Abstract
This study compared the thickness of each intraretinal layer in patients with neurofibromatosis 1 (NF1) and controls to analyze the association between intraretinal layer thickness and visual function. The macular spectral-domain optical coherence tomography volumetric dataset obtained from 68 eyes (25 adult eyes, 43 pediatric eyes) with NF1 without optic glioma and 143 control eyes (100 adult eyes, 43 pediatric eyes) was used for image auto-segmentation. The intraretinal layers segmented from the volumetric data included the macular retinal nerve fiber layer (RNFL), ganglion cell-inner plexiform layer (GCIPL), inner nuclear layer, outer plexiform layer, outer nuclear layer, and photoreceptor layer. Cases and controls were compared after adjusting for age, sex, refractive error, and binocular use. The association between retinal layer thickness and visual acuity was also analyzed. The GCIPL was significantly thinner in both adult and pediatric patients with NF1 compared with healthy controls. Average RNFL and GCIPL thicknesses were associated with visual acuity in adult patients with NF1. In pediatric patients, average GCIPL thickness was associated with visual acuity. These results suggest that changes in the inner retinal layer could be a biomarker of the structural and functional status of patients with NF1.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Neurofibromatosis type 1 (NF1) is an autosomal dominant disorder caused by mutations within the NF1 gene on chromosome 17q11.21. NF1 is a multisystemic disease with cutaneous, ocular, and neurological manifestations with an estimated incidence of 1 in 3000 births1. Common ocular features of NF1 include Lisch nodules and optic gliomas (OPG)2. Optical coherence tomography (OCT) is a non-invasive diagnostic technology that displays cross-sectional images of the retina and optic nerve. Several studies on OCT in patients with NF1 have revealed decreased peripapillary retinal nerve fiber layer (RNFL) thickness3,4,5 and retinal microvascular abnormalities6. OCT segmentation analysis demonstrates the macular structures of each retinal layer separately, including the RNFL and ganglion cell layer, thereby enabling the evaluation of the extent of axonal loss in many neurodegenerative diseases7. Macular layer thickness measured using OCT varies with age and refractive errors, necessitating adjustment for confounders8,9. However, studies evaluating retinal layer segmentation using spectral-domain OCT in patients with NF1 are limited, particularly among the pediatric population10. A reduction in RNFL and ganglion cell-inner plexiform layer (GCIPL) thickness has been reported in these patients compared to healthy controls10.
In this study, we compared whole retinal layer thicknesses in both pediatric and adult patients with NF1 to those in healthy controls using OCT segmentation analysis and investigated the associations between retinal layer parameters and functional parameters after adjusting for age, sex, refractive error, and binocular use.
Results
A total of 25 eyes from 14 adult patients with NF1, 100 eyes from 100 adult controls, 43 eyes from 23 pediatric patients with NF1, and 43 eyes from 43 pediatric controls were analyzed in this study. The demographic and clinical characteristics of the patients with NF1 and the controls are presented in Table 1.
The thickness of each retinal layer in all patients and controls is shown in Table 2. The GCIPL in all patients with NF1 was thinner when compared with healthy controls after adjusting for age, sex, spherical equivalent (SE), and binocular data use (estimates [standard error], − 6.061 [1.757], p < 0.001). There were no significant differences in the thickness of RNFL, inner nuclear layer (INL), outer plexiform layer (OPL), outer nuclear layer (ONL), or photoreceptor layer (PRL) between the two groups.
Patients with NF1 were divided into two subgroups (children and adults) to compare retinal layer thickness. Tables 3 and 4 present the measurements of the thickness of each retinal layer in adult and pediatric patients with NF1 compared to controls. Significant differences were observed in GCIPL thickness between patients with NF1 and controls after adjusting for age, sex, SE, and binocular use in both adults (88.06 ± 10.14 μm in NF1 vs. 93.24 ± 6.57 μm in controls, p = 0.023) and pediatric groups (88.03 ± 11.21 μm in NF1 vs. 93.20 ± 5.87 μm in controls, p = 0.018).
Table 5 presents the association between retinal layer thickness and best-corrected visual acuity (BCVA). BCVA was associated with RNFL thickness (estimates [standard error], − 0.530 [0.236], p = 0.025) and GCIPL (− 0.226 [0.114], p = 0.048) in adult patients with NF1, while in pediatric patients with NF1, only GCIPL was associated with BCVA (− 0.124 [0.058], p = 0.032) (Fig. 2).
Table 6 demonstrates the significant association between GCIPL thickness and visual field sensitivity indices, including the mean deviation (MD), visual field index (VFI), and central mean deviation (CMD) across all patient groups: overall, adult patients, and pediatric patients. Thinner GCIPL layers were significantly correlated with a worse visual field sensitivity in each group.
Discussion
Earlier studies have mainly focused on patients with NF1 combined with OPG, reporting decreased peripapillary RNFL thickness in patients with NF1-associated OPG4,5,11. Chang et al.5 and Topcu-Yilmaz et al.11 reported decreased peripapillary RNFL thickness in NF1 patients with OPG in studies involving 15 and 27 NF1 patients with or without OPG, respectively. Avery et al. also analyzed peripapillary RNFL thickness in 89 eyes with OPGs, including 61 eyes with NF14, and demonstrated that most children with OPG and decreased RNFL thickness had deteriorated visual function, suggesting that OCT is a rapid, non-invasive, and objective quantitative measure of visual pathway integrity in these patients4. Chang et al. also reported that patients with OPGs had a thinner total macular thickness and peripapillary RNFL than age-matched controls and patients with NF1 without OPGs5. In addition, Topcu-Yilmaz et al. reported that the macular volume significantly decreased only in patients with OPG having decreased visual acuity11. Peripapillary RNFL thinning and reduced total macular volume in patients with OPG may be primarily caused by the retrograde degeneration of the optic nerve due to OPG itself4,5,11.
Regarding patients with NF1 without OPGs, Chang et al. reported that the peripapillary RNFL thickness and macular volume in six patients with NF1 (ages 7, 8, 9, 13, 19, and 20 years) without OPGs were equivalent to the controls5. Abdolrahimzadeh et al. reported that the peripapillary RNFL, macular RNFL, and GCIPL were decreased in 17 adult patients with NF1 without OPGs compared to the healthy controls12. In addition, a correlation between peripapillary RNFL and GCIPL thicknesses in patients with NF1 was demonstrated in their study12. They suggested that thinning of the macular RNFL, peripapillary RNFL, and GCIPL in adulthood was due to the chronic progression of the disease, as other manifestations of NF1, such as cutaneous neurofibromas, Lisch nodules, and choroidal nodules are age-dependent13,14,15.
In the present study, we also confirmed that the macular GCIPL decreased in adult patients with NF1, thereby supporting the outcomes of a previous report12, and revealed that the macular GCIPL also decreased in children with NF1 compared with healthy controls. The different OCT findings in children with NF1 between the studies may be attributed to differences in the study settings, such as the size of the study population, demographic characteristics of the subjects, and phenotypic expression of the diseases. In this study, the mean thickness of macular RNFL and GCIPL was 23.99 ± 4.09 μm and 88.06 ± 10.14 μm, respectively, in adult patients with NF1; while their values were 21.25 ± 3.58 μm and 88.03 ± 11.21 μm, respectively, in pediatric patients with NF1. Because the loss of retinal neurons is a part of the normal aging process9,16,17,18,19 and data were collected cross-sectionally rather than longitudinally, a direct comparison between adult and pediatric patients was impossible in this study. Further longitudinal studies on normal aging changes in retinal microstructures are needed to clarify the nature of pathological changes over time.
Regarding the mechanism of neuronal loss in NF1 eyes, Abdolrahimzadeh et al. explained that this may be caused by disease progression, which is characterized by the aberrant proliferation of multiple tissues of neural crest origin20. They also raised the possibility that choroidal alterations due to characteristic nodules21,22,23,24 may lead to choroidal and retinal thinning12. It is well known that the majority of patients with NF1 have diverse neuronal abnormalities that primarily affect the central nervous system, such as difficulties with attention, executive function, language, visual perception, and learning25,26,27,28,29,30. Although the precise mechanisms underlying neuronal abnormalities remain largely unknown, several experimental studies have suggested that the underlying pathophysiology is of genetic origin. In vitro and in vivo studies on neuronal and glial differentiation from neural stem cells demonstrated that Nf1 − / − neurons exhibited decreased neurite lengths, thereby resulting in reduced secondary somatosensory cortical thickness31. In addition, Cui et al. reported that mice heterozygous for an inactivating Nf1 mutation in synapsin-I-expressing neurons in the brain exhibited learning and memory deficits32. Hegedus et al. also showed that Nf1 + / − hippocampal and retinal ganglion neurons had reduced neurite lengths, growth cone areas, and survival33.
Previous studies have suggested that changes in the GCIPL thickness can be attributed to both neuronal degeneration and synaptic remodeling. Synaptic remodeling is a dynamic process that occurs in response to various stimuli and can lead to alterations in the synaptic architecture without necessarily causing neuronal cell loss. Marc et al. described neural remodeling in retinal degeneration, indicating that synaptic reorganization can contribute to the changes observed in the retinal layers34. Additionally, Al-Louzi et al. have reported retrograde trans-synaptic degeneration in multiple sclerosis, resulting in GCIPL thinning35. Therefore, the observed reduction in GCIPL thickness in patients with NF1 may reflect a combination of synaptic remodeling and neurodegenerative processes.
The present study demonstrated a significant positive association between the intraretinal layer thickness and visual acuity in patients with NF1 without OPG. Additionally, an association between the RNFL, GCIPL, and visual acuity in adult patients has been demonstrated. Adult patients with NF1 and a thicker RNFL and GCIPL showed better visual acuity. In pediatric patients, the GCIPL was significantly associated with visual acuity. Pediatric patients with NF1 and a thicker GCIPL showed better visual acuity (Fig. 2C). These results suggest that changes in the inner retinal layer can be a good biomarker of both the structural and visual functional status in NF1.
Previous studies have demonstrated a significant correlation between GCIPL thickness and visual acuity in various ocular conditions, including severe glaucoma36 and early stages of diabetic retinopathy37. Li et al.37 explained that the loss of retinal ganglion cells results in a decrease in GCIPL thickness, which subsequently impairs the transmission of visual information. Our findings align with this pattern, as a decrease in the GCIPL thickness in patients with NF1 was found to be significantly correlated with visual acuity.
In addition, our analysis revealed a significant correlation between GCIPL thickness and loss of visual field sensitivity in both adult and pediatric patients with NF1. The significant correlation observed between GCIPL thickness and visual field sensitivity supports the use of GCIPL thickness as a reliable biomarker and functional parameter for neurofibromatosis.
Our study has several limitations that should be considered when interpreting the data. Firstly, we used a retrospective cross-sectional design, which limited our ability to reveal the temporal aspects of changes in OCT parameters. Secondly, the dataset was relatively small. A larger longitudinal cohort study is needed to observe serial changes in the intraretinal layer thickness. Thirdly, since not all subjects underwent annual repeated imaging, there is a possibility that early-stage OPGs, which are difficult to detect on MRI, may have been present in the study population. Lastly, as this was an exploratory study and a primary analysis was not planned before the study, all results should be read as descriptive and interpreted with caution38.
In conclusion, this study revealed the inner retinal layer degeneration in both pediatric and adult patients with NF1. Both adult and pediatric patients with NF1 exhibited GCIPL atrophy. Thinning of the inner retinal layer was associated with visual function. These results suggest that retinal layer analysis using OCT may be a useful tool for reflecting both the structural and functional statuses of patients with NF1. We hope that future studies will reveal the temporal aspects and precise mechanisms of retinal neurodegeneration in patients with NF1.
Methods
Study participants
This retrospective study included 14 adult patients (25 eyes), 23 pediatric patients (43 eyes) with NF1, 100 adult controls (100 eyes), and 43 pediatric controls (43 eyes). Patients and controls were enrolled from the Neuro-ophthalmology Department of Samsung Medical Center between March 2012 and February 2020. The study adhered to the principles of the Declaration of Helsinki. The research protocol (No. 2021-11-139) was approved by the Institutional Review Board of the Samsung Medical Center. The requirement for informed consent was waived by the Institutional Review Board of the Samsung Medical Center for this retrospective study. For all included patients, the diagnosis of NF1 was based on the National Institutes of Health criteria39. The mean age at OCT examination was 40.4 ± 17.9 years for adult patients and 12.1 ± 4.7 years for pediatric patients. Age-matched controls were recruited from among patients who underwent routine eye examinations at the same department. The control group consisted of 6–18-year-old and 19–78-year-old healthy volunteers. Some controls participated in other studies conducted in the same department.
Only healthy controls with normal visual acuity, normal optic disc, and no history of ocular or neurological diseases were enrolled. Patients and controls with other ophthalmic diseases (age-related macular degeneration, epiretinal membrane, retinal artery/vein occlusion, diabetic retinopathy, optic neuritis, glaucoma, and other optic neuropathies, including OPG), previous retinal surgery, and systemic or neurological diseases that could affect the OCT results, except NF1 in the patient group, were excluded from the study.
Ophthalmic examinations
The BCVA in the logarithm of the minimum angle of resolution (logMAR) and the SE of manifest refraction were measured in all patients and controls. A thorough ophthalmological examination, including anterior segment examination, fundus photography, and spectral-domain OCT (SD-OCT; Spectralis, Heidelberg Engineering, Heidelberg, Germany), was also performed. Additionally, visual field tests were conducted in several patients.
OCT analysis and segmentation
Twenty-five raster B-scans covering an area of 20° × 15° were obtained using the Spectralis OCT. Each B-scan consisted of 512 A-lines, 6.0 mm long, and 240 μm apart. Automatic real-time eye tracking (TruTrack Active Eye Tracking; Heidelberg Engineering) was used to improve the quality and accuracy of segmentation. All OCT images met the OSCAR-IB quality control criteria for retinal OCT scans.
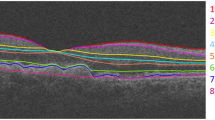
The retinal layers were automatically segmented into six retinal layers using Spectralis software based on a validated algorithm40: RNFL, GCIPL, INL, OPL, ONL, and PRL (Fig. 1). Manual corrections were made if necessary. The average thickness of each retinal layer within the 1-, 3-, and 6 mm zones based on the Early Treatment Diabetic Retinopathy was calculated using Spectralis mapping software (Fig. 2). In this study, the thickness of each retina was compared using the average value of the four quadrants of the 1–3 mm subfields. Two independent graders (M.J.K. and S.Y.H) evaluated image quality. Any errors in automated segmentation were manually corrected, as previously described by Oberwahrenbrock et al.41.
(A) Relationship between retinal nerve fiber layer (RNFL) thickness and best-corrected visual acuity (BCVA) in adult patients with NF1, showing that BCVA was significantly associated with RNFL thickness (p = 0.025). (B) Relationship between ganglion cell-inner plexiform layer (GCIPL) thickness and BCVA in adult patients with NF1, indicating a significant association between BCVA and GCIPL thickness (p = 0.048). (C) Relationship between GCIPL thickness and BCVA in pediatric patients with NF1, demonstrating a significant association between BCVA and GCIPL thickness (p = 0.032).
Visual field testing
Visual field testing was conducted on 14 eyes from adult patients and 34 eyes from pediatric patients. The VF assessment utilized standard automated perimetry with the 30–2 Swedish Interactive Thresholding Algorithm (SITA) standard protocol, performed using the Humphrey 740 Visual Field Analyzer (Carl Zeiss Meditec, Inc., Dublin, CA, U.S.A). To ensure reliability, the criteria included a false-positive or false-negative rate of ≤ 30%, and a fixation loss of < 20%. The MD and VFI values were used in the analysis. Additionally, CMD was calculated in both decibels (dB) and 1/Lambert (1/L) units following the method used by Monteiro et al.42
Statistical analysis
Statistical analyses were performed using R software version 4.2.1 (R Project for Statistical Computing) and SPSS software version 25.0 (SPSS Inc., Chicago, IL, USA). Continuous variables, such as age, were expressed as the mean ± standard deviation, and categorical variables, such as sex, were expressed as numbers (%). The Mann–Whitney U test was performed to compare continuous variables between the patient and healthy control groups. The chi-square test was used to compare categorical variables between groups. A p-value below 0.05 was considered statistically significant.
Because both eyes of patients with NF1 were used for the analysis, a generalized estimating equation was used to compare the intraretinal layer thickness between the two groups after adjusting for age, sex, and SE. We divided all patients with NF1 into two groups (adult and pediatric groups) and performed a subgroup analysis. Bonferroni correction was applied to the p-values by multiplying the uncorrected p-values by two in the subgroup analysis. In the NF1 group, a generalized estimating equation model was used to identify the correlation between each intraretinal layer thickness and visual acuity, as well as the correlation between intraretinal layer thickness and visual field sensitivity.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Samsung Medical Center.
References
Gutmann, D. H. et al. Neurofibromatosis type 1. Nat. Rev. Dis. Prim. 3, 17004. https://doi.org/10.1038/nrdp.2017.4 (2017).
Kinori, M., Hodgson, N. & Zeid, J. L. Ophthalmic manifestations in neurofibromatosis type 1. Surv. Ophthalmol. 63, 518–533. https://doi.org/10.1016/j.survophthal.2017.10.007 (2018).
Parrozzani, R. et al. Optical coherence tomography in the diagnosis of optic pathway gliomas. Investig. Ophthalmol. Vis. Sci. 54, 8112–8118. https://doi.org/10.1167/iovs.13-13093 (2013).
Avery, R. A. et al. Retinal nerve fiber layer thickness in children with optic pathway gliomas. Am. J. Ophthalmol. 151, 542-549.e542. https://doi.org/10.1016/j.ajo.2010.08.046 (2011).
Chang, L. et al. Optical coherence tomography in the evaluation of neurofibromatosis type-1 subjects with optic pathway gliomas. J. AAPOS 14, 511–517. https://doi.org/10.1016/j.jaapos.2010.08.014 (2010).
Moramarco, A. et al. Retinal microvascular abnormalities in neurofibromatosis type 1. Br. J. Ophthalmol. 103, 1590–1594. https://doi.org/10.1136/bjophthalmol-2018-313002 (2019).
Satue, M. et al. Optical coherence tomography as a biomarker for diagnosis, progression, and prognosis of neurodegenerative diseases. J. Ophthalmol. 2016, 8503859. https://doi.org/10.1155/2016/8503859 (2016).
Duan, X. R. et al. Normal macular thickness measurements using optical coherence tomography in healthy eyes of adult Chinese persons: The Handan Eye Study. Ophthalmology 117, 1585–1594. https://doi.org/10.1016/j.ophtha.2009.12.036 (2010).
Ooto, S. et al. Effects of age, sex, and axial length on the three-dimensional profile of normal macular layer structures. Investig. Ophthalmol. Vis. Sci. 52, 8769–8779. https://doi.org/10.1167/iovs.11-8388 (2011).
Abdolrahimzadeh, S. et al. Spectral domain optical coherence tomography evidence of retinal nerve fiber layer and ganglion cell loss in adult patients with neurofibromatosis Type 1. Retina 36, 75–81. https://doi.org/10.1097/iae.0000000000000650 (2016).
Topcu-Yilmaz, P., Kasim, B. & Kiratli, H. Investigation of retinal nerve fiber layer thickness in patients with neurofibromatosis-1. Jpn. J. Ophthalmol. 58, 172–176. https://doi.org/10.1007/s10384-014-0308-6 (2014).
Abdolrahimzadeh, B., Piraino, D. C., Albanese, G., Cruciani, F. & Rahimi, S. Neurofibromatosis: An update of ophthalmic characteristics and applications of optical coherence tomography. Clin. Ophthalmol. 10, 851–860. https://doi.org/10.2147/opth.s102830 (2016).
Schnur, R. E. Type I neurofibromatosis: A geno-oculo-dermatologic update. Curr. Opin. Ophthalmol. 23, 364–372. https://doi.org/10.1097/ICU.0b013e3283570127 (2012).
Richetta, A. et al. Lisch nodules of the iris in neurofibromatosis type 1. J. Eur. Acad. Dermatol. Venereol. 18, 342–344. https://doi.org/10.1111/j.1468-3083.2004.00915.x (2004).
Makino, S., Tampo, H., Arai, Y. & Obata, H. Correlations between choroidal abnormalities, Lisch nodules, and age in patients with neurofibromatosis type 1. Clin. Ophthalmol. 8, 165–168. https://doi.org/10.2147/opth.s56327 (2014).
Parikh, R. S. et al. Normal age-related decay of retinal nerve fiber layer thickness. Ophthalmology 114, 921–926. https://doi.org/10.1016/j.ophtha.2007.01.023 (2007).
Dolman, C. L., McCormick, A. Q. & Drance, S. M. Aging of the optic nerve. Arch. Ophthalmol. 98, 2053–2058. https://doi.org/10.1001/archopht.1980.01020040905024 (1980).
Balazsi, A. G., Rootman, J., Drance, S. M., Schulzer, M. & Douglas, G. R. The effect of age on the nerve fiber population of the human optic nerve. Am. J. Ophthalmol. 97, 760–766. https://doi.org/10.1016/0002-9394(84)90509-9 (1984).
Repka, M. X. & Quigley, H. A. The effect of age on normal human optic nerve fiber number and diameter. Ophthalmology 96, 26–32. https://doi.org/10.1016/s0161-6420(89)32928-9 (1989).
Kissel, P., André, J. M. & Jacquier, A. The Neurocristopathies 223–232 (Masson, 1981).
Abdolrahimzadeh, S. et al. Morphologic and vasculature features of the choroid and associated choroid-retinal thickness alterations in neurofibromatosis type 1. Br. J. Ophthalmol. 99, 789–793. https://doi.org/10.1136/bjophthalmol-2014-306062 (2015).
Viola, F. et al. Choroidal abnormalities detected by near-infrared reflectance imaging as a new diagnostic criterion for neurofibromatosis 1. Ophthalmology 119, 369–375. https://doi.org/10.1016/j.ophtha.2011.07.046 (2012).
Rescaldani, C., Nicolini, P., Fatigati, G. & Bottoni, F. G. Clinical application of digital indocyanine green angiography in choroidal neurofibromatosis. Ophthalmologica 212, 99–104. https://doi.org/10.1159/000027287 (1998).
Ayata, A., Unal, M., Ersanli, D. & Tatlipinar, S. Near infrared fluorescence and OCT features of choroidal abnormalities in type 1 neurofibromatosis. Clin. Exp. Ophthalmol. 36, 390–392. https://doi.org/10.1111/j.1442-9071.2008.001742.x (2008).
Ferner, R. E. The neurofibromatoses. Pract. Neurol. 10, 82–93. https://doi.org/10.1136/jnnp.2010.206532 (2010).
Hyman, S. L., Arthur Shores, E. & North, K. N. Learning disabilities in children with neurofibromatosis type 1: Subtypes, cognitive profile, and attention-deficit-hyperactivity disorder. Dev. Med. Child Neurol. 48, 973–977. https://doi.org/10.1017/s0012162206002131 (2006).
Hyman, S. L., Shores, A. & North, K. N. The nature and frequency of cognitive deficits in children with neurofibromatosis type 1. Neurology 65, 1037–1044. https://doi.org/10.1212/01.wnl.0000179303.72345.ce (2005).
Mautner, V. F., Kluwe, L., Thakker, S. D. & Leark, R. A. Treatment of ADHD in neurofibromatosis type 1. Dev. Med. Child Neurol. 44, 164–170. https://doi.org/10.1017/s0012162201001876 (2002).
Eliason, M. J. Neurofibromatosis: Implications for learning and behavior. J. Dev. Behav. Pediatr. 7, 175–179 (1986).
Ozonoff, S. Cognitive impairment in neurofibromatosis type 1. Am. J. Med. Genet. 89, 45–52 (1999).
Hegedus, B. et al. Neurofibromatosis-1 regulates neuronal and glial cell differentiation from neuroglial progenitors in vivo by both cAMP- and Ras-dependent mechanisms. Cell Stem Cell 1, 443–457. https://doi.org/10.1016/j.stem.2007.07.008 (2007).
Cui, Y. et al. Neurofibromin regulation of ERK signaling modulates GABA release and learning. Cell 135, 549–560. https://doi.org/10.1016/j.cell.2008.09.060 (2008).
Brown, J. A., Gianino, S. M. & Gutmann, D. H. Defective cAMP generation underlies the sensitivity of CNS neurons to neurofibromatosis-1 heterozygosity. J. Neurosci. 30, 5579–5589. https://doi.org/10.1523/jneurosci.3994-09.2010 (2010).
Marc, R. E., Jones, B. W., Watt, C. B. & Strettoi, E. Neural remodeling in retinal degeneration. Prog. Retin. Eye Res. 22, 607–655. https://doi.org/10.1016/s1350-9462(03)00039-9 (2003).
Al-Louzi, O., Button, J., Newsome, S. D., Calabresi, P. A. & Saidha, S. Retrograde trans-synaptic visual pathway degeneration in multiple sclerosis: A case series. Mult. Scler. 23, 1035–1039. https://doi.org/10.1177/1352458516679035 (2017).
Aksoy, N. O., Cakir, B., Dogan, E. & Alagoz, G. CORRELATIONS between functional and structural tests measured by spectral domain optical coherence tomography in severe glaucoma. Semin. Ophthalmol. 34, 446–450. https://doi.org/10.1080/08820538.2019.1648688 (2019).
Li, J. et al. Visual acuity is correlated with ischemia and neurodegeneration in patients with early stages of diabetic retinopathy. Eye Vis. (Lond.) 8, 38. https://doi.org/10.1186/s40662-021-00260-4 (2021).
Bender, R. & Lange, S. Adjusting for multiple testing–when and how?. J. Clin. Epidemiol. 54, 343–349. https://doi.org/10.1016/s0895-4356(00)00314-0 (2001).
Neurofibromatosis. Conference statement. National Institutes of Health Consensus Development Conference. Arch. Neurol. 45, 575–578 (1988).
Lang, A. et al. Retinal layer segmentation of macular OCT images using boundary classification. Biomed. Opt. Express 4, 1133–1152. https://doi.org/10.1364/BOE.4.001133 (2013).
Oberwahrenbrock, T. et al. Multicenter reliability of semiautomatic retinal layer segmentation using OCT. Neurol. Neuroimmunol. Neuroinflamm. 5, e449. https://doi.org/10.1212/nxi.0000000000000449 (2018).
Monteiro, M. L., Cunha, L. P., Costa-Cunha, L. V., Maia, O. O. Jr. & Oyamada, M. K. Relationship between optical coherence tomography, pattern electroretinogram and automated perimetry in eyes with temporal hemianopia from chiasmal compression. Investig. Ophthalmol. Vis. Sci. 50, 3535–3541. https://doi.org/10.1167/iovs.08-3093 (2009).
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (RS-2024-00341030) to Kyung-Ah Park, and the Basic Science Research Program through the NRF funded by the Ministry of Science and ICT (NTX 121267) to Sei Yeul Oh.
Author information
Authors and Affiliations
Contributions
K.A.P designed and conducted the study. S.G.L, S.Y.H, and M.J.K collected the data. S.Y.H and M.J.K managed the study, analyzed and interpreted the data, and drafted the manuscript. K.A.P and S.Y.O reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Han, S.Y., Kim, MJ., Lim, S.G. et al. Inner retinal layer thickness alterations in adult and pediatric patients with neurofibromatosis 1. Sci Rep 14, 20829 (2024). https://doi.org/10.1038/s41598-024-71832-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71832-2
- Springer Nature Limited