Abstract
To compare the clinical efficacy of interlaminar endoscopic surgical system delta (iLESSYS-Delta) discectomy with that of classical fenestration discectomy for treating lumbar disc herniation. Patients who underwent iLESSYS-Delta or fenestration discectomy were enrolled in this study. Baseline information and clinical indicators were collected. The baseline data were matched using propensity score matching. Fifty-two patients were in each group. In the iLESSYS-Delta cohort, the volume of intraoperative bleeding was 18.17 ± 4.20 ml, the length of postoperative hospital stay was 4.16 ± 2.29 days, and the length of postoperative off-bed activity was 1.58 ± 0.88 days. In contrast, in the fenestration group, the volume of intraoperative bleeding was 32.50 ± 17.13 ml, the length of postoperative hospital stay was 6.66 ± 2.44 days, and the length of postoperative off-bed activity was 3.18 ± 1.28 days. The difference between the two groups was statistically significant (P < 0.05). The operation time was 88.90 ± 19.14 min in the iLESSYS-Delta group and 67.63 ± 19.32 min in the fenestration group, and the difference between the two groups was statistically significant (P < 0.05). Regarding the pain visual analogue scale scores at 24, 48, and 72 h after surgery, patients in the iLESSYS-Delta group had less pain than did those in the fenestration group (P < 0.05). The Oswestry disability indices of postoperative patients in both groups significantly improved at 3 months after surgery and at the last follow-up (P < 0.05); however, there was no statistically significant difference in the postoperative ODI scores between the two surgery groups (P > 0.05). The two groups showed no significant differences in clinical effects, postoperative recurrence rates, or perioperative complications. iLESSYS-Delta can cause less intraoperative bleeding and faster recovery than fenestration discectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Lumbar disc herniation (LDH) is one of the leading causes of lower back and leg pain. Recent studies have shown that LDH often begins with intervertebral disc degeneration1. The increasing prevalence of LDH has become a serious public health problem. It severely impacts patients’ life and work and burdens society2.
Discectomy is commonly performed to treat LDH if conservative treatment fails3. Conventional open fenestration discectomy often requires paraspinal muscle stripping and bone resection. Destruction of the dorsal structure of the spinal column leads to complications such as chronic back pain and spinal instability4,5,6. In recent years, enhanced recovery after surgery (ERAS) or fast-track surgery (FTS), which aims to reduce patients’ stress response and the incidence of complications, has played a positive role in patient recovery7,8. Minimally invasive surgeries cause less trauma, a lower stress response, and fewer complications than open surgeries9. As a minimally invasive surgery, percutaneous endoscopic lumbar discectomy is widely used to treat LDH, and its efficacy is promising10,11. The interlaminar endoscopic surgical system delta (iLESSYS-Delta), developed by Joimax, is an endoscopic system that achieves fenestration similar to that of conventional surgery through a minimally invasive method. Moreover, this approach has the advantages of requiring a large surgical exploratory area and adequate decompression compared with other endoscopic methods12,13. Owing to the larger working channel (6 mm in diameter), better resection of the bony structure and soft tissues can be performed, which makes this approach suitable for a wide range of indications in contrast to other endoscopic spinal surgery systems14. As a minimal surgical system was initially invented to treat lumbar spinal stenosis, studies on its application in the treatment of LDH are rare. A retrospective study published in 2021 suggested that the use of the iLESSYS-Delta could achieve good outcomes in treating extruded herniation of the lumbar disc15. However, further studies are needed to determine whether the iLESSYS-Delta has advantages over traditional open fenestration techniques for the treatment of LDH.
This study aimed to compare the clinical effects of iLESSYS-Delta and open fenestration discectomy for the treatment of LDH.
Materials and methods
Study design and PICO points
Study design: This was a retrospective study.
Patient: A total of 201 patients were included in this study.
Intervention: Patients who underwent discectomy with iLESSYS-Delta at the Qilu Hospital of Shandong University between January 2019 and March 2021 were included.
Comparison: Patients who underwent discectomy with open fenestration at the Qilu Hospital of Shandong University between January 2019 and March 2021 were included.
Outcome: Hospitalization cost, operative time, postoperative hospital stay (days), intraoperative bleeding (ml), postoperative activity time, VAS scale, ODI scale.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) had classic symptoms or signs caused by compression of the nerve root, such as low back pain and radicular pain in the leg, and (2) Imaging on CT and MRI demonstrated a herniated or prolapsed disc with signs of significant compression of the dural sac and nerve roots. (3) Conservative treatment for more than 3 months without symptomatic relief or recurrence. (4) Age ≥ 18 years, sign the informed consent and accept regular follow-up.
The exclusion criteria were as follows: (1) did not match the clinical symptoms according to radiography; (2) had spondylolisthesis, spinal instability, lumbar infection, or malignant tumour; (3) were unable to undergo surgery for a dire medical situation; (4) had a mental illness; (5) had previous lumbar surgery; (6) had internal fixation or interbody fusion; (7) had discectomy involving both the iLESSYS-Delta and fenestration; and (8) had incomplete medical records.
All eligible patients met surgical indications and underwent L4/5 or L5/S1 discectomy under iLESSYS-Delta or open fenestration. All patients were treated and managed by the same team. This study was approved by the ethics committee of Qilu Hospital. Informed consent was obtained from all participants.
Surgical technique
iLESSYS-delta approach
After general anaesthesia, the patient was placed in a prone position, and the abdomen was removed. The C-arm was used to locate the desired level. A guide needle was inserted at the medial inferior edge of the upper lamina with fluoroscopic assistance. A 1 cm long longitudinal skin incision was made at the guide needle. Sequential dilators were used to expand the surrounding tissue until it reached the bony structure. The dilators were again observed via fluoroscopy at the desired level. The working channel was placed along the dilators, and the dilators were withdrawn. The irrigation systems were connected. Soft tissues were removed using bipolar radiofrequency. To expose the nerve root and thecal sac, the partial articular joint, edge of the lamina, and adequate ligamentum flavum were removed using an endo-Kerrison punch. A retractor was used to protect and pull nerve roots medially. The herniated intervertebral disc and partial degenerative nucleus pulposus were removed. Complete decompression was determined based on the mobility of the nerve roots. Careful haemostasis was achieved, and the incision was sutured, disinfected, and bandaged.
Open Fenestration approach
This procedure was performed under general anaesthesia with tracheal incubation. The patient was placed in the prone position, and the abdomen was suspended. A posterior medial incision was made after disinfection and spreading of the towels. The unilateral paraspinal muscle was removed to expose the cephalic and caudal lamina, ligamentum flavum, and zygapophyseal joints. The supraspinous and interspinous ligaments were protected carefully. Fluoroscopy was performed to confirm the desired level. Fenestration was performed by partially resecting the lamina and inferior articular process; the window size was approximately 1.2 cm × 1.5 cm. The ligamentum flavum was then cut using a #15 knife. After nerve exposure, the nerve root was pulled medially by a nerve stripper to reveal the intervertebral disc. The annulus fibrosus was cut using a #15 knife, and the herniated or extruded nucleus pulposus was removed using nucleus pulposus forceps. To ensure complete decompression of the nerve root, mobility and tension had to be checked. After proper haemostasis and rinsing, the incision was sutured layer by layer.
Data collection
A hospital information system was used to collect data regarding the inclusion and exclusion criteria. Follow-up data were collected via telephone or via communication software at the outpatient clinic.
Patient demographic characteristics, including name, sex, age, hospital admission number, contact method, body mass index (BMI), personal history (smoking history and alcohol history), medical history (diabetes, hypertension, and heart disease), surgical segment (L4/5 or L5/S1), Pfirrmann grade, and occurrence of endplate degeneration, were obtained.
To compare these two surgical methods, hospitalization cost (RMB), surgical data including operative time (time from incision to closure), postoperative hospital stay (days), intraoperative bleeding (ml), postoperative activity time, and patient-reported outcomes (PROs), were collected. Postoperative pain was assessed using the pain visual analogue scale (VAS), and the following cut-off points were used in this study: mild pain (1–3), moderate pain (4–6), and severe pain (≥ 7). VAS scores were evaluated at 24, 48, and 72 h. The Oswestry Disability Index (ODI) at three months and one year after surgery was used to assess functional outcomes. The recurrence criteria included the same or adjacent segment, pain relief for at least six months, first-time recurrence, and consistency of the radiographic and clinical examinations.
Propensity score matching (PSM)
Propensity score matching (PSM) refers to the reduction of variability in baseline clinical data between patients in the two surgical groups by screening the delta-scope surgery group and the open-window surgery group so that the screened study subjects are comparable in terms of baseline clinical data. PSM was conducted with the R package Matchit (v4.3.2).
Statistical analysis
The dataset was separated into two groups: the iLESSYS-Delta group (patients who underwent discectomy by the iLESSYS Delta) and the fenestration group (patients who underwent discectomy by open fenestration discectomy). Propensity score matching (PSM) was used to reduce the influence of confounders and the difference between the iLESSYS-Delta and fenestration groups16,17. The R package Matchit was utilized to perform PSM using 1:1 nearest neighbour matching, and the calliper value was 0.02. After PSM, 52 of 102 patients in the iLESSYS-Delta cohort were matched with 52 of 99 patients in the fenestration cohort based on their propensity score. Quantile‒quantile (Q–Q) plots, histograms showing the density of the propensity score distribution, and a Jittered plot were generated to show the wellness of the PSM.
Categorical variables are represented by the frequency and percentage. Continuous variables are represented by the mean and standard deviation when the distribution was normal, and they are represented by the median and interquartile range. For categorical variables, the chi-square test was used if the expectation was greater than or equal to 5 and the total number was no less than 40. Fisher’s exact test was used when the expected value was less than 5. Continuous variables conforming to a normal distribution were tested using an independent sample t test, and nonnormally distributed data were tested using a nonparametric test. The data from the iLESSYS-Delta and fenestration groups, including sex, age, BMI, personal history (history of smoking, history of alcohol consumption), medical history (heart disease, diabetes, hypertension), surgical segment, presence of endplate degeneration, Pfirrmann grading, presence of combined lumbosacral migrating spine, VAS score, ODI score, operative time, intraoperative bleeding, and postoperative activity time, were statistically analysed to evaluate improvements in the baseline data, postoperative symptoms, and function of the patients. P < 0.05 was considered to indicate a statistically significant difference. The remaining statistical analyses were conducted using IBM SPSS V21.0 (IBM Corporation).
Ethics approval and consent to participate
This research protocol was approved by the Institutional Review Board of Qilu Hospital of Shandong University and The First Affiliated Hospital of Jinan University (KYLL-2021(KS)-614). The clinical procedures adhered to the principles of the declaration of Helsinki. Informed consent was obtained from all individual participants included in the study. This study confirming that all experiments were performed in accordance with relevant guidelines and regulations.
Results
We excluded the following patients from the selection process. Finally, 201 patients were enrolled in this study, with 102 and 99 patients in the iLESSYS-Delta and fenestration groups, respectively.
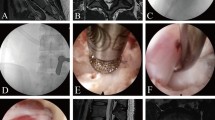
Because the baseline data before matching were significantly different (Table 1), propensity score matching was performed to minimize selection bias. A quantile‒quantile (Q–Q) plot, a histogram showing the density of the propensity score distribution, and a Jittered plot (Fig. 1) showed that the balance of baseline data between the two groups was significantly improved. There was no statistically significant difference between the baseline values of the two matched groups (Table 2).
Propensity score matching. (A) Q‒Q plot comparing the probability distributions of the two surgical groups with regard to covariates. The results show that although the matched point is not precisely on the y = x-line, it significantly improves compared to that before matching. (B) Histogram showing the distribution density of the propensity scores before and after matching the two surgical groups. The propensity scores of the prematch treatment group were significantly greater than those of the control group. After matching, the density distributions of the two groups became similar. (C) Jittered plot showing the matched and nonmatched observations. The distribution of the propensity scores was similar between the matched groups.
A comparison of the postoperative clinical indicators revealed that patients in the iLESSYS-Delta group had less intraoperative bleeding, shorter hospital stays, and shorter postoperative off-bed activity times but longer operation times (P < 0.05). (Table 3).
Detailed hospitalization costs for the iLESSYS-Delta and Fenestration groups are summarized below. Total costs were significantly higher in the Fenestration group than in the iLESSYS-Delta group. Mainly, the cost of surgery, drugs and nursing care were lower in group iLESSYS-Delta compared to group Fenestration. However, the cost of anesthesia for iLESSYS-Delta was higher than that of group Fenestration, probably due to the fact that the duration of surgery for iLESSYS-Delta was longer than that for Fenestration (Table 4).
The postoperative outcomes in the iLESSYS-Delta and fenestration groups were compared (Table 4). Within 24 h after surgery, 29 patients in the iLESSYS-Delta group experienced mild pain, and 22 patients had moderate pain. In the fenestration group, five patients had mild pain, and 32 patients had moderate pain. The difference in the VAS score 24 h after surgery was statistically significant (P < 0.001). Within 48 h after surgery, 41 patients in the iLESSYS-Delta group had no pain, 10 had mild pain, and 1 had moderate pain. In the fenestration group, 25 patients had no pain, 26 had mild pain, and one had moderate pain. The VAS scores of the iLESSYS-Delta group and fenestration group were significantly different at 48 h after surgery (P = 0.01). Within 72 h after surgery, 51 patients in the iLESSYS-Delta group experienced pain relief, and one patient experienced mild pain. In the fenestration group, 46 patients were painless, and six had mild pain. The difference in the VAS scores between the two groups at 72 h postsurgery was statistically significant (P < 0.001).
The preoperative ODI of the iLESSYS-Delta group was 25.23 ± 5.90, whereas that of the fenestration group was 26.00 ± 5.73. Moreover, there was no statistically significant difference between the two groups (P = 0.247). Regarding the short-term efficacy of surgery, within three months after surgery, the ODI of the iLESSYS-Delta group was 1.58 ± 1.69. The ODI of the fenestration group was 2.23 ± 2.72, and the difference between the two surgical groups was not statistically significant (P = 0.351). The last follow-up time was one year after surgery, and the ODI was 2.04 ± 4.98 in the iLESSYS-Delta group. In the fenestration group, the ODI was 3.17 ± 6.75, and the difference between the two groups was not statistically significant (P = 0.704) (Table 5).
Four postoperative complications were assessed and analysed. Deep vein thrombosis was observed in the iLESSYS-Delta and fenestration groups. Incision infection and exudates were found only in the fenestration group. One patient in the iLESSYS-Delta group showed symptoms related to nerve damage that were not observed in the fenestration group (Table 6).
According to the criteria for recurrence, four patients in the iLESSYS-Delta group relapsed, and eight in the fenestration group relapsed. The difference between the two groups was not statistically significant (P = 0.360) (Table 7 for details).
Discussion
Lumbar disc herniation (LDH) is a common degenerative spinal disorder. Conservative treatment is effective and feasible for most patients with LDH. Surgery should be considered if conservative treatment fails18,19. Fenestration discectomy is the classical surgical procedure for LDH and is widely accepted by spine surgeons because of its simplicity, low osteotomy rate, low impact on spinal stability, and validity20. However, with the occurrence and development of ERAS, minimally invasive spine surgery is increasingly being favoured by spine surgeons because of the advantages of less surgical damage and faster recovery after surgery21. Percutaneous endoscopic discectomy is more minimally invasive than open fenestration. The iLESSYS-Delta has advantages over other endoscopic systems. To investigate the optimal procedure for treating LDH, we compared the efficacy of fenestration discectomy with that of iLESSYS-Delta discectomy.
The ODI is an important indicator for evaluating the outcome of lumbar spinal surgery. In this study, we evaluated the efficacy of the two surgical modalities in short-term (3 months postoperatively) and the long-term (1 year postoperatively), respectively. This study showed that both iLESSYS-Delta and fenestration discectomies achieved similar improvements. Compared to fenestration discectomy, the iLESSYS-Delta discectomy did not increase the recurrence rate (P = 0.36). These results suggest that iLESSYS-Delta discectomy is a reliable surgical procedure for treating LDH. However, longer-term efficacy data, recurrence rates, and complications of the two surgical procedures will be the focus of our next study.
Compared to other endoscopic systems, the iLESSYS-Delta has a larger working channel (1 cm in diameter), which supports the use of a larger Kerrison punch, grinding drill, and nucleus pulposus forceps for better decompression. Moreover, this system allows for a wide oscillating range, wide field of view, and more thorough exploration, allowing for the detection of residual prolapsed nucleus pulposus tissue. Under clear illumination, continuous saline irrigation, and a visual field magnification system, fissures in the annulus fibrosus can be detected, and a further reduction in the risk of recurrence can be achieved. Therefore, iLESSYS-Delta discectomy can achieve better decompression of the nerve root than can other endoscopic methods and has an effect similar to that of fenestration.
It has been suggested that mechanical compression of nerve roots without inflammatory stimuli cannot cause pain but leads to changes in sensation and muscle strength only in the area innervated by the nerve root22. Mechanical compression can cause ischaemia of the nerve root, leading to a local inflammatory response. Several studies have shown elevated expression of inflammatory factors in degenerated intervertebral discs, indicating that the inflammatory response is involved in IDD23. Various inflammatory cytokines are known to be involved in the development of disc degeneration. Elevated TNF-α expression has been found in the disc and peripheral blood serum of patients with intervertebral disc degeneration24. IL-1β and IL-6 in the interleukin family can contribute to disc degeneration by causing an imbalance in the metabolism of the extracellular matrix of the nucleus pulposus, which in turn disrupts homeostasis of the intramedullary environment, leading to nucleus pulposus degeneration25. During endoscopic discectomy, in addition to removing degenerated herniated nucleus pulposus tissue, local inflammatory factors can be flushed and diluted by continuous saline irrigation during the procedure, thereby reducing the local inflammatory response and the probability of postoperative back and leg pain.
In addition, the iLESSYS-Delta discectomy has several advantages over fenestration discectomy. First, compared with fenestration, iLESSYS-Delta was associated with less bleeding, earlier postoperative off-beding, and shorter postoperative hospital stays. Second, regarding postoperative pain, the iLESSYS-Delta group experienced less pain at all postoperative time points than did the fenestration group. This may be due to the smaller incision (1 cm) and lesser resection of the paravertebral muscles. In addition, endoscopic discectomy causes less damage to the bony structure, muscles, and ligament complexes; less trauma to the patient; and less bleeding, resulting in less postoperative pain and less postoperative stress, allowing for faster postoperative recovery. Moreover, bipolar radiofrequency allows precise haemostasis of the perineural tissue, resulting in less intraoperative bleeding. Our study showed that the total cost of Fenestration was RMB 3,767 higher than iLESSYS-Delta. Further analysis showed that the Fenestration group had higher surgical and drug costs and nursing costs than the iLESSYS-Delta group, respectively. These outcomes could be logically predicted by more structural damage during surgery and longer hospitalization in the Fenestration group. However, the lack of consistency in cost outcomes between studies makes it difficult to compare cost data between this study and previous studies.
In this study, 8 patients developed complications. Two patients (one with deep vein thrombosis and one with short-term postoperative nerve injury) were included in the iLESSYS-Delta group, and six patients were included in the fenestration group (two with deep vein thrombosis, one with postoperative incisional infection, and three with incisional oozing). Fisher’s exact test showed no significant difference between the two groups (P > 0.05), which may be related to the limited number of patients in the study.
Patients with thrombosis were considered as a result of prolonged postoperative bed rest and low bed mobility in the main patient. This suggests the importance of perioperative education. Short-term postoperative nerve injury was considered to be caused by the inflammatory reaction of the nerve root due to long-term compression of the herniated nerve root, as well as the pulling of the nerve root in order to completely remove the herniated nucleus pulposus during the operation. After postoperative treatment with nerve nutrition, edema elimination and analgesia, the patient's pain improved and muscle strength recovered. Incisional infection and incisional oozing were considered to be related to the patient's obesity and early and excessive postoperative activity.
Although the iLESSYS-Delta discectomy has many advantages over fenestration discectomy, it has several limitations. For example, as a minimally invasive procedure, the extent of visualization is still limited compared with that of traditional open surgery. Moreover, the mean operation time was greater than that of fenestration discectomy because of the smaller incision size and limited operating space. In addition to the above reasons, additional surgical steps required for iLESSYS-Delta discectomy such as cannula installation and device connection also contribute to the longer surgery time. Furthermore, more time is needed to correctly identify anatomical structures, and surgeons need to be familiar with the instruments, which increases the operative time. As well as the need for the operator to operate without tactile sensation, the understanding of three-dimensional anatomy through two-dimensional imaging underneath, and the training cycle for manual dexterity. These are the reasons for the longer learning curve of minimally invasive surgery. Although the procedure had a positive effect on reducing hospital stays and returning to work, good training is still needed for beginners.
By comparing the two procedures in different aspects, the study revealed that the iLESSYS-Delta discectomy could be an optional alternative to fenestration discectomy. This study has several limitations. This was a retrospective study, and the level of evidence in evidence-based medicine was not high enough. In addition, a larger sample and a multicentre project are needed for further validation before conclusions can be drawn that are consistent with a wide range of populations. Propensity score matching inevitably causes the loss of cases during the matching process, and the effect of these samples should not be ignored. In the future, we will recruit larger sample sizes through multicenter studies to further validate the effectiveness of our work with external data. As well as, in the future, we will be able to better select appropriate surgical procedures for our patients through research.
Conclusion
In summary, our study revealed no significant differences in clinical effects, postoperative recurrence rates, or perioperative complications between the iLESSYS-Delta and fenestration groups. However, the iLESSYS-Delta discectomy causes less intraoperative bleeding but has a longer operation time. A minimally invasive approach results in less pain, faster recovery, and a shorter postoperative hospital stay. Therefore, upon achieving proficiency in the learning process, iLESSYS-Delta discectomy can be regarded as a secure substitute for fenestration surgery. This study provides a new theoretical basis for choosing an appropriate surgical approach for the treatment of LDH.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Rodrigues-Pinto, R., Richardson, S. M. & Hoyland, J. A. An understanding of intervertebral disc development, maturation and cell phenotype provides clues to direct cell-based tissue regeneration therapies for disc degeneration. Eur. Spine J. 23, 1803–1814. https://doi.org/10.1007/s00586-014-3305-z (2014).
Zhang, A. S. et al. Lumbar disc herniation: Diagnosis and management. Am. J. Med. 136, 645–651. https://doi.org/10.1016/j.amjmed.2023.03.024 (2023).
Benzakour, T., Igoumenou, V., Mavrogenis, A. F. & Benzakour, A. Current concepts for lumbar disc herniation. Int. Orthop. 43, 841–851. https://doi.org/10.1007/s00264-018-4247-6 (2019).
Li, X. et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Austral. 33, 19–27. https://doi.org/10.1016/j.jocn.2016.01.043 (2016).
Bokov, A. et al. An analysis of reasons for failed back surgery syndrome and partial results after different types of surgical lumbar nerve root decompression. Pain Phys. 14, 545–557 (2011).
Fritsch, E. W., Heisel, J. & Rupp, S. The failed back surgery syndrome: Reasons, intraoperative findings, and long-term results: A report of 182 operative treatments. Spine 21, 626–633. https://doi.org/10.1097/00007632-199603010-00017 (1996).
Ansari, D., Gianotti, L., Schröder, J. & Andersson, R. Fast-track surgery: Procedure-specific aspects and future direction. Langenbeck’s Arch. Surg. 398, 29–37. https://doi.org/10.1007/s00423-012-1006-9 (2013).
Ljungqvist, O., Scott, M. & Fearon, K. C. Enhanced recovery after surgery: A review. JAMA Surg. 152, 292–298. https://doi.org/10.1001/jamasurg.2016.4952 (2017).
Ding, W., Yin, J., Yan, T., Nong, L. & Xu, N. Meta-analysis of percutaneous transforaminal endoscopic discectomy vs. fenestration discectomy in the treatment of lumbar disc herniation. Der Orthopade 47, 574–584. https://doi.org/10.1007/s00132-018-3528-5 (2018).
Kim, M. et al. Evolution of spinal endoscopic surgery. Neurospine 16, 6–14. https://doi.org/10.14245/ns.1836322.161 (2019).
Kim, J. H. et al. Feasibility of full endoscopic spine surgery in patients over the age of 70 years with degenerative lumbar spine disease. Neurospine 15, 131–137. https://doi.org/10.14245/ns.1836046.023 (2018).
Lee, C. H. et al. Efficacy and safety of full-endoscopic decompression via interlaminar approach for central or lateral recess spinal stenosis of the lumbar spine: A meta-analysis. Spine 43, 1756–1764. https://doi.org/10.1097/brs.0000000000002708 (2018).
Kim, H. S. et al. Percutaneous full endoscopic bilateral lumbar decompression of spinal stenosis through uniportal-contralateral approach: Techniques and preliminary results. World Neurosurg. 103, 201–209. https://doi.org/10.1016/j.wneu.2017.03.130 (2017).
Perez-Roman, R. J., Basil, G. W., Boddu, J. V., Bashti, M. & Wang, M. Y. Size matters—From the working channel to the wavelength of light: Optimizing visualization in endoscopic spine surgery. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas. 105, 73–78. https://doi.org/10.1016/j.jocn.2022.08.024 (2022).
Meng, S. W. et al. Massively prolapsed intervertebral disc herniation with interlaminar endoscopic spine system Delta endoscope: A case series. World J. Clin. Cases 9, 61–70. https://doi.org/10.12998/wjcc.v9.i1.61 (2021).
Benedetto, U., Head, S. J., Angelini, G. D. & Blackstone, E. H. Statistical primer: Propensity score matching and its alternatives. Eur. J. Cardio Thorac. Surg. Off. J. Eur. Assoc. Cardio Thorac. Surg. 53, 1112–1117. https://doi.org/10.1093/ejcts/ezy167 (2018).
Kane, L. T. et al. Propensity score matching: A statistical method. Clin. Spine Surg. 33, 120–122. https://doi.org/10.1097/bsd.0000000000000932 (2020).
Lewis, R. A. et al. Comparative clinical effectiveness of management strategies for sciatica: Systematic review and network meta-analyses. Spine J. Off. J. N. Am. Spine Soc. 15, 1461–1477. https://doi.org/10.1016/j.spinee.2013.08.049 (2015).
Gibson, J. N. & Waddell, G. Surgical interventions for lumbar disc prolapse: Updated Cochrane Review. Spine 32, 1735–1747. https://doi.org/10.1097/BRS.0b013e3180bc2431 (2007).
Alvi, M. A., Kerezoudis, P., Wahood, W., Goyal, A. & Bydon, M. Operative approaches for lumbar disc herniation: A systematic review and multiple treatment meta-analysis of conventional and minimally invasive surgeries. World Neurosurg. 114, 391-407.e392. https://doi.org/10.1016/j.wneu.2018.02.156 (2018).
Kanno, H., Aizawa, T., Hahimoto, K. & Itoi, E. Minimally invasive discectomy for lumbar disc herniation: Current concepts, surgical techniques, and outcomes. Int. Orthopaed. 43, 917–922. https://doi.org/10.1007/s00264-018-4256-5 (2019).
Smyth, M. J. & Wright, V. Sciatica and the intervertebral disc; an experimental study. J. Bone Joint Surg. Am. 40-a, 1401–1418 (1958).
Lyu, F. J. et al. Painful intervertebral disc degeneration and inflammation: From laboratory evidence to clinical interventions. Bone Res. 9, 7. https://doi.org/10.1038/s41413-020-00125-x (2021).
Ding, H. et al. Progranulin derived engineered protein Atsttrin suppresses TNF-α-mediated inflammation in intervertebral disc degenerative disease. Oncotarget 8, 109692–109702. https://doi.org/10.18632/oncotarget.22766 (2017).
Gawri, R. et al. High mechanical strain of primary intervertebral disc cells promotes secretion of inflammatory factors associated with disc degeneration and pain. Arth. Res. Ther. 16, R21. https://doi.org/10.1186/ar4449 (2014).
Author information
Authors and Affiliations
Contributions
Xuetao Zhu, Yixiang Zhao and Kaiwen Liu: writing—original draft, methodology, investigation, data curation, formal analysis. Yuan Qiang Zhang and Lei Cheng: conceptualization, supervision, writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, X., Zhao, Y., Liu, K. et al. Clinical outcomes of fenestration discectomy and iLESSYS-Delta interlaminar endoscopic system for treatment of LDH: a single-center retrospective cohort study. Sci Rep 14, 20087 (2024). https://doi.org/10.1038/s41598-024-70973-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70973-8
- Springer Nature Limited