Abstract
Background
Little is known about the natural history of hearing loss in adults, despite it being an important public health problem. The purpose of this study is to describe the rate of hearing change per year over the adult lifespan.
Methods
The 1436 participants are from the MUSC Longitudinal Cohort Study of Age-related Hearing Loss (1988-present). Outcomes are audiometric thresholds at 250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz, averaged across right and left ears, and pure-tone average (PTA). Demographic factors are sex (female/male), race, which is categorized as white or racial Minority, and baseline age group (18-39, 40–59, 60–69, 70+ years). Linear mixed regression models are used to estimate the effect of age (per year) on the rate of threshold and PTA change.
Results
Participants’ mean age is 63.1 (SD 14.9) years, 57.7% are female, and 17.8% are racial Minority (17.1% were Black or African American). In sex-race-adjusted models, rates of threshold change are 0.42 to 1.44 dB across thresholds. Rates of change differ by sex at most individual thresholds, but not PTA. Females (versus males) showed higher rates of threshold change in higher frequencies but less decline per year in lower frequencies. Black/African American (versus white) participants have lower rates of threshold and PTA change per year. Hearing thresholds decline across the adult lifespan, with older (versus younger) baseline age groups showing higher rates of decline per year.
Conclusions
Declines to hearing occur across the adult lifespan, and the rate of decline varies by sex, race, and baseline age.
Plain language summary
Hearing loss is a common health condition, yet little is known about how hearing changes over time. In this study of 1436 individuals from across the adult lifespan, declines in hearing occurred throughout adulthood. The rate of decline per year varied by sex, in that females experienced more decline in higher pitches but less decline in lower pitches. The rate of decline per year varied by race, in that Black/African American (versus white) participants showed lower rates of hearing decline per year. The rate of decline per year also varied by age, in that older (versus younger) baseline age groups had higher rates of hearing decline per year. This study contributes to understanding of the natural history of hearing loss and could be used to better understand how to focus efforts to prevent and/or manage hearing loss across populations.
Similar content being viewed by others
Introduction
Hearing loss is a common chronic condition among middle-aged to older adults and poses an important public health problem given its wide-ranging impacts on individuals and society1,2,3,4,5,6. However, there is little information on how hearing changes over time in samples of the general population, which is likely attributable to the paucity of high-quality longitudinal studies focused on hearing7. Such data are fundamental to public health research and are needed to understand the natural history of disease, which can inform resource allocation for clinical services and public health initiatives, including those focused on hearing loss prevention. Similarly, these data could provide a benchmark for the rate of hearing change that occurs in the general population, to which individual or population-level changes in hearing could be compared. For example, these data could be used to evaluate the success of hearing loss prevention efforts, such as those to reduce exposure to occupational noise, and the public health efforts to improve cardiovascular and metabolic health and nutrition, all of which are risk factors for hearing loss1,2,8,9.
Some epidemiological studies have reported the prevalence and incidence of hearing loss in middle-aged to older adults, but fewer have detailed how hearing changes over time5,8,9,10,11,12,13,14,15. Often, hearing loss prevalence or incidence is defined by a pure-tone average (PTA) of hearing thresholds at frequencies most important for speech comprehension. While PTA is useful as a single measure of hearing acuity, definitions of PTA vary, and PTA lacks the granularity needed to comprehensively understand how hearing changes across the frequency range. Some studies have evaluated how individual hearing thresholds change over time; however, most are limited in their generalizability. For example, studies have been conducted in restricted samples, including only men11, participants without risk factors associated with hearing loss11,12,16, specific age groups, such as younger or older adults only15,17, and importantly, most studies are conducted in racially homogenous samples consisting primarily of white individuals10,11,12,13,15,16. Evaluating changes to hearing in a representative sample of the general population could improve generalizability of findings and facilitate the understanding of demographic differences in changes to hearing. Understanding the natural history of hearing loss is important because hearing loss can be at least partially prevented1,5,18,19,20,21, thus reducing its negative impacts on many middle-aged to older adults.
Evidence from cross-sectional and longitudinal epidemiological studies shows marked age and sex differences in hearing loss prevalence and incidence, and some studies show age and sex differences in longitudinal changes to hearing1,9,10,13,14. Although there is epidemiological evidence for racial differences in hearing loss prevalence, namely that Black/African American, versus white, individuals have a lower prevalence of hearing loss and a better PTA22,23,24, to our knowledge, no studies have evaluated whether there are racial differences in changes to hearing over time.
Therefore, the purpose of this study, conducted in a diverse, community-based cohort of adults across the adult lifespan, is to describe the rate of pure-tone threshold and PTA change per year, and to evaluate differences in the rate of change among demographic subgroups, including sex, race, and baseline age group. Results from this study show that hearing declines across the entire adult lifespan, and that rates of decline vary by demographic subgroups, which can contribute to our understanding of the natural history of hearing loss.
Methods
Study population
The MUSC Longitudinal Cohort Study of Age-related Hearing Loss (ARHL) is an ongoing (1988-current) community-based cohort study of ARHL based in Charleston, SC. Scientific findings from studies conducted in this cohort are presented in past publications14,25,26,27. Participants are continuously enrolled into the cohort and are recruited from the community through in-person community events, online and print advertisements, and participant referral. Participants must be aged 18 years or older, and in good general health with no evidence of conductive hearing loss or active otologic or neurologic disease. All protocols for the MUSC Longitudinal Cohort Study of ARHL were approved by the Institutional Review Board at MUSC (approval ID: E-607R). This approval covers analysis of stored data, and therefore additional IRB approval was not required for the specific study presented in this article. All participants provided informed written consent to participate in the longitudinal cohort study. All participation was voluntary, and participants could withdraw from participation at any time.
The baseline examination consists of three to six visits that include comprehensive measures of hearing, and health and hearing-related history. The battery of tests includes pure-tone audiometry, speech recognition measures in quiet and noise, middle ear measurements, otoacoustic emissions, auditory brainstem responses, and surveys focused on demographics and general and hearing-related health. Participants attend an annual follow-up visit, during which audiometric threshold data are collected. Every 2 to 3 years after baseline, participants attend a comprehensive follow-up visit where most of the measures described above, and audiometry, are repeated.
At the time of analysis, there were 1776 participants with baseline data. To be included in this longitudinal study, participants must have had audiometric data from at least two time points.
Audiometric testing
Pure-tone thresholds at frequencies 250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz were measured with a clinical audiometer equipped with TDH-39 headphones (Telephonics Corporation, Farmingdale, NY) in a sound-treated booth. All audiological equipment is calibrated annually to appropriate ANSI standards by manufacturers’ representatives28. Thresholds were measured in 5 dB steps following American Speech-Language-Hearing Association (ASHA) standards29. All audiometric testing was conducted by ASHA-certified audiologists or fourth year Au.D. externs under the supervision of the certified audiologists.
For this study, threshold values from the right and left ears were averaged, following descriptive analyses that showed similar mean threshold values in both ears. A PTA was calculated from averaged right and left ear threshold values at frequencies 500, 1000, 2000 and 4000 Hz. Outcome measures for this study were individual audiometric thresholds (250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz) and PTA.
Demographic factors
Participants reported age in years, sex (response options: female or male), and race according to US Census Bureau classifications (response options [can select all that apply]: American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, white, and other)30. Baseline age was categorized as 18–39, 40-59, 60–69, or 70+ years. Race was categorized as white, Black/African American, or other race. Analyses specifically focused on race were limited to a comparison of white and Black/African American participants only, given the small sample size of participants who were categorized as other race (described below). Participants in the other race category self-reported as Asian, American Indian or Alaska Native, and/or other.
Statistics and reproducibility
All statistical analyses were conducted in SAS version 9.4 software (Cary, NC). Four participants had missing race data, and hot-deck imputation was used to account for these missing data to ensure equal sample sizes across analyses31.
Descriptive statistics were conducted to describe the study population, including their demographics and baseline thresholds. We used chi-square for categorical variables and one-way analysis of variance for continuous variables to determine differences by baseline age, sex, race, and baseline PTA for participants that were included and excluded from this study.
Linear mixed regression models were used to estimate the effect of age (per +1 year) on the rate of change of thresholds at each frequency, separately, and PTA. Age (at each examination) was used as the repeated time measure; therefore, ‘rate’ is interpreted as rate of change per one year in age. Linear mixed models are appropriate for repeated measures data with varying lengths of follow-up time, such as these, and manage fixed (population-level) and random (subject-specific) effects. Fixed effect parameters are shared by the study population, whereas random effect parameters can vary across individuals, reflecting the natural heterogeneity of the sample and accounting for within-individual clustering of data points32.
First, we built unadjusted regression models, which are presented in the Supplementary Materials, as discussed later. Next, we built regression models adjusted for sex and race. Results from regression models are presented as Beta coefficients with corresponding 95% confidence intervals (95% CI). We also evaluated differences between demographic factors by i) stratifying models by sex, race (white versus Black/African American), and baseline age groups, and ii) including interaction terms of the demographic factor and age (longitudinal time variable) in final models. Statistical significance was defined by an alpha level of p < 0.05.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Of the 1776 participants with baseline data, 1436 met the eligibility criteria described above and were included in this study. Participants included in this study (versus not included) were more likely to be older (p < 0.0001), white (p = 0.0021) and have a higher (worse) PTA (p = 0.0178) but did not differ by sex (p = 0.0598).
Table 1 shows baseline characteristics of the 1436 participants. Participants’ mean baseline age was 63.1 (SD 14.9; range 18–89 + ), 57.7% were female, and 17.8% were Minority (17.1% of the sample was Black/African American). The mean number of audiograms was 8.3; details on the year of baseline examinations are also in Table 1. Additional non-demographic baseline study sample characteristics and their corresponding definitions are in Supplementary Table 1.
Baseline thresholds and PTA for the entire study sample are in Table 1. Baseline thresholds stratified by sex and race, and baseline age group, are in Tables 2 and 3, respectively. The baseline thresholds for sex and race by age group are in Supplementary Table 2.
Changes to pure-tone thresholds and PTA
Table 4 displays sex- and race-adjusted average rates of threshold and PTA change per year. In these adjusted models, rates of threshold change per year ranged from 0.42 to 1.44 dB across frequencies. In general, the rate of threshold change per year was less for lower frequencies and was more for higher frequencies. The rate of PTA change per year was 0.83 (95% CI 0.79, 0.86) dB.
Rate of threshold and PTA change per year by sex
Figure 1 shows race-adjusted average rates of threshold and PTA change per year for females and males, separately. The corresponding numerical estimates are in Supplementary Table 3. Females had lower baseline thresholds for all reported frequencies except 250 and 500 Hz, and a lower PTA (Table 2). Across all frequencies, the rate of threshold change per year ranged from 0.41 to 1.53 dB for females, and 0.42 to 1.31 dB for males. Compared to females, males generally show a higher rate of change per year at frequencies below 3000 Hz and a lower rate of change at frequencies 3000 Hz and above. Females show a significantly higher rate of change per year at frequencies 4000, 6000, and 8000 Hz, and a significantly lower rate of change at 2000 Hz. The rate of PTA change per year was not significantly different for females and males (Supplementary Table 3).
Results are presented as Beta coefficients with corresponding 95% confidence intervals (error bars) for female (blue circles; n = 828) and male (green squares; n = 608) participants. Estimates are adjusted for race. *p < 0.05; significance determined by including age*sex interaction term in models. PTA pure-tone average, calculated from frequencies 500, 1000, 2000 and 4000 Hz averaged across right and left ears.
Rate of threshold and PTA change per year by race
Average rates of threshold and PTA change per year, stratified by race and adjusted for sex, are displayed in Fig. 2, with the corresponding numerical estimates in Supplementary Table 4. Black/African American, versus white, participants had lower baseline thresholds for all reported frequencies, although the threshold at 250 Hz was similar (within 0.5 dB), and thus a lower PTA (Table 2). Rates of change per year across all frequencies ranged from 0.44 to 1.46 dB for white participants, and 0.30 to 1.27 dB for Black/African American participants. Black/African American participants had lower rates of change per year at all frequencies and PTA, as compared to white participants. Rates of change were significantly smaller for Black/African American (versus white) participants at 250, 1000, 2000, 3000, and 6000 Hz, and for PTA (Supplementary Table 4).
Results are presented as Beta coefficients with corresponding 95% confidence intervals (error bars) for white (blue circles; n = 1180) and Black/African American (green squares; n = 246) participants. Estimates are adjusted for sex. *p < 0.05; significance determined by including age*race interaction term in models. Participants who were not white or Black/African American race (categorized as other race) were excluded from these analyses given the small sample size (n = 10; see Table 1). PTA: pure-tone average, calculated from frequencies 500, 1000, 2000 and 4000 Hz averaged across right and left ears. AA: African American.
Rate of threshold and PTA change per year by baseline age group
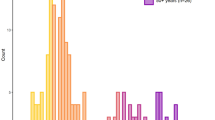
Figure 3 shows average sex- and race-adjusted rates of threshold and PTA change per year, stratified by baseline age group. The corresponding numerical estimates are in Supplementary Table 5. At each frequency, baseline thresholds increased by baseline age group (Table 3). In general, younger age groups showed smaller rates of threshold and PTA change per year. Consistent with the results described above, average rates of change per year were generally smaller for lower frequencies and more for higher frequencies (Supplementary Table 5).
Results are presented as Beta coefficients with corresponding 95% confidence intervals (error bars) for participants aged 18–39 (blue circles; n = 154), 40-59 (orange squares; n = 231), 60-69 (green triangles; n = 547) and 70+ (grey Xs; n = 504) years at the baseline examination. Estimates are adjusted for sex and race. *p < 0.05; significance determined by including age*baseline age interaction term in models. PTA: pure-tone average, calculated from frequencies 500, 1000, 2000 and 4000 Hz averaged across right and left ears.
Supplementary Table 6 shows average rates of threshold and PTA change per year, stratified by baseline age group, then sex and race, separately. Estimates stratified by baseline age group, then sex, are plotted in Supplementary Fig. 1. In terms of sex, average rates of threshold change are generally similar for females and males among 18–39- and 40–59-year age groups. In the 60–69-year group, males show higher average rates of threshold change at 1000 and 2000 Hz, whereas females show higher rates of change at 4000 Hz and above. In the 70+ year group, males show higher rates of threshold change at 250 Hz, whereas females show higher rates of change at 3000 and 4000 Hz. In terms of race, Black/African American participants generally have lower rates of threshold change across all age groups than white participants.
Supplementary unadjusted models
Unadjusted estimates, overall and stratified by sex, race, and baseline age group, are in Supplementary Tables 7 through 10. In general, adjustment for demographic factors did not substantially change effect estimates, and unadjusted and adjusted models showed the same trends, as presented above.
Discussion
This study described the average rate of threshold and PTA change per year in a diverse community-based sample of adults across the adult lifespan, overall and stratified by sex, race, and baseline age group. In this sample, the rate of threshold change ranged from 0.42 to 1.44 dB per year, and findings suggest that hearing declines across the entire adult lifespan. Key findings from stratified analyses include: i) average rates of hearing declines differed by sex; these differences were observed across most individual thresholds, but not PTA, ii) Black/African American participants had a lower rate of threshold and PTA change per year as compared to white participants, and iii) in general, hearing declined across the adult lifespan, although older (versus younger) age groups had higher rates of threshold and PTA declines per year.
To compare our results to those from other studies, it is first necessary to highlight important differences in study methodologies and sample compositions, in terms of age, sex, and race, which can influence the comparability of results. The rates of threshold change per year reported in this study (0.42 to 1.44 dB) are similar to results from an earlier study conducted in 188 participants from the same cohort, which reported the rates of change to be 0.7 to 1.2 dB per year across frequencies14. The slight discrepancies in estimates can likely be explained by the present study having a larger sample size with more follow-up time, a wider age range, and more Minority (namely, Black/African American) participants. Studies conducted in other cohorts have also reported rates of threshold change that are generally consistent with findings from this study. For example, a study conducted in males aged 20 to 95 years and with 11 years of follow up reported rates of threshold change as 0.7 to 1.7 dB per year12. Next, a study in younger adults (31 to 50 years) reported the 5-year rates of threshold change as 0 to 2.5 dB across frequencies15, which are similar to the estimates presented for 18- to 40-year-olds in this study if estimated over 5 years. Two studies conducted in 60 to 80+ and <30 to 80+ year old adults reported the rates of threshold change to be 1 to 15 dB in 6 years and 0 to 18 dB in 10 years, respectively12,13. As compared to the present study, those studies reported greater rates of change in the high frequencies. Differences in the rates of high-frequency threshold change may be explained by differences in sample composition, namely that other samples did not include a substantial proportion of Minority participants. In addition to demographic differences in sample composition, there may be cohort differences in exposures to risk factors for hearing loss, such as excessive noise or cardiovascular or metabolic ill-health, which would contribute to differences in estimated rates of change33,34,35,36. There may also be birth cohort (generational) differences across cohorts, which would likely influence rates of hearing decline19. To facilitate comparison of results from this study with those from the previous studies described above, we assessed differences in rate of hearing change by demographic factors, but did not assess other risk factors for hearing loss. This point will be discussed later.
Previous studies have consistently shown hearing loss prevalence and incidence is higher in males1,2,8,9, and that hearing loss onset in men occurs earlier than it does in females9. In this study, there were clear sex differences in rates of threshold change per year, in that females had higher rates of change in the higher frequencies, but men had higher rates of change in some lower frequencies. This is likely because hearing in males has already declined and the thresholds in males are closer to the limits of hearing, particularly for the high frequencies, where hearing loss often presents first37. This is supported by the results showing males have higher baseline thresholds at higher frequencies than females (Table 2) and that this trend exists across all age groups (Supplementary Table 2). In general, this notion is also supported by the results shown in Supplementary Fig. 1. That is, males aged 18 to 39 years at baseline showed significantly (6000 Hz) or non-significantly higher rates of threshold change than females. The pattern where females had higher rates of change in the higher frequencies emerges in the 60- to 69-year baseline age group. Among 60- to 69-year-olds at baseline, females show significantly higher threshold change at 4000 to 8000 Hz, and among 70+ year olds at baseline, females show significantly higher threshold change at 3000 and 4000 Hz, suggesting that changes to hearing among females progress to the lower frequencies as baseline age increases. Studies conducted in other cohorts similarly reported rates of decline are higher for females than males, particularly in the higher frequencies10,13,14. In this study, sex differences were not observed for rate of PTA change. This suggests that using an average, such as PTA, may mask the sex differences in rate of change observed at individual frequencies.
In this study, white participants showed higher rates of threshold change than Black/African American participants across all frequencies and PTA and had higher average baseline thresholds overall and at most frequencies across each group. Results are consistent with research showing Black/African American individuals have better pure-tone thresholds and a lower prevalence of hearing loss23,24,38. To our knowledge, this is the first study to report racial differences in rates of hearing change in a sample of the general population. Our analyses focused on racial differences were limited to white and Black/African American participants given low sample sizes of participants of other races. Previous research indicates there are differences in the prevalence of hearing loss among other racial and ethnic groups, including non-white Hispanic and Asian individuals22,23,24,38,39,40,41. There is a need for future epidemiological hearing research, including how hearing changes over time, to be conducted in diverse samples of the general population.
In general, rates of threshold and PTA change per year were higher in older age groups, which was rather consistent across all thresholds. However, in participants aged 70 years or older, the rates of change in the higher frequencies were lower and were similar to rates of change for participants aged 40 to 59 years. One explanation for this is that, as mentioned above, hearing at the higher frequencies among older people may have already declined and thresholds may be approaching the limits of hearing. This is reflected by the higher baseline thresholds for participants aged 70 or older, particularly at high frequencies (Table 3). Findings from analyses stratified by baseline age group indicate hearing declines across the adult lifespan. Furthermore, findings indicate older individuals experience high rates of threshold decline across the frequency range. These findings are consistent with other cohort studies that have shown older adults experience high rates of hearing declines10,11,12,13,14.
In this study, we present rates of hearing change adjusted for and stratified by demographic factors to understand rates of hearing change in the general population, regardless of the sample’s non-demographic risk factors. Considering only demographic factors is common in studies that describe changes to hearing over time5,8,9,10,11,12,13,14,15, and allows authors to comprehensively describe changes to hearing across demographic subgroups. Importantly, as described above, this study overcomes several critical limitations of previous studies that, for example, were conducted only in men11, in younger or older adults15,17, in individuals without risk factors for hearing loss, such as noise exposure11,12,16, and in samples of primarily white individuals10,11,12,13,15,16. Although there are some limitations to this cohort (discussed below), this is one of the only studies to comprehensively describe changes to hearing in a diverse sample of the general population from across the lifespan.
The goal of this study was to describe the rate of hearing decline across the adult lifespan, rather than to determine the reasons for decline. However, it is important to note that the observed demographic differences in the rate of hearing decline may, in part, capture differences in exposure to risk factors for hearing loss. That is, demographic factors may be surrogate measures for other risk factors for hearing loss. For example, white males are more likely to experience noise exposure than Black/African American males or females of any race42,43,44. Furthermore, there are sex, race, and age differences in other risk factors for hearing loss, including nutrition and metabolic and cardiovascular health45,46,47. Several other longitudinal studies have determined risk factors associated with hearing loss incidence or progression, such as noise exposure, nutrition, and factors related to metabolic and cardiovascular health, and have concluded that ARHL is at least partially preventable5,8,19,48,49. Future research should evaluate associations of modifiable risk factors with the rate of hearing decline. Such research is crucial to informing public health initiatives related to hearing loss prevention.
Data on the rate of hearing change in the general population, such as these, could provide a benchmark for the rate of hearing change that occurs in the general population. These data also have implications towards screening for ARHL in the general population. A recent report from the US Preventive Services Task Force concluded there was insufficient evidence to support screening for ARHL in asymptomatic adults aged 50 years and older50. However, some guidance related to screening for ARHL suggests that screening could begin at age 50 or age 65 years51,52. In the current study, the mean baseline PTAs of participants aged 40–59 and 60–69 years were 18 dB HL and 24 dB HL, respectively. Among participants aged 50–59 years (results not shown), the mean baseline PTA was 18 dB HL. Therefore, results from this study are consistent with guidance that screening for ARHL could begin at 50 years of age to detect early cases of hearing loss, and that screening at 65 years of age could detect more severe cases of hearing loss. Importantly, definitions of hearing loss vary across sources51,52, and there is ongoing discussion on how hearing loss should be defined53. Future research is needed to determine the appropriate age to begin screening using the definitions of hearing loss designated by the agencies recommending screening.
Strengths of this community-based cohort study spanning 35 years include its large and diverse sample and comprehensive measures of hearing, and its longitudinal design. This cohort study is similar to other epidemiological studies of ARHL in terms of age and audiometric hearing loss, which may enhance generalizability of study findings2,25,54. However, some limitations exist. Most participants in this study were white or Black/African American, so differences in the rate of hearing changes by other races could not be evaluated. Research suggests there are differences in the prevalence of hearing loss by race and ethnicity, which this study could not evaluate22,23,24,38,39,40,41. While this community-based sample is conducted in individuals from the general population, results may not be generalizable to the entire population, as participants reside in one geographic region and have relatively high socioeconomic position. It was not possible to evaluate sex- and race-specific rates of change by age group given sample size limitations.
This descriptive study conducted in a diverse, community-based sample of the general population from across the adult age range suggests that declines to hearing occur across the adult lifespan, and that the rate of decline varies by sex, race, and baseline age group. To the authors’ knowledge, this is the first study to document the rate of hearing change per year is lower in Black/African American individuals. Findings from this study highlight the need to prioritize the prevention and/or management of hearing loss in individuals across the adult lifespan and can provide a benchmark for comparing individual or population-level declines to hearing.
Data availability
Data are not publicly available to protect privacy of study participants. Deidentified participant data are available upon reasonable request to the corresponding author under a data use agreement.
Code availability
Code is not publicly available due to institutional restrictions and the sensitive nature of the data and associated analysis code. The code can be made available from the corresponding author upon reasonable request.
References
Nash, S. D. et al. The prevalence of hearing impairment and associated risk factors: the Beaver Dam Offspring Study. Arch. Otolaryngol. Head Neck Surg. 137, 432–439 (2011).
Cruickshanks, K. J. et al. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin: The Epidemiology of Hearing Loss Study. Am. J. Epidemiol. 148, 879–886 (1998).
Strawbridge, W. J., Wallhagen, M. I., Shema, S. J. & Kaplan, G. A. Negative consequences of hearing impairment in old age: a longitudinal analysis. Gerontologist. 40, 320–326 (2000).
Dalton, D. S. et al. The impact of hearing loss on quality of life in older adults. Gerontologist. 43, 661–668 (2003).
Dalton, D. S. et al. Cadmium, obesity, and education, and the 10‐year incidence of hearing impairment: The Beaver Dam Offspring Study. Laryngoscope. 130, 1396–1401 (2020).
McDaid, D., Park, A. L. & Chadha, S. Estimating the global costs of hearing loss. Int. J. Audiol. 60, 162–170 (2021).
Blazer, D. G., Domnitz, S., & Liverman, C. T., National Academies of Sciences, Engineering, and Medicine. Hearing health care services: Improving access and quality. Hearing Health Care for Adults: Priorities for Improving Access and Affordability. 6 (2016).
Cruickshanks, K. J. et al. The 5-year incidence and progression of hearing loss: the Epidemiology of Hearing Loss Study. Arch. Otolaryngol. Head Neck Surg. 129, 1041–1046 (2003).
Cruickshanks, K. J. et al. Education, occupation, noise exposure history and the 10-yr cumulative incidence of hearing impairment in older adults. Hear. Res. 264, 3–9 (2010).
Wiley, T. L., Chappell, R., Carmichael, L., Nondahl, D. M. & Cruickshanks, K. J. Changes in hearing thresholds over 10 years in older adults. J. Am. Acad. Audiol. 19, 281–292 (2008).
Brant, L. J. & Fozard, J. L. Age changes in pure‐tone hearing thresholds in a longitudinal study of normal human aging. J. Acoust. Soc. Am. 88, 813–820 (1990).
Pearson, J. D. et al. Gender differences in a longitudinal study of age‐associated hearing loss. J. Acoust. Soc. Am. 97, 1196–1205 (1995).
Gates, G. A. & Cooper, J. C. Incidence of hearing decline in the elderly. Acta. Otolaryngol. 111, 240–248 (1991).
Lee, F. S., Matthews, L. J., Dubno, J. R. & Mills, J. H. Longitudinal study of pure-tone thresholds in older persons. Ear Hear. 26, 1–11 (2005).
Karlsmose, B., Lauritzen, T., Engberg, M. & Parving, A. A five-year longitudinal study of hearing in a Danish rural population aged 31–50 years. Br. J. Audiol. 34, 47–55 (2000).
Morrell, C. H., Gordon‐Salant, S., Pearson, J. D., Brant, L. J. & Fozard, J. L. Age‐and gender‐specific reference ranges for hearing level and longitudinal changes in hearing level. J. Acoust. Soc. Am. 100, 1949–1967 (1996).
Møller, M. B. Hearing in 70 and 75 year old people: results from a cross sectional and longitudinal population study. Am. J. Otolaryngol. 2, 22–29 (1981).
Zhan, W. et al. Modifiable determinants of hearing impairment in adults. Prevent. Med. 53, 338–342 (2011).
Paulsen, A. J. et al. Incidence of hearing impairment and changes in pure-tone average across generations. JAMA Otolaryngol. Head Neck Surg. 147, 151–158 (2021).
Cruickshanks, K. J. et al. Cigarette smoking and hearing loss: the Epidemiology of Hearing Loss Study. JAMA. 279, 1715–1719 (1998).
Gopinath, B. et al. The effects of smoking and alcohol consumption on age-related hearing loss: the Blue Mountains Hearing Study. Ear Hear. 31, 277–282 (2010).
Cruickshanks, K. J. et al. Hearing impairment prevalence and associated risk factors in the Hispanic Community Health Study/Study of Latinos. JAMA Otolaryngol. Head Neck Surg. 141, 641–648 (2015).
Agrawal, Y., Platz, E. A. & Niparko, J. K. Prevalence of hearing loss and differences by demographic characteristics among US adults: Data from the National Health and Nutrition Examination Survey, 1999-2004. Arch. Intern. Med. 168, 1522–1530 (2008).
Lin, F. R. et al. Association of skin color, race/ethnicity, and hearing loss among adults in the USA. J. Assoc. Res. Otolaryngol. 13, 109–1017 (2012).
Dubno, J. R. et al. Longitudinal changes in speech recognition in older persons. J. Acoust. Soc. Am. 123, 462–475 (2008).
Matthews, L. J., Lee, F. S., Mills, J. H. & Dubno, J. R. Extended high-frequency thresholds in older adults. J. Speech Lang. Hear. Res. 40, 208–214 (1997).
Simpson, A. N., Matthews, L. J., Cassarly, C. & Dubno, J. R. Time from hearing-aid candidacy to hearing-aid adoption: A longitudinal cohort study. Ear Hear. 40, 468–476 (2019).
American National Standards Institute (ANSI). American National Standard Specifications for Audiometers. ANSI S2.6-2018. (Revision of ANSI S3.6-2010, revision of ANSI S3.6-2004, revision of ANSI S3.6-1996, Revision of ANSI S3.6-1989, Revision of ANSI S3.6-1969). (2018).
American Speech-Language-Hearing Association. Guidelines for manual pure-tone threshold audiometry. Retrieved from https://www.asha.org/policy/gl2005-00014/ (2005).
US Census Bureau. About the topic of race. Retrieved from: https://www.census.gov/topics/population/race/about.html. (2022).
Andridge, R. R. & Little, R. J. A review of hot deck imputation for survey non‐response. Int. Stat. Rev. 78, 40–64 (2010).
Pinheiro, J. C., & Bates, D. M. Linear mixed-effects models: basic concepts and examples. Mixed-effects models in S and S-Plus. 3-56 (2000).
Dalton, D. S., Cruickshanks, K. J., Klein, R., Klein, B. E. & Wiley, T. L. Association of NIDDM and hearing loss. Diabetes Care. 21, 1540–1544 (1998).
Austin, D. F. et al. Diabetes‐related changes in hearing. Laryngoscope. 119, 1788–1796 (2009).
Gates, G. A., Cobb, J. L., D’Agostino, R. B. & Wolf, P. A. The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Arch. Otolaryngol. Head Neck Surg. 119, 156–161 (1993).
Fischer, M. E. et al. Subclinical atherosclerosis and increased risk of hearing impairment. Atherosclerosis. 238, 344–349 (2015).
Ruben, R. J. The developing concept of tonotopic organization of the inner ear. J. Assoc. Res. Otolaryngol. 21, 1–20 (2010).
Helzner, E. P. et al. Race and sex differences in age‐related hearing loss: The Health, Aging and Body Composition Study. J. Am. Geriatr. Soc. 53, 2119–2127 (2005).
Hoffman, H. J., Dobie, R. A., Losonczy, K. G., Themann, C. L. & Flamme, G. A. Declining prevalence of hearing loss in US adults aged 20 to 69 years. JAMA. Otolaryngol. Head Neck Surg. 143, 274–285 (2017).
Choi, J. S., Kari, E., Friedman, R. A. & Fisher, L. M. Prevalence of hearing loss and hearing care use among Asian Americans: A nationally representative sample. Otol. Neurotol. 39, 158–167 (2018).
Lor, M., Thao, S. & Misurelli, S. M. Review of hearing loss among racial/ethnic minorities in the United States. West. J. Nurs. Res. 43, 859–876 (2021).
Ishii, E. K. & Talbott, E. O. Race/ethnicity differences in the prevalence of noise-induced hearing loss in a group of metal fabricating workers. J. Occup. Environ. Med. 40, 661–666 (1998).
Henselman, L. W. et al. Effects of noise exposure, race, and years of service on hearing in US Army soldiers. Ear Hear. 1, 382–391 (1995).
Eng, A. et al. Gender differences in occupational exposure patterns. Occup. Environ. Med. 68, 888–894 (2011).
Bennett, E., Peters, S. A. & Woodward, M. Sex differences in macronutrient intake and adherence to dietary recommendations: Findings from the UK Biobank. BMJ Open. 8, e020017 (2018).
Appelman, Y., van Rijn, B. B., Ten Haaf, M. E., Boersma, E. & Peters, S. A. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis. 241, 211–218 (2015).
Pradhan, A. D. Sex differences in the metabolic syndrome: implications for cardiovascular health in women. Clin. Chem. 60, 44–52 (2014).
Johnson, A. C. et al. Influence of well-known risk factors for hearing loss in a longitudinal twin study. Int. J. Audiol. 56, 63–73 (2017).
Gopinath, B. et al. Dietary antioxidant intake is associated with the prevalence but not incidence of age-related hearing loss. J. Nutr. Health Aging. 15, 896–900 (2011).
US Preventive Services Task Force. Screening for hearing loss in older adults. JAMA. 325, 1196–1201 (2021).
World Health Organization. Hearing screening: Consideration for implementation. World Health Organization: Geneva, Switzerland (2021).
Royal Australian College of General Practitioners. Guidelines for preventive activities in general practice. 9th edition, updated. East Melbourne, Vic: RACGP (2018).
Gatlin, A. E. & Dhar, S. History and lingering impact of the arbitrary 25-dB cutoff for normal hearing. Am. J. Audiol. 30, 231–234 (2021).
Gates, G. A., Cooper, J. C., Kannel, W. B. & Miller, N. J. Hearing in the elderly: The Framingham Cohort, 1983-1985: Part 1. Basic audiometric test results. Ear Hear. 11, 247–256 (1990).
Acknowledgements
This work was funded (in part) by the National Institutes of Health/National Institute on Deafness and Other Communication Disorders Individual Postdoctoral Fellowship Grant (F32 DC021078), Institutional Training Grant (T32 DC014435) and Clinical Research Center (P50 DC 000422) awarded to the Medical University of South Carolina and by the South Carolina Clinical and Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, NIH/NCATS Grant number UL1 TR001450. This investigation was conducted in a facility constructed with support from Research Facilities Improvement Program Grant Number C06 RR14516 from the NIH/NCRR.
Author information
Authors and Affiliations
Contributions
L.K.D. Conceptualization, methodology, formal analysis, writing-original draft, visualization. L.J.M. Resources, data curation, writing-review & editing, project administration. L.M. methodology, writing-review & editing. A.N.S. methodology, writing-review & editing. J.R.D. Conceptualization, methodology, resources, writing-review & editing, supervision, project administration, funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dillard, L.K., Matthews, L.J., Maldonado, L. et al. Demographic factors impact the rate of hearing decline across the adult lifespan. Commun Med 4, 171 (2024). https://doi.org/10.1038/s43856-024-00593-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-024-00593-w
- Springer Nature Limited