Abstract
The newly developed portable oxygen concentrator with an auto-demand oxygen delivery system (auto-DODS) automatically switches between 3 sensitivities according to the negative pressure gradient of inhalation and supplies oxygen only during inhalation. The aim of this study was to verify the effectiveness and safety of auto-demand devices compared with a continuous flow oxygen concentrator, during sleep, in a randomized crossover noninferiority trial. We alternatively used an auto-DODS or a continuous-flow oxygen concentrator, all night on separate days for HOT (Home Oxygen Therapy) patients with nocturnal hypoxemic symptoms. The primary endpoints were the mean value of oxygen saturation (SpO2) over the total sleep time. The secondary endpoints included the efficacy endpoints and the safety endpoints. Regarding the primary endpoint, the difference in SpO2 between the auto-DODS and continuous flow was 0.835%. Since the upper limit of this difference did not exceed 2.8, which was set as the noninferiority margin, it was shown that the auto-DODS did not reduce SpO2 by at least 2.8% on average compared to continuous flow. No equipment failure or exacerbation of disease was observed, confirming the safety of the auto-DODS during the night.
Similar content being viewed by others
Introduction
Currently, home oxygen therapy (HOT) is provided to patients with severe chronic respiratory failure, pulmonary hypertension, chronic heart failure, cyanotic congenital heart disease, and severe cluster headaches. HOT has been reported to improve hypoxemia and survival rates and is covered by health insurance1. HOT generally uses “oxygen concentrators” at home and “portable oxygen cylinders” when outside the home. Respiratory synchronizers (demand devices) are devices that supply oxygen from an oxygen cylinder only when the patient breathes in, according to the patient's breathing, saving oxygen and increasing the usable time of the oxygen cylinder by 2 to 3 times. The simplicity of using a single device for all functions is also expected. However, there is concern that this demand oxygen delivery system (DODS) may not be able to supply sufficient oxygen because the flow sensor may not work due to low tidal flow2. The newly developed auto-DODS has an auto-demand mode (the device automatically adjusts the sensitivity according to the frequency of breath detection, progressing from standard to high to extra high sensitivity, so that even shallower breaths can be detected; if no respiration is detected for a certain period of time, the device will automatically supply a predetermined number of intermittent pulses in addition to an alarm sound)3. Therefore, hypothesizing that this auto-DODS is superior to the conventional DODS in improving oxygenation and useful in the treatment of nocturnal hypoxemia, the aim of the current study was to compare the clinically important sleep assessment indices between the oxygen supply of auto-DODS and continuous flow.
Methods
Design
This clinical trial is a single-center, randomized, open-label, crossover, noninferiority study to evaluate the efficacy and safety of the auto-DODS in patients undergoing HOT. This trial was performed at Kobe University Hospital and was approved by the Kobe University Clinical Research Ethical Committee (permission number: CRB5180009). This trial was also registered in the Japan Registry of Clinical Trials (jRCT) on August 23, 2019 (trial ID: jRCTs052190042). The registration period was set from August 2019 to August 2022. Patients eligible for the study were scheduled for two consecutive nights of therapy sessions. On the first night, patients utilized one device. On the subsequent night, patients used the other device. Four weeks later, they were checked for safety. The details are shown in a previous publication4.
Written informed consent was obtained from all the participants included in this study. All procedures were performed in accordance with the ethical standards of the institutional and national committees and with the Helsinki Declaration in 1964 and its later amendments or comparable ethical standards.
Participants
We recruited patients who met all of the selection criteria and none of the exclusion criteria. The selection criteria included patients (1) who required HOT at night (nighttime prescription flow ≤ 3 L/min), (2) with chronic obstructive pulmonary disease (COPD) or interstitial pneumonia, (3) who were able to walk independently while holding a portable device, (4) with written consent for participation in this study, and (5) who were at least 20 years of age. The exclusion criteria included patients (1) receiving noninvasive positive pressure ventilation (NPPV) therapy, (2) receiving continuous positive airway pressure (CPAP) therapy, (3) with symptomatic congestive heart failure, unstable angina, a history of myocardial infarction within 1 year prior to enrollment, or clinically significant arrhythmia (complete left bundle branch block [LBBB], 3rd degree atrioventricular block [AVB], 2nd degree AVB, ventricular fibrillation [Vf]) on electrocardiogram (ECG), (4) with hemoglobin < 9 g/dl within 3 months of screening, (5) with exacerbation of COPD or interstitial pneumonia (IP) within 3 months of screening, (6) who were pregnant, possibly pregnant, or lactating women, and (7) who had been deemed ineligible for inclusion by the study investigator or subinvestigator.
Randomization
After registration, 20 participants were randomly assigned by permuted block randomization to either Group 1 (auto-DODS on Day 1 followed by continuous flow on Day 2) or Group 2 (continuous flow on Day 1 followed by auto-DODS on Day 2) (allocation ratio 1:1). The allocation table was managed at the data center and kept confidential from the investigators. The allocated group was not masked to the patients and investigators.
Sample size
Referring to the results of a previous study when using continuous flow and auto-DODS (sensitivity fixed to extra high) at night in HOT patients: results of an unpublished clinical trial, the difference in mean SpO2 values was 1.8% between the continuous flow group and the auto-demand group, and the value was higher in the continuous flow group. The standard deviation (SD) of the SpO2 difference was 1.37%. The noninferiority margin was 2.8%, equivalent to 70% of the minimal clinically important difference (± 4%) of SpO25. This value was previously reported as the predominant SpO2 drop during exertion in patients with pulmonary disease6. When we used a t test for the difference of the difference, assuming a difference of 1.8% of mean SpO2 and a standard deviation of 1.4, we required 8 patients per group to maintain 80% power. The target number of cases for this clinical study was set at 10 with the expectation of approximately 20% ineligible cases. The details are shown in a previous publication4.
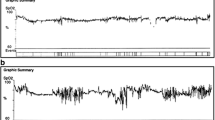
Device and measurement
Hi-Sanso Portable αII (Teijin Pharma Ltd., Tokyo, Japan) and Hi-Sanso 5S (Teijin Pharma Ltd., Tokyo, Japan) were employed all night (from 10 pm to 8 am) on separate days. The former had an auto-DODS, and the latter had a continuous-flow oxygen concentrator. The equipment was used according to the manual, and a personal computer was connected for sensitivity setpoint data acquisition. The oxygen flow rate on the Hi-Sanso Portable αII was adjusted so that the SpO2 was approximately the same as the SpO2 at continuous flow that the patient normally used. Participants were equipped with either devices and physiological data were continuously recorded by sleep evaluation device, Alice PDx (Philips Japan, Ltd., Tokyo, Japan). SpO2 were measured with attached finger sensors.
Endpoints
The primary endpoint was the mean value of SpO2 over the total sleep time (%): mean SpO2 at the time when Alice PDx confirmed that the patient was asleep. The secondary endpoints as the efficacy endpoints were (1) percentage of time when the auto-DODS operated at each sensitivity during the total sleep time (%), (2) percentage of time when SpO2 was below 90% during the total sleep time (%), (3) time when SpO2 was below 90% during the total sleep time (min), (4) minimum value of SpO2 during the total sleep time (%), (5) mean pulse rate during the total sleep time (beats per min), (6) maximum pulse rate during the total sleep time (beats per min), (7) frequency of apnea during the total sleep time (events per h): Apnea Index (AI), (8) frequency of apnea and hypopnea during the total sleep time (events per h): AHI, (9) total sleep time confirmed by an electroencephalogram (min), and (10) comfort and reliability evaluated by the numerical rating scale (NRS) and total score of responses to the questionnaire below in Fig. 1 (points). The secondary endpoints, i.e., safety endpoints, were incidence of disease: occurrence of disease, etc., among the number of study subjects excluding those who never received protocol treatment among all enrolled patients. The severity (grade) of each observed disease is the worst grade during the observation period.
Data presentation and statistical analysis
The number of cases, mean value, standard deviation are reported herein for continuous variables, and the frequency and percentage are reported for nominal and ordinal scales. The noninferiority margin for the primary endpoint was set at 2.8%, and the one-sided significance level for the test was 2.5%. For the secondary endpoints, the null hypothesis was that the differences between the two devices would be equal. The significance level for the test was set at a two sided 0.05. Subgroup analyses were performed by underlying disease (COPD/interstitial pneumonia) or the degree of AHI for each endpoint. The confidence level for interval estimation was set at 95%.
SAS Ver. 9.4 (SAS Institute Inc., Cary, NC) was used for analytical statistics. Statistical analyses were performed by a biostatistician at the Clinical and Translational Research Center at Kobe University Hospital (S.M.).
Results
The result of randomization and participants’ characteristics
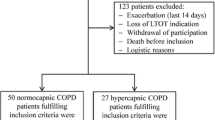
The flow diagram of the patients is shown in Fig. 2. One patient in the auto-demand followed by continuous flow group was excluded from the full analysis set (FAS) because baseline data for VISIT1 were not available. The characteristics of the participants in this study are summarized in Table 1. The clinical trial enrollment date for the first patient (enrollment #01) was 07/10/2019.
Twenty participants were assessed for eligibility. None of them met the exclusion criteria, and all of them were randomly assigned to either the auto-DODS followed by continuous flow group or the continuous flow followed by auto-DODS group (allocation ratio 1:1). One patient in the auto-DODS followed by continuous flow group was excluded from the largest analysis population because baseline data for VISIT1 were not available.
The primary endpoints
The mean values of SpO2 over the total sleep time are shown in Fig. 3. The difference in SpO2 between continuous flow and auto-DODS was 0.835% (95% confidence interval (CI) [0.133, 1.54]) in the study based on the difference in periods. Since the upper limit of the instrument difference was 1.54 and did not exceed 2.8, which was set as the noninferiority margin, it is thought that the auto-DODS showed noninferiority in the mean SpO2 compared to the continuous flow. A similar trend was observed in the analysis of covariance conducted as a sensitivity analysis (Δ0.86: 95% CI [0.16, 1.57]). On the other hand, in the group with an AHI of 30 or higher, the upper limit of value exceeded 2.8.
The secondary endpoints
The percentage of time when the auto-DODS operated at each sensitivity during the total sleep time is shown in Fig. 4. The percentage of time when SpO2 was below 90% during the total sleep time is shown in Fig. 5. There was no significant difference between the different devices (continuous flow—auto-DODS, -4.17, 95% CI [-12.28, 3.94]). The times when SpO2 was below 90% during the total sleep time are shown in Fig. 6. There was no significant difference between the different devices (continuous flow—auto-DODS, − 14.25, 95% CI [− 40.82, 12.32]). There was no significant difference in the minimum values of SpO2 during the total sleep time between the different devices (continuous flow—auto-DODS, 1.06, 95% CI [-0.426, 2.55]). However, in the subgroup analysis, values in the auto-DODS group tended to be lower in COPD patients. In the group with an AHI of 30 or higher, the values were also lower in 3 out of 4 patients with auto-DODS. There was no significant difference in the mean pulse rates during the total sleep time between the different devices (continuous flow—auto-DODS, − 0.375, 95% CI [− 1.92, 1.17]). There was no significant difference in the maximum pulse rates during the total sleep time between the different devices (continuous flow—auto-DODS, − 0.500, 95% CI [− 4.59, 3.59]). There was no significant difference in AI values between the different devices (continuous flow—auto-DODS, 1.04, 95% CI [− 0.737, 2.81]). The AHI was significantly higher in auto-DODS than in continuous flow (continuous flow – auto-DODS, − 4.96, 95% CI [− 9.16, − 0.758]). There was no significant difference in the total sleep time confirmed by an electroencephalogram between the different devices (continuous flow—auto-DODS, 24.2, 95% CI [-9.03, 57.4]). There was no significant difference in the comfort level and reliability between the different devices in terms of the NRS (continuous flow—auto-DODS, 0.113, 95% CI [− 1.31, 1.54]) and total scores of the responses to the questionnaire (continuous flow—auto-DODS, − 1.31, 95% CI [− 2.91, 0.283]). A list of overall differences is shown in Fig. 7.
Safety when using the demand oxygen delivery system
Two patients had Common Terminology Criteria for Adverse Events (CTCAE) version 5.0 Grade 1 illnesses such as skin itching due to the application of the measuring device, but no illnesses due to HOT were observed. There were no cases of equipment malfunctions.
Discussion
Long-term oxygen therapy is an established treatment for patients with chronic hypoxemia. Its scientific basis is derived mainly from two trials from the early 1980s that showed a survival advantage for patients with COPD who were treated with long-term oxygen therapy7,8. The goals of the therapy are to improve quality of life and exercise performance, as well as to reduce morbidity and mortality9. In addition to devices with a continuous flow of oxygen, devices with “demand” systems release an oxygen bolus when negative pressure occurs in the oxygen nasal cannula during inspiration. This delivery form can make the oxygen supply last significantly longer10.
In a previous report evaluating the nocturnal efficiency of the demand oxygen delivery system (DODS), the oxygen savings with the DODS was, on average, 60%. In a comparison of DODS and continuous flow, there were no significant differences in oxygenation or sleep quality, but the continuous flow tended to be slightly better for oxygenation11. Tiep et al. compared deoxygenation at rest and during exertion in 10 patients with chronic respiratory disease. It was found that SpO2 at rest was 93.8 ± 1.9% with continuous flow and 93.7 ± 2.1% with demand flow, which were comparable; during exertion, SpO2 was 93.1 ± 3.1% with continuous flow, 90.5 ± 3.8% with corresponding settings for demand flow, and 92.5 ± 2.8% with higher settings for demand flow12. Garrod et al. also conducted a randomized controlled trial of continuous flow versus demand flow in 14 COPD patients and reported no significant difference in deoxygenation between continuous flow and demand flow in terms of the walking distance under 2 L/min oxygen inhalation (P = 0.72)13. Overall, continuous flow and demand flow are now considered to have comparable oxygenation trends, whether at rest or during exertion, and demand devices are widely used in the marketplace. On the other hand, the auto-demand device newly developed in this study has 3 levels of sensitivity and generates pulsed flow in the absence of respiration detection. Previous studies have confirmed that there is no difference in oxygenation between auto-demand and conventional demand in daytime (at rest: P = 0.73, 6-min walk test: P = 0.99)3.
Most outcomes show similar results between continuous flow and auto-DODS Specifically, the times when SpO2 was below 90% during the total sleep time and the total sleep time to be better in continuous flow. However, as illustrated in Fig. 6, only one patient exhibited significantly higher values in auto-DODS, which had a considerable impact on the overall results for the times when SpO2 was below 90% during the total sleep time due to the small sample size. On the other hand, time to sleep may shorter in DODS and it is possible that the lack of statistical differences is simply due to the small number of cases.
Despite the longer time when SpO2 was below 90% during the total sleep time and shorter total sleep time, even in this regard, we predicted that the usefulness and safety of auto-demand devices would be no less than that of continuous flow. In this study, we evaluated the efficacy of demand flow during sleep for the first time and showed that the primary endpoint, nocturnal SpO2, was not inferior between the auto-demand mode and the respective oxygen delivery of continuous flow.
There were four patients whose SpO2 was more than 2% lower in the auto-demand mode, but there were no other distinguishing characteristics except that all were male. For the secondary endpoint of comfort, almost half of the patients answered that auto-DODS was better, half of the patients answered that it was worse, and among the patients who answered that auto-DODS was more comfortable, none showed a more than 2% drop in SpO2, suggesting that auto-DODS may be safe for patients who evaluated it on the comfort scale. Ventilation in patients with chronic respiratory diseases is heavily dependent on the ventilatory assist muscles, which are affected during sleep and may have contributed to apnea and hypopnea. The AHI was significantly higher in the auto-demand mode (P = 0.0240), and this may have been due to the absence of airflow during exhalation (zero PEEP), but since the patients themselves did not seem to be bothered by the increased AHI based on the results of the questionnaire, we do not consider this to be a particular problem. There was no significant difference between the different devices in sleep duration or comfort. There was no significant difference in overall cases, and the patients with COPD on auto-DODS had significantly shorter sleep times. The COPD group had more patients with a higher AHI, which may be the reason for this. Three patients had higher mean SpO2 in the auto-demand mode, all with AHI less than 30, and the set flow rate of auto-DODS was as low as 1 L/min. Thus, with the exception of patients with severe SAS, auto- DODS may be appropriate for patients with low flow rates at night.
In terms of sensitivity, using auto-DODS, it may be possible to detect cannula dislodgement or mouth breathing based on the presence or absence of a constant pulse rate (alarm). In the group with AHI greater than 30, noninferiority of auto-DODS was not demonstrated for mean SpO2 (P = 0.277). This indicates that a constant pulse rate may not work well enough in patients with a high AHI, and certain precautions may need to be taken. In other words, although this is a subgroup analysis, it is possible that patients with high AHIs should not use auto-demand devices. The previous study reported that obstructive sleep apnea (OSA) was highly prevalent in patients for whom HOT was indicated with moderate-to-severe COPD14, so we should screen for SAS in actual clinical practice.
Our study had several limitations. First, one patient was excluded from the largest analysis population because the electrode was dislodged by body movement during sleep, resulting in inaccurate measurements. Moreover, there were two patients in each group whose SpO2 could not be properly evaluated because the finger sensors were disconnected during sleep. However, since approximately 20% ineligible cases were anticipated when the target number of patients was set, we believe this would not have a significant impact on the results of this study. Second, the primary endpoint was evaluated using SpO2 measured by pulse oximetry rather than arterial blood oxygen saturation or arterial blood oxygen pressure. However, pulse oximetry has proven to be effective in measuring arterial blood oxygen saturation, so we also believe it is not a major issue in this case15. Third, the small sample size might have resulted in lack of power for some endpoints. Fourth, we decided the endpoints of auto-DODS based on the data from only one-day treatment to minimize the length of hospitalization. Fifth, the mean value of SpO2 can be normal, but still with significant desaturations. Sixth, we were not able to evaluate CO2 levels because we did not routinely perform arterial blood gas testing or use capnometers on all patients.
We recruited patients with COPD or interstitial pneumonia from outpatient clinic in this time, but would like to include patients with other pathologies such as heart failure in the future, considering that these patients usually have nocturnal desaturation and irregular breathing patterns.
Conclusions
The primary endpoint was met since the upper limit of the difference did not exceed 2.8, which was set as the noninferiority margin. Therefore, it was shown that auto-DODS did not reduce SpO2 compared to continuous flow. No equipment failure or exacerbation of disease was observed, confirming the safety of the auto-demand device during the night.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ekström, M. Clinical usefulness of long-term oxygen therapy in adults. N Engl. J. Med. 375, 1683–1684 (2016).
Roberts, C. M., Bell, J. & Wedzicha, J. A. Comparison of the efficacy of a demand oxygen delivery system with continuous low flow oxygen in subjects with stable COPD and severe oxygen desaturation on walking. Thorax. 51, 831–834 (1996).
Otoshi, T. et al. A randomized crossover pilot study comparing the efficacy of an auto-demand oxygen delivery system with that of a conventional demand oxygen delivery system in patients with chronic respiratory failure. Medicine (Baltimore). 100, e27191 (2021).
Nagano, T. et al. Randomized cross-over trial of demand oxygen delivery system in nocturnal hypoxemia. Medicine (Baltimore). 99, e20031 (2020).
Tang, J., Mandrusiak, A. & Russell, T. The feasibility and validity of a remote pulse oximetry system for pulmonary rehabilitation: a pilot study. Int. J. Telemed. Appl. 2012, 1–12 (2012).
Balfour-Lynn, I. M. et al. A step in the right direction: assessing exercise tolerance in cystic fibrosis. Pediatr. Pulmonol. 25, 278–284 (1998).
Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: A clinical trial. Ann. Intern. Med. 93, 391–398 (1980).
Report of the Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1, 681–686 (1981).
Magnussen, H. et al. Leitlinien zur Langzeit-Sauerstofftherapie. Pneumologie. 62, 748–756 (2008).
Tiep, B. & Carter, R. Oxygen conserving devices and methodologies. Chron. Respir. Dis. 5, 109–114 (2008).
Cuvelier, A. et al. Nocturnal efficiency and tolerance of a demand oxygen delivery system in COPD patients with nocturnal hypoxemia. Chest. 116, 22–29 (1999).
Tiep, B. L., Barnett, J., Schiffman, G., Sanchez, O. & Carter, R. Maintaining oxygenation via demand oxygen delivery during rest and exercise. Respir. Care. 47, 887–892 (2002).
Garrod, R., Bestall, J. C., Paul, E. & Wedzicha, J. A. Evaluation of pulsed dose oxygen delivery during exercise in patients with severe chronic obstructive pulmonary disease. Thorax. 54, 242–244 (1999).
Yoshizaki, A. et al. Prospective study of nocturnal desaturation in patients receiving home oxygen therapy. Intern Med. 60, 3071–3079 (2021).
Mihm, F. G. & Halperin, B. D. Noninvasive detection of profound arterial desaturations using a pulse oximetry device. Anesthesiology. 62, 85–87 (1985).
Acknowledgements
The authors are grateful to all participating patients, the staff of the Clinical and Translational Research Center and the Division of Respiratory Medicine of Kobe University Hospital. They also acknowledge assistance from medical writers, proof-readers and editors.
Author information
Authors and Affiliations
Contributions
T.N. was responsible for the organization and coordination of the trial. S.M. was the chief investigator and responsible for the data analysis. A.Y. drafted the original manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
This study is funded by Teijin Pharma Limited. Teijin Pharma Limited was not involved in the study design, patient recruitment, management, analysis, interpretation of data, writing of the report, or the decision to submit the report for publication. Teijin Pharma Limited does not have any authority over these activities. Motoko Tachihara received a research grant from Teijin Pharma Limited. Tatsuya Nagano received honoraria from AstraZeneca and GlaxoSmithKline. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yatani, A., Nagano, T., Murakami, S. et al. Randomized crossover trial of a demand oxygen delivery system in nocturnal hypoxemia. Sci Rep 14, 20505 (2024). https://doi.org/10.1038/s41598-024-71320-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71320-7
- Springer Nature Limited