer-assisted navigation and positioning34. Some recent years, surgeons preferred to use FNS to fix UFNFs, and some biomechanical studies have shown that it has better biomechanical advantages than that of three CSs and comparable stability to DHS12. But, FNS is still an extramedullary fixation with a long moment. Although intramedullary fixation device has better biomechanical performance than that of extramedullary fixation, there is no special intramedullary implant for treating these fractures.
In the current study, our aim was to assess the biomechanical performance of the GNS for the fixation of UFNFs and compare it with the standard fixation strategies of three parallel cannulated screws and a DHSS. The biomechanical results demonstrated that the GNS showed superior construct performance over the 3CS in terms of initial axial stiffness, interfragmental displacement, and load to failure during the loading test. When compared to the DHSS, the GNS exhibited similar biomechanical performance, including interfragmental displacement after cyclic compressive testing and load to failure. Additionally, the GNS displayed a higher initial axial stiffness than the DHSS (P < 0.05).
The Gamma 3 nail is a common and well-established intramedullary implant used for fixing intertrochanteric fractures. Previous studies have suggested that patients treated with intramedullary nails for intertrochanteric fractures experience faster and better mobilization compared to those fixed with sliding hip screws35,36,37,38. In this study, we employed Gamma 3 nails combined with an anti-rotation nail to treat unstable Pauwels III femoral neck fractures. Bonnaire et al.39 demonstrated that an anti-rotation screw acts as a rotational safeguard, enabling early full loading in the treatment of dislocated femoral neck fractures fixed with DHS without osteosynthesis failure. Therefore, in our study, an anti-rotation screw was utilized to enhance the biomechanical stability of the Gamma 3 nail.
The DHSS demonstrated a higher initial axial stiffness than the 3CS in the inverted trigonometry configuration (P < 0.05). However, Bliven et al.29 conducted a study using a model based on fresh-frozen human femora, similar to the one explored in this study, and demonstrated that the DHSS and 3CS (inverted trigonometry) exhibited similar initial axial stiffness. One possible reason for this difference could be that the model used in this study was composed of synthetic bone rather than cadaveric bone. Karl et al.12 concluded that although no statistical significance was found, the mean axial stiffness of the DHSS was greater than that of the 3CS (inverted trigonometry) in Pauwels III femoral neck fractures of fresh-frozen human cadaveric femora. However, other studies have shown that for vertical fractures of the femoral neck, the DHSS construct provided stronger biomechanical advantages compared to the 3CS in an inverted triangle configuration, in human cadavers39,40 and synthetic femora41. These findings suggest that the DHSS fixation system achieved greater biomechanical stability, attributed to its angular stability, when compared to the 3CS construct.
The Gamma 3 nail system theoretically has stronger angular stability than the DHSS due to the change in lag screw support from extramedullary to intramedullary. However, an important drawback of the Gamma 3 nails in treating femoral neck fractures is the insertion of an anti-rotation screw, which can be challenging for surgeons due to the blockage of the proximal intramedullary nail. Therefore, the anatomy of the femoral neck was reexamined and studied in this research. Given the oblique oval anatomical structure of the femoral neck, it is possible to implant an anti-rotation screw in the anterosuperior position of the femoral neck. In the current study, the GNS exhibited the highest axial stiffness during initial loading, but both the GNS and DHSS demonstrated similar biomechanical properties in terms of interfragmental displacement and load to failure. The mechanical environment of the injury during the primary postoperative stages is crucial for achieving satisfactory hip joint function. For UFNFs in younger patients, achieving successful fracture healing necessitates anatomical reduction and stabilization of the fractures. The higher load to failure demonstrated by the GNS and DHSS also provides clinical benefits by reducing the risk of cut-out and screw penetration, which are common causes of implant failure, especially in the elderly42.
In this study, the common observation in the 3CS group with failure to load was the splitting of the proximal femur along the axis of the cannulated screws (Fig. 3). However, both the GNS and DHS primarily exhibited collapse and sinking of the femoral head at the end of the failure to load. These findings indicate that angular stable implants provide better mechanical stability compared to the 3CS implants, allowing for early weight-bearing exercises. Meanwhile, GNS can protect the lateral cortex of the proximal femur, and its effect is the same as DHSS. limitations were present in this study. The composite bone fracture model used differs significantly from the actual clinical situation compared to the cadaveric femoral neck fracture model. However, the composite bone model ensured greater consistency in the fracture model and experimental data. Synthetic femurs are more accessible and manageable than cadaver specimens. Moreover, vertical femoral neck fractures are more common in younger patients and differ from most cadaveric bones, which are inherently osteoporotic. The synthetic model provided denser cancellous bone, allowing for a better simulation of real-life scenarios. The insertion of an anti-rotation screw in the superior position of the Gamma 3 lag screw proved to be challenging. However, given the anatomical structure of the femoral neck, the anterosuperior position can accommodate the anti-rotation screw effectively. Notably, the study did not simulate the functions of the joint capsule, ligaments, and muscle soft tissues, despite their significant roles in hip stabilization and function. Furthermore, all specimens were implanted by a single surgeon following the instruction manual. However, minor deviations in implant position and direction may have occurred within controllable conditions, especially during the insertion of the anti-rotation screw.
Conclusions
The GNS demonstrated significantly higher initial axial stiffness compared to the other two standard fixation methods in an unstable femoral neck fracture model. When considering the failure load and loss of fracture reduction in the 3CS group, both the GNS and DHSS exhibited similar or better biomechanical properties in fixing Pauwels type III femoral neck fractures. These findings suggest that the Gamma 3 system, with an anti-rotation screw, offers sufficient biomechanical stability for UFNFs, broadening its potential applications. The GNS may serve as a promising alternative to the hip-screw system for UFNFs with extensive posterior comminution. However, the applicability of these results to patients should be further investigated through clinical studies.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Gullberg, B., Johnell, O. & Kanis, J. A. World-wide projections for hip fracture. Osteoporos. Int. 7, 407–413 (1997).
Parker, M. J. The management of intracapsular fractures of the proximal femur. J. Bone Jt. Surg. 82, 937–941 (2000).
Gnudi, S., Sitta, E. & Pignotti, E. Prediction of incident hip fracture by femoral neck bone mineral density and neck-shaft angle: A 5-year longitudinal study in post-menopausal females. Br. J. Radiol. 85, e467-473 (2012).
Augat, P., Bliven, E. & Hackl, S. Biomechanics of femoral neck fractures and implications for fixation. J. Orthop. Trauma. 33(Suppl 1), S27–S32 (2019).
Damany, D. S., Parker, M. J. & Chojnowski, A. Complications after intracapsular hip fractures in young adults. A meta-analysis of 18 published studies involving 564 fractures. Injury. 36, 131–141 (2005).
Zlowodzki, M. et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: A multi-centre cohort study. J. Bone Jt. Surg. 90, 1487–1494 (2008).
Blomfeldt, R. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J. Bone Jt. Surg. 87, 1701–1702 (2005).
Nauth, A. et al. Fracture fixation in the operative management of hip fractures (FAITH): An international, multicentre, randomised controlled trial. Lancet. 389, 1519–1527 (2017).
Florschutz, A. V., Langford, J. R., Haidukewych, G. J. & Koval, K. J. Femoral neck fractures: Current management. J. Orthop. Trauma. 29, 121–129 (2015).
Ma, J. X. et al. Sliding hip screw versus cannulated cancellous screws for fixation of femoral neck fracture in adults: A systematic review. Int. J. Surg. 52, 89–97 (2018).
Schwartsmann, C. R., Lammerhirt, H. M., Spinelli, L. D. F. & Neto, A. D. S. U. Treatment of displaced femoral neck fractures in young patients with DHS and its association to osteonecrosis. Rev. Bras. Ortop. 53, 82–87 (2018).
Stoffel, K., IvanGras, F., ChristophEberli, U., DavidOswald, M. & Boyko, G. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws. J. Orthop. Trauma. 31, 131–137 (2017).
Bäcker, H. C. et al. Breakage of intramedullary femoral nailing or femoral plating: How to prevent implant failure. Eur. J. Med. Res. 27, 7 (2022).
Wu, K. T. et al. Ipsilateral femoral neck and shaft fractures fixation with proximal femoral nail antirotation II (PFNA II): Technical note and cases series. J. Orthop. Surg. Res. 15, 20 (2020).
Tornetta, P. 3rd., Kain, M. S. & Creevy, W. R. Diagnosis of femoral neck fractures in patients with a femoral shaft fracture. Improvement with a standard protocol. J. Bone Jt. Surg. Am. 89, 39–43 (2007).
Baghel, A., Keshav, K., Kumar, A. & Sharma, P. Clinicoradiological outcome of concomitant fractures of proximal femur and femoral shaft treated with second-generation cephalomedullary nailing. Cureus. 13, e15381 (2021).
Vidyadhara, S. & Rao, S. K. Cephalomedullary nails in the management of ipsilateral neck and shaft fractures of the femur–one or two femoral neck screws. Injury. 40, 296–303 (2009).
Tsarouhas, A., Hantes, M. E., Karachalios, T., Bargiotas, K. & Malizos, K. N. Reconstruction nailing for ipsilateral femoral neck and shaft fractures. Strateg. Trauma Limb Reconstr. 6, 69–75 (2011).
Singh, R. et al. Ipsilateral femoral neck and shaft fractures: A retrospective analysis of two treatment methods. J. Orthop. Traumatol. 9, 141–147 (2008).
Hak, D. J., Mauffrey, C., Hake, M., Hammerberg, E. M. & Stahel, P. F. Ipsilateral femoral neck and shaft fractures: Current diagnostic and treatment strategies. Orthopedics. 38, 247–251 (2015).
Rana, R., Behera, H., Behera, S. 2nd., G, A. & Singh, M. Outcomes of ipsilateral femoral neck and shaft fractures treated with proximal femoral nail antirotation 2. Cureus. 13, e18511 (2021).
Oh, C. W. et al. “Reverse miss-a-nail technique” of reconstruction nailing for successful fixation of the ipsilateral femoral neck and shaft fracture. Arch. Orthop. Trauma Surg. 141, 959–969 (2021).
Spitler, C. A., Kiner, D., Swafford, R., Bruce, J. & Nowotarski, P. Treatment of ipsilateral femoral neck and shaft fractures with cannulated screws and antegrade reconstruction nail. J. Orthop. Trauma. 34, e176–e180 (2020).
Kilian, M. et al. Locking plate fixation with multiple telescoping sliding screws for femoral neck fractures. Ortop. Traumatol. Rehab. 20, 493–498 (2018).
Zhu, Q., Shi, B., Xu, B. & Yuan, J. Obtuse triangle screw configuration for optimal internal fixation of femoral neck fracture: An anatomical analysis. Hip Int. 29, 72–76 (2019).
Kate, B. R. Anteversion versus torsion of the femoral neck. Acta Anatom. 94, 457–463 (1976).
Zhang, R. Y. et al. The oval-like cross-section of femoral neck isthmus in three-dimensional morphological analysis. Orthop. Surg. 13, 321–327 (2021).
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D. & Kellam, J. F. Fracture and dislocation classification compendium-2018. J. Orthop. Trauma. 32(Suppl 1), S1–S170 (2018).
Bliven, E., Sandriesser, S., Augat, P., von Rüden, C. & Hackl, S. Biomechanical evaluation of locked plating fixation for unstable femoral neck fractures. Bone Jt. Res. 9, 314–321 (2020).
Nowotarski, P. J. et al. Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel’s type C femoral neck fractures. Injury. 43, 802–806 (2012).
Kuan, F. C. et al. Biomechanical properties of off-axis screw in Pauwels III femoral neck fracture fixation: Bicortical screw construct is superior to unicortical screw construct. Injury 50, 1889–1894 (2019).
Slobogean, G. P., Sprague, S. A., Scott, T. & Bhandari, M. Complications following young femoral neck fractures. Injury. 46, 484–491 (2015).
Ye, Y. et al. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: Surgical technique and preliminary results. Injury. 48, 2189–2193 (2017).
Jaiswal, A., Tanwar, Y. S. & Habib, M. Four quadrant parallel peripheral screw fixation for displaced femoral neck fractures in elderly patients. Indian J. Orthop. 47, 532–533 (2013).
Ekström, W., Karlsson-Thur, C., Larsson, S., Ragnarsson, B. & Alberts, K. A. Functional outcome in treatment of unstable trochanteric and subtrochanteric fractures with the proximal femoral nail and the Medoff sliding plate. J. Orthop. Trauma. 21, 18–25 (2007).
Hardy, D. C. et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J. Bone Jt. Surg. Am. 80, 618–630 (1998).
Pajarinen, J., Lindahl, J., Michelsson, O., Savolainen, V. & Hirvensalo, E. Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J. Bone Jt. Surg. 87, 76–81 (2005).
Utrilla, A. L., Reig, J. S., Muñoz, F. M. & Tufanisco, C. B. Trochanteric gamma nail and compression hip screw for trochanteric fractures: A randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J. Orthop. Trauma. 19, 229–233 (2005).
Bonnaire, F. A. & Weber, A. T. Analysis of fracture gap changes, dynamic and static stability of different osteosynthetic procedures in the femoral neck. Injury. 33(Suppl 3), C24-32 (2002).
Aminian, A. et al. Vertically oriented femoral neck fractures: Mechanical analysis of four fixation techniques. J. Orthop. Trauma. 21, 544–548 (2007).
Imren, Y. et al. Biomechanical comparison of dynamic hip screw, proximal femoral nail, cannulated screw, and monoaxial external fixation in the treatment of basicervical femoral neck fractures. Acta Chir. Orthop. Traumatol. Cech. 82, 140–144 (2015).
Yih-Shiunn, L., Chien-Rae, H. & Wen-Yun, L. Surgical treatment of undisplaced femoral neck fractures in the elderly. Int. Orthop. 31, 677–682 (2007).
Acknowledgements
I wish to thank professor Teng Ma for his valuable suggestion in the whole manuscript. All other authors should also be appreciated for their contributions. The successful completion of the experiment and article comes from the efforts of everyone.
Author information
Authors and Affiliations
Contributions
Collected, analyzed and interpreted the data, Wrote the primary manuscript, DY.L., Q.H., and CF.W.; methodology, C.R.; data curation, YB.X.; formal analysis, CJ.H.; validation, K.Z.and DW.Z.; writing-review and editing, CM.Z., T.M. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, D., Huang, Q., Wang, C. et al. Biomechanical evaluation of Gamma 3 nail with anti-rotation screw fixation for unstable femoral neck fractures: a biomechanical study. Sci Rep 14, 19356 (2024). https://doi.org/10.1038/s41598-024-70346-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70346-1
- Springer Nature Limited