Abstract
Atrial fibrillation (AF)/atrial flutter (AFL) is the most common cardiac tachyarrhythmia, with an increasing trend in its burden in recent years. However, the burden of AF/AFL in Iran remains unclear. This study aimed to estimate the burden of AF/AFL and its attributable risk factors from 1990 to 2019 at national and subnational levels. Using the comparative risk assessment method of the Global Burden of Disease (GBD) Study 2019, we extracted data on AF/AFL incidence, prevalence, deaths, disability-adjusted life years (DALYs), and their age-standardized rates from 1990 to 2019 and analyzed them based on by age, sex, and socio-demographic index (SDI). The percentage contribution of AF/AFL major risk factors was calculated. Moreover, the AF/AFL burden in 2050 was projected using the United Nations world population prospect data. In 2019, there were 339.1 (259.4–433.7) thousand AF/AFL patients in Iran, with 30.2 (23.2–38.5) thousand new cases, 1.7 (1.5–2) thousand deaths and 48 (37.7–60.5) thousand DALYs. Females and 50–69-year-old patients recorded a higher burden for AF/AFL; however, the increasing trend was more pronounced in males and more than 85-year-old patients. High systolic blood pressure and elevated body mass index (BMI) were the predominant attributable risk factors for AF/AFL-related deaths and DALYs. It is estimated that in 2050, the number of AF/AFL patients will increase to 1.1 million people, the incidence of AF/AFL will increase to 91 thousand patients, and the number of AF/AFL-related deaths and DALYs will surge to 7.2 and 170.8 thousand, respectively. Despite advancements in prevention and treatment, AF/AFL remains a major public health problem in Iran. Given its largely preventable and treatable nature, more cost-effective strategies are required to target modifiable risk factors, especially within susceptible age and sex groups.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF)/atrial flutter (AFL) stands as the most common type of cardiac tachyarrhythmia, affecting more than 33 million people worldwide1. AF/AFL affects patients’ quality of life besides imposing severe complications such as myocardial infarction, heart failure, and stroke2, leading to AF/AFL-related deaths, which were as high as 315,337 people in 2019 (3]. Based on the 2019 Global Burden of Disease (GBD) study, the absolute number of AF/AFL patients has more than doubled, and the AF/AFL-related deaths and disability-adjusted life years (DALYs) increased significantly, making it one of the leading causes of disability worldwide3.
Population growth and aging are considered the main factors behind the increasing number of AF/AFL cases4,5. The prevalent cases of AF/AFL are projected to double by 2050 and 2060 in the USA and Europe, respectively6,7. Moreover, estimations indicated that the overall AF burden could surge by over 60% by the year 2050, making it a serious public health problem around the world8.
Iran, experiencing epidemiological transitions and population aging, is poised to follow this trend, with an anticipated 17.6% of the population being 60 years and older by 20359. The burden of AF/AFL in Iran, however, remains unclear. It is worth mentioning that Iran’s diverse population encompasses various ethnicities with distinct lifestyles and genetic backgrounds, potentially leading to disparities within the country10. Therefore, it would be important to report and evaluate the burden of AF/AFL in this country and compare results among its provinces to better understand possible differences and inequalities.
Herein, we aimed to analyze and report the GBD 2019 estimations regarding AF/AFL to demonstrate and compare their incidence, prevalence, attributable deaths, years of lost life (YLLs), years lived with disability (YLDs), and DALYs among 31 provinces of Iran from 1990 to 2019 for the first time. Moreover, we provided an estimation for the epidemiology and burden metrics of AF/AFL through 2050. The results of the present study could offer valuable insights to health authorities and policymakers by providing a clearer perspective, guiding them toward more effective strategies and proper allocation of resources among the population to mitigate the burden of AF/AFL and related disorders in the future.
Materials and methods
Data sources
This study was conducted according to the Global Burden of Diseases, Injuries, and Risk Factors Study 2019 investigation, a multinational collaborative research project by the Institute for Health Metrics and Evaluation with the goal of producing consistent estimates of health loss due to various diseases and injuries. The outcomes were reported based on the Guidelines for Accurate and Transparent Health Estimates Reporting (the GATHER statement)11. Details of the GBD framework, methodology, and data estimation for the burden of diseases, injuries, and risk factors have been described previously12,13. The entry data for the present study were obtained from the publicly accessible GBD database14. In this investigation, thirty-one provinces of Iran were used on a subnational scale to report epidemiologic measures and investigate disparities of the burden metrics attributable to AF/AFL.
Definitions
In the study, AF/AFL was identified using the International Classification of Diseases and Injuries (ICD-9 and ICD-10). Specifically, any cardiovascular disease falling under the ICD-9 codes 427.3–427.32 or the ICD-10 codes I48–I48.92 were classified as instances of AF/AFL. YLLs were calculated by multiplying the number of deaths and the standard life expectancy at the age of demise. YLDs were computed by assessing the number of YLLs attributed to health conditions, considering the severity-based disability weight. The sum of YLDs and YLLs arising from premature mortality within the population was considered DALYs.
The Socio-Demographic Index (SDI) was deployed as an analytical tool for positioning each geographical region at a subnational level along the development spectrum. It represents the geometric average of an index ranging from 0 to 1, encompassing factors such as the total fertility rate for individuals under 25, the average educational attainment of those aged 15 and above, and the distribution of income per capita with a lag effect12,15. When considering this composite measure, an SDI value of 0 signifies the lowest conceivable level of development related to health, while an SDI of 1 indicates the highest feasible level. This categorization entailed the division of provinces of Iran into five distinct quintiles, specifically, low, low-middle, middle, high-middle, and high SDI12,15.
In the GBD 2019 study, six risk factors (namely, alcohol use, diet high in sodium, high body-mass index (BMI), high systolic blood pressure, lead exposure, and smoking) were associated with AF/AFL based on the following criteria: adequate evidence for the cause of AF/AFL, availability of exposure data, and the possibility of modification3. The exact definition of these risk factors and methods for quantifying the contribution percentage of these risk factors to AF/AFL-related death and DALY have been demonstrated in previous studies13,15.
Statistical analysis
We calculated the epidemiology and burden metrics of AF/AFL such as incidence, prevalence, DALYs, YLLs, YLDs, and AF/AFL-related deaths beside their age-standardized rate (ASR) per 100,000 people stratified by sex and age groups at both national and subnational levels. Moreover, the age-standardized mortality-to-incidence ratio (MIR), DALY-to-prevalence ratio, YLL-to-YLD ratio, and prevalence-to-incidence ratio were assessed as secondary outcomes for further AF/AFL burden statistics16. The ASR of AF/AFL-related mortality and DALY were calculated to compare its burden in different SDI quantiles. Further decomposition analysis was conducted based on two scenarios to assess the impact of population aging and population growth on the absolute change in AF/AFL incidence. In the first scenario, the age structure, sex structure, and age-specific rates from 1990 were applied to model the total population in 2019. The difference between the total number of cases in 1990 and the hypothetical scenario was attributed to population growth. In the second hypothetical scenario, we applied the age-specific rates from 1990 to the age structure, sex structure, and population size of 2019. Differences between the second and first hypothetical scenarios were attributed to population aging. Furthermore, given no alterations in age-standardized epidemiology, burden metrics, and risk factors of AF/AFL in the future, we used the age and sex-specified ASR of the aforementioned indices between 1990 and 2019 on United Nations world population prospect data to project the incidence, prevalence, DAYs, and deaths attributed to AF/AFL in 205017.
The reported values in this article were represented in point estimation accompanied by the 95% uncertainty intervals (95% UI) extracted using the 25th and 975th ranked draws of the uncertainty distribution by taking 1,000 samples from the posterior distribution. Percent change between 1990 and 2019 was calculated and represented only the change between the beginning and ending years of the period. It’s noteworthy that AF/AFL cannot lead to death directly, but it can increase the risk of mortality by complications including stroke or heart failure. Therefore, the crude case fatality rate in patients with AF/AFL does not seem appropriate, and mortality due to AF/AFL is preferred. All for this study statistical analyses, data visualization, and numerical calculations were carried out using R Programming language (R for Windows, version 4.1.3, Vienna, Austria) and R Studio version 1.1.463 (Posit PBC, Boston, MA, United States).
Results
National epidemiology and burden metrics of AF/AFL
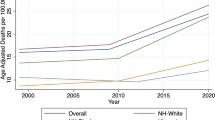
The disease burden of AF/AFL increased significantly over the 30 years. The number of incidences increased from 10,318 (7743–13,431) people in 1990 to 30,246 (23,219–38,550) in 2019, with a 193.1% (174.7–219.6) increase. The age-standardized incidence, however, remained steady. The number of AF/AFL cases escalated from 105,860 (79,863–137,492) people in 1990 to 339,164 (259,425–433,714) in 2019, with a 220.4% (204.7–240.9) increase. The age-standardized prevalence, however, slightly decreased from 518.8 per 100,000 (394.6–666.6) in 1990 to 514 per 100,000 (391.9–659). The number of AF/AFL-related deaths surged from 371 (262–449) in 1990 to 1,766 (1509–2003) in 2019, showing a 375.4% (283.3–587.7) increase. The standardized death slightly increased from 3.1 per 100,000 (2.1–3.8) in 1990 to 3.2 per 100,000 (2.7–3.6). DALY increased from 13,783 (10,574–17,796) in 1990 to 47,997 (37,710–60,548) in 2019, reflecting a 248.2% (216.7–301.7) increase. From 1990 to 2019, the study found an interesting trend: the ASR of incidence, prevalence, and DALYs exhibited a gradual decrease from 1996, reaching a minimum in 2009, followed by a gradual increase after 2009. However, the phenomenon was less pronounced in the ASR of AF/AFL-related deaths, and the parameter didn’t decrease much in the mentioned years (Fig. 1). The epidemiology and burden metrics of AF/AFL are presented in Table 1.
Subnational epidemiology and burden metrics of AF/AFL
At the subnational level, three of Iran’s most populous provinces, namely Tehran, Khorasan Razavi, and Fars, recorded the highest AF/AFL incidence and prevalence in 2019, accounting for 33% of the total number. Moreover, the provinces of Alborz, Tehran, and Qom experienced the most significant increase in AF/AFL incidence [365.3% (337.1–395.7); 255.4% (229.2–288.1); and 254.4% (225.9–285.2), respectively] and prevalence [390.2% (364.8–420.3); 290.3% (262.5–319.1); and 280.6% (257.4–303.6), respectively] over the study period. After age standardization, Fars province recorded the highest incidence [53.1 (39.9–68,9)] and prevalence [644.3 (482.6–837)] rates of AF/AFL in 2019. The detailed results of subnational metrics are presented in Supplementary Tables 1 and 2.
Moreover, three of Iran’s most populous provinces, namely Tehran, Khorasan Razavi, and Isfahan, had the highest AF/AFL-related deaths and DALYs in 2019, accounting for 31% of the national number. Interestingly, the northwestern provinces of Iran (East and West Azarbayejan) recorded the highest age-standardized death [4.5 (3.7–5.4) and 4.6 (3.8–5.5), respectively] and DALY [87.9 (70.8–108.8) and 85.9 (69.3–104.6), respectively] rates attributed to AF/AFL in 2019 (Fig. 2).
Age distribution of AF/AFL epidemiology and burden metrics
Through age stratification, 50–69 individuals had the highest AF/AFL incidence and prevalence in 2019 [14,823 (9925–20,778) and 131,838 (92,387–181,414), respectively]. Additionally, both 50–69-year-old and 70–74-year-old groups had the highest AF/AFL attributed DALY in 2019 [15,164 (10,789–20,773) and 14,252 (11,321–17,842), respectively]. Notably, elderly patients (+ 85 years old) had the highest AF/AFL-related deaths in 2019 [887 (710–1021)] and experienced the most prominent increase in the epidemiology and morbidity metrics compared to other age groups (Fig. 3).
Gender distribution of AF/AFL epidemiology and burden metrics
From 1990 to 2019, there was a notable increase in the incidence, prevalence, deaths, and DALYs for both males and females. The rise in incidence and prevalence was more noticeable in females [204.9% (189.9–226.8) vs. 180.3% (158.3–212.2); and 232.7% (218.9–249.5) vs. 207% (190.3–234.5), respectively]. On the other hand, the increase in AF/AFL-related deaths and DALY was more prominent in males [505.3% (299.3–691.8) vs. 310.9% (222.5–607.6); and 251.6% (194.6–302.9) vs. 245.5% (209.2–338.2), respectively]. The standardized incidence and prevalence in females decreased from 47.3 (35.6–60.9) and 551.8 (419.2–707.9) in 1990 to 46.8 (35.1–60.3) and 546.1 (415.4–700.6) in 2019, respectively. Conversely, the standardized incidence and prevalence in males increased from 38.4 (29.3–49.1) and 478.3 (366.5–615.7) to 38.6 (29.4–49.8) and 482.3 (367.3–617.9) in 2019, respectively. Similarly, the standardized AF/AFL attributed deaths and DALY decreased in females over the 30 years [3.9 (2.4–4.9) vs. 3.8 (3.2–4.5); and 87 (63.1–111.4) vs. 84.5 (67.7–106.3), respectively]. However, the aforementioned metrics increased in males in the same period (2.1 (1.4–2.8) vs. 2.6 (1.8–3) and 61.5 (47–79.5) vs. 66.5 (51.3–84.2), respectively]. Our analysis revealed a higher number and ASR of AF/AFL epidemiological and burden metrics in females in both 1990 and 2019; however, the gap between females and males decreased over the 30 years. The epidemiology and burden metrics of AF/AFL in males and females are presented in Table 1.
In females, the incidence and prevalence of AF/AFL were highest in 50–69-year-old patients both in 1990 [3,057 (2023–4276) and 25,122 (17,542–34,511), respectively] and 2019 [8,102 (5390–11,327); and 66,422 (46,609–91,099), respectively]. AF/AFL-related death was highest in + 85 years old patients both in 1990 [107 (65–136)] and 2019 [486 (389–596]. DALY was highest in 50–69-year-old females in 1990 [3059 (2200–4197.7)], whereas 75–84 years old patients recorded the highest DALY in 2019 [8317 (6619–10,466)]. The rate of all burden metrics of AF/AFL was highest in + 85 years participants both in 1990 and 2019.
In males, the number of incidence, prevalence, and DALY were highest in 50–69-year-old patients both in 1990 [2965 (1987–4,151); 29,286 (20,909–39,998); and 3,192 (2,184–4,492), respectively] and 2019 [6721 (4503–9445); 65,416 (46,557–89,455); and 7241 (5,044–10,102), respectively]. AF/AFL-related death was highest in + 85 years old patients both in 1990 [45 (28–60)] and 2019 [401 (253–474)]. The rate of all burden metrics of AF/AFL was highest in + 85 years participants both in 1990 and 2019.
Socio-demographic distribution of AF/AFL epidemiology and burden metrics
The incidence and prevalence of AF/AFL were higher in high-SDI provinces. Nevertheless, after standardization, there was no difference between different SDI groups regarding the AF/AFL burden both in 1990 and 2019 (Supplementary Fig. 1).
Secondary outcomes
At the national level, the age-standardized MIR remained steady in 2019 compared to 1990 (0.074 vs. 0.072). Moreover, MIR remained steady in females (0.081 vs. 0.082); however, MIR increased in males (0.067 vs. 0.054) (Fig. 4). At the West Azarbayejan subnational level, province reported the highest MIR (0.107), while MIR was the lowest in Chahar Mahaal and Bakhtiari province (0.056) (Supplementary Fig. 2).
Other secondary outcomes, namely, the DALY-to-prevalence ratio, YLL-to-YLD ratio, and prevalence-to-incidence ratio, remained unchanged over the 30 years (0.14 vs. 0.14; 0.91 vs. 0.9; and 12.1 vs. 12, respectively). The secondary outcomes of females didn’t change significantly in 2019 compared to 1990; however, the YLL-to-YLD ratio increased in males in 2019 compared to 1990 (0.78 vs. 0.67).
AF/AFL DALY and death rates attributable to risk factors
A substantial proportion of AF/AFL-related deaths in males and females were attributable to high systolic blood pressure (46% and 47.9%, respectively) and elevated BMI (33.6% and 43.4%, respectively) in 2019. Furthermore, the majority of AF/AFL attributed DALY in males and females were linked to high systolic blood pressure (45.1% and 50.7%, respectively) and high BMI (29.3% and 39.7%, respectively). Of note, the impact of high BMI on AF/AFL-related death and DALY became more pronounced in 2019. Additionally, the effect of elevated BMI on AF/AFL-related death and DALY was more pronounced in females (43.4% vs. 33.6% and 39.7% vs. 29.3%, respectively). In comparison, smoking had a more prominent effect in males (8.6% vs. 1.2%, and 14.2% vs. 2.4%, respectively). (Figs. 5 and 6).
Decomposition analysis
Overall, the increase in AF/AFL cases at the national level was mainly attributed to population aging. This trend held for most provinces, and the effect of population aging was more prominent in Alborz province. On the other hand, in Hormozgan, Sistan, and Baluchistan provinces, the upsurge in AF/AFL cases was primarily due to population growth. The decomposition analysis of new AF/AFL cases at the national and subnational levels is presented in Supplementary Table 3.
Future projections
In 2050 projections of AF/AFL, the incidence will surge to 91,510 people, with a 202.55% increase compared to 2019. Moreover, the prevalence will increase to 1,154,116 people with a 240.28% increase compared to 2019. The rise in AF/AFL incidence and prevalence was more pronounced in females (227% vs. 172% and 275% vs. 201%, respectively). Furthermore, the projected AF/AFL-related death and DALY escalated by 312% and 255% to 7,286 and 170,820 in 2050, respectively. Similar to previous indices, the increase in AF/AFL DALY and mortality was more noticeable in females (298% vs. 203%, and 386% vs. 211%, respectively). Of note, the rise in AF/AFL-related deaths and DALY was more pronounced compared to the increase in incidence and prevalence. Future projections of the epidemiology and burden metrics of AF/AFL are shown in Table 2.
Discussion
Our study provides a comprehensive analysis of the epidemiological and burden metrics of AF/AFL in Iran. We evaluated the incidence, prevalence, deaths, and DALYs of AF/AFL from 1990 to 2019 using high-quality data. Although the age-standardized incidence and prevalence rates of AF/ AFL remained stable during the study period, the absolute number of new cases increased by 193.1% to 30 thousand people, and the prevalence surged by 220.4% to approximately 339 thousand people in 2019. Projections based on United Nations world population data indicate that, in the absence of effective interventions, the annual incidence of AF/AFL will reach about 91 thousand people, and the prevalence will exceed 1 million people by 2050. These increases are notably higher than the global trends, which show a 103.9% rise in incidence and a 111% rise in prevalence over the 30 years18. The findings are in line with previous studies demonstrating that the increase in AF/AFL incidence and prevalence are higher in the Middle East region, which can attributed to many factors, including population aging, rapid economic developments in recent years, and the shift toward westernized diets, despite the slower progress in education and medical care19,20.
Furthermore, our analyses showed that AF/AFL burden is progressively rising, with a 375.4% increase in AF/AFL-related deaths and a 248.2% increase in DALYs. These numbers are higher than global figures, which show a 169.2% increase in AF/AFL-related deaths and a 121.6% increase in DALYs18. Projections suggest that by 2050, AF/AFL-related deaths and DALYs could reach about 7 and 170 thousand annually. Notably, we found that the number of AF/AFL-related deaths and DALY increased faster than the prevalent and incident cases. These trends highlight the urgent need for early detection of AF/AFL beside developing more effective treatment strategies. Global observations showed that the European nations have been more successful in managing the burden of AF/AFL18. Therefore, Iran could benefit from increasing investments in education and medical care alongside employing the public health strategies of European countries to mitigate the following trend.
Disparities in the disease burden of AF/AFL were evident in different gender groups, with overall incidence, prevalence, and AF/AFL-attributed deaths and DALYs higher in females than in males both in 1990 and 2019. The higher incidence and prevalence in females can be explained through two hypotheses. Previous studies have reported that females presented more symptoms for AF/AFL21, which showed that higher amounts of AF/AFL are undetectable in males. Besides that, males may be more prone to neglecting their symptoms and not approaching medical services for further investigations. Moreover, the studies suggested that females are less likely to use rhythm control strategies such as electrical cardioversion, catheter ablation, or surgical ablation22,23, which leads to higher deaths and DALYs. It is noteworthy that the observed gender gap has exhibited a diminishing trend over 30 years. Nevertheless, further research and resource allocation are needed to eliminate the remaining gender inequality.
This study also showed that 50–69-year-old patients exhibited the highest incidence, prevalence, and DALY for AF/AFL. Nonetheless, patients aged 85 years and above had the highest AF/AFL-related mortality with the highest increase in epidemiological and burden metrics. Likewise, previous studies demonstrated that more than 90% of AF/AFL-related mortality occurs above the age of 6524. Even though the underlying mechanisms are still unknown, aging may increase the risk of AF/AFL through several ways, including the myocardial remodeling caused by aging-related underlying diseases, myocardial fibrosis, or age-dependent left atrial dilation (senile amyloidosis)25. Considering the substantial impact of population aging on the increase of AF/AFL burden, the results suggest that the management of AF/AFL in the elderly is insufficient and requires more attention. It is worth mentioning that in contrast to previous studies18, we found no discernible difference between AF/AFL burden metrics among SDI groups after age standardization. This finding highlights the need for further investment in AF/AFL prognosis and treatment without considering the SDI of provinces.
We found that a substantial portion of the disease burden of AF/AFL (including deaths and DALYs) can be traced back to modifiable factors such as high systolic blood pressure, elevated BMI, smoking, and diet. Therefore, diverse strategies are needed to prevent and treat these risk factors. Similar to previous studies, high systolic blood pressure emerged as the leading risk factor in the disease burden of AF/AFL26,27. Therefore, a more aggressive approach to hypertension prevention and treatment is recommended. On the other hand, the impact of elevated BMI on the disease burden of AF/AFL is on the rise, making it a risk factor that cannot be ignored. Studies have shown that, as an independent risk factor, each unit increase in BMI corresponds to a 4–5% increase in the risk of AF/AFL28. Moreover, elevated BMI contributes to the increased risk of AF/AFL by increasing the risk of hypertension29. It is necessary for today’s national and regional health departments to actively seek health, education, and economic-based approaches to mitigate the aforementioned risk factors through healthy lifestyle behaviors like smoking and alcohol cessation programs, encouraging low-salt and low-fat diets, and appropriate exercise.
Limitations
Our study comes with some shortcomings that should be taken into account. First, despite the advancements in AF/AFL diagnosis, a large number of AF/AFL cases are asymptomatic or have paroxysmal attacks and remain undiagnosed with electrocardiogram assessments, leading to underestimating the true burden of AF/AFL. Second, AF/AFL is categorized into different types, including paroxysmal AF/AFL, persistent AF/AFL, and permanent AF/AFL. However, the GBD database failed to distinguish between these variations and recognized all of them as AF/AFL. Therefore, further analyses on AF/AFL types were not possible. Third, the GBD database was unable to specify the specific cause of AF/AFL-related deaths and DALYs in this study. However, it employed various methods to enhance the comparability of the outcomes reported. Fourth, the GBD database was unable to provide the specific treatment strategies for AF/AFL throughout the study period. Nevertheless, we reported ASRs of epidemiological and burden metrics to provide a more robust measure for comparing the effect of old prevention and treatment strategies with newer ones. Fifth, our predictions regarding the future burden of AF/AFL relied on the United Nations world population prospect data by using the age-standardized metrics from 2019. This approach did not consider other influencing factors, which add a degree of uncertainty to the results and should be weighed carefully.
Conclusions
This study showed that despite noticeable advancements, AF/AFL remains a major public health problem in Iran. Over the past 30 years, the epidemiological and burden metrics of AF/AFL have increased significantly, mostly due to population aging and population growth. The burden of AF/AFL varies between different age and gender groups and is more pronounced in over 50–69-year-old patients and females. Moreover, the prevention of AF/AFL is largely achievable through the adoption of healthier lifestyle behaviors.
Data availability
The datasets generated and analyzed during the current study are available on the GBD Study 2019 and the “GBD Compare” web pages. (https://ghdx.healthdata.org/gbd-results-tool and https://vizhub.healthdata.org/gbd-compare/ respectively).
References
Batra, G. et al. Data standards for atrial fibrillation/flutter and catheter ablation: The European Unified registries for heart care evaluation and randomized trials (EuroHeart). Eur. Heart J. Qual. Care Clin. Outcomes 9(6), 609–620 (2023).
Kirchhof, P. et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration With EACTS. Rev. Esp. Cardiol. (Engl Ed). 70(1), 50 (2017).
Dong, X. J. et al. Global burden of atrial fibrillation/atrial flutter and its attributable risk factors from 1990 to 2019. Europace 25(3), 793–803 (2023).
Kornej, J., Börschel, C. S., Benjamin, E. J. & Schnabel, R. B. Epidemiology of atrial fibrillation in the 21st century: Novel methods and new insights. Circ. Res. 127(1), 4–20 (2020).
Staerk, L., Sherer, J. A., Ko, D., Benjamin, E. J. & Helm, R. H. Atrial fibrillation: Epidemiology, pathophysiology, and clinical outcomes. Circ. Res. 120(9), 1501–1517 (2017).
Naccarelli, G. V., Varker, H., Lin, J. & Schulman, K. L. Increasing prevalence of atrial fibrillation and flutter in the United States. Am. J. Cardiol. 104(11), 1534–1539 (2009).
Krijthe, B. P. et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 34(35), 2746–2751 (2013).
Lippi, G., Sanchis-Gomar, F. & Cervellin, G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int. J. Stroke 16(2), 217–221 (2021).
Aghamohamadi, S., Hajinabi, K., Jahangiri, K., Asl, I. M. & Dehnavieh, R. Population and mortality profile in the Islamic Republic of Iran, 2006–2035. East Mediterr. Health J. 24(5), 469–476 (2018).
Health system performance in Iran. A systematic analysis for the global burden of disease study 2019. Lancet 399(10335), 1625–1645 (2022).
Stevens, G. A. et al. Guidelines for accurate and transparent health estimates reporting: The gather statement. Lancet 388(10062), e19–e23 (2016).
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1204–1222 (2020).
Collaborators, G. B. & Ärnlöv, J. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1223–1249 (2020).
Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington (2020). Accessed November 10, 2023. Available online at: http://vizhub.healthdata.org/gbd-compare
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76(25), 2982–3021 (2020).
Azadnajafabad, S. et al. Global, regional, and national burden and quality of care index (QCI) of thyroid cancer: A systematic analysis of the global burden of disease study 1990–2017. Cancer Med. 10(7), 2496–2508 (2021).
United Nations world population prospects website: https://population.un.org/wpp/.
Li, H. et al. Global, regional, and national burden of disease study of atrial fibrillation/flutter, 1990–2019: Results from a global burden of disease study, 2019. BMC Public Health 22(1), 2015 (2022).
Aljefree, N. & Ahmed, F. Association between dietary pattern and risk of cardiovascular disease among adults in the Middle East and North Africa region: A systematic review. Food Nutr. Res. 59, 27486 (2015).
Bhagavathula, A. S., Shehab, A., Ullah, A. & Rahmani, J. The burden of cardiovascular disease risk factors in the middle east: A systematic review and meta-analysis focusing on primary prevention. Curr. Vasc. Pharmacol. 19(4), 379–389 (2021).
Dagres, N. et al. Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: A report from the euro heart survey on atrial fibrillation. J. Am. Coll. Cardiol. 49(5), 572–577 (2007).
Piccini, J. P. et al. Differences in clinical and functional outcomes of atrial fibrillation in women and men: Two-year results from the ORBIT-AF registry. JAMA Cardiol. 1(3), 282–291 (2016).
Schnabel, R. B. et al. Gender differences in clinical presentation and 1-year outcomes in atrial fibrillation. Heart 103(13), 1024–1030 (2017).
Ohlrogge, A. H., Brederecke, J. & Schnabel, R. B. Global burden of atrial fibrillation and flutter by national income: Results from the global burden of disease 2019 database. J. Am. Heart Assoc. 12(17), e030438 (2023).
Ravassa, S., Ballesteros, G. & Díez, J. Aging and atrial fibrillation: A matter of fibrosis. Aging (Albany NY) 11(22), 9965–9966 (2019).
Joglar, J. A. et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: A report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation 149(1), e1–e156 (2023).
Garg, P. K. et al. Association of hypertension severity and control with risk of incident atrial fibrillation: The reasons for geographic and racial differences in stroke (REGARDS) study. Clin. Cardiol. 46(11), 1418–1425 (2023).
De Sensi, F., Costantino, S., Limbruno, U. & Paneni, F. Atrial fibrillation in the cardiometabolic patient. Minerva Med. 110(2), 157–167 (2019).
Grundvold, I. et al. Body weight and risk of atrial fibrillation in 7169 patients with newly diagnosed type 2 diabetes; an observational study. Cardiovasc. Diabetol. 14, 5 (2015).
Author information
Authors and Affiliations
Contributions
H.S., K.T., and A.N. have contributed to the designing, preparing, and analyzing the study’s data. S.A., M.M., and P.E. have contributed to writing the first draft and provided media and tables for the manuscript. F.M., A.V., and K.H. have contributed to the revision, preparing the final draft, and supervising the study. All authors reviewed the manuscript and confirmed the final contents, figures, and tables.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Soleimani, H., Tavakoli, K., Nasrollahizadeh, A. et al. Estimating the burden of atrial fibrillation and atrial flutter with projection to 2050 in Iran. Sci Rep 14, 20264 (2024). https://doi.org/10.1038/s41598-024-71296-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71296-4
- Springer Nature Limited