Abstract
Despite low incidence, neuroblastoma, an immunologically cold tumor, is the most common extracranial solid neoplasm in pediatrics. In relapsed/refractory cases, the benefits of autologous hematopoietic stem cell transplantation (auto-HSCT) and other therapies are limited. Natural killer (NK) cells apply cytotoxicity against tumor cells independently of antigen-presenting cells and the adaptive immune system. The primary endpoint of this trial was to assess the safety of the injection of allogenic, ex vivo-expanded and primed NK cells in relapsed/refractory neuroblastoma patients after auto-HSCT. The secondary endpoint included the efficacy of this intervention in controlling tumors. NK cells were isolated and primed ex vivo (by adding interleukin [IL]-2, IL-15, and IL-21) in a GMP-compliant CliniMACS system and administered to four patients with relapsed/refractory MYCN-positive neuroblastoma. NK cell injections (1 and 5 × 107 cells/kg in the first and second injections, respectively) were safe, and no acute or sub-acute adverse events were observed. During the follow-up period, one complete response (CR) and one partial response (PR) were observed, while two cases exhibited progressive disease (PD). In follow-up evaluations, two died due to disease progression, including the case with a PR. The patient with CR had regular growth at the 31-month follow-up, and another patient with PD is still alive and receiving chemotherapies 20 months after therapy. This therapy is an appealing and feasible approach for managing refractory neuroblastomas post-HSCT. Further studies are needed to explore its efficacy with higher doses and more frequent administrations for high-risk neuroblastomas and other immunologically cold tumors.
Trial registration number: irct.behdasht.gov.ir (Iranian Registry of Clinical Trials, No. IRCT20201202049568N1).
Similar content being viewed by others
Introduction
As the most encountered extracranial solid malignancies in childhood1, neuroblastomas comprise a heterogeneous group of tumors with variable clinicopathological and prognostic features2. Despite their rarity, with an incidence of 10.2 cases per million children younger than 15 years of age3, these neural crest-originated tumors are among the main cause of cancer-related mortalities during childhood3. The prognosis of patients with neuroblastoma varies considerably and depends on age at the time of diagnosis, the presence of high-risk genetic aberrations, tumor size, lymph node involvement, and distant metastases. Accordingly, observation and close monitoring may be sufficient in certain scenarios2. However, approximately 50% of the diagnoses were categorized as high-risk at the time of diagnosis. While the 5-year overall survival (OS) of low- and intermediate-risk disease has reached over 90%, the tide turns for high-risk and relapsed/refractory disease4,5. As a result of the establishment of myeloablative therapy and autologous hematopoietic stem cell transplantation (auto-HSCT) followed by isotretinoin treatment for residual disease, the five-year OS of such patients has risen to more than 50%4,6. However, it is estimated that half of the cases that undergo auto-HSCT will suffer a relapse of malignancy, and robust therapeutic approaches against this scenario are not well-established7.
Neuroblastomas are considered immune-cold tumors; T-cell and natural killer (NK) cell infiltrations within neuroblastomas are considerably lower than those of most other tumors, and the infiltrated cells express higher levels of inhibitory receptors, causing their exhaustion8,9,10. Moreover, the tumor microenvironment (TME) of neuroblastomas is enriched with immunosuppressive myeloid-derived suppressor cells (MDSCs) and cancer-associated fibroblasts8,11. Above these, neuroblastomas have diminished expression of major histocompatibility complex (MHC, also known as human leukocyte antigen [HLA]) class I and NK-activating ligands and generally harbor a low tumor mutational burden (TMB)11,12.
The cardinal impacts of the immune system in defeating neoplastic growth are undeniable; particularly for neuroblastomas, as higher NK cell and T-cell infiltrations and higher MHC-I expression status correlate with a more favorable prognosis11,13. A large body of evidence suggests that NK cells, as innate immune cells, do not rely on signals from antigen-presenting cells (APCs) and instead recognize their target cells based on reduced and/or allogeneic or haploidentical HLA-I expression without the need for prior sensitization. NK cell activation during their maturation is regulated by inhibitory killer immunoglobulin-like receptors (KIRs, a process known as licensing), among other mechanisms14, and their interactions with self-MHC-I prevent further NK cell activation14. Therefore, in recent years, NK cells from different sources and with various expansion/priming methods have been harvested to combat a wide variety of hematological malignancies and solid tumors15,16,17,18,19,20,21,22,23,24,25,26. In fact, the superiority of chimeric antigen receptor (CAR) NK cells over CAR T-cells in exerting comparable anti-tumoral effects with lesser complications has recently been shown18. Moreover, nonmodified NK cells can be harvested for extended periods without losing anti-tumor and memory-like features, making them intriguing tools for feasible and cost-effective cancer immunotherapies17.
Based on these observations, it can be postulated that NK cells can exhibit considerable antitumor activity against neuroblastoma cells. Observations from preclinical27,28 and clinical studies are consistent with the efficacy of ex vivo-primed NK cells in treating neuroblastomas29,30,31. In addition, NK cells are integral mediators of antibody-dependent cellular cytotoxicity (ADCC) and, as a result, putatively enhance the efficacy of anti-disialoganglioside (i.e., anti-GD2) therapies32,33. The impact of NK cell therapy alone on the fate of post-auto-HSCT relapsed neuroblastomas has not yet been addressed. Therefore, this study was designed to delineate the safety and efficacy of allogeneic NK cell transfer in the management of relapsed neuroblastomas.
Results
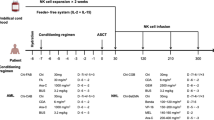
NK cells were effectively separated from the peripheral blood of allogeneic donors (Fig. 1). Likewise, ex vivo NK cell expansion and priming procedures were functional (Tables 1 and 2).
Of the five identified patients, four met the eligibility criteria, consented to participate in the trial, and received two doses of allogeneic ex vivo expanded and activated NK cells. The fifth patient was excluded due to the presence of bone marrow involvement at both biopsy sites. The baseline characteristics of the enrolled patients are shown in Table 3.
Overall, the treatment was safe, and no acute (e.g., anaphylaxis or cytokine storm) or subacute (e.g., fever, hemolysis, urticaria, etc.) toxicities were observed. All enrolled patients received two doses of allogeneic NK cells (total dose of 6 × 107 cells/kg). The efficacy of this treatment was modest; one patient exhibited CR, and another patient had PR during the F/U period (Tables 3 and 4).
The first patient was a four-year-old boy who presented with new bone metastases 11 months after a successful auto-HSCT. The patient received NK cell therapy one month after the diagnosis of new metastases. In the two-month F/U evaluations, he exhibited signs of progressive disease (PD), but at the three-month F/U, a considerable reduction in the burden of 131I-MIBG-avid lesions was noted. The MIBG scans of this patient are depicted in Fig. 2. This PR lasted nine months; however, one year after therapy, the patient presented with new bone lesions. His parents refused to receive any further treatment, and 15 months after NK cell therapy, the patient died due to PD.
Partial response of the first case to NK cell therapy. (A, H) A decrease in the uptake of the right paravertebral lesion (at the level of T9–T10) is evident about four months after NK cell therapy (solid white arrows). (B, G) The diffuse uptake by bone is decreased four months after receiving NK cells (dotted white arrows). (B–D, G) MIBG uptake by a suspicious lymph node in the left paracaval region is dampened (red arrows). (E, F) A decrease in the general MIBG uptake within the torso can be seen.
The second patient, a 5-year-old girl, underwent auto-HSCT two years after the diagnosis of neuroblastoma and, after observing no response to this therapy, received allogeneic NK cells five months later. After NK cell therapy, despite an initial progression in bone metastases, she showed some degree of regression in 4-month scans, and her disease remained stable in 7-month scans. Nevertheless, despite receiving no anti-neuroblastoma therapies except isotretinoin, her 131I-MIBG scans demonstrated resolution of bone and soft tissue metastases 13 months after treatment with NK cells, suggestive of CR. Accordingly, three months after receiving NK cells, she gained weight and reached developmental landmarks in a regular manner in subsequent F/Us.
In the third patient, despite the observation of some degree of response in bone metastases, new 131I-MIBG-avid soft-tissue lesions appeared in the F/U evaluations, suggesting PD. However, his three- and five-month Curie scores showed a reduction of more than 50%. The patient subsequently started receiving conventional chemotherapies five months after NK cell injection. He was alive at the latest F/U (20 months after NK cell injections) and received conventional chemotherapies against neuroblastoma.
The last case exhibited prominent signs of progressive disease in subsequent evaluations after NK cell injection. Accordingly, he was admitted to the oncology ward several times to receive conventional chemotherapy and to manage the associated complications. Approximately seven months after therapy, he presented with an episode of neutropenic fever and died of this complication.
Notably, none of the patients presented with bone marrow metastases after NK cell therapy. The safety profile of our NK cell therapy was acceptable; none of the enrolled cases were afflicted with acute or chronic graft-versus-host disease (GVHD), and excluding the last case, the other three did not present with infectious complications or reactivation of viral infections. The second patient had mild, manageable anemia and thrombocytopenia, which were triggered by the conditioning regimen before the transfusion of NK cells.
Discussion
As briefly mentioned, NK cells are the main effector components of the innate immune system that exert antitumor and antiviral responses directly by inducing apoptosis through Fas signaling and secreting lytic granules containing perforin and granzymes and indirectly by secreting a vast number of proinflammatory cytokines (such as TNF-α, IFN-γ, and granulocyte/monocyte colony-stimulating factor [GM-CSF]) and chemokines14,34,35. Of note, NK cells are not dependent on the stimulating signals from APCs14, which, at least in theory, can be of great importance in defeating neuroblastoma cells, owing to their low TMB, neoantigen, and MHC-I expression. In addition, NK cell-derived exosomes and their secreted microRNAs have been demonstrated to alleviate neuroblastoma-induced immunosuppression36.
Although the application of adoptive NK cell transfer in pediatric tumors has not been widely explored, several immune-based therapies (particularly CAR T-cells and immune checkpoint inhibitors) have emerged as promising approaches for treating hematologic malignancies37,38,39. However, CAR T-cell therapies are quite expensive, require meticulous preparation processes, have considerable side effects (namely, cytokine release syndrome), and demonstrate limited efficacy against solid tumors37. Therefore, there is an unmet need for safe, feasible, and effective cancer immune cell therapies, and adoptive NK cell transfer merits further investigation.
In 1985, Rosenberg et al. demonstrated the relative efficacy of the combined administration of interleukin (IL)-2 and autologous lymphokine-activated killer (LAK) cells in controlling the progression of metastatic cancers40,41. Afterward, in 2002, Ruggeri et al. reported that KIR-mismatched NK cells from HSCT donors exhibited graft-versus-leukemia effects and, unlike T-cells, did not induce GVHD42. This report establishes the rationale for allogeneic KIR-mismatched NK cell therapy in the clinical setting.
However, despite the promising outcomes of adoptive NK cell transfer strategies in managing hematologic malignancies, their activity against solid tumors faces several hurdles. The neoplastic cells and TME of most solid tumors harbor considerable degrees of heterogeneity43,44, which can negatively affect immune cell functions. In addition, their infiltration into tumoral tissues is suboptimal, a challenge that has yet to be encountered44. The immunosuppressive characteristics of the TME (e.g., accumulation of regulatory T-cells, immunosuppressive cytokines, and hypoxia) are other factors that can critically compromise the antitumor abilities of immune cells44. Additionally, traditional approaches to transferring NK cells do not yield long-lasting NK cell activity in vivo.
Hence, unprecedented progress has ensued in their ex vivo expansion and activation and characterization of their cardinal regulators (including KIRs). For instance, an in vitro investigation exhibited that KIR-incompatible allogeneic NK cells are superior in exerting anti-tumor functions against renal cell carcinoma and melanoma cells than autologous NK cells45. In fact, KIR genes exhibit profound variations in terms of copy numbers and allelic pleomorphisms46. Accordingly, the KIR genotype can simply be categorized as A or B, in which the A haplotype mainly contains inhibitory KIRs, while the B haplotype contains several activating KIRs46. Intriguingly, several investigations have demonstrated that KIR haplotypes predict the prognosis and the conversion of MDS to AML47; the incidence of leukemia48 and solid tumors49; the prognosis of classical Hodgkin’s lymphoma50; the prognosis and response to targeted therapies in colorectal cancer51,52; and the response of high-risk NB to auto-HSCT53. Moreover, higher frequencies of inhibitory KIRs have been associated with an increased risk of the development of NBs54. Subsequent trials after the Ruggeri et al. study42 demonstrated the efficacy of haploidentical and donor-recipient KIR-mismatched NK-cells treatment along with IL-2 in the resolution of AML55,56. Interestingly, KIR genotyping of bone marrow donors is proposed to be effective in promoting the prognosis of patients with AML who received reduced-intensity conditioning before transplantation, regardless of HLA typing57. It should also be noted that although most of these reports have implicated better outcomes with the presence of activating KIRs, the tide turns in the context of cancer immunotherapies, i.e., inhibitory KIRs have been associated with better responses to such therapies. For instance, a recent investigation on KIR/KIR-ligand genotyping of NB patients who had received anti-GD2 therapies determined that the presence of inhibitory KIR2DL2 and KIR3DL1 and their ligands (HLA-C1 and HLA-Bw4, respectively) significantly improves the event-free survival (EFS) and OS58.
One of the more studied and promising approaches to increase the efficacy and stemness of adoptive NK cell therapies is priming them with cytokines and growth factors. Pre-clinical and clinical experiments have shown that the addition of IL-2, IL-15, IL-18, IL-21, or IL-27 to the culture media of NK cells can promote their cytotoxic and cytokine-producing capacities and induce a memory-like phenotype, and infusion of IL-2 following NK cell transfer can enhance their proliferation and engraftment in vivo19. Accordingly, in 2004 Ishikawa et al.59 attempted to co-culture autologous, patient-derived NK cells with irradiated human feeder cell line (HFWT) in RHAM-alpha medium and IL-2. They subsequently administered these cells along with low-dose IFN-β by intravenous with or without focal injections to patients with recurrent malignant gliomas, and an acceptable efficacy and safety profile was observed59. However, transfer of autologous, ex vivo activated NK cells did not show an acceptable efficacy in progressive stage IV melanoma or renal cell cancer60 and unresectable, locally advanced, and/or metastatic gastrointestinal cancers61, which was attributed to a lack of activation in the peripheral blood60.
Given the importance of KIR-HLA interactions in determining the activation or inhibition of NK cells and the GvL phenomenon, subsequent trials have aimed to investigate the safety and efficacy of allogeneic NK cells. For instance, a trial on relapsed/refractory non-Hodgkin lymphomas and multiple myeloma cases used ex vivo expanded allogeneic NK cells with nicotinamide and IL-15 and injected them with low-dose IL-2 and rituximab or elotuzumab to enhance their in vivo proliferation and ADCC. Expectedly, this adoptive NK cell transfer exhibited promising efficacies as well, given the advanced status of the disease in enrolled cases62.
Reports on the efficacy of adoptive NK cell therapy for pediatric solid malignancies are scarce22, and in the case of neuroblastoma, most studies have combined NK cell transfer with anti-GD2 therapies. However, adoptive NK cell transfer approaches have yielded promising outcomes in pediatric bone and soft tissue sarcomas, which are immunologically cold, similar to neuroblastomas20,37.
Much effort has been made to enhance the prognosis of patients with high-risk neuroblastomas, and cancer immunotherapies have shown promising outcomes in this venue. Monoclonal antibodies (mAbs) against GD2 (such as dinutuximab), along with cytokine therapies (including IL-2), can improve survival outcomes63,64 by priming NK cell- and neutrophil-mediated ADCC and direct and complement-mediated cytotoxicity2. For instance, in those with newly diagnosed neuroblastoma, the addition of non-primed haploidentical NK cells (4.1–113.98 × 106 CD56+ cells/kg) to auto-HSCT, hu14.18K322A (an anti-GD2 mAb), GM-CSF, and IL-2 combination therapy (as consolidation therapy) appeared tolerable and effective and did not induce significant toxicity23. However, the phase II trial of this study did not observe any added benefits from NK cell transfers, which was attributed to the lack of ex vivo activation and transient engraftment21,23.
Focusing on more advanced stages of the disease, early trials on recurrent/refractory neuroblastoma have shown the safety and relative efficacy of haploidentical NK cell therapy (with doses of < 1 × 106 to 59.5 × 106 CD3−CD56+ cells/kg) combined with anti-GD2 mAbs25,26, IL-2, conventional chemotherapies25, with response rates of 61.5%25 and 29%25,26. However, anti-GD2 therapies are expensive and not widely available65. Putting anti-GD2 mAbs aside, Choi et al.24 enrolled seven patients with relapse/progression of neuroblastoma after auto-HSCT to receive haploidentical NK cells from their parents. The patients received a dose of 3 × 107/kg of ex vivo expanded NK cells in three doses, along with IL-2. Acute (7/7) and chronic (5/7) GVHD and cytomegalovirus (7/7), BK virus (7/7), and Epstein-Barr virus reactivation were common complications after NK cell transfer, and of note, CD16+CD56+CD3– comprised the preponderance of lymphocytes until one-month post-transplantation24. One patient died due to infectious complications, two showed CR, and the other four cases exhibited SD at the three-month F/U, implicating the promising outcomes of haploidentical NK cell and IL-2 therapy. At the end of F/Us, one patient remained alive (after salvage therapy), whereas the other five died due to disease progression24.
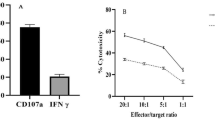
NK cell expansion, activation, and injection are indeed feasible and cost-effective methods of cancer immunotherapy. We and others have previously shown the safety, efficacy, and feasibility of allogeneic NK cell transfer against solid tumors in experimental66,67,68 and clinical69 settings. As discussed above, there are several approaches for priming NK cells ex vivo and in vitro. Preclinical and clinical experiments have shown that the addition of IL-2, IL-15, IL-18, and IL-21 to the culture medium of NK cells promotes their cytotoxic and cytokine-producing capacities and induces a memory-like phenotype, and infusion of IL-2 following NK cell transfer can enhance their proliferation and engraftment in vivo19,59. In our study, we used a combination of IL-2, IL-15, and IL-21, as they have been shown to promote the ex vivo expansion of NK cells more effectively70. These NK cells exhibit acceptable cytokine release and cytolytic activity in vitro. We also utilized a low-intensity conditioning regimen and applied a lower dose of NK cells than in previous studies. In fact, these might be the reasons for the absence of adverse reactions and complications (namely, GVHD and cytokine release syndrome) in our patients. Only one patient exhibited serious side effects (neutropenic fever), and notably, we could not reliably attribute it to NK cell transfer.
While the sample size of our trial was small, and robust conclusions could not be drawn, NK cell therapy alone was modestly effective against recurrent neuroblastomas after auto-HSCT. One patient achieved CR (which lasted for 18 months), and the other achieved PR which lasted for nine months. Two patients (i.e., those with CR and PD in a soft tissue lesion) were alive in 26-month and 15-month F/Us, respectively. Of note, the former exhibited normal growth and functional status. Therefore, considering its favorable safety profile, allogeneic NK cell transfer is a promising therapy for patients with neuroblastoma, even as neoadjuvant therapy for high-risk patients.
This study has several limitations. We did not assess the efficacy of NK cell engraftment, the composition of peripheral blood lymphocytes and other immune cells, or the infiltration rate of transplanted cells into tumoral tissues following injections. Likewise, the cytotoxicity and cytokine release capacities of NK cells were not investigated in F/U evaluations. Finally, considering the small sample size of this study, robust conclusions could not be drawn reliably.
In conclusion, we report the results of a pilot trial on the administration of allogeneic ex vivo expanded NK cells in patients with relapsed neuroblastoma after auto-HSCT. The treatment was safe, feasible, and cost-effective (compared to CAR T-cell and anti-GD2 therapies) and, considering the high-risk nature of the disease, showed a relatively acceptable efficacy in controlling disease progression. Further studies with larger enrolled cases, higher doses of NK cells, and more frequent injections are warranted to evaluate the efficacy of this therapy in the adjuvant (after the failure of or in combination with auto-HSCT) and even neoadjuvant settings for high-risk cases and to characterize the intratumoral infiltration and cytotoxicity of allogeneic NK cells after transfer.
Materials and methods
Study design and patient selection
We conducted an open-label, nonrandomized phase I trial to assess the safety and efficacy of allogeneic NK cell injection in pediatric patients (aged between 2 and 15 years) with relapsed/refractory neuroblastomas after auto-HSCT. All patients without evidence of bone marrow metastases who had received an auto-HSCT in our center between February 2020 and June 2021 and had evidence of relapsed/refractory disease in the subsequent follow-up (F/U) studies were evaluated for enrollment in this trial, according to the inclusion and exclusion criteria presented in Supplementary Table S1 online. As neuroblastoma is a rare pediatric cancer, we did not consider randomization, blinding, or the introduction of a control arm. Similarly, statistical calculations of sample size were not applied in this study.
Written informed consent was obtained from peripheral blood donors and each patient’s parents/legal guardians after a detailed clarification of the experimental nature of the trial and the anonymity of the enrolled individuals. This trial was conducted following the guidelines of the Declaration of Helsinki and was approved by the ethics committee of the Tehran University of Medical Sciences (ethics registration code, IR.TUMS.MEDICINE.REC.1399.817). The findings of this trial are described according to the Consolidated Standards of Reporting Trials (CONSORT) recommendations.
NK cell isolation
NK cell separation was conducted using a good manufacturing practice (GMP)-compliant closed system (CliniMACS Prodigy, Miltenyi Biotec, Germany) designed for clinical applications. Apheresis (10–15 L, using the Spectra Optia Apheresis System, Terumo Blood and Cell Technologies) was performed on eligible healthy donors. Approximately 80–120 cm3 of blood was taken, which was then transferred to transfer bags (Baxter AG, Switzerland). After dilution with PBS/EDTA buffer and 0.5% human albumin serum, the solutions were centrifuged (300 × g for 15 min at room temperature) to isolate peripheral blood mononuclear cells (PBMCs). The buffy coat containing PBMCs was harvested and resuspended in EDTA/PBS and 0.5% human albumin and incubated with CD3 (1 vial for a total of 40 × 109 nucleated cells) and CD56 (1 vial for a total of 40 × 109 nucleated cells) microbeads for 30 min each at room temperature to deplete T-cells and enrich NK cells, respectively, using CliniMACS Tubing Set LS (CliniMACS Prodigy, Miltenyi Biotec, Germany).
NK cell viability, cytokine release, and cytolytic assays
To assess the viability of the isolated and cultured NK cells, we combined 20 µL of the cell suspension with 20 µL of 0.4% trypan blue. The resulting suspension was read using a Neubauer improved cell counting chamber according to established methods.
The release of tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ) was assessed by culturing NK cells in a 96-well enzyme-linked immunosorbent assay (ELISA) plate (10,000 per well) and adding NK MACS GMP medium, 20 ng/mL interleukin (IL)-2, and 50 ng/mL IL-15. After 3 days, cell viability was assessed by trypan blue staining, and the solution was centrifuged. The supernatant was then used for ELISA.
To assess the cytotoxicity of the cultured NK cells, we applied the lactate dehydrogenase assay. NK cells were exposed to tumoral cells (CHLA255 and SK-N-SH human neuroblastoma cell lines, Pasteur Institute of Iran, Tehran, Iran) at different ratios (1:1, 1:2, 1:5, and 1:10; target cells:effector cells), and after two hours of coculture, the solutions were centrifuged (250 × g for 10 min). The supernatant was then passed through 0.22 µm sterile syringe filters, and 100 µL of the filtered solution was transferred to diagnostic plates (Roche Diagnostics, Germany). The reactions were conducted for 30 min in the dark, and the results were read using an ELISA reader with 492 nm filters. The readings were compared with the corresponding values of the background, low, and high control groups.
NK cell culture
The isolated NK cells were initially transferred to T25 flasks containing NK MACS GMP medium (Miltenyi Biotec, Germany) supplemented with 5% human albumin solution (Valley Biomedical, USA), IL-2 (500 IU/mL, Miltenyi Biotec, Germany), IL-15 (140 IU/mL, Miltenyi Biotec, Germany), and IL-21 (1 IU/mL, Miltenyi Biotec, Germany). NK cells were cultured for 48 h at 37 °C and 5% CO2. After 48 h, the cultured cells were transferred to culture bags (VueLife). In compliance with the manufacturer’s guidelines, fresh expansion NK MACS medium, in addition to IL-2 and IL-15, was added to the medium without removing the older medium. The volume of the newly added culture medium and cytokines was determined according to the cell count of each bag70,71. NK cells were cultured for a total duration of 22 ± 3 days.
NK cell administration
After reviewing the inclusion and exclusion criteria, eligible patients were hospitalized and received cyclophosphamide (60 mg/kg, for two hours of continuous intravenous [IV] infusion) on days − 5 and − 4. On day zero, the first dose of NK cells (1 × 107 cells/kg) was infused intravenously for one hour with 200 mL of physiological serum containing 2% human albumin solution (Albumedix, United Kingdom). If the first dose was tolerated, the second escalated dose of NK cells (5 × 107 cells/kg) was administered three weeks later using the same protocol. After each injection, the patients were closely monitored for signs and symptoms of possible allergic and acute reactions (fever, angioedema, hives, etc.), cardiopulmonary decompensation, and infectious complications for one week. Subsequently, routine antifungal and antiviral drugs were prescribed as the preventive strategy for opportunistic infections, and isotretinoin treatment was reinstituted.
NK cells were first isolated by centrifugation of the culture medium at 500 × g for 10 min. Afterward, we assessed their viability, cytotoxicity, and cytokine release, as described previously. In addition, karyotyping, viral, bacterial, and mycoplasma infection control, and bacterial endotoxin release control (using the limulus amebocyte lysate [LAL] test) were performed before infusion.
Outcome measure and endpoints
The primary objective of this trial was to assess the safety and tolerability of allogeneic NK cells in children with relapsed/refractory neuroblastomas following auto-HSCT. Secondary objectives included the assessment of primary and/or metastatic tumor responses to allogeneic NK cells (defined as complete response [CR], partial response [PR], or stable disease [SD]), according to the recommendations of the revised International Neuroblastoma Response Criteria (INRC)72.
One week after the injection of NK cells, the patients were discharged, and their parents were instructed on regular outpatient visits to the pediatric stem cell transplantation clinic at least once a week for the first month after the injection of NK cells. Subsequent F/U visits were planned according to the INRC recommendations. Assessments included computed tomography (CT) scans and bone marrow biopsies (bilateral aspirates and bilateral trephine biopsies) at 3 and 6 months and iodine-131 (131I)-metaiodobenzylguanidine (MIBG) scans at 1, 3, and 6 months after the injection of the last dose of NK cells. More frequent assessments would be performed on the appearance of new signs and/or symptoms of disease or the development of complications.
Expert pediatric radiologists and a nuclear medicine specialist interpreted the CT and 131I-MIBG scans. Two expert pathologists evaluated the bone marrow aspirates and biopsies. A semiquantitative scoring system was adopted to assess 131I-MIBG scans based on the Curies scale73. The response of the primary tumor and bone, bone marrow, and soft tissue metastases to treatment was evaluated by adopting changes in the Curies scores of 131I-MIBG scans, Response Evaluation Criteria in Solid Tumors (RECIST) of CT scans72, and pathological assessment of bone marrow samples74.
Ethics approval and consent to participate
All procedures performed in this study were approved by the appropriate ethics committee and performed in compliance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from the patients’ parents or legal guardians before participation in the study. This study (Phase I study of safety and efficacy of allogeneic natural killer cell therapy in relapsed/refractory neuroblastomas post autologous hematopoietic stem cell transplantation) was approved by the ethics committee of Tehran University of Medical Sciences (Reference Number: IR.TUMS.MEDICINE.REC.1399.817, approved November 21, 2020).
Data availability
Detailed information on patients’ MIBG and CT scan findings is available from the corresponding author upon reasonable request. All other data generated or analyzed during this study are included in this published article and its supplementary information.
Abbreviations
- Auto-HSCT:
-
Autologous stem cell transplantation
- MIBG:
-
Metaiodobenzylguanidine
- NK:
-
Natural killer
- IL:
-
Interleukin
- CR:
-
Complete response
- PR:
-
Partial response
- PD:
-
Progressive disease
- OS:
-
Overall survival
- TME:
-
Tumor microenvironment
- MDSC:
-
Myeloid-derived suppressor cell
- MHC:
-
Major histocompatibility complex
- HLA:
-
Human leukocyte antigen
- TMB:
-
Tumor mutational burden
- APC:
-
Antigen-presenting cell
- KIR:
-
Killer immunoglobulin-like receptor
- ADCC:
-
Antibody-dependent cellular cytotoxicity
- F/U:
-
Follow-up
- CT:
-
Computed tomography
- CONSORT:
-
Consolidated Standards of Reporting Trials
- GMP:
-
Good manufacturing practice
- PBMC:
-
Peripheral blood mononuclear cells
- TNF-α:
-
Tumor necrosis factor-α
- IFN-γ:
-
Interferon-γ
- ELISA:
-
Enzyme-linked immunosorbent assay
- IV:
-
Intravenous
- LAL:
-
Limulus amebocyte lysate
- SD:
-
Stable disease
- INRC:
-
International Neuroblastoma Response Criteria
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- mL:
-
Milliliters
- ng:
-
Nanogram
- CEM:
-
Carboplatin, etoposide, and melphalan
- Dx:
-
Diagnosis
- LN:
-
Lymph node
- No:
-
Number
- Pt:
-
Patient
- BM:
-
Bone marrow
- BMA/BMB:
-
Bone marrow aspiration and biopsy
- N/A:
-
Not assessed
- GVHD:
-
Graft-versus-host disease
- GM-CSF:
-
Granulocyte/monocyte colony-stimulating factor
- CAR:
-
Chimeric antigen receptor
- LAK:
-
Lymphokine-activated killer
- mAb:
-
Monoclonal antibody
References
Knaul, F. M. et al. Avoidable mortality: The core of the global cancer divide. J. Glob. Oncol. 4, 1–12 (2018).
Qiu, B. & Matthay, K. K. Advancing therapy for neuroblastoma. Nat. Rev. Clin. Oncol. 19(8), 515–533 (2022).
Maris, J. M. Recent advances in neuroblastoma. N. Engl. J. Med. 362(23), 2202–2211 (2010).
Irwin, M. S. et al. Revised neuroblastoma risk classification system: A report from the children’s oncology group. J. Clin. Oncol. 39(29), 3229–3241 (2021).
Pinto, N. et al. Impact of genomic and clinical factors on outcome of children ≥18 months of age with stage 3 neuroblastoma with unfavorable histology and without MYCN amplification: A children’s oncology group (COG) report. Clin. Cancer Res. 29(8), 1546–1556 (2023).
Hamidieh, A. A. et al. Comparison of autologous hematopoietic stem cell transplantation with and without metaiodobenzylguanidine (MIBG) in patients with high risk neuroblastoma. Biol. Blood Marrow Transplant. 18(2), S251 (2012).
Shusterman, S. et al. Antitumor activity and tolerability of hu14.18-IL2 with GMCSF and isotretinoin in recurrent or refractory neuroblastoma: A children’s oncology group phase II study. Clin. Cancer Res. 25(20), 6044–6051 (2019).
Costa, A. et al. Single-cell transcriptomics reveals shared immunosuppressive landscapes of mouse and human neuroblastoma. J. Immunother. Cancer 10(8), e004807 (2022).
Louault, K., De Clerck, Y. A. & Janoueix-Lerosey, I. The neuroblastoma tumor microenvironment: From an in-depth characterization towards novel therapies. EJC Paediatr. Oncol. 3, 100161 (2024).
Di Matteo, S. et al. Transition to a mesenchymal state in neuroblastoma may be characterized by a high expression of GD2 and by the acquisition of immune escape from NK cells. Front. Immunol. 15, 1382931 (2024).
Wienke, J. et al. The immune landscape of neuroblastoma: Challenges and opportunities for novel therapeutic strategies in pediatric oncology. Eur. J. Cancer 144, 123–150 (2021).
Yang, J. et al. A novel ganglioside-related risk signature can reveal the distinct immune landscape of neuroblastoma and predict the immunotherapeutic response. Front. Immunol. 13, 1061814 (2022).
Melaiu, O. et al. Cellular and gene signatures of tumor-infiltrating dendritic cells and natural-killer cells predict prognosis of neuroblastoma. Nat. Commun. 11(1), 5992 (2020).
Abel, A. M. et al. Natural killer cells: Development, maturation, and clinical utilization. Front. Immunol. 9, 1869 (2018).
Lupo, K. B. et al. synNotch-programmed iPSC-derived NK cells usurp TIGIT and CD73 activities for glioblastoma therapy. Nat. Commun. 15(1), 1909 (2024).
Coënon, L. et al. Generation of non-genetically modified, CAR-like, NK cells. J. Immunother. Cancer 12(7), e009070 (2024).
Allan, D. S. J. et al. Expanded NK cells used for adoptive cell therapy maintain diverse clonality and contain long-lived memory-like NK cell populations. Mol. Ther. Oncolytics 28, 74–87 (2023).
Marin, D. et al. Safety, efficacy and determinants of response of allogeneic CD19-specific CAR-NK cells in CD19(+) B cell tumors: A phase 1/2 trial. Nat. Med. 30(3), 772–784 (2024).
Liu, S. et al. NK cell-based cancer immunotherapy: From basic biology to clinical development. J. Hematol. Oncol. 14(1), 7 (2021).
Thakar, M. S. et al. Phase II trial using haploidentical hematopoietic cell transplantation (HCT) followed by donor natural killer (NK) cell infusion and sirolimus maintenance for patients with high-risk solid tumors. J. Clin. Oncol. 38(15_suppl), e23551–e23551 (2020).
Furman, W. L. et al. Improved outcome in children with newly diagnosed high-risk neuroblastoma treated with chemoimmunotherapy: Updated results of a phase II study using hu14.18K322A. J. Clin. Oncol. 40(4), 335–344 (2022).
Kanold, J. et al. NK cell immunotherapy for high-risk neuroblastoma relapse after haploidentical HSCT. Pediatr. Blood Cancer 59(4), 739–742 (2012).
Talleur, A. C. et al. Consolidation therapy for newly diagnosed pediatric patients with high-risk neuroblastoma using Busulfan/Melphalan, autologous hematopoietic cell transplantation, anti-GD2 antibody, granulocyte-macrophage colony-stimulating factor, interleukin-2, and haploidentical natural killer cells. Biol. Blood Marrow Transplant. 23(11), 1910–1917 (2017).
Choi, Y. B. et al. Safety and immune cell kinetics after donor natural killer cell infusion following haploidentical stem cell transplantation in children with recurrent neuroblastoma. PLoS One 14(12), e0225998 (2019).
Federico, S. M. et al. A pilot trial of humanized anti-GD2 monoclonal antibody (hu14.18K322A) with chemotherapy and natural killer cells in children with recurrent/refractory neuroblastoma. Clin. Cancer Res. 23(21), 6441–6449 (2017).
Modak, S. et al. Adoptive immunotherapy with haploidentical natural killer cells and Anti-GD2 monoclonal antibody m3F8 for resistant neuroblastoma: Results of a phase I study. Oncoimmunology 7(8), e1461305 (2018).
Shoae-Hassani, A. et al. NK cell-derived exosomes from NK cells previously exposed to neuroblastoma cells augment the antitumor activity of cytokine-activated NK cells. J. Immunother. 40(7), 265–276 (2017).
Lode, H. N. et al. Natural killer cell-mediated eradication of neuroblastoma metastases to bone marrow by targeted interleukin-2 therapy. Blood 91(5), 1706–1715 (1998).
Tarek, N. et al. Unlicensed NK cells target neuroblastoma following anti-GD2 antibody treatment. J. Clin. Invest. 122(9), 3260–3270 (2012).
Liu, Y. et al. Growth and activation of natural killer cells ex vivo from children with neuroblastoma for adoptive cell therapy. Clin. Cancer Res. 19(8), 2132–2143 (2013).
Kloess, S. et al. IL-2-activated haploidentical NK cells restore NKG2D-mediated NK-cell cytotoxicity in neuroblastoma patients by scavenging of plasma MICA. Eur. J. Immunol. 40(11), 3255–3267 (2010).
Anderson, J., Majzner, R. G. & Sondel, P. M. Immunotherapy of neuroblastoma: facts and hopes. Clin. Cancer Res. 28(15), 3196–3206 (2022).
Nguyen, R. et al. Anti-GD2 antibodies conjugated to IL15 and IL21 mediate potent antitumor cytotoxicity against neuroblastoma. Clin. Cancer Res. 28(17), 3785–3796 (2022).
Walzer, T. et al. Natural-killer cells and dendritic cells: “l’union fait la force”. Blood 106(7), 2252–2258 (2005).
Mahdavi Sharif, P. et al. Importance of TNF-alpha and its alterations in the development of cancers. Cytokine 130, 155066 (2020).
Neviani, P. et al. Natural killer-derived exosomal miR-186 inhibits neuroblastoma growth and immune escape mechanisms. Cancer Res. 79(6), 1151–1164 (2019).
Mahdavi Sharif, P. et al. Chapter 4-tumor immunology. In Clinical Immunology (ed. Rezaei, N.) 245–452 (Academic Press, 2023).
Lutskovich, D., Meleshko, A. & Katsin, M. State of the art and perspectives of chimeric antigen receptor T cells cell therapy for neuroblastoma. Cytotherapy (2024).
Bergaggio, E. et al. ALK inhibitors increase ALK expression and sensitize neuroblastoma cells to ALK.CAR-T cells. Cancer Cell 41(12), 2100–2116 (2023).
Rosenberg, S. A. et al. A progress report on the treatment of 157 patients with advanced cancer using lymphokine-activated killer cells and interleukin-2 or high-dose interleukin-2 alone. N. Engl. J. Med. 316(15), 889–897 (1987).
Rosenberg, S. A. et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N. Engl. J. Med. 313(23), 1485–1492 (1985).
Ruggeri, L. et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 295(5562), 2097–2100 (2002).
Punt, C. J., Koopman, M. & Vermeulen, L. From tumour heterogeneity to advances in precision treatment of colorectal cancer. Nat. Rev. Clin. Oncol. 14(4), 235–246 (2017).
Nayyar, G., Chu, Y. & Cairo, M. S. Overcoming resistance to natural killer cell based immunotherapies for solid tumors. Front. Oncol. 9, 51 (2019).
Igarashi, T. et al. Enhanced cytotoxicity of allogeneic NK cells with killer immunoglobulin-like receptor ligand incompatibility against melanoma and renal cell carcinoma cells. Blood 104(1), 170–177 (2004).
Cisneros, E. et al. Haplotype-based analysis of KIR-gene profiles in a south European population-distribution of standard and variant haplotypes, and identification of novel recombinant structures. Front. Immunol. 11, 440 (2020).
Stringaris, K. et al. KIR gene haplotype: An independent predictor of clinical outcome in MDS patients. Blood 128(24), 2819–2823 (2016).
Verheyden, S., Bernier, M. & Demanet, C. Identification of natural killer cell receptor phenotypes associated with leukemia. Leukemia 18(12), 2002–2007 (2004).
Al Omar, S. et al. Associations between genes for killer immunoglobulin-like receptors and their ligands in patients with solid tumors. Hum. Immunol. 71(10), 976–981 (2010).
La Nasa, G. et al. The favorable role of homozygosity for killer immunoglobulin-like receptor (KIR) A haplotype in patients with advanced-stage classic Hodgkin lymphoma. J. Hematol. Oncol. 9, 26 (2016).
Beksac, K. et al. Impact of “killer immunoglobulin-like receptor /ligand” genotypes on outcome following surgery among patients with colorectal cancer: Activating kirs are associated with long-term disease free survival. PLoS One 10(7), e0132526 (2015).
Manzanares-Martin, B. et al. Improving selection of patients with metastatic colorectal cancer to benefit from cetuximab based on KIR genotypes. J. Immunother. Cancer 9(4), e001705 (2021).
Venstrom, J. M. et al. KIR and HLA genotypes are associated with disease progression and survival following autologous hematopoietic stem cell transplantation for high-risk neuroblastoma. Clin. Cancer Res. 15(23), 7330–7334 (2009).
Keating, S. E. et al. Increased frequencies of the killer immunoglobulin-like receptor genes KIR2DL2 and KIR2DS2 are associated with neuroblastoma. Tissue Antigens 86(3), 172–177 (2015).
Miller, J. S. et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood 105(8), 3051–3057 (2005).
Rubnitz, J. E. et al. NKAML: A pilot study to determine the safety and feasibility of haploidentical natural killer cell transplantation in childhood acute myeloid leukemia. J. Clin. Oncol. 28(6), 955–959 (2010).
Weisdorf, D. et al. KIR B donors improve the outcome for AML patients given reduced intensity conditioning and unrelated donor transplantation. Blood Adv. 4(4), 740–754 (2020).
Erbe, A. K. et al. KIR/KIR-ligand genotypes and clinical outcomes following chemoimmunotherapy in patients with relapsed or refractory neuroblastoma: A report from the Children’s Oncology Group. J. Immunother. Cancer 11(2), e006530 (2023).
Ishikawa, E. et al. Autologous natural killer cell therapy for human recurrent malignant glioma. Anticancer Res. 24(3b), 1861–1871 (2004).
Parkhurst, M. R. et al. Adoptive transfer of autologous natural killer cells leads to high levels of circulating natural killer cells but does not mediate tumor regression. Clin. Cancer Res. 17(19), 6287–6297 (2011).
Sakamoto, N. et al. Phase I clinical trial of autologous NK cell therapy using novel expansion method in patients with advanced digestive cancer. J. Transl. Med. 13, 277 (2015).
Bachanova, V. et al. Results of a phase 1 trial of Gda-201, nicotinamide-expanded allogeneic natural killer cells (NAM-NK) in patients with refractory non-hodgkin lymphoma (NHL) and multiple myeloma (MM). Blood 134(Supplement_1), 777–777 (2019).
Yu, A. L. et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N. Engl. J. Med. 363(14), 1324–1334 (2010).
Ladenstein, R. et al. Interleukin 2 with anti-GD2 antibody ch14.18/CHO (dinutuximab beta) in patients with high-risk neuroblastoma (HR-NBL1/SIOPEN): A multicentre, randomised, phase 3 trial. Lancet Oncol. 19(12), 1617–1629 (2018).
Li, C. et al. Excellent early outcomes of combined chemotherapy with arsenic trioxide for stage 4/M neuroblastoma in children: A multicenter nonrandomized controlled trial. Oncol. Res. 28(7), 791–800 (2021).
Sharifzad, F. et al. HSP70/IL-2 treated NK cells effectively cross the blood brain barrier and target tumor cells in a rat model of induced glioblastoma multiforme (GBM). Int. J. Mol. Sci. 21(7), 2263 (2020).
Behfar, M. et al. Adoptive NK-cell transfer as a potential treatment paradigm for Wilms tumor: A preclinical study. Pediatr. Blood Cancer 69(8), e29676 (2022).
Hamidieh, A. A. et al. Natural killer cells treated with CD11b expressing subpopulation of exosomes show highly activated phenotype against neuroblastoma: A future prospect for the treatment of high-risk neuroblastoma. Biol. Blood Marrow Transplant. 24(3), S474 (2018).
Asl, N. S. et al. Intra-lesion injection of activated natural killer (NK) cells in recurrent malignant brain tumors. Int. Immunopharmacol. 120, 110345 (2023).
Oberschmidt, O. et al. Development of automated separation, expansion, and quality control protocols for clinical-scale manufacturing of primary human NK cells and alpharetroviral chimeric antigen receptor engineering. Hum. Gene Ther. Methods 30(3), 102–120 (2019).
Heinze, A. et al. The synergistic use of IL-15 and IL-21 for the generation of NK cells from CD3/CD19-depleted grafts improves their ex vivo expansion and cytotoxic potential against neuroblastoma: Perspective for optimized immunotherapy post haploidentical stem cell transplantation. Front. Immunol. 10, 2816 (2019).
Park, J. R. et al. Revisions to the International Neuroblastoma Response Criteria: A consensus statement from the national cancer institute clinical trials planning meeting. J. Clin. Oncol. 35(22), 2580–2587 (2017).
Sharp, S. E. et al. MIBG in neuroblastoma diagnostic imaging and therapy. Radiographics 36(1), 258–278 (2016).
Burchill, S. A. et al. Recommendations for the standardization of bone marrow disease assessment and reporting in children with neuroblastoma on behalf of the International Neuroblastoma Response Criteria Bone Marrow Working Group. Cancer 123(7), 1095–1105 (2017).
Funding
This study is partially funded by the Tehran University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
R.M. conceptualized the trial, designed the study protocol, and performed the functional assays of NK cells. P.M.S. gathered patient data, interpreted the data, drafted the manuscript, and designed the figures. M.B. conceptualized the trial and performed the follow-up visits as a transplantation specialist. S.S. obtained and cultured NK cells. A.S. obtained and cultured NK cells. L.J. partially contributed to functional assays of NK cells. A.K. partially contributed to NK cell isolation. Z.N. administered NK cells to the enrolled patients and was responsible for administering conditioning regimens. A.A.H. conceptualized the study, designed the study protocol, performed F/U visits (as the head of transplantation specialists), critically appraised the draft, and supervised the project. All the authors have read and approved the final manuscript. The parents or legal guardians of the included cases consented to the participation of their children in this trial and the anonymous publication of their data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mohseni, R., Mahdavi Sharif, P., Behfar, M. et al. Phase I study of safety and efficacy of allogeneic natural killer cell therapy in relapsed/refractory neuroblastomas post autologous hematopoietic stem cell transplantation. Sci Rep 14, 20971 (2024). https://doi.org/10.1038/s41598-024-70958-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70958-7
- Springer Nature Limited