Abstract
Epithelial ovarian cancer (EOC) presents considerable difficulties in prognostication and treatment strategy development. Bevacizumab, an anti-angiogenic medication, has demonstrated potential in enhancing progression-free survival (PFS) in EOC patients. Nevertheless, the identification of individuals at elevated risk of disease progression following treatment remains a challenging task. This study was to develop and validate a deep learning (DL) model using retrospectively collected computed tomography (CT) plain scans of inoperable and recurrent EOC patients receiving bevacizumab treatment diagnosed between January 2013 and January 2024. A total of 525 patients from three different institutions were retrospectively included in the study and divided into training set (N = 400), internal test set (N = 97) and external test set (N = 28). The model’s performance was evaluated using Harrell’s C-index. Patients were categorized into high-risk and low-risk group based on a predetermined cutoff in the training set. Additionally, a multimodal model was evaluated, incorporating the risk score generated by the DL model and the pretreatment level of carbohydrate antigen 125 as input variables. The Net Reclassification Improvement (NRI) metric quantified the reclassification performance of our optimal model in comparison to the International Federation of Gynecology and Obstetrics (FIGO) staging model. The results indicated that DL model achieved a PFS predictive C-index of 0.73 in the internal test set and a C-index of 0.61 in the external test set, along with hazard ratios of 34.24 in the training set (95% CI: 21.7, 54.1; P < 0.001) and 8.16 in the internal test set (95% CI: 2.5, 26.8; P < 0.001). The multimodal model demonstrated a C-index of 0.76 in the internal test set and a C-index of 0.64 in the external test set. Comparative analysis against FIGO staging revealed an NRI of 0.06 (P < 0.001) for the multimodal model. The model presents opportunities for prognostic assessment, treatment strategizing, and ongoing patient monitoring.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Ovarian cancer is recognized as a highly lethal gynecologic malignancy, ranking sixth in terms of mortality rates among women1. Epithelial ovarian cancer (EOC) represents the most prevalent subtype, accounting for approximately 90% of all ovarian cancer cases. The standard treatment regimen for patients with EOC typically involves debulking surgery followed by platinum-based chemotherapy2. In the realm of clinical practice, some patients present with surgical contraindications upon initial diagnosis, rendering them ineligible for ovarian tumor debulking surgery. Furthermore, individuals who encounter recurrence following debulking surgery in conjunction with platinum-containing chemotherapy may be precluded from undergoing further tumor reduction surgery due to factors such as extensive tumor burden. In cases of postoperative recurrence and ineligibility for surgical intervention, the recommended course of treatment is platinum-based chemotherapy. However, a considerable number of patients experience relapse within three years of platinum-based chemotherapy3, with subsequent recurrences characterized by a diminishing progression-free survival (PFS)4. Despite the emergence of various treatment approaches in ovarian cancer, drug resistance has developed, leading to therapeutic refractoriness. Although bevacizumab treatment, which is a combination of the anti-angiogenic drug bevacizumab with platinum-based chemotherapy has demonstrated efficacy in extending PFS in certain patients, its utility is constrained by limitations5,6. The prognosis of EOC patients receiving bevacizumab treatment is influenced by factors such as disease stage, recurrence rate, and the development of drug resistance7. Due to the considerable expense, potential adverse effects, and notable variability in treatment effectiveness among individuals, it is imperative to develop a precise prognostic prediction model prior to initiating bevacizumab therapy.
The clinical management and prognostic evaluation of ovarian cancer are heavily reliant on the stage of the disease8. Ovarian cancer staging guidelines are established by the International Federation of Gynecology and Obstetrics (FIGO), providing a crucial framework for healthcare professionals to make prognostic assessments. It is important to note that patients with the same FIGO stage may experience varying survival rates. Carbohydrate antigen 125 (CA125) has become a prominent biomarker in ovarian cancer screening9,10, attracting significant attention and utilization in clinical practice. While it is valuable for evaluating response to chemotherapy and predicting prognosis, the clinical effectiveness of CA125 is a topic of debate11. Therefore, there is an urgent requirement to improve prognostic accuracy by integrating additional indicators.
Prior to establishing a treatment plan, ovarian cancer patients commonly undergo thorough clinical evaluations, including physical examinations, blood tests, and computed tomography (CT) scans. The amalgamation of information obtained from these various assessments plays a crucial role in predicting prognosis12,13. Nevertheless, traditional statistical approaches may face difficulties in analyzing the complex and extensive nature of multimodal data. Recent advancements in artificial intelligence have significantly enhanced the ability to analyze complex datasets14. Deep learning (DL) has emerged as a particularly promising approach within machine learning for the examination of multimodal data, eliminating the need for domain experts to manually extract or curate features15, as opposed to conventional machine learning techniques. It has the inherent ability to process raw data directly and independently generate necessary representations essential for pattern recognition, thus bypassing the explicit definition of rules or characteristics16. When provided with sufficient data points, deep learning has demonstrated superior performance compared to traditional radiological analyses17. Recent advancements in deep learning techniques have even resulted in achieving expertise comparable to experienced medical professionals in various medical image analysis tasks18,19.
This study involved the development and validation of a DL model, referred to as the risk score, utilizing preprocessed CT images of EOC tumors. The main objective was to predict the survival outcomes of EOC patients receiving bevacizumab treatment. Additionally, we investigated the potential enhancement of the model’s predictive accuracy by incorporating the CA125 biomarker.
Results
Patient baseline characteristics
From the initial cohort comprising 712 EOC patients receiving bevacizumab treatment, 127 individuals were omitted due to the unavailability of preprocessed CT plain images or suboptimal image quality, in addition to 60 patients with incomplete survival data. A comparison of baseline characteristics among the training set (N = 400), the internal test set (N = 97) and the external test set (N = 28) revealed no statistically significant differences, as depicted in Table 1.
Performance of the ResNet18 DL model
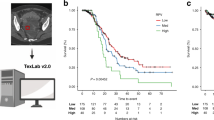
A ResNet18 DL model was developed to predict PFS predicated on tumor volume segmented from preprocessed CT plain images20. The ResNet18 DL model achieved a C-index of 0.73 for predicting PFS in the internal test set and 0.61 in the external test set. Employing the training set, risk scores were computed based on the output of the ResNet18 DL model. Patients were then categorized into high-risk and low-risk groups utilizing the optimal cutoff value derived from the risk scores generated by the ResNet18 DL model. The Kaplan–Meier survival curves presented in Fig. 1 illustrate the survival outcomes of distinct patient groups, revealing a significant difference in survival probabilities between low-risk and median- and high-risk groups (P < 0.05). Nonetheless, the deep learning model exhibits limitations in accurately distinguishing between medium and high-risk groups. The clinical attributes characterizing these patient groups were outlined in Table 2. Furthermore, Fig. 2 showcased the distribution of risk scores calculated by the ResNet18 DL model and exemplars of original images within the internal test set.
Independent predictive ability of ResNet18 DL model
As depicted in Fig. 3, regarding PFS, the multivariate Cox regression-adjusted hazard ratios (HR) pertaining to risk prediction derived from the ResNet18 DL model were determined to be 34.24 (95% CI: 21.7, 54.1; P < 0.001), 8.16 (95% CI: 2.5, 26.8; P < 0.001), surpassing those associated with FIGO stage. Analogously, comparisons of the C-index values for these variables also yielded consistent findings, as illustrated in Fig. 4.
a Multivariable Cox regression analysis between ResNet18 DL model’s risk and clinical features for PFS in the training set; b Multivariable Cox regression analysis between ResNet18 DL model’s risk and clinical features for PFS in the internal test set. The multivariate Cox regression plot shows the coefficients representing the HR (Hazard Ratio) values for each variable. The horizontal lines indicate the 95% confidence interval for the HR values. Variables that have a significant impact are represented by solid symbols, while those considered not to have a significant impact are represented by hollow circles.
This boxplot compares the performance of three models—ResNet18 DL, LightGBM, and the FIGO staging model—across different datasets: training, internal test, and external test sets. Each boxplot shows the middle 50% of the data, with the top and bottom edges representing the third quartile (Q3) and first quartile (Q1), respectively. The box height (Q3 - Q1) indicates performance variability. The line inside the box shows the median (Q2), reflecting the central tendency. Whiskers extend from the box to 1.5 times the interquartile range, capturing typical values. Points outside this range are outliers, indicating extreme values that significantly deviate from the majority of the data.
Performance of the LightGBM model
The risk score was chosen as an input for the LightGBM model. Furthermore, we augmented the model by incorporating CA125, a pertinent tumor marker, which improved the predictive capacity for PFS among EOC patients receiving bevacizumab treatment (Fig. 4). The LightGBM model achieved a C-index of 0.76 for predicting PFS in the internal test set and 0.63 in the external test set. Elevated scores corresponded to heightened progression risk. Subsequently, the progression risk score was applied to the test set to validate its efficacy. The threshold value employed for stratifying the risk score aligns with the tertiles. Patients exhibiting elevated scores demonstrated a markedly escalated risk of progression compared to those with lower scores, as demonstrated in Fig. 5.
Figure 6 elucidated the delineation and reclassification of patients exhibiting adverse prognostic outcomes based on their respective scores. Notably, the scores assigned to high-risk progression patients markedly exceeded those assigned to their low-risk counterparts. As depicted in Table 3, comparison with the conventional classification relying on FIGO staging as a prognostic measure demonstrated the LightGBM model’s notable effect on prognostic reclassification. With the LightGBM model, grounded in the anticipated progression risk subsequent to bevacizumab treatment, the Net Reclassification Improvement (NRI) reached 0.06 (P < 0.001).
a Density plot of the FIGO staging model among training set; b Density plot of the LightGBM model among training set; c Density plot of the FIGO stage model among internal test set; d Density plot of the LightGBM model among internal test set; e Density plot of the FIGO stage model among external test set; f Density plot of the FIGO stage model among external test set. The horizontal axis represents the Risk Score values, while the vertical axis represents the corresponding population density. The integral of all probability density functions equals the total number of patients.
Discussion
EOC represents a highly aggressive malignancy originating from ovarian tissues. The prognostication of EOC patients receiving bevacizumab treatment is contingent upon established indicators such as pretreatment FIGO stage21,22, disease recurrence, and treatment refractoriness, all of which significantly influence PFS outcomes. Extensive clinical investigations have underscored the considerable variability in PFS observed among EOC patients receiving bevacizumab treatment within both first- and second-line treatment contexts5,23,24. However, it is crucial to conduct additional research to determine the most effective timing and duration of bevacizumab treatment, as well as to evaluate its cost-effectiveness. Furthermore, identifying predictive markers that can differentiate between positive and negative treatment outcomes is an important area of focus. Utilizing these markers strategically has the potential to expand the range of therapeutic applications for bevacizumab and aid in selecting patient populations that will derive the greatest benefit from its use.
CT imaging plays a crucial role in modern medical practice by assisting in the development of treatment plans and the identification of medical conditions25,26. The extensive image data provided by CT scans allows for detailed analysis of various aspects of tumors in patients, such as the extent of metastasis, depth of infiltration, and spatial location27,28,29. This information is valuable for healthcare professionals in evaluating and predicting outcomes for cancer patients. Utilizing the capabilities of CT imaging, we utilized a ResNet18 deep learning model to predict PFS based on tumor volume extracted from preprocessed CT images. The ResNet18 DL model demonstrated significant predictive accuracy, as indicated by the multivariate Cox regression-adjusted hazard ratios obtained from the model. These hazard ratios were found to be 34.24 in the training set (95% CI: 21.7, 54.1; P < 0.001) and 8.16 in the internal test set (95% CI: 2.5, 26.8; P < 0.001), surpassing those associated with FIGO stage. Moreover, after accounting for relevant clinicopathologic variables such as FIGO stage, age, and CA125 levels, the risk score generated by the ResNet18 deep learning model remained a statistically significant independent predictor of patient outcomes. The subsequent stratification of patients into high-risk and low-risk groups, based on the optimal cutoff value obtained from risk scores, played a crucial role in identifying distinct survival trajectories. This was demonstrated by notable differences in survival probabilities between the two cohorts, as shown by Kaplan–Meier survival curves (P < 0.05). These results provide comprehensive validation of the prognostic utility of the ResNet18 deep learning model in informing treatment decisions for EOC patients receiving bevacizumab treatment.
Radiomics methodologies often require precise manual tumor annotation and empirical feature extraction17,30,31, which can limit the reproducibility and scalability of studies in this field. In contrast, our study employed a practical approach by carefully selecting the CT slice with the largest tumor region as the primary input for modeling. Additionally, in survival prediction research, accurately ordering survival time is crucial, unlike in image classification tasks. However, the existence of censored data within subsequent records presents a difficulty for utilizing ResNet18 deep learning models in predicting survival. Previous studies have often utilized binary classification methods to tackle this problem32,33,34. In our study, we implemented a customized loss function based on the Cox partial likelihood35,36 to address the varied range of survival risks among patients during the optimization process. This personalized loss function enabled continuous adjustments to the model parameters, with the primary goal of reducing overall loss. Additionally, we incorporated tailored loss functions related to PFS into the training dataset, allowing the ResNet18 deep learning model to capture the relevant characteristics linked to recurrence, metastasis, and mortality. This approach enhances the model’s predictive capabilities beyond individual event forecasts.
Identifying patients at high risk post-bevacizumab treatment completion continues to present a persistent challenge. The discriminative capabilities of the ResNet18 DL model’s risk score in distinguishing between high- and low-risk patients highlight its potential utility in identifying individuals at elevated risk who may benefit from more aggressive therapeutic interventions, even in cases where a favorable response is initially observed following bevacizumab treatment. Such integration of risk assessment scores could serve as a valuable adjunct to the decision-making process for these patients. The Harrell’s C-index serves as a crucial performance assessment measure for DL models, with a value of 1 indicating flawless model performance and a score of 0.5 or below suggesting inadequate performance on datasets. Therefore, a Harrell’s C-index approaching 1 indicates optimal training of the DL model. In the specific context of predicting PFS, the ResNet18 DL model achieved a Harrell’s C-index of 0.73 in the internal test set, demonstrating its noteworthy predictive accuracy.
This study introduced a LightGBM model, integrating CA125 and ResNet18 risk scores as inputs. CA125, a well-known blood biomarker, has been linked to unfavorable outcomes when found in elevated levels37. The Harrell’s C-index for the LightGBM model, in terms of predicting PFS, was calculated to be 0.76, outperforming the 0.73 achieved by the ResNet18 DL model alone. Furthermore, compared to the ResNet18 DL model, the LightGBM model can classify patients into more refined subgroups. We believe this is because while the ResNet18 DL model is trained solely on imaging data, the LightGBM model integrates both imaging and blood test features. Therefore, it can predict patient risk scores more accurately from the multimodal data, resulting in a higher c-index and evident differences in the KM curve outcomes. LightGBM builds upon the results of the ResNet18 DL model and incorporates blood test data, representing a progressive enhancement. Future research could investigate the inclusion of additional prognostic factors to further enhance the predictive accuracy of the model. In order to evaluate the effectiveness of the LightGBM model, the NRI metric was utilized to measure its ability to correctly reclassify patients compared to the established model. This metric aimed to assess how well the LightGBM model improved the classification of patient progression risk when compared to the traditional FIGO staging model. The results showed a significant NRI value of 0.06 (P < 0.001), indicating its substantial impact on prognostic reclassification when compared to the FIGO staging system.
The study is limited by factors such as its retrospective design. Additionally, the dataset used in this research may lack generalizability to populations in diverse geographic regions due to its reliance on data exclusively from the authors’ institution, potentially leading to variability in outcomes. To address these limitations, future research endeavors should prioritize external validation of the findings and incorporate data from a broader array of sources to enhance the robustness and applicability of the conclusions drawn from this study.
In conclusion, we developed and validated a DL model based on pretreatment CT imaging to prognosticate survival outcomes in EOC patients receiving bevacizumab treatment, obviating the need for manual feature extraction or selection. The risk score produced by our DL model demonstrates autonomous prognostic value and offers promise as a pretreatment risk assessment tool for the patients. While we have developed a model for EOC patients, our future research will focus on investigating deep learning prognostic methods for various subtypes of EOC. Additional validation through prospective clinical trials is necessary to confirm the effectiveness and consistency of our model in various clinical environments.
Methods
Data collection
This retrospective study was conducted in accordance with the ethical guidelines set forth in the Helsinki Declaration. Ethical approval was obtained from the Medical Ethics Committees of the First Affiliated Hospital of Anhui Medical University, the First Affiliated Hospital of Anhui Medical University High Branch and the Institutional Review Board of the Second People’s Hospital of Hefei. Given the retrospective design of the study, the need for informed consent was waived.
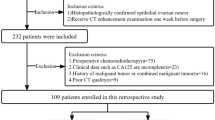
This retrospective study aimed to gather data on inoperable and recurrent EOC patients receiving bevacizumab treatment between January 2013 and January 2024 at three different medical institutions. Inclusion criteria comprised individuals meeting the following stipulations: (1) age ≥18 years; (2) histologically confirmed diagnosis of epithelial ovarian cancer; (3) FIGO stage II-IV classification; (4) Eastern Cooperative Oncology Group (ECOG) performance status ≤2; (5) absence of prior malignant neoplasms; (6) absence of concurrent severe chronic internal medical conditions; and (7) availability of clear and comprehensive CT imaging data acquired within a 2-week interval preceding the initiation of treatment.
Conversely, exclusion criteria were defined as follows: (1) age <18 years; (2) histologically confirmed non-EOC malignancies; (3) ECOG performance status >2; (4) concomitant presence of other malignancies; (5) concurrent severe chronic internal medical conditions; and (6) discernible artifacts, blurring, errors, or disordered slices evident within CT imaging. Within the initial group of 712 EOC patients receiving bevacizumab treatment, 127 individuals were eliminated from the study due to the absence of preprocessed CT plain images or suboptimal image quality, in addition to 60 patients with incomplete survival data. As a result, a total of 525 EOC patients from the designated institutions were included in the study, with 484 patients diagnosed with high-grade serous carcinoma, 21 patients with low-grade serous carcinoma, and 20 patients with clear cell carcinoma. Prior to the initiation of treatment, baseline assessments, including physical examinations, tumor marker evaluations, and CT scans, were carried out for all participants. Data collection for this investigation persisted until January 2024. The patient cohort for this study was visually represented in Figs. 7 and 8a, with a total of 400 cases from institutions 1 and 2 included in the training set, 97 cases from institutions 1 and 2 included in the internal test set, and 28 cases from institution 3 included in the external test set.
a Patient cohorts and data preprocessing. Workflow shows the development and validation of our model. b schematic diagram of the ResNet18 DL model. Diagram shows the model structure. c model validation. Flowchart shows the overall grouping and statistical analysis process, including the assessment of risk scores according to Kaplan-Meier (KM) survival analysis, Cox regression analysis and Harrell C-index.
Patient cohorts
A total of 525 EOC patients receiving bevacizumab treatment between January 2013 and January 2024 were retrospectively analyzed. As shown in Fig. 8a, regular monitoring of tumor markers was implemented during the treatment phase, with follow-up assessments conducted within 2 months post-treatment culmination. During these follow-up evaluations, comprehensive blood analyses including routine hematology, biochemical profiling, and tumor marker assessments were performed. Furthermore, efficacy evaluation entailed physical examinations and computed tomography (CT) scanning, adhering to the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines (version 1.1)38. Tumor response on CT scans was adjudicated based on the vertical length and maximum transverse thickness of the lesion. Complete response (CR) was characterized by the absence of discernible primary tumor areas, while partial response (PR) was defined as a reduction of ≥30% in the sum of diameters of all measurable target lesions, sustained for a minimum of 4 weeks relative to baseline measurements. Progressive disease (PD) was delineated by either a ≥20% increase from baseline in the sum of target lesion diameters, an absolute increase of ≥5 mm, or the emergence of new lesions. Stable disease (SD) was identified by fluctuations in lesion volume and number, exhibiting characteristics between partial response and disease progression. Post-treatment, follow-up appointments were scheduled bi-monthly in the initial year, tri-monthly in the subsequent two years, and semi-annually thereafter. Disease progression was ascertained utilizing RECIST criteria, incorporating clinical manifestations, imaging modalities, or escalating levels of CA12539.
Data preprocessing
The study systematically documented patient demographics, including variables such as age, height, weight, body mass index (BMI), ECOG performance status, pre-treatment FIGO stage, and pre-treatment blood tumor markers, as clinical attributes. The target variable of interest was PFS data. CT plain imaging data acquired prior to treatment initiation were retained for analysis. Two experienced clinicians, each with more than ten years of clinical experience, manually outlined the boundaries of the tumor on each CT slice corresponding to the EOC tumor region. Following this, a senior clinician with over twenty years of expertise reviewed and modified these outlines. For original DICOM images, we apply a windowing technique using Window Width (WW) and Window Level (WL) parameters tailored to the mediastinum window. Grayscale processed CT images undergo min-max normalization to scale pixel values to 0-1 range, followed by histogram equalization with a contrast threshold of 2.0 and a grid size of 8 × 8. This is succeeded by another round of min-max normalization before inputting data into the network. Regarding CA125 data from blood tests, values like ‘>1000’ and ‘>500’ are replaced with their respective numeric values of 1000 and 500. During model training, min-max normalization is applied to CA125 values across all cases, mapping them to the 0-1 range. The CT slice containing the largest tumor region was selected as the input for further modeling efforts (Fig. 8a).
DL model construction
A deep learning architecture, specifically Residual Network (ResNet18)40 pretrained on imagenet-1k (ImageNet: A large-scale hierarchical image database) was developed to predict PFS predicated on tumor volume segmented from preprocessed CT plain images. Patients from two different institutions were randomly divided into training and internal test subsets at an 8:2 ratio. Among them, 188 patients from institution one and 212 patients from institution two were assigned to the training set, while 45 patients from institution one and 52 patients from institution two were assigned to the internal test set (Fig. 8a). Patients from the third institution were gathered to form an external test set. The study involved conducting comparative experiments using pre-trained deep learning models, including ResNet18, ResNet50, DenseNet, and ViT, all trained on ImageNet-1K. Each experiment was repeated ten times for each model, with the model parameters saved for analysis. The ResNet18 deep learning model with the highest overall C-index was selected for further analysis. This model was then used to develop a predictive model aimed at estimating patient risk scores directly from preprocessed CT plain images depicting segmented tumors (Fig. 8b). These images encompassed a region of interest (ROI) centered on the tumor, along with a 3-pixel margin surrounding the tumor’s periphery. During the optimization phase, a customized loss function based on the Cox partial likelihood41 was utilized to address the diverse levels of survival risk among patients. This loss function enabled iterative adjustments to the model parameters with the goal of reducing overall loss. Figure 8b illustrated a schematic representation of the ResNet18 deep learning model for clarification.
Statistical analysis
The primary methodologies utilized for assessing the prognostic efficacy of the developed model were Harrell’s C-index and Kaplan–Meier survival analysis. Patients were categorized into different risk groups based on disease progression, and Kaplan–Meier survival curves were generated for each group. Disparities in survival prognosis among these groups were quantified through the calculation of P values, where P < 0.05 indicates a significant difference in survival prognosis. Kaplan–Meier survival analysis was employed to examine prognostic differences between these risk groups. Furthermore, post-hoc analyses were undertaken to discern potential associations between variables such as age, FIGO stage, CA125 levels, and various patient groups and subgroups.
As shown in Fig. 8c, a light gradient boosting machine (LightGBM)42 learning model was developed using CA125 and ResNet18 risk scores as input variables. The LightGBM model was further processed with weights to integrate multimodal data and derive a progression risk score tailored to EOC patients receiving bevacizumab treatment. Subsequently, patients were categorized into different risk groups based on disease progression, and Kaplan–Meier survival curves were generated for each group. Disparities in survival prognosis among these groups were quantified through the calculation of P values, where P < 0.05 indicates a significant difference in survival prognosis.
The comparative analysis of these models included an evaluation of the C-index of the ResNet18 DL model, the LightGBM model, and the conventional FIGO staging model, each utilized independently for prognosis prediction. This evaluation was enhanced by the incorporation of the Net Reclassification Improvement (NRI) metric43, which measured the extent to which a new model correctly or incorrectly reclassified patients compared to an existing model. The overarching objective was to assess the degree to which the model with the highest C-index in the internal test set improved the classification of patient progression risk compared to the traditional FIGO staging model. A significance threshold of p < 0.05 was employed to determine if the new model significantly enhanced the accuracy of patient progression risk classification.
Statistical analyses were performed using R 3.4.0 software. Continuous variables were assessed using t-tests, while categorical variables were analyzed using either the χ2 test or Fisher’s exact test, as deemed appropriate. The primary endpoint of interest in this study was PFS, defined as the duration from the initiation of bevacizumab treatment to either tumor progression or tumor-related death, or until the date of the last follow-up. All statistical tests were two-tailed, with significance set at a threshold of p < 0.05.
Data availability
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding authors.
Code availability
The code can be used only for non-commercial purpose and under the permission of the corresponding authors. Source code used in this study can be found at https://github.com/phaeton2017/PredictionEOC.
References
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer. J. Clin. 74, 12–49 (2024).
Armstrong, D. K. et al. Ovarian Cancer, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 19, 191–226 (2021).
Ledermann, J. A. et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 29, iv259 (2018).
Mirza, M. R. et al. Long-term safety in patients with recurrent ovarian cancer treated with niraparib versus placebo: Results from the phase III ENGOT-OV16/NOVA trial. Gynecol. Oncol. 159, 442–448 (2020).
Coleman, R. L. et al. Bevacizumab and paclitaxel-carboplatin chemotherapy and secondary cytoreduction in recurrent, platinum-sensitive ovarian cancer (NRG Oncology/Gynecologic Oncology Group study GOG-0213): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 18, 779–791 (2017).
Perren, T. J. et al. A phase 3 trial of bevacizumab in ovarian cancer. N. Engl. J. Med. 365, 2484–2496 (2011).
Haunschild, C. E. & Tewari, K. S. Bevacizumab use in the frontline, maintenance and recurrent settings for ovarian cancer. Fut. Oncol. 16, 225–246 (2020).
O’Shea, A. S. Clinical Staging of Ovarian Cancer. Methods Mol. Biol. 2424, 3–10 (2022).
Salminen, L. et al. A longitudinal analysis of CA125 glycoforms in the monitoring and follow up of high grade serous ovarian cancer. Gynecol. Oncol. 156, 689–694 (2020).
Zhang, D. et al. Serum CA125 levels predict outcome of interval debulking surgery after neoadjuvant chemotherapy in patients with advanced ovarian cancer. Clin. Chim. Acta. 484, 32–35 (2018).
Zhang, M., Cheng, S., Jin, Y., Zhao, Y. & Wang, Y. Roles of CA125 in diagnosis, prediction, and oncogenesis of ovarian cancer. Biochim. Biophys. Acta Rev. Cancer. 1875, 188503 (2021).
Boehm, K. M. et al. Multimodal data integration using machine learning improves risk stratification of high-grade serous ovarian cancer. Nat. Cancer. 3, 723–733 (2022).
Shi, M., Li, X., Li, M. & Si, Y. Attention-based generative adversarial networks improve prognostic outcome prediction of cancer from multimodal data. Brief. Bioinform. 24, bbad329 (2023).
Hollon, T. et al. Artificial-intelligence-based molecular classification of diffuse gliomas using rapid, label-free optical imaging. Nat. Med. 29, 828–832 (2023).
Truhn, D. et al. Radiomic versus Convolutional Neural Networks Analysis for Classification of Contrast-enhancing Lesions at Multiparametric Breast MRI. Radiology 290, 290–297 (2019).
Cifci, D., Foersch, S. & Kather, J. N. Artificial intelligence to identify genetic alterations in conventional histopathology. J. Pathol. 257, 430–444 (2022).
Bera, K., Braman, N., Gupta, A., Velcheti, V. & Madabhushi, A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat. Rev. Clin. Oncol. 19, 132–146 (2022).
Jin, C. et al. Predicting treatment response from longitudinal images using multi-task deep learning. Nat. Commun. 12, 1851 (2021).
Jiang, X. et al. An MRI Deep Learning Model Predicts Outcome in Rectal Cancer. Radiology 307, e222223 (2023).
Deng, J. et al. ImageNet: A large-scale hierarchical image database. In 2009 IEEE Conference on Computer Vision and Pattern Recognition, p. 248–255 (IEEE, 2009).
Xiao, Y. & Linghu, H. Survival Outcomes of Patients with International Federation of Gynecology and Obstetrics Stage IV Ovarian Cancer: Cytoreduction Still Matters. Cancer Control 30, 1379389470 (2023).
Michel, E. et al. Impact of complete surgical staging on survival of patients with early-stage (FIGO I or II) ovarian cancer: Data from the Cote d’Or Registry of Gynecological Cancers from 1998 to 2015. Bull. Cancer. 110, 352–359 (2023).
Musella, A. et al. Bevacizumab in Ovarian Cancer: State of the Art and Unanswered Questions. Chemotherapy 62, 111–120 (2017).
Oza, A. M. et al. Standard chemotherapy with or without bevacizumab for women with newly diagnosed ovarian cancer (ICON7): overall survival results of a phase 3 randomised trial. Lancet Oncol. 16, 928–936 (2015).
Sanomachi, T. & Ishiki, H. Classifying and grading liposarcoma by CT. Lancet Oncol. 25, e53 (2024).
Barat, M. et al. CT and MRI of abdominal cancers: current trends and perspectives in the era of radiomics and artificial intelligence. Jpn. J. Radiol. 42, 246–260 (2024).
Bonomi, A. et al. Diagnosis and staging of small intestinal neuroendocrine tumors with CT enterography and PET with Gallium-68: preoperative risk stratification protocol. Langenbecks Arch. Surg. 409, 63 (2024).
Maino, C. et al. Radiomics and liver: Where we are and where we are headed? Eur. J. Radiol. 171, 111297 (2024).
Rokhshad, R. et al. Deep learning for diagnosis of head and neck cancers through radiographic data: a systematic review and meta-analysis. Oral Radiol. 40, 1–20 (2024).
Yip, S. S. & Aerts, H. J. Applications and limitations of radiomics. Phys. Med. Biol. 61, R150–R166 (2016).
Taha, B., Boley, D., Sun, J. & Chen, C. Potential and limitations of radiomics in neuro-oncology. J. Clin. Neurosci. 90, 206–211 (2021).
Yang, Y., Zhou, Y., Zhou, C. & Ma, X. Deep learning radiomics based on contrast enhanced computed tomography predicts microvascular invasion and survival outcome in early stage hepatocellular carcinoma. Eur. J. Surg. Oncol. 48, 1068–1077 (2022).
Zhou, S. et al. Deep radiomics-based fusion model for prediction of bevacizumab treatment response and outcome in patients with colorectal cancer liver metastases: a multicentre cohort study. Eclinicalmedicine 65, 102271 (2023).
Liu, X. et al. Deep learning radiomics-based prediction of distant metastasis in patients with locally advanced rectal cancer after neoadjuvant chemoradiotherapy: A multicentre study. Ebiomedicine 69, 103442 (2021).
Jiang, Y. et al. Development and Validation of a Deep Learning CT Signature to Predict Survival and Chemotherapy Benefit in Gastric Cancer: A Multicenter, Retrospective Study. Ann. Surg. 274, e1153–e1161 (2021).
Katzman, J. L. et al. DeepSurv: personalized treatment recommender system using a Cox proportional hazards deep neural network. BMC Med. Res. Methodol. 18, 24 (2018).
Sharma, T. et al. Current and emerging biomarkers in ovarian cancer diagnosis; CA125 and beyond. Adv. Protein Chem. Struct. Biol. 133, 85–114 (2023).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer. 45, 228–247 (2009).
Wang, Z. et al. Apatinib treatment efficiently delays biochemical-only recurrent ovarian cancer progression. J. Ovarian Res. 14, 91 (2021).
He, K., Zhang, X., Ren, S., & Sun, J. Deep Residual Learning for Image Recognition. In 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), p. 770-778 (IEEE, 2016).
Wilson, C. M., Li, K., Sun, Q., Kuan, P. F. & Wang, X. Fenchel duality of Cox partial likelihood with an application in survival kernel learning. Artif. Intell. Med. 116, 102077 (2021).
Ke., G. et al. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. In Neural Information Processing Systems (Curran Associates Inc; 2017).
Jewell, E. S., Maile, M. D., Engoren, M. & Elliott, M. Net Reclassification Improvement. Anesth. Analg. 122, 818–824 (2016).
Acknowledgements
The authors would like to thank all participating patients.
Author information
Authors and Affiliations
Contributions
X.H.: Data curation, Methodology, Formal analysis, Investigation, Writing − original draft. Y.H.: Formal analysis, Data curation, Investigation, Resources, Writing − original draft. K.L.: Formal analysis, Data curation. F.Z.: Formal analysis, Data curation. K.X.: Visualization, Methodology, Software. Z.Z.: Project administration, Validation. P.L.: Writing − review & editing, Formal analysis, Project administration. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, X., Huang, Y., Liu, K. et al. Predicting prognosis for epithelial ovarian cancer patients receiving bevacizumab treatment with CT-based deep learning. npj Precis. Onc. 8, 202 (2024). https://doi.org/10.1038/s41698-024-00688-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-024-00688-6
- Springer Nature Limited