Abstract
To explore whether the potential instability of the cervical spine and cervical muscle degeneration in patients with cervical spondylotic radiculopathy (CSR) affect the efficacy of cervical traction, and whether cervical traction can aggravate the potential instability of the cervical spine. We divided the 113 recruited CRS patients into three groups based on the differences in horizontal displacement and abnormal angle, and measured the degree of cervical muscle degeneration in the patients through MRI. Considering functional scores, VAS, NDI and PCS scores of the three groups post-treatment were significantly improved. Through the intergroup analysis, we found that the improvement in functional scores in the mild and moderate instability trend groups was better than that in the severe group. Through MRI measurements, we found that the degree of cervical muscle degeneration was significantly increased in the severe instability trend group. Regarding the changes in X-Ray imaging parameters pre- and post-treatment, no significant differences were observed pre- and post-treatment. For patients with CSR, the more serious their predisposition for cervical instability was, the more severe the degree of cervical muscle degeneration was, which means the worse the curative effect was, but cervical traction did not aggravate the potential degree of cervical instability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Cervical spondylotic radiculopathy (CSR) primarily results from the lateral protrusion of the intervertebral disc or the narrowing of the intervertebral foramen. This condition is characterized by degenerative cervical disease, manifesting as radiating pain and numbness in the neck, shoulders, and upper limbs. As the population ages and lifestyles evolve, there is a growing prevalence of cervical spondylosis, with CSR constituting 60–70% of reported cases1. It has been reported that the annual incidence rate of CSR is approximately 1.79/10002. In recent years, the number of patients has increased year by year, with the onset of CSR gradually impacting younger populations, which has attracted extensive attention3.
CSR is presently managed using a gradual approach, and it is advised to pursue conservative treatment initially. Surgical intervention is recommended for patients who do not respond to nonsurgical treatments or those experiencing severe clinical symptoms1. Lately, a guideline addressing cervical spondylotic radiculopathy highlighted that improvements in patient-reported pain have been linked to cervical halter traction, as well as combinations of medications, physical therapy, injections, and traction, as observed in uncontrolled case series4.
The main content of diagnosing spinal instability is the loss of stability of functional spinal units (vertebrae, ligaments, and muscle complexes), which may lead to decreased elasticity, increased mobility, and abnormal movement5,6,7. Since White et al.5 first reported the X-ray measurement method of cervical instability: (1) More than 3.5 mm horizontal displacement of one vertebra in relation to an adjacent vertebra, anteriorly or posteriorly, measured on resting lateral or flexion–extension roentgenograms of the spine; (2) More than 11 degree of rotational difference to that of either adjacent vertebra, measured on a resting lateral or flexion–extension roentgenogram. And it has been widely used in the clinical setting8. Meanwhile, with the deepening understanding of cervical muscle, the degree of cervical muscle degeneration is also widely used to evaluate the degree of symptoms and postoperative efficacy in patients with cervical spondylosis9,10,11,12,13.
The Efficacy of Cervical Traction in Individuals Afflicted with CSR has been studied and reported by an increasing number of scholars14,15. However, there are few reports on whether the potential degree of cervical instability and cervical muscle degeneration in patients with CSR affect the efficacy of cervical traction. Hence, this study aimed to investigate two primary aspects: (1) the impact of the potential degree of cervical instability on the efficacy of cervical traction and its potential to exacerbate cervical instability in patients with CSR, and (2) whether the extent of cervical muscle degeneration influences the effectiveness of cervical traction in individuals with CSR.
Materials and methods
Ethics
Ethical approval for this study was provided by the Ethics Committee of Fujian Medical University Union Hospital on May 13, 2022. The ethical review number is 2022KY092.
Statement
We declare that we confirm that all methods were performed in accordance with relevant guidelines and regulations and that all experimental protocols have been approved by notified agencies and/or licensing committees. At the same time, we ensure that informed consent has been obtained from all subjects and/or their legal guardians.
Study participants
This study, conducted as a retrospective cohort investigation, spanned from January 2019 to January 2022, during which 152 patients diagnosed with cervical spondylotic radiculopathy (CSR) participated. Approval for this study was granted by the ethics committee, as detailed in the Ethics section of the “Materials and methods”. Inclusion criteria comprised: (1) initial diagnosis of cervical spondylotic radiculopathy based on clinical symptoms and imaging examinations; (2) patients with fully discernible lateral cervical radiographs displaying all relevant bone markers for accurate measurements; (3) patients with clear cervical MR images enabling precise measurement of imaging parameters; and (4) patients with comprehensive records of the visual analog scale (VAS), neck disability index (NDI) scores, and Medical Outcomes Study Short-Form 36 (SF-36). Exclusion criteria included: (1) cervical spondylotic myelopathy; (2) evident cervical spinal instability (horizontal displacement > 3.5 mm or abnormal angle > 11° on neutral or flexion–extension cervical radiographs); (3) cervical extraspinal lesions like thoracic outlet syndrome, humeral epicondylitis, carpal tunnel syndrome, cubital tunnel syndrome, and frozen shoulder; (4) severe underlying diseases such as diabetes or cardiopulmonary conditions; (5) a history of spinal surgery, cervical trauma, or other disorders affecting spinal function (e.g., rheumatoid arthritis, ankylosing spondylitis, infectious rheumatic diseases, tumors, tuberculosis); and (6) incomplete imaging or functional score data. Figure 1 provides a summary of patients excluded based on the inclusion criteria, and ultimately, 113 patients with CSR were included in the study.
Conservative treatment: Cervical traction was supplemented by one nonsteroidal analgesic and one neurotrophic drug. The patient underwent cervical traction while seated, maintaining a 10–15°forward flexion of the cervical spine. The traction involved a weight equivalent to 15–20% of the body weight and lasted for 15–20 min once daily (Equipment model: Electric intermittent traction device (produced by NIHON MEDIX, Japan, model 5021E)). Specific parameters were adjusted based on the patient’s tolerance and the observed treatment effects. The treatment time was 2 weeks.
According to the difference in horizontal displacement and abnormal angle measured on cervical lateral or flexion/extension radiographs, the patients were divided into three groups: mild instability trend group (horizontal displacement < 1.2 mm or abnormal angle < 4°), moderate instability trend group (1.2 mm ≤ horizontal displacement < 2.4 mm or 4° ≤ abnormal angle < 8°) and severe instability trend group (2.4 mm ≤ horizontal displacement < 3.5 mm or 8° ≤ abnormal angle < 11°).
Basic data collection and parameters measured
-
1.
Basic data: Age, sex, BMI, smoking history, alcohol consumption history, VAS scores, NDI scores, SF-36 scores and therapeutic efficacy rate;
Smoking background: Individuals who have smoked more than one cigarette daily for over six months or those who have consumed more than 100 cigarettes in total. Alcohol usage history: Individuals who engage in drinking at least once a week for over half a year.
The Visual Analog Score (VAS) was documented using an 11-point numeric rating scale ranging from zero (indicating no pain) to ten (representing the worst imaginable pain). Neck function was assessed using the Neck Disability Index (NDI). Patient evaluations encompassed pain intensity, self-care proficiency, weightlifting capability, reading aptitude, presence of headaches, concentration, work performance, sleep quality, driving, and engagement in recreational activities. The total NDI score was capped at 100, with higher scores indicative of poorer neck function.The Medical Outcomes Study Short-Form 36 (SF-36) comprises eight scales (vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning, and mental health), along with two summary measures: the Physical Component Summary (PCS) and the Mental Component Summary (MCS).
Therapeutic effectiveness rate: Our study defines the therapeutic efficacy rate as a 20% decrease in the Neck Disability Index (NDI) following conservative treatment, considering that the minimal clinically important difference (MCID) in NDI has been previously documented to range between 15 and 17%, with a standard deviation of 17%.16,17.
-
2.
Cervical spinal parameters in X-rays: C2-C7 Cobb angle (CL), T1 slope (T1S), C2-7 sagittal vertical axis (SVA), CL (Flexion, F), CL (Extension, E), CL (Range of motion, ROM), horizontal displacement and abnormal angle. Meanwhile, the relevant parameters of the cervical vertebrae and spinal canal with the most obvious unstable trend were measured: Anteroposterior diameter of the vertebral body (AP), Sagittal developmental diameter of the cervical canal (SDD) and Pavlov ratio (SDD/AP).
Standard radiographic techniques were employed for capturing lateral cervical radiographs. The tube-to-subject distance was set at 72 inches, and the radiographic tube was precisely centered at the C4–C5 intervertebral disc space, without any magnification. The lateral radiographs of the cervical spine were acquired with the patient in a comfortable standing position. During the procedure, the upper extremities were positioned naturally at the sides of the trunk, and the patient maintained a straight-ahead gaze.
Cervical radiographs in flexion or extension were obtained with the patient positioned laterally in front of the camera frame. During the procedure, the patient maximally flexed or extended the head and neck, aligning the long axis of the neck parallel to the film's long axis. Additionally, the shoulders were allowed to droop as much as possible. The imaging technician consistently captured all images, maintaining the same requirements as those for lateral films. Range of motion (ROM) was determined by calculating the difference between extension and flexion.
Table 1 and Fig. 2 provide detailed explanations of the methods employed to measure cervical sagittal parameters in the radiographs.
For assessing corresponding segmental paravertebral muscle degeneration on MRI, the following categories were considered: up(low)-fat/muscle, up(low)-fat/centrum, and up(low)-muscle/centrum.
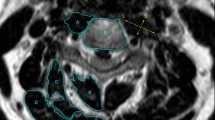
All enrolled patients underwent a preoperative 3.0 T MRI scan using Siemens Medical Solutions equipment in Erlangen, Germany. Axial MRI images were aligned parallel to the inferior endplate of the vertebral body. The cross-sectional area (CSA) of the vertebral body served as a reference point. CSA at each level was calculated by outlining a polygon shape around the outer margins of fat tissue, extensor muscles, and the vertebral body on axial T2-weighted images. ImageJ was utilized for measurements, distinguishing functional muscle (without fatty infiltration) using the software's threshold. The measurement protocol focused on the fan-shaped region enclosed by lines connecting the midpoint of the anterior vertebral body and the front vertices of the sides of the vertebrae. Extensor muscles, including multifidus, rotators, semispinalis capitis and cervicis, splenius capitis and cervicis, levator scapulae, and longissimus, were included in the assessment. CSA ratios between fat, muscle, and centrum were also measured.
Table 1 and Fig. 3 elaborate on the methods used to measure cervical MRI parameters. In cases of multisegment degeneration, measurement focused on the most severe segment.
The measurement range is within the fan shape enclosed by the bilateral lines connecting the midpoint of the anterior vertebral body and the front vertices of the side blocks. A, Vertebral body; B, Multifidus; C, Semispinalis cervicis; D, Semispinalis capitis; E, Splenius capitis and cervicis; F, Levator scapulae and Longissimus; G, Fat; Muscle area = B + C + D + E + F. Fat area = G + Fat infiltration in the muscle area.
Statistical analysis
DICOM data containing all images were transferred to a computer. Two independent observers utilized OsiriX Lite v 7.5 imaging software (Icestar Media Ltd, Essex, UK) to conduct measurements. Following consensus between the observers, two orthopedic spine surgeons individually measured each parameter twice. The intraclass correlation coefficient (ICC) was employed for analysis. Intra- and interobserver agreement were evaluated using ICC values, with scores of 0.8 to 1.0 considered excellent, 0.6 to 0.79 deemed good, and less than 0.6 classified as poor.
Statistical analyses were performed using SPSS 24.0, with statistically significant differences identified at P values < 0.05. For continuous variables, the Shapiro–Wilk normality test determined expression as mean ± standard deviation for normally distributed variables and as median (lower quartile–upper quartile) for non-normally distributed variables. Intergroup analysis followed these guidelines: the chi-square test for categorical variables, one-way ANOVA/Paired sample t test for normally distributed continuous variables, and the Kruskal–Wallis H test for non-normally distributed continuous variables. Pearson and Spearman correlation coefficients were employed to calculate the correlation between each parameter.
Reliability analysis
Concerning the parameters of the cervical spine, the intraobserver and interobserver reliability findings demonstrated excellent and good agreement, respectively, with an Intraclass Correlation Coefficient (ICC) of 0.8 or higher.
Results
Basic data
The mild instability trend group included 40 patients, 21 males (52.5%) and 19 females (47.5%), with an average age of 53.0 ± 10.3 years. The mean BMI was 22.6 ± 3.0 kg/m2. There were 11 smokers (27.5%) and 4 alcohol drinkers (10.0%). The mean AP was 17.38 ± 1.07 mm, the mean SDD was 17.16 ± 1.09 mm, the mean Pavlov ratio was 0.99 ± 0.06, the mean horizontal displacement was 0.82 ± 0.21 mm, and the mean abnormal angle was 2.7 ± 0.7°. The therapeutic efficacy rate was 85.0% (34/40).
The moderate instability trend group included 46 patients, 32 males (69.6%) and 14 females (30.4%), with an average age of 55.3 ± 11.3 years. The mean BMI was 23.3 ± 2.7 kg/m2. There were 10 smokers (21.7%) and 6 alcohol drinkers (13.0%). The mean AP was 17.60 ± 1.01 mm, the mean SDD was 17.23 ± 1.02 mm, the mean Pavlov ratio was 0.98 ± 0.06, the mean horizontal displacement was 1.93 ± 0.24 mm, and the mean abnormal angle was 6.6 ± 0.8°. The therapeutic efficacy rate was 69.6% (32/46).
The severe instability trend group included 27 patients, 13 males (48.1%) and 14 females (51.9%), with an average age of 52.3 ± 10.0 years. The mean BMI was 23.3 ± 2.3 kg/m2. There were 7 smokers (25.9%) and 3 alcohol drinkers (11.1%). The mean AP was 17.39 ± 0.99 mm, the mean SDD was 16.82 ± 1.06 mm, the mean Pavlov ratio was 0.97 ± 0.05, the mean horizontal displacement was 2.91 ± 0.19 mm, and the mean abnormal angle was 9.7 ± 0.5°. The therapeutic efficacy rate was 44.4% (12/27).
The degree of cervical muscle degeneration and remaining basic data results are shown in Tables 2 and 3.
Comparison among the mild/moderate/severe instability trend groups
In the basic data, there was no significant difference among the three groups regarding age, sex, BMI, smoking history, drinking history, Pre-VAS, Pre-NDI, Pre-PCS and Pre-MCS (P > 0.05). Therefore, there was comparability in the difference in curative effects after conservative treatment (Table 2).
In imaging parameters, there were significant differences in Pre-CL(F), Pre-CL(E), Pre-CL(ROM), (Pre)Up-fat/muscle, (Pre)Up-fat/centrum, (Pre)Low-fat/muscle, (Pre) Low-fat/centrum, Post-CL(F), Post-CL(E), Post-CL(ROM) (P < 0.05) (Table 3).
In functional scores after conservative treatment, there were significant differences in Post-VAS, Post-NDI, Post-PCS, Post-MCS (P < 0.05) (Table 2).
Changes in X-ray imaging parameters pre- and postconservative treatment
To further determine whether cervical traction will cause the aggravation of cervical instability, we evaluated the imaging parameters pre- and post-treatment. We found that there was no significant difference in CL, T1S, C2-7 SVA, CL(F), CL(E) or CL(ROM) between all groups pre- and post-treatment (P < 0.05) (Table 4).
Changes in functional scores in each group pre- and postconservative treatment
Mild instability trend group: The mean Pre-VAS was 7.0 ± 1.5, and the mean Post-VAS was 2.9 ± 2.3 (P < 0.001); The mean Pre-NDI was 23.7 ± 7.1, and the mean Post-NDI was 10.3 ± 7.7 (P < 0.001); The mean Pre-PCS was 31.2 ± 5.3, and the mean Post-PCS was 42.2 ± 7.0 (P < 0.001); The mean Pre-MCS was 38.9 ± 8.2, and the mean Post-MCS was 46.9 ± 6.8 (P < 0.001).
Moderate instability trend group: The mean Pre-VAS was 6.8 ± 1.2, the mean Post-VAS was 3.0 ± 1.9 (P < 0.001); The mean Pre-NDI was 22.9 ± 6.7, the mean Post-NDI was 10.6 ± 6.9 (P < 0.001); The mean Pre-PCS was 32.3 ± 4.8, the mean Post-PCS was 38.7 ± 7.2 (P < 0.001); The mean Pre-MCS was 37.8 ± 8.5, the mean Post-MCS was 43.2 ± 5.8 (P = 0.001).
Severe instability trend group: The mean Pre-VAS was 7.0 ± 1.0, and the mean Post-VAS was 4.8 ± 1.7 (P < 0.001); The mean Pre-NDI was 25.0 ± 4.1, and the mean Post-NDI was 17.6 ± 5.5 (P < 0.001); The mean Pre-PCS was 30.7 ± 5.0, and the mean Post-PCS was 36.5 ± 5.7 (P < 0.001); The mean Pre-MCS was 39.2 ± 7.9, and the mean Post-MCS was 43.4 ± 8.2 (P = 0.062).
Details are described in Table 5 and Fig. 4.
Intragroup analysis results of imaging parameters and functional scores of each group pre- and postconservative treatment
The correlation between each parameter was determined using Pearson and Spearman correlation coefficients. In the mild instability trend group, Pre-VAS was negatively correlated with Pre-CL, Pre-T1S, Pre-CL(F) and Pre-CL(E). Pre-NDI was negatively correlated with Pre-CL, Pre-T1S, Pre-CL(F) and Pre-CL(E). Post-VAS was negatively correlated with Pre-CL, Pre-T1S, Pre-CL(E), Post-CL, Post-T1S and Post-CL(E). Post-NDI was negatively correlated with Pre-CL, Pre-T1S, Pre-CL(F), Pre-CL(E), Post-CL, PostT1S, Post-CL(F) and Post-CL(E). Post-MCS was positively correlated with Pre-CL, Pre-CL(F), Post-CL and Post-CL(F).
In the moderate instability trend group, the pre- and post-functional scores were consistent with the mild group in X-ray parameters and showed a significant correlation with the degree of fat infiltration. Pre-VAS was negatively correlated with (Pre) Up-muscle/centrum and (Pre) Low-muscle/centrum. Pre-NDI was negatively correlated with (Pre) Up-muscle/centrum and (Pre) Low-muscle/centrum. Post-VAS was positively correlated with (Pre) Up-fat/muscle and negatively correlated with (Pre) Up-muscle/centrum and (Pre) Low-muscle/centrum. Post-NDI was positively correlated with (Pre) Up-fat/muscle and negatively correlated with (Pre) Up-muscle/centrum and (Pre) Low-muscle/centrum.
In the severe instability trend group, Pre-VAS was negatively correlated with Pre-CL, Pre-T1S, (Pre) Up-muscle/centrum and (Pre) Low-muscle/centrum. Pre-NDI was negatively correlated with Pre-CL, Pre-T1S, (Pre) Up-muscle/centrum and (Pre) Low-muscle/centrum. Post-VAS was negatively correlated with Pre-CL and Post-CL. Post-NDI was negatively correlated with Pre-CL, (Pre) Up-muscle/centrum and Post-CL.
Details are described in Table 6.
Discussion
In the field of spinal degeneration, Meyerding has established a basic grading system for spinal spondylolisthesis, which is commonly used to determine the severity of spinal spondylolisthesis, especially in the lumbar region. Based on the degree of forward sliding of the upper vertebral body towards the lower vertebral body, the degree of spondylolisthesis is divided into five levels, and has been widely used in clinical practice18,19. Kirkaldy-Willis proposed a three-phase model for the progression of degenerative spondylolisthesis: (1) Phase of Dysfunction: This initial phase is characterized by functional abnormalities but minimal noticeable anatomical changes; (2) Phase of Instability: This phase involves further degeneration of the intervertebral disc, facet joints, and ligaments, leading to instability; (3) Phase of Restabilization: In this final phase, the body attempts to stabilize the affected segment through osteophyte formation and fibrosis of the facet joints and intervertebral disc20,21. Therefore, spinal degeneration and spinal instability are not the same concept.
Cervical instability is a manifestation of cervical degenerative changes. It refers to the excessive or abnormal activity in the horizontal direction or relative rotation under physiological load5,22. Some authors propose the concept of “clinical” or “functional” instability, which suggests that instability can exist even without visible defects in the spine's structure or excessive movement on imaging. They believe that poor trunk muscle function and inadequate motor control can contribute to abnormal intervertebral movement and pain. However, this type of instability lacks sufficient evidence to be considered a distinct clinical entity and cannot be definitively measured by any gold standard. Nevertheless, it remains a key area of interest and focus for chiropractors and manual therapists23,24. Structural spine instability is attributed to various factors, including disc degeneration, spinal fusion surgery (which can place abnormal stress on adjacent unfused segments), extensive surgical decompression or disc removal, and a history of trauma or recurring pain. Additionally, several coexisting anatomical features, such as traction spurs, facet joint hypertrophy, and osteophyte formation, have been linked to structural spine instability6,7,24. Since White et al.5 first reported the X-ray measurement method of cervical instability: (1) More than 3.5 mm horizontal displacement of one vertebra in relation to an adjacent vertebra, anteriorly or posteriorly, measured on resting lateral or flexion–extension roentgenograms of the spine; (2) More than 11 degree of rotational difference to that of either adjacent vertebra, measured on a resting lateral or flexion–extension roentgenogram. And it has been widely used in the clinical setting8. Also, it should be noted that White et al.'s measurement method includes not only dynamic imaging (flexion–extension X-rays) of the cervical spine, but also static imaging (lateral X-rays). However, most scholars believe that instability is related to dynamic environments and should be evaluated through dynamic imaging (flexion–extension X-rays)25,26. But some scholars also believe that lateral cervical X-rays also have important significance in the diagnosis of cervical instability22. In some cases, it is safer than flexion–extension X-rays22. In our study, One of the hazards we worry about is whether cervical traction will exacerbate cervical instability, therefore, in order to screen as strictly as possible and avoid adverse effects on patients, we chose the method of White et al.5. Namely, there are abnormal angles (11°) or displacements (3.5 mm) on the lateral or flexion–extension roentgenograms of the cervical spine. And the patients were divided into three groups according to the difference in horizontal displacement and abnormal angle. Considering that we cannot determine the benefits and hazards of cervical traction in patients with obvious cervical instability (horizontal displacement > 3.5 mm or abnormal angle > 11°), we excluded such patients.
The efficacy of cervical traction in individuals with cervicogenic somatic referred pain has been studied and reported by an increasing number of scholars14,15. Jellad A’s research14 included analgesics and found that manual or mechanical cervical traction appears to be a major contribution to the rehabilitation of cervical radiculopathy patients. A recent systematic review15 observed a statistically significant enhancement in both pain levels and the cervical disability index among participants in the manual therapy intervention group. This improvement was consistent across various protocols and manual therapy techniques employed, including cervical manipulations, thoracic manipulations, cervical mobilization towards the opening of the intervertebral foramen, cervical traction, and neural mobilizations. However, some scholars hold different views. Investigations by Young27 revealed that incorporating mechanical cervical traction into a comprehensive treatment regimen involving manual therapy and exercise does not result in any notable extra advantages in terms of pain relief, functional improvement, or reduction in disability for patients with cervical radiculopathy. Through clinical practice and observation, we found that different traction efficiencies may be related to the degree of cervical instability and cervical muscle degeneration, so we designed this study. In our study, we found that the therapeutic efficacy rates of the mild, moderate and severe instability trend groups were 85.0%, 69.6% and 44.4%, respectively (P = 0.002), and the improvement in functional scores in the mild and moderate groups was also significantly better than that in the severe group. Therefore, we found that the more serious the trend of cervical instability, the more severe the degree of cervical muscle degeneration, which means the less effective conservative treatment was, that may be a reason for the difference in the efficacy rate of cervical traction research by various scholars.
However, in clinical practice, there have been few reports on whether CSR patients with cervical instability will benefit from cervical traction. One of the hazards we worry about is whether cervical traction will exacerbate cervical instability. Therefore, based on the criteria for cervical instability, we included patients without cervical instability, but divided them into three groups based on the horizontal displacement and abnormal angle measured on their cervical X-rays. The closer the patients were to the diagnostic criteria for cervical instability, the more likely they were to have cervical instability. We used this to determine whether patients with a greater trend of cervical instability would have a harder time benefiting from cervical traction. Consequently, for the three groups we studied, we measured the changes in cervical sagittal parameters and instability indices pre- and post-treatment. We found that for all groups, cervical sagittal parameters and instability indices did not change significantly pre- and post-treatment. This finding suggests that cervical traction does not lead to the aggravation of cervical instability.
Cervical sagittal parameters are widely used in the evaluation of cervical spondylotic, cervical surgery and cervical functional status28,29,30,31. In our study, we found that regardless of the group, the Pre-CL had a significant correlation with pre- and post-functional scores. The larger the Pre-CL was, the better the curative effect was, which is consistent with a previous study by Lin et al.1. Current research suggests that abnormal expansion of cervical mobility may indicate the presence of cervical instability32. CL (ROM) is also widely used in clinical practice for evaluating cervical range of motion33. In our study, we found that in CSR patients, the more pronounced the trend of cervical instability was, the larger CL (F), CL (E), and CL (ROM) were. This is consistent with the reports of the aforementioned scholars, further confirming the significance of using cervical range of motion to indicate cervical instability. Recently, More and more scholars are paying attention to the association between cervical instability and cervical spinal stenosis34. Increased intervertebral displacement caused by cervical instability, as well as cervical spondylolisthesis, may exacerbate symptoms of cervical spinal stenosis. In our study, we found that there was no significant differences in AP, SDD and Pavlov ratio among the three groups with different trends in cervical instability. This may be because the patients we included did not have cervical instability, but were grouped according to the criteria for instability, based on whether they were closer to the diagnostic criteria for cervical instability.
In recent years, research on the degree of cervical muscle degeneration has also attracted increasing attention9,10,11,12. James et al.9 found that neck dysfunction was significantly correlated with fat infiltration in cervical muscle. Kim et al.10 discovered a correlation between the degeneration of the upper cervical extensor group and the loss of cervical lordosis, while the degeneration of the lower cervical extensor group was associated with cervical dysfunction. Our study identified significant variations in the extent of fat infiltration among distinct groups. Notably, the severe instability trend group exhibited a significantly higher degree of fat infiltration compared to the mild and moderate groups, which could contribute to the suboptimal treatment outcomes observed in the severe instability trend group.
Our research has the following limitations. First, the study’s scope is constrained by a limited number of cases, all originating from a singular center. This insufficient case pool prevents the formulation of conclusive findings. Second, our study excluded patients with obvious cervical instability, while our results showed that cervical traction did not aggravate the instability even in the severe instability trend group. Therefore, more high-quality evidence is needed before our conclusion can be extended to patients with obvious cervical instability.
Conclusion
For patients with CSR, the more serious their predisposition for cervical instability was, the more severe the degree of cervical muscle degeneration was, which means the worse the curative effect was, but cervical traction did not aggravate the potential degree of cervical instability.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Lin, T. T., Wang, Z. Y., Chen, G. & Liu, W. G. Predictive effect of cervical sagittal parameters on conservative treatment of single-segment cervical spondylotic radiculopathy. World Neurosurg. 134, e1028–e1036 (2020).
Schoenfeld, A. J. et al. Incidence and epidemiology of cervical radiculopathy in the United States military:2000 to 2009. J. Spinal Disord. Tech. 25(1), 17–22 (2012).
Yu, R. et al. Tobacco smoke-induced brain white matter myelin dysfunction: Potential co-factor roleof smoking in neurodegeneration. J. Alzheim. Dis. 50(1), 133–148 (2015).
Bono, C. M. et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 11(1), 64–72 (2011).
White, A. A., Johnson, R. M., Panjabi, M. M. & Southwick, W. O. Biomechanical analysis of clinical stability in the cervical spine. Clin. Orthop. Relat. Res. 109, 85–96 (1975).
Kuligowski, T. Prevalence of lumbar segmental instability in young individuals with the different types of lumbar disc herniation-preliminary report. Int. J. Environ. Res. Public Health 19(15), 9378 (2022).
Gopinath, P. Lumbar segmental instability: Points to ponder. J. Orthop. 12(4), 165–167 (2015).
Dion, S. et al. Criteria to screen for traumatic cervical spine instability: A consensus of chiropractic radiologists. J. Manipul. Physiol. Ther. 41(2), 156–163 (2018).
James, M. et al. The rapid and progressive degeneration of the cervical multifidus in whiplash: An MRI study of fatty infiltration. Spine 40, E694-700 (2015).
Kim, C.-Y., Lee, S.-M., Lim, S.-A. & Choi, Y.-S. Impact of fat infiltration in cervical extensor muscles on cervical lordosis and neck pain: A cross-sectional study. Clin. Orthoped. Surg. 10, 197–203 (2018).
Tamai, K. et al. The impact of cervical spinal muscle degeneration on cervical sagittal balance and spinal degenerative disorders. Clin. Spine Surg. 32, E206–E213 (2019).
Alpayci, M. et al. Decreased neck muscle strength in patients with the loss of cervical lordosis. Clin. Biomech. (Bristol, Avon) 33, 98–102 (2016).
Lin, S. et al. Does the asymmetry and extension function of the preoperative cervical paraspinal extensor predict postoperative cervical sagittal deformity in patients who undergo modified laminoplasty?. Spine J. 22(12), 1953–1963 (2022).
Jellad, A. et al. The value of intermittent cervical traction in recent cervical radiculopathy. Ann. Phys. Rehabil. Med. 52(9), 638–652 (2009).
Borrella-Andrés, S. et al. Manual therapy as a management of cervical radiculopathy: A systematic review. Biomed. Res. Int. 2021, 9936981 (2021).
Young, I. A., Cleland, J. A., Michener, L. A. & Brown, C. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am. J. Phys. Med. Rehabil. 89, 831–839 (2010).
MacDowall, A. et al. Posterior foraminotomy versus anterior decompression and fusion in patients with cervical degenerative disc disease with radiculopathy: Up to 5 years of outcome from the national Swedish Spine Register. J. Neurosurg. Spine 32, 344–352 (2020).
Koslosky, E. & Gendelberg, D. Classification in brief: The meyerding classification system of spondylolisthesis. Clin. Orthop. Relat. Res. 478(5), 1125–1130 (2020).
Polly, D. W. Jr. et al. Management of high-grade dysplastic spondylolisthesis. Neurosurg. Clin. N. Am. 34(4), 567–572 (2023).
Yong-Hing, K. & Kirkaldy-Willis, W. H. The pathophysiology of degenerative disease of the lumbar spine. Orthop. Clin. N. Am. 14(3), 491–504 (1983).
Saremi, A. et al. Evolution of lumbar degenerative spondylolisthesis with key radiographic features. Spine J. 24(6), 989–1000 (2024).
Simon, H. et al. Erect radiographs to assess clinical instability in patients with blunt cervical spine trauma. J. Bone Joint Surg. Am. 94(23), e1741–e1744 (2012).
Ferrari, S. et al. A literature review of clinical tests for lumbar instability in low back pain: Validity and applicability in clinical practice. Chiropr. Man Therap. 8(23), 14 (2015).
Alqarni, A. M., Schneiders, A. G. & Hendrick, P. A. Clinical tests to diagnose lumbar segmental instability: A systematic review. J. Orthop. Sports Phys. Ther. 41(3), 130–140 (2011).
Zheng, H. L. et al. Anterior cervical discectomy and fusion to treat cervical instability with vertigo and dizziness: A single center, retrospective, observational study. Front. Surg. 6(9), 1047504 (2023).
Obo, T. et al. Segmental cervical instability does not drive the loss of cervical lordosis after laminoplasty in patients with cervical spondylotic myelopathy. Spine J. 22(11), 1837–1847 (2022).
Young, I. A. et al. Manual therapy, exercise, and traction for patients with cervical radiculopathy: A randomized clinical trial. Phys. Ther. 89(7), 632–642 (2009).
Nicholson, K. J. et al. Cervical sagittal range of motion as a predictor of symptom severity in cervical spondylotic myelopathy. Spine (Phila Pa 1976) 43, 883–889 (2018).
Tang, J. A. et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 71, 662–669 (2012).
Iyer, S. et al. Impact of cervical sagittal alignment parameters on neck disability. Spine (Phila Pa 1976) 41, 371–377 (2016).
Moustafa, I. M. et al. Does rehabilitation of cervical lordosis influence sagittal cervical spine flexion extension kinematics in cervical spondylotic radiculopathy subjects?. J. Back Musculoskelet. Rehabil. 30(4), 937–941 (2017).
Tan, L. A., Riew, K. D. & Traynelis, V. C. Cervical spine deformity-part 1: Biomechanics, radiographic parameters, and classification. Neurosurgery. 81(2), 197–203 (2017).
Liu, C. X. et al. The preservation of cervical flexibility helps maintain cervical sagittal alignment after laminoplasty. Spine J. S1529–9430(24), 00301–00302 (2024).
Abudouaini, H. et al. A possible correlation between facet orientation and development of degenerative cervical spinal stenosis. BMC Musculoskelet. Disord. 25(1), 181 (2024).
Author information
Authors and Affiliations
Contributions
TL:Lead the writing of the original draft of the project and responsible for overall project management, including resource allocation and progress tracking. ZS: Offer innovative suggestions and strategic guidance during the conceptualization phase and contribute to the initial drafting of project content. ZX: Responsible for collecting and organizing relevant data to provide reliable research support. RW, YZ and DC: Assist in developing formal analysis methods and standards to ensure accuracy and completeness. LZ and ZW: Lead the investigation phase, ensuring the project is based on thorough facts and information and responsible for reviewing and editing written content. WL: Lead the overall conceptualization of the project, defining its core ideas and goals, provide professional guidance and support in methodology to ensure the team works according to specified methods and participate in the review and editing process, ensuring the quality and coherence of the final written material. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, T., Shangguan, Z., Xiao, Z. et al. Whether the potential degree of cervical instability and cervical muscle degeneration in patients with cervical spondylosis radicular affect the efficacy of cervical traction. Sci Rep 14, 20467 (2024). https://doi.org/10.1038/s41598-024-71429-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71429-9
- Springer Nature Limited