Abstract
Staphylococcus aureus infections are hard to treat due to the emergence of antibiotic resistant strains, as well as their ability to form biofilms. The MazEF toxin–antitoxin system is thought play a role in bacterial biofilm phenotype as well as antibiotic resistance. In S. aureus, the physiologic function of the mazEF gene in the disease transition from acute to chronic infection is not well understood. In methicillin resistant S. aureus (MRSA), loss of mazF expression results in loss of resistance to first generation cephalosporins. mazF::tn displayed sensitivity while the isogenic wild type (WT) remained resistant. mazF::tn displayed significantly increased growth of biofilms on metal implants over 48 h compared to WT and the complemented transposon mutant. mazF::tn biofilms displayed significantly decreased antibiotic tolerance to vancomycin and cefazolin in comparison to WT and complement biofilms. Mice given mazF::tn in a sepsis model displayed less abscess burden and increased survival (100%) when treated with cefazolin compared to WT bacteremia treated with cefazolin (20%). mazF::tn periprosthetic joint infections displayed increased biofilm burden at acute time points and decreased biofilm burden at chronic time points. Our data suggests MazEF in MRSA is responsible for controlling growth of biofilms, antibiotic tolerance, and influence chronic infections in vivo.
Similar content being viewed by others
Introduction
Methicillin resistant Staphylococcus aureus (MRSA) infections are a major concern in surgical procedures, including orthopaedic surgery accounting for 50% of all S. aureus infections1,2. Clinical treatment for these infections is dependent on the antibiotic resistance profile determined using the Clinical and Laboratory Standards Institute (CLSI) broth microdilution assay for minimum inhibitory concentrations (MIC). Infectious Diseases Society of America (IDSA) guidelines recommend a first-generation cephalosporin for Methicillin susceptible S. aureus (MSSA), and either the cell envelope targeting daptomycin or the glycoprotein vancomycin for methicillin resistant S. aureus (MRSA)3. MRSA infections display twice the mortality rate of MSSA infections4. Further complicating matters, MSSA and MRSA can develop extensive biofilms on implants and contact tissue. S. aureus biofilms can be highly tolerant and difficult to eliminate5,6,7,8.
An altered bacterial metabolism is needed for antibiotic survival and growth of biofilms, which is accomplished by multiple stress response signaling systems including toxin–antitoxin systems9,10,11,14,15,16,17,18,19,20,21. The most well-known and widely studied chromosomal toxin–antitoxin (TA) system in S. aureus is the MazEF system11,12,13. The MazF toxin has been shown to act as an endoribonuclease cleaving specific sequences in transcripts of many bacterial metabolic processes including protein synthesis, cell wall production, cell division, and virulence factors14,15. Studies have shown that planktonic S. aureus cells lacking MazF expression displayed increased sensitivity to beta-lactam antibiotics12 and increased biofilm production13 in comparison to their corresponding wild type (WT) strains.
There can be variation between an antibiotic resistance genotype and phenotype, induced by different culture and environmental conditions16. Quantifying clinical antibiotic sensitivity using the CLSI protocol in Muller Hinton Broth may fail to replicate the actual metabolic and environmental conditions of the infection, leading to a variation between the actual and measured antibiotic resistance phenotype17,18. (R2.1) In an earlier study, we utilized WT JE2 along with the previously described JE2 mutant lacking mazEF expression (mazF::tn) as well as this mutant with expression added back in trans (mazF::tn + complement)19 and determined the growth rate and ability to form biofilms in mazF::tn was increased. As environmental stress regulation has been shown to influence antibiotic sensitivity in S. aureus, we utilized the same JE2 mazF transposon mutant in MRSA strain JE2 to further understand how this toxin antitoxin system is involved in antibiotic resistance and pathogenesis. Our objectives were to (1) test the susceptibility of MRSA laboratory and clinical isolates to cefazolin when grown in mammalian serum, (2) evaluate control of mazEF in MRSA antibiotic sensitivity, (3) evaluate how MazEF contributes to chronic infection of MRSA in vivo using sepsis and surgical implant infection animal models.
Results
Culturing MRSA isolates in mammalian serum results in phenotypic sensitivity to the beta-lactam antibiotic cefazolin
To determine if serum can influence antibiotic sensitivity, the MIC of cefazolin and vancomycin were first tested against MRSA USA300 JE2 planktonic cells cultured in MHB, TSB, and fetal bovine serum (FBS). FBS has antimicrobial properties against certain bacterial species and strains, so the ability of strains to grow reliably in this culture media was initially determined. Growth curves of each strain in each culture condition was determined using serially diluted CFU analysis over 24 h. Stains did not display significantly reduced CFU after 24 h of culture in FBS compared to MHB (data not shown). As expected, JE2 predictively displayed resistance to the beta-lactam antibiotic cefazolin and sensitivity to the glycoprotein vancomycin when grown in microbiological broths (MHB and TSB). However, when cultured in FBS, JE2 surprisingly displayed susceptibility to cefazolin with an MIC of 1 µg/mL (Table 1). After observing the reduced cefazolin resistance of JE2 in FBS, we questioned if this phenotype existed in other common MRSA laboratory strains. The laboratory MRSA strains USA300 LAC300 and USA400 MW2 exhibited decreased cefazolin MICs in FBS compared to MHB (Table 1). However, MRSA strains COL and USA200 MRSA 252 retained high level cefazolin resistance in FBS. Given JE2 and similar MRSA laboratory strains’ reduced cefazolin resistance in FBS compared to MHB, we decided to test if MRSA clinical isolates obtained from our registry displayed the same phenotype. Using MRSA isolates collected from patients presenting with periprosthetic joint infections, we conducted vancomycin and cefazolin MIC tests in MHB and FBS. (R1.8) Like the laboratory strains, this difference disappeared when tested in FBS. These clinical isolates had a MIC90 of 96 μg/mL in MHB which decreased to 2.0 μg/mL in FBS (Table 1).
Loss of mazEF expression in MRSA increases planktonic cell and biofilm susceptibility to cefazolin
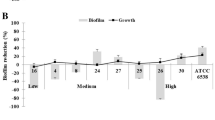
Planktonic MRSA cultures were subjected to fold increases of cefazolin and vancomycin to obtain MIC values. When grown in MHB, mazF::tn displayed sensitivity to cefazolin (MIC-1 µg/mL) while WT and mazF::tn + complement remained resistant to the beta-lactam antibiotic (MIC > 96 µg/mL) (Table 2). When grown in FBS mazF::tn displayed a reduction in cefazolin MIC compared to WT and mazF::tn + complement (Table 2). WT, mazF::tn, and mazF::tn + complement biofilms cultured on metal implant pieces and treated with 10×MIC of cefazolin or vancomycin. After 24 h of treatment, neither cefazolin nor vancomycin were able to achieve an over 99.9% reduction of bacterial burden of WT and complement strains when grown in MHB (Fig. 1A). In comparison, mazF::tn biofilms were reduced well over 99.9% when treated with either cefazolin or vancomycin (Fig. 1A). Biofilm antibiotic tolerance was reduced when grown in FBS compared to MHB. When grown in FBS cefazolin and vancomycin both failed to achieve over 99.9% reduction (< 0.1% survival) in WT and complemented strains while this was achieved in mazF::tn biofilms (Fig. 1B). JE2 strains were grown as mature biofilms on metal implant pieces over 48 h in MHB or FBS. After washing and sonication of implants, CFU analysis of sonicate samples showed mazF::tn established significantly more biofilm compared to WT and mazF::tn + complement when grown in both media types (Fig. 1C).
MRSA lacking mazEF expression displays sensitivity to cefazolin and increased growth of planktonic cells and mature biofilms. Biofilms of each strain were treated with 10×MIC of cefazolin and vancomycin for 24 h in MHB (A) or FBS (B) and percent survival compared to untreated controls was performed. mazF::tn displayed increased susceptibility to cefazolin and vancomycin in both media conditions compared to WT and complement strains. Colony forming unit analysis displayed mazF::tn grew significantly more biofilms on implant material compared to WT and mazF::tn + complement in both MHB and FBS (*p < 0.05) (C).
mazEF::tn sepsis can be effectively treated with cefazolin in vivo
Our previous work displayed differences in muscle abscess burden and vancomycin treatment efficacy in vivo using JE2 WT and JE2 mazF::tn strains19. To further test the observed re-sensitization to cefazolin in vivo, a murine sepsis model was utilized. Mice were given an intravenous challenge of S. aureus strains, divided into untreated, cefazolin, and vancomycin treated groups, and followed for 7 days. WT challenged mice displayed 80% mortality in the untreated and cefazolin treated groups, while the vancomycin group displayed 0% mortality (Fig. 2A). At the time of euthanasia, animal tissue (liver, kidney, spleen, and lung) was harvested and processed to obtain metastatic abscess burden resulting from sepsis. In WT challenged mice, the vancomycin treated group displayed significantly reduced abscess burden in the liver, kidney, and spleen compared to the untreated group (*p < 0.05) (Fig. 2B). Cefazolin treated mice displayed equivalent burden compared with untreated mice. mazF::tn challenged mice displayed 80% mortality in the untreated group, while the vancomycin and cefazolin groups displayed 0% mortality (Fig. 2C). For mazF::tn challenged mice, metastatic abscess burden in the liver, kidney, and spleen of vancomycin and cefazolin treated groups displayed significantly reduced burden compared to the untreated group (*p < 0.05) (Fig. 2D).
mazEF::tn sepsis can be effectively treated in vivo using cefazolin. Intravenous infection was given by retro-orbital challenge using a mouse sepsis model (n = 5). In JE2 WT sepsis, untreated and cefazolin treated groups displayed similar mortality ~ 20%, compared to vancomycin treated group (A). At time of euthanasia, intraperitoneal organs were collected and processed to determine metastatic abscess formation of blood borne infection. In JE2 WT sepsis, there were significant reductions in organ abscess burden in the vancomycin treated group compared to untreated group (B). In mazF::tn sepsis, cefazolin and vancomycin treated groups displayed similar mortality ~ 100% compared to untreated group (C). Cefazolin and vancomycin treated groups displayed significantly reduced metastatic abscess burden compared to the untreated group (*p < 0.05) (D).
mazEF aids S. aureus in developing chronic implant infections in vivo
As S. aureus are a notorious pathogen responsible for a myriad of disparate infections, we wanted to examine how the mazEF::tn would behave during pathogenesis of a biomedical implant infection. S. aureus is the most common pathogen observed in periprosthetic joint infection, and bacterial biofilms growing on implanted material and surrounding tissue is responsible for chronic infections6,20. We utilized a murine PJI model wherein metal implants are inserted into reamed femoral bone followed by inoculation with S. aureus strains. All animals were followed for 14 days and we observed 0% mortality in all mice tested. mazF::tn displayed increased biofilm burden on infected implants at the acute time points of 1- and 3-days post infection compared to WT, while displaying decreased counts on chronic time points of 7- and 14-days poste infection (Fig. 3A). Quantification of biomedical implant biofilm burden displayed that mazF::tn had significantly increased acute burden compared to WT (Fig. 3B) and less burden during chronic infection (Fig. 3C). Analysis of biofilm burden was repeated in surrounding tissue and we observed a similar pattern of increased burden at acute time points and decreased burden at chronic time points (Fig. 3D–F).
Loss of mazEF expression decreases survival of MRSA during chronic PJI in vivo. Mice given PJI were euthanized at 1-, 3-, 7-, and 14-day post infection (n = 3 per group). Infected implants were quantified over time (A). Acute (days 1 and 3) and chronic (days 7 and 14) displayed mazF::tn increased acute bacterial burden (**p < 0.01) (B) and decreased chronic bacterial burden (C) compared to WT. Proximal bone tissue of infected joint also displayed this same trend as implants (*p < 0.05) (D–F).
Discussion
Previous studies have displayed that the absence of the MazEF toxin antitoxin system in S. aureus can result in increased susceptibility to beta-lactam antibiotics12. We have shown here, MRSA resistance to cefazolin is dramatically reduced when cultured in mammalian serum compared to standard microbiological growth medium, at least in some strains. Additionally, MRSA lacking mazEF expression displayed a reduction in resistance to cefazolin and a significant increase in biofilm formation on metal implant material when cultured MHB and mammalian serum. MRSA JE2 lacking mazEF expression displayed decreased mortality in a murine bacteremia model when treated with cefazolin compared to WT bacteremia. For the first time using in vivo models, we have additionally demonstrated the toxin–antitoxin system mazEF acts to inhibit biofilm formation and promote biofilm antibiotic tolerance, which allows S. aureus to transition from an acute to a chronic infection which is less virulent but more antibiotic tolerant.
The presence of an antibiotic resistance gene does not guarantee its expression21. How mammalian serum is contributing to attenuation of beta-lactam resistance in MRSA is not currently understood. Other groups have shown serum can both enhance and attenuate antimicrobial action against S. aureus. Human serum was involved in manipulating antibiotic tolerance, which was shown to be due to host defense peptides such as LL-37 engaging with the staphylococcal GraRS two-component system22. Mammalian serum apolipoprotein A-I has been shown to potentiate the therapeutic effects of lysocin E against S. aureus23. Additionally, multiple clinical studies have demonstrated possible therapeutic benefits and improved clinical outcomes in MRSA sepsis when dual therapy with vancomycin or daptomycin and the beta lactam antibiotic, cefazolin, is used as compared to monotherapy alone (vancomycin or daptomycin). A prospective randomized clinical study comparing dual therapy to standard of care monotherapy was halted as the monotherapy group had higher rates of mortality as compared to combination therapy24. In a second randomized prospective study, dual therapy decreased the overall time of bacteremia as compared to monotherapy25. Based on this and the unexpected benefit of dual therapy in MRSA infections with a beta-lactam antibiotic, an antibiotic for which the bacteria possess a resistance genotype, we questioned if there was a variability in the resistance phenotype of the first-generation cephalosporin, cefazolin, between physiologically relevant media, mammalian serum, and MHB. Additionally, we questioned how the mazEF system exerts control over antibiotic resistance and infection severity in vivo by using a MRSA mutant lacking mazEF expression.
Bacterial toxin antitoxin systems are thought to be involved in environmental stress signaling and directly connected to other regulatory networks, such as mazEF and its genetic proximity being adjacent to the rsbUVWsigB operon. As such, better understanding of the link between toxin antitoxin systems and S. aureus pathophysiology will reveal if these systems are druggable targets. Previous work has displayed S. aureus deficient in mazF expression have increased beta-lactam sensitivity compared to the parental strain12. Overexpression of mazF has previously shown to reduce growth rate of S. aureus and mazF mutants displayed increased biofilm growth13. RNA-seq, Ribo-seq, and mass spectrometry was more recently performed on a S. aureus deficient in mazEF compared to the strain overexpressing mazF. Analysis of both canonical and a new extended target repertoire of the endoribonuclease MazF identified hundreds of cleaved products including many enzymes of cell wall production including penicillin binding proteins 1 and 2 (PBP1 and PBP2) which are the targets of beta lactam antibiotics14. These same S. aureus strains further displayed that a mazEF deficiency results in decreased cell wall thickness and increased cellular division rate15. MSSA and MRSA clinical isolates were analyzed for ability to form biofilm and PCR was performed to determine mazEF expression. MRSA isolates were able to make significantly more biofilms than MSSA isolates and mazEF expression was significantly correlated to methicillin resistance26.
This study has several limitations including use of only one MRSA strain when comparing how mazEF expression contributes to S. aureus metabolism and pathogenicity. An analysis of how MRSA, MSSA, methicillin sensitive Staphylococcus epidermidis (MRSE) and MSSE deficient in mazEF could further show global control of antibiotic tolerance and biofilm production. We only tested two antibiotics cefazolin and vancomycin, both which target cell wall production. A larger screen of clinically used antibiotics of differing classes (RNA, DNA, cell membrane targeting) could further display mazEF contribution to wider antibiotic tolerance. Last, CFU quantitation analysis was used for determination of biofilm burden on implants, no SEM or other qualitative were performed and included in our analysis. Our analysis here displayed that only some of the laboratory and clinical MRSA isolates were able to reverse their resistance to beta-lactam cefazolin when cultured in FBS. Future work will include characterization of the specific genetic elements of resistance among these laboratory and clinical strains, and how this may result in attenuation of resistance when exposed to FBS.
S. aureus antibiotic resistance and ability to grow into mature biofilms are major healthcare and public health issues. Understanding how S. aureus toxin–antitoxin systems influence pathophysiology in several different infection models will better reveal if they are druggable targets. We have shown that S. aureus can maintain chronic infections through a controlled balance between growth of cells and biofilms as well as antibiotic tolerance. The MazEF toxin antitoxin been shown to reduce biofilm growth but also increase sensitivity to beta lactam antibiotics and vancomycin. Targeting the MazEF toxin antitoxin system in chronic MRSA infection could result in increased antibiotic efficacy.
Methods
Bacterial cell culture
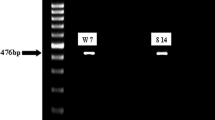
USA300 JE2 was obtained from ATCC. USA300 LAC300, USA400 MW2, COL, and USA200 MRSA 252, were kindly donated by Dr. Anthony Richardson. Institutional Review Board (IRB) guidelines and regulations were followed for the use of clinically derived MRSA strains. For all in vitro and in vivo experiments, S. aureus reference and mutant strains were used from previous studies19. A USA300 MRSA JE2 (ATCC) was used along with USA300 JE2 which underwent transposon mutagenesis (Nebraska Tn Mutant Library) to eliminate expression of mazEF (mazF::tn). We also utilized mazF::tn with complementary expression of mazEF added back by cloning into a pLZ12 shuttle vector (mazF::tn + complement)19. The mediums employed for in vitro testing assay for all organisms were Mueller–Hinton Broth (MHB) (Becton Dickinson), and heat inactivated fetal bovine serum (FBS) (Gibco).
Planktonic growth assays and doubling times
All strains were inoculated in Tryptic Soy Broth (TSB, Bectin Dickinson and Company) overnight at 37 °C with shaking at 250 rpm. Strains were diluted in Mueller Hinton Broth (MHB; Bectin Dickinson and Company) to a final concentration of 0.5 × 106 CFU/mL using the 0.5 MacFarland Standard (GFS Chemicals) and an Infinite M200 Spectrophotometer (Tecan). The optical density at 600 nm (OD600) absorbance, as well as quantitative colony forming unit (CFU) analysis on TSA II sheep blood CS100 (Remel) agar plates, was measured after 2 h, 8 h, and 24 h (Infinite M200; Tecan). Calculation of the doubling time was based on these measurements.
Planktonic cell antibiotic sensitivity
Broth dilution minimum inhibitory concentrations (MICs) and minimum bactericidal concentrations (MBCs) of cefazolin and vancomycin were determined in accordance with guidelines from the Clinical and Laboratory Standards Institute and our previous work27,28.
Growth of biofilms on arthroplasty material
Implant material was prepared from 0.6-mm diameter stainless steel Kirschner wire (Sklar Instruments) and cut into 6-mm length, autoclaved, and plated in wells along with S. aureus strains at 1 × 106 CFU/mL in MHB. After overnight culture, fresh MHB was exchanged to remove planktonic bacteria. At 48 h, wires with mature biofilm were washed in 1 of Dulbecco’s PBS (dPBS) and placed into 1 mL of 1% Tween 20 in dPBS. Implant pieces were sonicated for 10 min, sonicate was serial diluted, and plated on blood agar plates to obtain CFU counts for biofilm bacterial burden.
Biofilm antibiotic tolerance
Implant pieces were grown as above, and after 48 h implant pieces were washed with 1 mL of dPBS and then placed into cefazolin or vancomycin at 10×MIC (50 μg/mL and 100 μg/mL respectively) for 24 h. After treatment, they were placed in 1 mL sonication fluid consisting of 1% Tween 20 dPBS and sonicated for 10 min. The sonicate was serially diluted and plated on blood agar plates for CFU analysis. Reduction in CFUs was determined from the average of CFUs from untreated Kirschner wires of 48 h biofilms and after a dPBS wash prior to placing in PBS containing 1% Tween 20 (PBST) and sonicating for 10 min.
Murine sepsis model
All bacteremia experiments were performed after IACUC protocol approval in University of Pittsburgh Division of Laboratory Animal Resources, and authors complied with the ARRIVE guidelines. Twelve-week-old C57BL/6J female mice (The Jackson Laboratory) were used (n = 5). S. aureus strains were grown overnight in TSB before being resuspended to a concentration of 1 × 108 CFU/mL in PBS. 100 µL bacterial suspension was administered via retro-orbital injection and mice were monitored for 7 days. 100 µL of cefazolin and vancomycin were administered using an intra peritoneal injection immediately after S. aureus challenge at 50 mg/kg and 100 mg/kg respectively. Mice were euthanized at the end of the experiment (7 days post infection) or after losing 20% of their pre-infection weight as per IACUC guidelines. After euthanasia, mouse blood via cardiac puncture, lungs, spleen, liver, and kidney were obtained to determine colony forming units at these sites. All organs were individually homogenized and serial diluted before performing CFU analysis on blood agar plates.
Murine periprosthetic joint infection model
All experiments were performed under approved IACUC animal protocol in University of Pittsburgh Division of Laboratory Animal Resources, and the authors complied with the ARRIVE guidelines. Twelve-week-old C57BL/6J female mice (n = 3 per group per timepoint) (Jackson) were used for all experiments. Mice where anesthetized by 2% isoflurane, hair was removed from one leg and treated with betadine. With a scalpel, a medial parapatellar incision was made, and lateral displacement of the quadriceps-patellar complex allowed for visualization of the femoral intercondylar notch. With a 25-gauge needle, the femoral intramedullary canal was manually reamed. A 0.6 mm wide/6 mm long sterile Kirschner wire implant was inserted into the canal and was left protruding ~ 1 mm into the joint. The quadriceps-patellar complex was reduced back to midline and incision was closed using vicryl sutures27. An inoculation volume of 10 µL with 1 × 106 CFU of WT or MazEF was injected into the joint space. Mice were euthanized at 1-, 3-, 7-, and 14-days post infection. Kirschner wire implant as well as a ~ 2 mm × 2 mm piece of distal femur were removed and placed in PBS containing 1% Tween 20 on ice. Implants were sonicated for 10 min; the distal femur was mechanically homogenized for 30 s. All samples were serial diluted and CFU analysis on blood agar plates was performed.
Statistics
Survival statistics of animals was performed using a Kaplan–Meier log rank test. All in vitro and in vivo data was analyzed using descriptive statistics and multiple normality tests. Comparison between two groups was be analyzed using an unpaired t-test for parametric data or a Mann–Whitney test for non-parametric data. Comparison between more than two groups was analyzed using an ANOVA for parametric data or a Kruskal–Wallis test for non-parametric data. Data analysis was performed using Prism 9.0 (GraphPad, La Jolla CA). A p value < 0.05 was considered statistically significant.
Data availability
The data generated and analyzed during this study may be available from the corresponding author on a reasonable request to the corresponding author or the corresponding author’s delegate.
References
Lakhundi, S. & Zhang, K. Methicillin-resistant Staphylococcus aureus: Molecular characterization, evolution, and epidemiology. Clin. Microbiol. Rev. 31(4), e00020-18 (2018).
Panlilio, A. L. et al. Methicillin-resistant Staphylococcus aureus in U.S. hospitals, 1975–1991. Infect. Control Hosp. Epidemiol. 13(10), 582–586 (1992).
Liu, C. et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 52(3), e18-55 (2011).
Whitby, M., McLaws, M. L. & Berry, G. Risk of death from methicillin-resistant Staphylococcus aureus bacteraemia: A meta-analysis. Med. J. Aust. 175(5), 264–267 (2001).
Arciola, C. R., Campoccia, D., Ehrlich, G. D. & Montanaro, L. Biofilm-based implant infections in orthopaedics. Adv. Exp. Med. Biol. 830, 29–46 (2015).
Arciola, C. R., Campoccia, D. & Montanaro, L. Implant infections: Adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 16(7), 397–409 (2018).
Urish, K. L. et al. Antibiotic-tolerant Staphylococcus aureus biofilm persists on arthroplasty materials. Clin. Orthop. Relat. Res. 474(7), 1649–1656 (2016).
Zimmerli, W., Trampuz, A. & Ochsner, P. E. Prosthetic-joint infections. N. Engl. J. Med. 351(16), 1645–1654 (2004).
Tan, L., Li, S. R., Jiang, B., Hu, X. M. & Li, S. Therapeutic targeting of the Staphylococcus aureus accessory gene regulator (agr) system. Front. Microbiol. 9, 55 (2018).
Yarwood, J. M., Bartels, D. J., Volper, E. M. & Greenberg, E. P. Quorum sensing in Staphylococcus aureus biofilms. J. Bacteriol. 186(6), 1838–1850 (2004).
Schuster, C. F. & Bertram, R. Toxin–antitoxin systems of Staphylococcus aureus. Toxins (Basel) 8(5), 140 (2016).
Schuster, C. F. et al. The MazEF toxin–antitoxin system alters the beta-lactam susceptibility of Staphylococcus aureus. PLoS One 10(5), e0126118 (2015).
Kato, F., Yabuno, Y., Yamaguchi, Y., Sugai, M. & Inouye, M. Deletion of mazF increases Staphylococcus aureus biofilm formation in an ica-dependent manner. Pathog. Dis. https://doi.org/10.1093/femspd/ftx026 (2017).
Sierra, R. et al. Insights into the global effect on Staphylococcus aureus growth arrest by induction of the endoribonuclease MazF toxin. Nucleic Acids Res. 48(15), 8545–8561 (2020).
Bezrukov, F., Prados, J., Renzoni, A. & Panasenko, O. O. MazF toxin causes alterations in Staphylococcus aureus transcriptome, translatome and proteome that underlie bacterial dormancy. Nucleic Acids Res. 49(4), 2085–2101 (2021).
Hughes, D. & Andersson, D. I. Environmental and genetic modulation of the phenotypic expression of antibiotic resistance. FEMS Microbiol. Rev. 41(3), 374–391 (2017).
Radlinski, L. & Conlon, B. P. Antibiotic efficacy in the complex infection environment. Curr. Opin. Microbiol. 42, 19–24 (2018).
Ersoy, S. C. et al. Correcting a fundamental flaw in the paradigm for antimicrobial susceptibility testing. EBioMedicine 20, 173–181 (2017).
Ma, D. et al. The toxin–antitoxin MazEF drives Staphylococcus aureus biofilm formation, antibiotic tolerance, and chronic infection. mBio 10(6), e0165819 (2019).
Conlon, B. P., Rowe, S. E. & Lewis, K. Persister cells in biofilm associated infections. Adv. Exp. Med. Biol. 831, 1–9 (2015).
Zuniga, E. et al. Expression of genes encoding resistance in Staphylococcus spp. isolated from bovine subclinical mastitis in Brazil. J. Infect. Dev. Ctries. 14(7), 772–780 (2020).
Ledger, E. V. K., Mesnage, S. & Edwards, A. M. Human serum triggers antibiotic tolerance in Staphylococcus aureus. Nat. Commun. 13(1), 2041 (2022).
Hamamoto, H. et al. Serum apolipoprotein A-I potentiates the therapeutic efficacy of lysocin E against Staphylococcus aureus. Nat. Commun. 12(1), 6364 (2021).
Geriak, M. et al. Clinical data on daptomycin plus ceftaroline versus standard of care monotherapy in the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob. Agents Chemother. 63(5), e02483-18 (2019).
Tong, S. Y. C. et al. Effect of vancomycin or daptomycin with vs without an antistaphylococcal beta-lactam on mortality, bacteremia, relapse, or treatment failure in patients with MRSA bacteremia: A randomized clinical trial. JAMA 323(6), 527–537 (2020).
Abd El Rahman, A., El Kholy, Y. & Shash, R. Y. Correlation between mazEF toxin–antitoxin system expression and methicillin susceptibility in Staphylococcus aureus and its relation to biofilm-formation. Microorganisms 9(11), 2274 (2021).
Mandell, J. B. et al. Elimination of antibiotic resistant surgical implant biofilms using an engineered cationic amphipathic peptide WLBU2. Sci. Rep. 7(1), 18098 (2017).
Humphries, R., Bobenchik, A. M., Hindler, J. A. & Schuetz, A. N. Overview of changes to the clinical and laboratory standards institute performance standards for antimicrobial susceptibility testing, M100, 31st edition. J. Clin. Microbiol. 59(12), e0021321 (2021).
Funding
Dr. Kenneth Urish is supported in part by the Orthopaedic Research and Education Fund (OREF) New Investigator Award. This research is additionally supported by NIH/NIAMSD (RO3AR077602).
Author information
Authors and Affiliations
Contributions
J.B.M and K.L.U. conceived and designed the experiments, J.B.M., C.G., D.M.P., and A.J.C. performed the experiments. J.B.M., C.G., and K.M.B. analyzed the data. K.M.B. and D.M. contributed reagents/materials/analysis tools. J.B.M., K.M.B., C.G, and K.L.U. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mandell, J.B., Gish, C., Cappellini, A.J. et al. Methicillin resistant Staphylococcus aureus mazEF expression promotes infections by influencing cellular growth, antibiotic sensitivity, and formation of biofilms. Sci Rep 14, 21269 (2024). https://doi.org/10.1038/s41598-024-70829-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70829-1
- Springer Nature Limited