Abstract
Tumor hypoxia is the major hindrance behind cancer chemotherapy and the foremost reason for the less effectiveness of most anticancer drugs. We herein inquire into the mechanistic part and therapeutic efficacy of our previously reported compound, aqua-(2-formylbenzoato) triphenyltin (IV) (abbreviated as OTC), in a hypoxic solid tumor-bearing mouse model (BALB/c). In addition to solid tumors, we investigated the therapeutic potential of OTC in intraperitoneal tumor and in in vitro system. Following treatment, mitochondrial dynamics, tumor load regression, survival analysis and histopathological parameters were analyzed. Furthermore, the differential expression levels of cleaved PARP-1, Hif-1α, VEGF and apoptotic genes such as Bax, Bcl-2, p53, and caspase 3 at the mRNA and protein levels were assessed. Our findings demonstrate that OTC significantly induces tumor regression and increased survivability by down regulating the expression of the hypoxia-associated genes Hif-1α and VEGF while elevating the levels of cleaved PARP-1 and p53. In contrast, the commercially available drug doxorubicin was found less effective and failed to respond in the tumor microenvironment. Furthermore, increased mitochondrial aggregation and membrane permeability and activation of Bax, caspase 3 and caspase-9 and release of Cytochrome-c from the mitochondrial membrane at RNA level confirms the mitochondrial pathway of apoptosis. Therefore, our present findings reveal that newly synthesized OTC potentially induces apoptosis and could be a promising compound against the tumor microenvironment.
Similar content being viewed by others
Introduction
Cancer remains a cogent cause of morbidity and mortality worldwide. Tumor hypoxia refers to the imbalance between oxygen supply and consumption in tissue or cells is one of the important contributing factors to this condition. Malignant solid tumors are considered to be responsible for the majority of cancer cases that arise from various genetic abnormalities in cancerous and non-cancerous cells within the tumor microenvironment. Hence, the malignant tumor emergence and progression are significantly influenced by tumor microenvironment (TME), thereby highlighting its significance as a cancer hotspot1,2. However, hypoxic features of the TME are often seen, particularly in solid tumors, owing to the effect of tumor cells and abnormal vasculature. A solid malignant tumors hypoxic zones form when there is a disparity between the oxygen supply and demand. Typically, the oxygen pressure in these regions falls to a range between 0 and 20 mm Hg3. Several intricate intracellular signaling pathways are activated in response to hypoxia. One of them is the hypoxia-inducible factor (Hif) pathway. Hif-1 protein is overexpressed in most of the solid and malignant tumors when compared to normal tissues4. These include breast, gastric, colon, lung, pancreatic, ovarian, prostate, and renal carcinomas5,6,7. Increased patient mortality has been associated with Hif-1α overexpression in several cancer types, which may be brought on by intratumoral hypoxia and genetic alterations. Tumor cells adapt itself to reduce oxygen level by activating genetic processes which were involved in uptake and utilization of glucose, formation of new blood vessels, proliferation and cell death5. This adaptive response is governed by hypoxia-inducible transcription factors (HIFs), mainly Hif-1α. Hif-1α is a heterodimeric protein with two subunits, Hif-1α and Hif-1β8. Hif-1α promotes angiogenesis by increasing the synthesis of vascular endothelial growth factor (VEGF) and several other angiogenic factors, including placenta-like growth factor (PLGF), platelet-derived growth factor (PDGF), and angiopoietin (ANG)9. VEGF not only influences the process of angiogenesis but also plays a role in tumor initiation and progression because of its ability to affect cancer stem cell (CSC) size and self-renewal ability. One of the most commonly altered genes in human tumors is the p53 tumor suppressor gene, whose alteration occurs in almost 50% of cancers10. p53 reduces hypoxia-induced Hif-1α expression by promoting its ubiquitination and subsequent destruction11. Furthermore, hypoxia is associated with genomic instability because of changes in DNA damage repair pathways and increased formation of reactive oxygen species (ROS)12. A significant barrier in clinical oncology is resistance to standard therapy, which might result in cancer recurrence. Ionizing radiation, numerous types of chemotherapy, and photodynamic therapy may all be rendered ineffective by a lack of oxygen. To better withstand the damaging effects of radiation and chemotherapy, hypoxia induces a cellular state of quiescence and cell cycle arrest13. Resistance to chemotherapy induced by hypoxia is associated with many mechanisms, including the modulation of autophagy and p53 14. Hypoxia is inversely proportional to pH, indicates more hypoxic tumor site means less pH (acidic) in the TME. The acidic TME is also responsible for drug resistance via the induction and increased activity of multidrug resistance (MDR) transporters15. Evidence is also growing that hypoxia-affected cancer stem cells play a major role in tumor resistance and relapse after standard treatment with chemotherapy and radiotherapy. Literature findings also imply that hypoxia increases chemosensitivity in tumor cells3. Chemotherapy is the mainstay of treatment for cancer, but rising resistance and recurrence after chemotherapy provide a challenge to finding new, better drugs. Inhibiting the Hif pathway specifically to prevent angiogenesis is a promising new approach for cancer therapy. Solid tumor growth and metastasis may be hampered by blocking both Hif-1 and VEGF, two proteins that are essential for malignancies to survive in low oxygen environments. The first platinum-based chemotherapeutic drug, cisplatin, has better anticancer efficacy, but due to systemic toxicity and side effects, scientists are still looking for new chemotherapeutic agents. Several organotin compounds have chemical modifications with higher anticancer activity and minimal side effects16. Recently, various studies have demonstrated that certain organotin compounds have the ability to selectively target the hypoxic cancer cells. For example, triphenyltin hydroxide has been found to trigger apoptosis in hypoxic cancer cells without affecting normal cells. Additionally, triphenyltin hydroxide was also found to reduce the growth and metastasis of tumor in mice model. The exact mechanism by which organotin compounds target hypoxic cancer cells is not well understood. However, it is believed that these compounds may interfere with the expression of genes involved in hypoxic response pathways16,17. Considering the vast range of pharmacological uses, particularly the anticancer capabilities of diverse triazole derivatives, and as part of our ongoing study on physiologically active new compounds, we demonstrate the in vivo antitumor activity of OTC18. Herein, we have described a strategy in which OTC treatment alters the mitochondrial metabolism of tumor cells and promotes apoptosis in a Hif-1 α-dependent manner.
Materials and methods
Cell culture
The triple-negative breast cancer cell line MDA-MB-231 (Procured from NCCS Pune, India.) was grown in DMEM (Genetix Biotech Asia Pvt. Ltd. Cat no. CC3004) supplemented with 10% fetal bovine serum (FBS; South American origin; Genetix Biotech Asia Pvt. Ltd. (Cat no. CCS-500-SA-U), antibiotic-antimycotic solution (penicillin 1000 units/ml, streptomycin 10000 µg/ml and amphotericin B 25 µg/ml) (Cat no. CC4007) in a humidified CO2 incubator and 5% CO2 were supplied.
CoCl2 and OTC compound stock preparation and hypoxia treatment
Solution of CoCl2 (25 mM stock) was prepared in sterile triple distilled water and further diluted in complete medium to achieve the desired 25 µM concentration. For inducing hypoxia chemically, MDA-MB-231 cells were exposed with solution of CoCl2 at 25 µM concentration and incubated for 24 h, 100 mM stock solution of OTC was dissolved in DMSO (Cat no. SE2S720221), followed by serial dilution in complete medium.
Mitochondrial distribution pattern
It is well established that changes in the mitochondrial distribution pattern and the shape of mitochondria are proapoptotic signals after anticancer drug treatment19. In brief, 5 × 104 viable MDA-MB-231 cells were seeded in 12-well cell culture plates (Genetix Biotech Asia Pvt. Ltd.) and left overnight for adherence. Following incubation, to induce hypoxia chemically, the CoCl2 treatment was given and thereafter cells were exposed with OTC and doxorubicin. The cells were washed with PBS followed by staining with MitoTracker red (procured from Invitrogen, Cat no. M7512)) (1 µM) and Hoechst 33342 (Real gene Cat no. 221011) (10 µg/ml) for 30 min. After staining, the cells were rewashed with PBS and images were taken by EVOS FL microscopy in phase contrast, blue and red channels at 400X magnification. For quantitative analysis similar experiment was also performed and the cells were processed through flow cytometry to validate the qualitative (microscopy) results.
Mitochondrial membrane potential
The cationic fluorescent dye JC-1 displays versatile nature depending upon the physiological condition of the mitochondria20. During the induction of apoptosis, mitochondria lose their membrane potential (ΔΨ). When JC-1 (Cayman Cat No. 15003) dye binds to healthy mitochondria, it forms J-aggregates and exhibits red fluorescence (emission maxima at ̴ 590 nm) at higher membrane potential, while it forms J-monomers when bound to compromised mitochondrial membrane potential and exhibits green fluorescence (emission maxima at ̴ 529 nm)21. Briefly, 5 × 104 viable MDA-MB-231 cells were seeded in 6-well cell culture plate and processed according to the above-mentioned protocol. Finally, cells were stained with JC-1 dye at 2 µM (Thermo Fisher Scientific) in PBS for 30 min, and images were taken by EVOS FL microscopy at 400X magnifications. Additionally, the mitochondrial membrane potential was also quantitatively assessed by flow cytometry. The cells were directly subjected to flow cytometry after staining with 1 μm JC-1 dye.
In vivo study
After obtaining the approval from Institutional Animal Ethical Committee, Institute of Science, Banaras Hindu University, Varanasi India (Approval no. BHU/DoZ/IAEC/2021–2022/013). All the in vivo experiments were performed according to guidelines of (CPCSEA) Committee for the Purpose of Control and Supervision of Experiments on Animals (Reg. No. 1802/Go/RE/S/15/CPCSEA). The methods were reported in accordance with ARRIVE guidelines. Initially mice were procured from CDRI Lucknow India, and then colonies were grown by subsequent breeding in the departmental animal house facility. The BALB/c mice, 7–8 weeks old, with an average weight of 24 ± 4 g, including both males and females, were used in the study. BALB/c mice were kept in a departmental animal house in well-ventilated cages and standard quality mouse-feed and water ad libitum were provided. The animals were acclimatized to environmental conditions with 12-hour light-dark cycles across the experimental period, and a standard room temperature of 22 °C ± 5 °C was maintained. During experimentation isoflurane was given to the mice for anesthesia with the help of nosecones prior to cervical dislocation.
Intraperitoneal tumor study
Dalton’s lymphoma (DL) cells were maintained in the peritoneum of the mouse. Briefly, 1 × 106 DL cells were injected intraperitoneally and allowed to grow for 7 days. On the 8th day after tumor transplantation, the therapy schedule was executed. Both drug solutions were prepared daily immediately before injection by suspending them in 0.9% saline and were given intraperitoneally at 5 mg/kg body weight at each 4-day intervals.
Mean survival time and increase life span studies
The total number of days an animal lived after tumor induction was counted and the mean survival time (MST) for each group was calculated. The survival days of treated group were determined by comparing them with control group using the following equation:
Ex situ analysis of apoptosis by AnnexinV/PI assay
Furthermore, to analyze apoptotic induction in intraperitoneal tumor after 4 subsequent doses of treatment, the annexinV/PI (Cat no. 1947895) dual staining method was used. The cells were extracted from the peritoneum of the mice from both treated and untreated groups, further the cells were washed with PBS, stained with annexinV/PI according to the manufacturer’s protocol and processed for experimentation as described before.
Solid tumor model development body weight and tumor volume measurement
Dalton’s lymphoma (DL cells) is highly aggressive, transplantable T-cell lymphoma widely used as an appropriate model for cancer chemotherapy-related studies22. Following maintenance, the mice were divided into three different groups, with 4 mice in each group. For solid tumor generation, 0.5 × 106 Dalton’s lymphoma cells were injected intramuscularly into the hind limbs of the mice. After every four-day interval, the tumor volume was measured. The body weights of all the respective mice were measured on day 0, 4, 8, 12, 16 and 20, while the circumference of the peritoneal tumor was measured on days 0, 4, 8, 12, 16, 20, 24 and 28. The tumor volume of solid tumors was measured from the 0 to 36th day at every 4-day interval. The following equation was used to calculate the tumor volume:
Volume = 1/2 [(length)2 × width].
Determination of hypoxia in solid tumors through biochemical methods
To check the hypoxia induction in the tumor microenvironment, the tumors were isolated on the 8th, 12th and 16th consecutive days. The proteins were isolated in 10% homogenate of RIPA buffer (Bio-Chemax, Axiva Sichem Biotech), and total protein was quantified by using a BCA kit (according to the manufacturers protocol, BioVision, USA, Cat no. 1K190813). Hif-1α is one of the most commonly known marker for hypoxia induction23. Therefore, the Hif-1α (Cat no. 700505) expression level was assessed in bone marrow cells, Dalton’s lymphoma cells, 8th day tumor, 12th day tumor and 16th day tumor proteins. Among them, at day 16, the Hif-1α level was significantly increased (Figure S2; supplementary file); therefore, the treatment scheduled was design and initiated at that time following tumor induction.
Determination of tumor hypoxia through photoacoustic and ultrasound imaging systems
Photoacoustic (PA) imaging is a mongrel imaging technique which is merged with optical and ultrasonic resolution having spectroscopic contrast. Pulsed excitation light is absorbed by tissue during PA imaging, and the generated ultrasound (US) waves are then detected, processed, and used to create a picture24,25. Over the past decade, PA imaging has become a formidable biomedical imaging technique with enormous promise for a variety of clinical and preclinical applications26,27,28,29. Using a clinical US imaging probe, PA imaging and US imaging may be easily coupled. The pictures are naturally registered since the reception transducer components in the probe are the same. Structure and molecular contrast are both provided by these dual-mode photoacoustic and ultrasonic (PA/US) imaging devices27,30. Therefore, the experiment was further validated tumor hypoxia through photoacoustic and ultrasound imaging systems in live conditions by administering mild anaesthesia (isoflurane) to animals31. The analyzed photoacoustic and ultrasound images indicate that by day 16 tumors have developed a hypoxic core region of the solid tumor (Figure. S3; Supplementary file). Therefore, day 16 post tumor induction was considered for initiating the scheduled therapy.
Schedule of therapy
The mouse colony was maintained and solid tumors were induced according to the above-mentioned section. At every 4-day interval, intratumoral treatment of OTC and DOX was given at 5 mg/kg body weight up to 5 doses, and tumor volume was measured simultaneously. At day 36, mice were sacrificed (Isoflurane was given to the mice for anesthesia prior to cervical dislocation), followed by tumor isolation, and major vascular organs, such as liver, spleen, and kidney, were isolated for histopathological studies.
Histopathology studies
For histopathological studies, one mouse from each group was sacrificed by cervical dislocation, and major vascular organs (liver, spleen and kidney) as well as solid tumors were dissected out and stored in formalin at room temperature. The slides of liver and solid tumor were prepared by a standard method followed by eosin and hematoxylin staining. The slides were viewed and photographed by light microscopy.
Detection of differentially expressed genes at mRNA level through RT-PCR
The solid tumor was dissected out, and 10% homogenate was prepared in TRIzol reagent. Samples were kept on ice followed by three homogenizations at an interval of 10 min. Total RNA was extracted with the help of TRIzol reagent (Sigma-Aldrich, Cat. No. T3934) by using manufacturer’s protocol following RNA estimation by spectrophotometer (mySPEC). A Revert Aid H Minus First Strand c-DNA synthesis kit (Thermo Fisher Scientific) was used to synthesize c-DNA with 3 µg RNA. Furthermore, the differential expression patterns of the Hif-1α, VEGF, p53, Bax, Bcl-2, Cytochrome-c and Caspase 3 genes were determined in a thermal cycler (Applied Biosystem). Bioinformatics tools were used for designing the above-mentioned gene primers and purchased from Eurofins.
Detection of differentially expressed proteins through western blot analysis
To assess the differential protein expression in untreated and treated groups of mice, Western blot analysis was performed. Briefly, mice were sacrificed from each group, solid tumors were isolated, and 10% homogenate was prepared in RIPA buffer (Bio-Chemax, Axiva Sichem Biotech, India) containing PMSF. The samples were kept on ice and homogenized thrice at 10-minute intervals followed by 12 min of centrifugation at 12000 RPM at 4 °C. Quantification of total protein were done by bicinchoninic acid (BCA; BioVision USA, Cat No K813-2500 (Lot no. 1K190813) kit32. A total of 40–60 µg proteins were loaded onto 12% SDS-PAGE and thereafter with the help of wet transfer method, proteins were transferred to PVDF (Merck Millipore, USA, Cat. No. IPVH00010) membrane by incubating overnight at 4 °C. Following blocking, the primary antibodies anti-β-actin (Ambion, Cat no. AM4302), anti-Hif-1α (Cat no. 700505), anti-VEGF (Cat no. A17877), anti-PARP-1 (Cat no. TA804938S) (OriGene), anti-p53 (Cat No. E-AB-32469), anti-BAX (Cat no. TA810334S), anti-Bcl-2 (Cat no. E-AB-60012), anti-caspase 3 (Elabscience, Cat no. 700182) were individually added with their recommended dilutions. Further, membrane was washed three times with TBST and 5%NFDM (from Sigma Aldrich), and subsequently, each blot was subjected to incubation with their respective 2º antibodies (GeNei™) (for beta actin, Bcl-2, Bax, and caspase 3, ALP conjugated rabbit anti-mouse IgG, while for Hif-1α, VEGF and PARP-1, ALP conjugated goat anti-rabbit IgG) were used at a dilution of 3:15,000 for 2 h of incubation. Thereafter, membrane was subjected to washing thrice with TBST. Subsequently, substrate of alkaline phosphatase (BCIP/NBT solution) was added for 15–30 min. The resulting protein expression levels were taken by E-Gel imager (Thermo Fisher, USA).
Statistical analysis
For each experimental group, the mean and SD were examined using three independent measurements. Student’s t-test and One-way analysis of variance (ANOVA) were used to analyze group differences. Pairwise comparisons were performed using PRISM statistical analysis software (Graph Pad Software, Inc., San Diego, CA, USA) and SPSS 16. The calculated differences between the groups were significant. Significance was defined as p < 0.05. The log-rank test, performed with Graph Pad PRISM software, was used to determine the statistical significance of differences in mouse survival between groups.
Results
Mitochondrial distribution pattern
Many anticancer drugs exert their antitumor efficacy by efficiently targeting mitochondria to promote the intrinsic apoptotic pathway33. The results showed that the uniformly distributed mitochondria (in untreated hypoxic cells) were affected following exposure to OTC, as most of the mitochondria were aggregated at the perinuclear region of the hypoxic breast cancer cells. In contrast, treatment with doxorubicin failed to induce significant mitochondrial aggregation (Fig. 1 (A)). The above result was further validated by flow cytometry exhibiting similar trends, where 88.14% of mitochondrial aggregation was quantified compared to DOX (33.05%) under hypoxic conditions. However, under normoxic conditions, 83.75% aggregation was observed in OTC-treated cells compared to 56. 48% with DOX treated cells (Fig. 1 (B)). The obtained results corroborated a previous report where similar expression was observed34. Therefore, the present result can be concluded that OTC significantly induces mitochondrial aggregation in hypoxic breast cancer cells, whereas doxorubicin was found less effective under similar conditions.
(A) Pattern of mitochondrial distribution in MDA-MB-231 cells under both normoxic and hypoxic condition after OTC and doxorubicin treatment. The uniformly distribution were seen in control cells while aggregated mitochondria were observed in OTC treated group of cells. (B) Quantitative assessment of mitochondrial distribution pattern in MDA-MB-231 cells under both hypoxic and normoxic condition after OTC and doxorubicin treatment. The obtained histogram displayed that a significant increase in mitochondrial aggregation was found in OTC treatment group in both hypoxic and normoxic condition as compared DOX treatment under similar experimental condition.
Mitochondrial membrane potential
Several outer and inner membrane proteins are required for the energy production and metabolism of mitochondria. Any alteration in membrane proteins after anticancer drug treatment disrupts mitochondrial metabolism and mitochondrial transmembrane potential and ultimately promotes cell death35,36. Fluorescence microscopy and flow cytometry were used for the detection of J-aggregates and J-monomers in hypoxia induced MDA-MB-231 cells. OTC treatment significantly affected mitochondrial membrane potential under hypoxic conditions, as J-monomers were observed in Fig. 2 (A), while doxorubicin treatment did not alter the mitochondrial membrane potential, as J-aggregates were observed under similar conditions (Fig. 2 (A)). The obtained result was further validated by flow cytometry, where 52.29% (Q2 LR) J-monomers were observed in the OTC treated group compared to 17.53% (Q2 LR) in the DOX treated group (Fig. 2.(B)). However, 46.22% and 30.16% J-monomers were observed in the OTC and DOX treated groups respectively, under normoxic conditions. The obtained results were corroborated with other research articles and found to be similar to previously available articles37.
(A) The mitochondrial membrane potential has been assessed by JC-1 dye in cultured MDA-MB-231 cells under hypoxic as well as normoxic condition. Where (A) is showing untreated cells, (B) showing doxorubicin treated cells and (C) representing OTC treated cells in hypoxic condition while (D), (E) and (F) are representing control, doxorubicin and OTC treatment groups respectively under normoxic condition. (B) Quantitative detection of mitochondrial membrane potential of treated (OTC and Doxorubicin) and untreated MDA-MB-231 cells under both hypoxic and normoxic conditions through flow cytometry after staining with cationic dye JC-1. The obtained results demonstrated that OTC treatment significantly decreases mitochondrial potential as compared to DOX under both hypoxic and normoxic condition.
Intraperitoneal tumor study
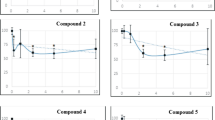
Measurement of tumor growth, survival and body weight
To check the antitumor potential of OTC in in vivo system, different parameters were used. Intraperitoneal (IP) treatment with OTC significantly inhibited the growth of intraperitoneally disseminate tumors by DL cells. The photographic results of peritoneum show that OTC has antiangiogenic properties, suppresses tumor growth, and increases the life expectancy of mice, while DOX treatment also suppresses the growth of tumors and inhibits angiogenesis but does not increase the life span of mice compared to OTC (Fig. 3). DOX-treated mice were survived till day 36, while OTC treated mice were survived up to the 59th day. Considering the overall outcome of the peritoneal tumor study, OTC treatment potentially inhibits tumor growth and increases the life span of animals compared to DOX.
The figure representing therapy schedule (A), circumference (B) and (C), Kaplan-Meier survival (D) and Body weight (E) of mice were determined after treatment with OTC and doxorubicin. (Sample size, n = 4 in each group). Statistical analysis has been done by One-way ANOVA followed by Tukey’s test where * denotes significant difference (p < 0.05) as compared to control.
Ex situ analysis of apoptosis by AnnexinV/PI assay
To investigate apoptosis, quantitative flow cytometry analysis was carried out on both intraperitoneally treated and untreated T-cell lymphoma (DL) bearing mice with both doxorubicin and OTC at 5 mg/kg body weight. OTC-treated cells showed a considerable increase in late apoptotic cells (UR-Upper Right), as 38.18% of the population was observed in comparison to controls (Figure 4). The doxorubicin-treated mouse group showed a substantial increase of 84.85% in the dead cell population (UL-upper left). Although doxorubicin treatment resulted in a 9.58% cell population (UR), OTC treatment resulted in a 46.54% dead cell population (UL), as shown in Fig. 4.
Analysis of apoptosis in T cell lymphoma bearing mice through flow cytometry. The differentiation between live cells, early apoptotic cells, late apoptotic cells and dead cells were done by AnnexinV/PI dual staining. No significant apoptosis was observed in control and saline treatment group whereas significant apoptotic and dead cell population were observed in OTC and DOX treatment group in T-cell lymphoma bearing mice.
Solid tumor study
The hypoxia marker Hif-1α is generally overexpressed in many types of cancer and solid tumors. Therefore, we first investigated Hif-1α expression in solid tumors at different time intervals through Western blotting. The obtained result shows that the level of Hif-1α expression was significantly increased at the 16th day tumor; therefore, therapy was scheduled from the 16th day onwards, and 5 consecutive doses at each 4-day interval were given.
Determination of tumor size regression and survival analysis
The regression in tumors after drug treatment was analyzed, and the obtained results showed that OTC treatment significantly decreases the tumor size compared to doxorubicin as well as the control group. Kaplan-Meier survival curve displayed that considerable increase in the life span of the hypoxic solid tumor-bearing mouse group was observed following OTC treatment compared with the life span of untreated mice (Fig. 5). The T/C ratio suggests that OTC treatment was active for hypoxic anticancer effectiveness and has the potential to be used for hypoxic solid tumor therapies. In addition, after conducting an analysis of the T/C value, it was discovered that OTC treatment of 5 mg/kg body weight had a survivability of beyond 80 days, while doxorubicin had a survivability of 57 days at the same dose.
Therapeutic efficacy of OTC and doxorubicin against experimental murine lymphoma. (A) representing the schedule therapy, (B) Photographic illustration of untreated and treated hypoxic solid tumor developed in right thigh intramuscularly in BALB/c mice at day 36. (C) photographic images of major vascularized organs, (D) Tumor weight analysis, (E) tumor volume, (F) Kaplan-Meier survival analysis and (G) is representing weight analysis of liver, spleen and kidney of the untreated and treated tumors. Statistical analysis has been done by One-way ANOVA followed by Tukey’s test where * denotes significant difference (p < 0.05) as compared to control. (Sample size, n = 7 in each group).
Determination of tumor regression through photoacoustic and ultrasound imaging system
The 3D visualization of vasculature may also be accomplished using an LED-based photoacoustic imaging system38. Rodent models are often employed in preclinical cancer research to examine the intricate physiological processes involved in tumor growth and treatment response. At the location where the tumor cells first appear, the tumor grows either subcutaneously or orthotopically38. Therefore, the tumor size regression was assessed after scheduled therapy with OTC and DOX through photoacoustic and ultrasound imaging systems. The analyzed photoacoustic images show that a significant decrease in tumor size was observed in the OTC treated group compared to the DOX and untreated groups (Fig. 6).
Photoacoustic ultrasound and 3D vasculature view of solid tumor in pretreatment (day 16) and post treatment (day 36) conditions after schedule therapy with DOX and OTC. The whole solid tumor is encircled in turquoise color and hypoxic region are encircled in red color in the respective tumors. The OTC administration significantly reduces tumor load as compared to DOX.
Effect of OTC on histopathological parameters
Two mice from each group as well as a control mouse were sacrificed by cervical dislocation after the completion of scheduled drug treatment. The liver, kidney, spleen, and solid tumor of each mouse were dissected out, and their weights were recorded and photographed before being fixed in 4% formalin. During tumor progression, due to metastasis, an infiltration of metastatic cells is generally observed in vascularized organs such as the liver, kidney and spleen. Due to this, significant inflammation was observed in these organs, but OTC treatment significantly decreased inflammation and promoted these organs toward normal physiological conditions, whereas doxorubicin was less effective in such cases (Fig. 7(A)).
Solid tumor-bearing mice showed significant morphological alterations in hepatocytes when compared to normal mice. Hepatocytes were arranged in a consistent pattern with regular central and portal veins in the liver sections of untreated mice (Fig. 7(A)). However, mice with hypoxic solid tumors showed altered hepatocytes with infiltrating lymphoid cells and disorganized portal and central veins. In lymphoma-bearing mice, OTC treatment restored the normal hepatic architecture, appropriate central and portal veins, and little cell infiltration. Similar severe pathological alterations were observed in the solid tumor sections of lymphoma-bearing animals, including necrosis and infiltration of inflammatory cells. However, neither mice treated with the drug nor those left untreated showed any such pronounced alterations. As a consequence, our findings reveal that OTC can reconstruct the liver histoarchitecture, which are equivalent to those of normal animals. Furthermore, H&E staining of solid tumor tissue data showed that OTC treatment significantly maintained the normal histoarchitecture of muscle tissue, whereas in solid tumor bearing mice, sections showed disorganized tissue architecture (Fig. 7. (B)).
(A) Histopathological sections of liver of normal mice, tumor bearing mouse and different treatment groups. Here untreated tumor bearing mouse showing altered hepatocytes with unfiltered lymphoid and metastatic foci were observed while the treatment of OTC compounds significantly recovered to the normal histoarchitecture. (B) Histopathological sections of the DL induced solid tumor in both treated as well as control (untreated) group after staining with H&E.
Detection of differentially expressed genes at mRNA level through RT-PCR
The band intensity of the qualitative PCR (RT-PCR) product was measured with an Alpha imager. The obtained relative density values were calculated after normalization to beta-actin. Bone marrow (BM) cells were used as a reference throughout the RT-PCR study. The hypoxia associated genes Hif-1α and VEGF were significantly downregulated in the OTC treated group compared to the DOX and untreated groups, whereas Hif-1α expression was significantly upregulated in the DOX treated groups (Fig. 8). Furthermore, the expression of the p53 gene was significantly upregulated in both the OTC and DOX treated groups compared to the control. The mitochondrial associated antiapoptotic gene Bcl-2 was significantly downregulated in the OTC treatment group, whereas the proapoptotic gene Bax was upregulated in both the OTC and DOX treatment groups. Furthermore, the mitochondrial outer membrane associated gene Cytochrome-c was significantly upregulated in the OTC treatment group, and the final executor of apoptosis caspase 3 was significantly upregulated in both the OTC and DOX treated groups compared to the control (Fig. 8). Therefore, considering the above outcomes, it can be concluded that OTC treatment displayed better efficacy than DOX in hypoxic solid tumors.
Semi-quantitative PCR of hypoxia as well as apoptosis associated gene Hif-1α, VEGF, p53, Bax, Bcl-2, Cytochrome-c and caspase 3. Statistical analysis has been done by One-way ANOVA followed by Tukey’s test where * denotes significant difference (p < 0.05) as compared control and # denotes significant difference (p < 0.05) between the treatment group.
Detection of differentially expressed proteins through Western blot analysis
The western blot data revealed gradual stabilization of Hif-1α expression in solid tumors on the 8th 12th and 16th days, confirming that progression of the tumor modulates its microenvironment (supplementary data Figure. S2 and S3). Furthermore, significant downregulation of Hif-1α in the OTC treated group clearly indicates that OTC overcomes hypoxia by inhibiting the expression of Hif-1α through an unknown mechanism, while doxorubicin treatment significantly increases the expression of Hif-1α (Fig. 9). The angiogenic protein VEGF was found to be significantly downregulated in the OTC-treated group compared to DOX, which potentially defends the anti-angiogenic activity of OTC (intraperitoneal treatment). The expression of the well-known cell cycle progression regulator p53 and nick sensor containing DNA damage repair protein PARP-1 (cleaved PARP-1) was significantly increased in the OTC treated group compared to the DOX (DXR) treated group. Furthermore, upregulation of caspase 3 and Bax while downregulation of the anti-apoptotic protein Bcl-2 strongly supports the in vitro study of mitochondrial membrane potential and mitochondrial aggregation assay outcomes and demonstrates mitochondria mediated apoptosis after OTC treatment. Western blot analysis clearly demonstrated that OTC treatment overcame hypoxia and promote apoptosis by inhibiting Hif-1α and VEGF while doxorubicin was less effective in the tumor microenvironment.
SDS-PAGE followed by western blot analysis of Hif-1α, VEGF, cleaved PARP-1, p53, Bax, Bcl-2 and caspase 3 proteins levels in control and treated groups of solid tumor bearing mice. Changes in expression were indicated after normalizing with beta-actin used as internal loading control. Statistical analysis has been done by One-way ANOVA followed by Tukey’s test where * denotes significant difference (p < 0.05) compared to control and # denotes significant difference (p < 0.05) between the treatment group.
Discussion
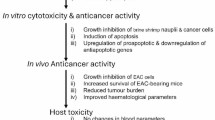
Hypoxia develops in tumor areas with inadequate oxygen delivery and is a significant impediment to cancer therapy. The range of hypoxia levels is very diverse, ranging from moderate (nearly nonhypoxic) to severe (almost anoxic) in solid tumors. Individual hypoxia levels cause a range of biological reactions that reduce the effectiveness of anticancer drug39. Numerous unconventional platinum compounds and nonplatinum metal complexes have been created and investigated since the use of cisplatin in cancer treatment. For instance, organotin derivatives have strong cytotoxic and antitumor effects40. To investigate the antitumor efficacy of OTC toward T-cell lymphoma bearing BALB/c mice, following treatment, survival days, antiangiogenic activity and tumor load regression were measured. The maximum tolerated dosage (MTD) for the chosen OTC was first established, and then the growth patterns of survival days, T/C values, body weight, and belly size were assessed. In the present study, it was observed that OTC significantly increased the life span of T-cell lymphoma-bearing mice while also significantly reducing their tumor load and belly size growth pattern without causing significant other distinct side effects. The effectiveness of OTC for intraperitoneal cancers has been the subject of preliminary research. The in vivo study revealed that 20% of OTC-treated animals survived more than 3 times compared to the untreated group and showed increased tumor regression with an 80% reduction in tumor size. The ex situ quantitative analysis of apoptosis data revealed that 4 consecutive doses of OTC were sufficient to induce apoptosis in intraperitoneal tumor bearing mice and suppress tumor growth. Therefore, considering all the outcomes of the intraperitoneal tumor study, it can be said that the newly synthesized compound OTC can be used as a potent anticancer agent against T-cell lymphoma. Furthermore, to determine the hypoxic anticancer potential of the OTC compound against hypoxic solid tumors, BALB/c mice were used. DOX is a valuable clinical antineoplastic agent, but severe cardiotoxicity and drug resistance in hypoxic solid tumors limit its use41. In the present investigation, DOX was found to be less effective at the pathophysiological and molecular levels. On the other hand, OTC treatment significantly exerted its anticancer potential even under hypoxic conditions. Tumors with hypoxic zones are likely to have lower levels of nutrients such as glucose and critical amino acids. The lower pH is also a reason behind the failure of several anticancer medications, including DOX, as these drugs are generally quite active at physiological pH42. Among the several clinical imaging modalities, ultrasound (US) makes use of sonic waves capacity to penetrate deeply into tissues and scatter back to the receiver. It is also nonionizing, inexpensive, portable, and real-time. Tumoral and healthy tissue may be distinguished from one another in an ultrasound picture by differences in echogenicity or acoustic impedance43. The photoacoustic and ultrasound imaging data showed that OTC therapy significantly decreased the hypoxic solid tumor size as the red-encircled area of the solid tumor was reduced to the cyan encircled area. On the other hand, DOX treatment did not induce much regression of the tumor, which clearly indicates the failure of DOX in hypoxic solid tumors. The histopathological sections of the liver and solid tumor data show that OTC therapy significantly promotes towards normal physiological conditions, whereas doxorubicin was found less effective in such cases. Many anticancer medications cause DNA damage when oxygen is present because they produce free radicals. In this regard, the expression of the most dynamic protein PARP-1 was assessed, and results showed that OTC treatment significantly increased the expression of cleaved PARP-1, which clearly indicates that OTC treatment causes DNA damage. The caspase 9 and caspase 3 cascade pathways proteolytically degrade PARP-1 from the C-terminus into 89 kDa protein44. Furthermore, Hif-1α expression was found to be significantly downregulated in the OTC treatment group, whereas DOX treatment significantly increased Hif-1α expression. The obtained data corroborated previous available research articles, and similar trend was observed45,46,47. Furthermore, the expression of VEGF and Bcl-2 was also found to be downregulated at the gene and protein levels in the OTC treatment group compared to the DOX and control groups, which also delineates the better efficacy of the OTC compound. The effect of doxorubicin on Hif-1α and VEGF corroborated other available literature where it was found in a similar pattern47. The significant upregulation of the pro-apoptotic gene Bax, the mitochondrial associated gene Cytochrome-c and the final executer of apoptosis caspase 3 at the mRNA and protein levels clearly demonstrates the superior activity of OTC. The whole outcomes of the present study have been represented in the Fig. 10. Therefore, considering all the above outcomes, it can be concluded that the newly synthesized compound OTC could be a promising compound for hypoxic solid tumors.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author and will be provided on reasonable request.
References
Seyfried, T. N. & Huysentruyt, L. C. On the origin of Cancer Metastasis. Crit. Rev. Oncog. 18, 43–73 (2013).
Fares, J., Fares, M. Y., Khachfe, H. H., Salhab, H. A. & Fares, Y. Molecular principles of metastasis: a hallmark of cancer revisited. Signal. Transduct. Target. Ther. 5, 28 (2020).
Emami Nejad, A. et al. The role of hypoxia in the tumor microenvironment and development of cancer stem cell: a novel approach to developing treatment. Cancer Cell Int. 21, 62 (2021).
Carmeliet, P. et al. Role of HIF-1alpha in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature 394, 485–490 (1998).
Majmundar, A. J., Wong, W. J. & Simon, M. C. Hypoxia inducible factors and the response to hypoxic stress. Mol. Cell. 40, 294–309 (2010).
Simiantonaki, N., Taxeidis, M., Jayasinghe, C., Kurzik-Dumke, U. & Kirkpatrick, C. J. Hypoxia-inducible factor 1 alpha expression increases during colorectal carcinogenesis and tumor progression. BMC Cancer. 8, 320 (2008).
Sun, H. C. et al. Expression of hypoxia-inducible factor-1 alpha and associated proteins in pancreatic ductal adenocarcinoma and their impact on prognosis. Int. J. Oncol. 30, 1359–1367 (2007).
Ke, Q. & Costa, M. Hypoxia-inducible Factor-1 (HIF-1). Mol. Pharmacol. 70, 1469–1480 (2006).
Zimna, A. & Kurpisz, M. Hypoxia-Inducible Factor-1 in Physiological and Pathophysiological Angiogenesis: Applications and Therapies. BioMed Research International 2015, e549412 (2015).
Levine, A. J. p53, the Cellular Gatekeeper for Growth and Division. Cell 88, 323–331 (1997).
Ravi, R. et al. Regulation of tumor angiogenesis by p53-induced degradation of hypoxia-inducible factor 1α. Genes Dev. 14, 34–44 (2000).
Bristow, R. G., Hill, R. P. & Hypoxia DNA repair and genetic instability. Nat. Rev. Cancer. 8, 180–192 (2008).
Das, B. et al. Hypoxia enhances tumor stemness by increasing the invasive and tumorigenic side population fraction. Stem Cells. 26, 1818–1830 (2008).
Rohwer, N. et al. Hypoxia-inducible factor 1alpha determines gastric cancer chemosensitivity via modulation of p53 and NF-kappaB. PLoS One. 5, e12038 (2010).
Zhitomirsky, B. & Assaraf, Y. G. Lysosomes as mediators of drug resistance in cancer. Drug Resist. Updates. 24, 23–33 (2016).
Varela-Ramirez, A., Costanzo, M., Carrasco, Y. P., Pannell, K. H. & Aguilera, R. J. Cytotoxic effects of two organotin compounds and their mode of inflicting cell death on four mammalian cancer cells. Cell. Biol. Toxicol. 27, 159–168 (2011).
Syed Annuar, S. N., Kamaludin, N. F., Awang, N. & Chan, K. M. Cellular basis of Organotin(IV) derivatives as Anticancer metallodrugs: a review. Front. Chem. 9, 657599 (2021).
Singh, V. et al. Aqua-(2-formylbenzoato)triphenyltin(IV) induces cell cycle arrest and apoptosis in hypoxic triple negative breast cancer cells. Toxicol. In Vitro. 86, 105484 (2023).
Smaili, S. S., Hsu, Y. T., Youle, R. J. & Russell, J. T. Mitochondria in Ca2 + signaling and apoptosis. J. Bioenerg Biomembr. 32, 35–46 (2000).
Elefantova, K., Lakatos, B., Kubickova, J., Sulova, Z. & Breier, A. Detection of the mitochondrial membrane potential by the Cationic Dye JC-1 in L1210 cells with massive overexpression of the plasma membrane ABCB1 drug transporter. Int. J. Mol. Sci. 19, E1985 (2018).
Chazotte, B. Labeling mitochondria with JC-1. Cold Spring Harb Protoc pdb.prot065490 (2011).
Koiri, R. K. et al. Dalton’s lymphoma as a murine model for understanding the progression and development of T-Cell lymphoma and its role in Drug Discovery. Int. J. Immunotherapy Cancer Res. 3, 001–006 (2017).
Vukovic, V., Haugland, H. K., Nicklee, T., Morrison, A. J. & Hedley, D. W. Hypoxia-inducible factor-1alpha is an intrinsic marker for hypoxia in cervical cancer xenografts. Cancer Res. 61, 7394–7398 (2001).
Zhou, Y., Yao, J. & Wang, L. V. Tutorial on photoacoustic tomography. J. Biomed. Opt. 21, 61007 (2016).
Beard, P. Biomedical photoacoustic imaging. Interface Focus. 1, 602–631 (2011).
Ermilov, S. A. et al. Laser optoacoustic imaging system for detection of breast cancer. J. Biomed. Opt. 14, 024007 (2009).
Xu, G. et al. Photoacoustic and ultrasound dual-modality imaging of human peripheral joints. J. Biomed. Opt. 18, 10502 (2013).
Xia, W. et al. Design and evaluation of a laboratory prototype system for 3D photoacoustic full breast tomography. Biomed. Opt. Express. 4, 2555–2569 (2013).
Kim, C., Favazza, C. & Wang, L. V. In vivo photoacoustic tomography of chemicals: high-resolution functional and molecular optical imaging at new depths. Chem. Rev. 110, 2756–2782 (2010).
Park, S., Jang, J., Kim, J., Kim, Y. S. & Kim, C. Real-time triple-modal Photoacoustic, Ultrasound, and magnetic Resonance Fusion Imaging of humans. IEEE Trans. Med. Imaging. 36, 1912–1921 (2017).
Hawkley, T. F., Preston, M. & Maani, C. V. Isoflurane. In StatPearls (StatPearls Publishing, 2022).
Rana, N. K., Singh, P. & Koch, B. CoCl2 simulated hypoxia induce cell proliferation and alter the expression pattern of hypoxia associated genes involved in angiogenesis and apoptosis. Biol. Res. 52, 12 (2019).
Haga, N., Fujita, N. & Tsuruo, T. Mitochondrial aggregation precedes cytochrome c release from mitochondria during apoptosis. Oncogene 22, 5579–5585 (2003).
Sharma, G. et al. p53 dependent apoptosis and cell cycle delay induced by heteroleptic complexes in human cervical cancer cells. Biomed. Pharmacother. 88, 218–231 (2017).
Green, D. R. & Reed, J. C. Mitochondria and apoptosis. Science 281, 1309–1312 (1998).
Jeena, M. T., Kim, S., Jin, S. & Ryu, J. H. Recent progress in Mitochondria-targeted drug and drug-free agents for Cancer Therapy. Cancers (Basel). 12, E4 (2019).
Yang, F. et al. Doxorubicin Caused apoptosis of mesenchymal stem cells via p38, JNK and p53 pathway. CPB 32, 1072–1082 (2013).
Xavierselvan, M., Singh, M. K. A. & Mallidi, S. In Vivo Tumor Vascular Imaging with light emitting diode-based photoacoustic imaging system. Sensors 20, 4503 (2020).
Hompland, T., Fjeldbo, C. S. & Lyng, H. Tumor Hypoxia as a barrier in Cancer Therapy: why levels Matter. Cancers 13, 499 (2021).
Arjmand, F., Parveen, S., Tabassum, S. & Pettinari, C. Organo-tin antitumor compounds: their present status in drug development and future perspectives. Inorg. Chim. Acta. 423, 26–37 (2014).
Kaye, S. & Merry, S. Tumour cell resistance to anthracyclines–a review. Cancer Chemother. Pharmacol. 14, 96–103 (1985).
Frederiksen, L. J. et al. Hypoxia Induced Resistance to Doxorubicin in prostate Cancer cells is inhibited by low concentrations of Glyceryl Trinitrate. J. Urol. 170, 1003–1007 (2003).
Hester, S. C., Kuriakose, M., Nguyen, C. D. & Mallidi, S. Role of Ultrasound and Photoacoustic Imaging in Photodynamic Therapy for Cancer. Photochem. Photobiol. 96, 260–279 (2020).
Soldani, C. & Scovassi, A. I. Poly(ADP-ribose) polymerase-1 cleavage during apoptosis: an update. Apoptosis 7, 321–328 (2002).
Osada-Oka, M. et al. Suppression of the doxorubicin response by hypoxia-inducible factor-1α is strictly dependent on oxygen concentrations under hypoxic conditions. Eur. J. Pharmacol. 920, 174845 (2022).
Doublier, S. et al. HIF-1 activation induces doxorubicin resistance in MCF7 3-D spheroids via P-glycoprotein expression: a potential model of the chemo-resistance of invasive micropapillary carcinoma of the breast. BMC Cancer. 12, 4 (2012).
Cao, Y. et al. Tumor cells upregulate normoxic HIF-1α in response to Doxorubicin. Cancer Res. 73, 6230–6242 (2013).
Acknowledgements
The author Virendra Singh acknowledges ICMR, New Delhi for providing Senior Research Fellowship (SRF) and contingency (File No. 45/23/2022-PHA/BMS). The authors also acknowledge Mr. Braj Nandan Kumar, CDC (Central Discovery Centre) Banaras Hindu University Varanasi, for assisting in the flow cytometry facility (Beckman Coulter). The author Virendra Singh also acknowledges Ms. Samita Verma and Mr. Vipin Singh for assisting in Western blot analysis.
Funding
The author BK acknowledges ICMR, New Delhi for financial assistance under Ad-hoc scheme (File No. 5/13/36/2022/NCD-III) and Banaras Hindu University for providing funding under the IoE scheme (File No. R/Dev/D/IoE/Incentive/2021-22/32449).
Author information
Authors and Affiliations
Contributions
Virendra Singh: Investigation, Formal analysis, Visualization, Conceptualization, Writing- original draft. Ranjeet Singh: Methodology, Investigation. Partha Pratim Manna: Investigation, Supervision. Pooja Goswami: Methodology, Writing. Tushar S. Basu Baul: Methodology, Investigation.Abhijit Mandal: Methodology, Formal analysis. Arvind Kumar Singh: Methodology, Formal analysis.Biplob Koch: Conceptualization, Methodology, review & editing, Supervision, Project administration, Funding acquisition. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
In vivo experimental protocols were approved by Institutional Animal Ethical Committee, Institute of Science, Banaras Hindu University, Varanasi India (Approval no. BHU/DoZ/IAEC/2021–2022/013). All the in vivo experiments were performed according to guidelines of (CPCSEA) Committee for the Purpose of Control and Supervision of Experiments on Animals (Reg. No. 1802/Go/RE/S/15/CPCSEA). The methods were reported in accordance with ARRIVE guidelines.
Consent to participate
The study does not include any human subjects, samples or case studies; hence this statement is not applicable.
Consent to publish
All the authors are giving their consent to publish an original research article entitled “Influences of aqua-(2-formylbenzoato) triphenyltin(IV) on regression of hypoxic solid tumor through mitochondrial mediated pathway by inhibiting Hif-1 alpha” for publication in the Scientific Reports journal.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Singh, V., Singh, R., Goswami, P. et al. Influences of aqua-(2-formylbenzoato) triphenyltin(IV) on regression of hypoxic solid tumor through mitochondrial mediated pathway by inhibiting Hif-1 alpha. Sci Rep 15, 5302 (2025). https://doi.org/10.1038/s41598-025-89761-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-89761-z
- Springer Nature Limited