Abstract
Background
Calcified band keratopathy is a chronic degenerative disease characterized by the deposition of gray to white opacity in superficial layers of the cornea that typically develops over months or years. It is associated with a variety of conditions, including chronic uveitis.
Purpose
The objective of this study is to assess visual acuity and corneal changes in patients with band keratopathy secondary to uveitis who underwent phototherapeutic keratectomy (PTK).
Setting
The place where this study was performed was in the Department of Ophthalmology and Visual Sciences, Federal University of Sao Paulo.
Design
This is a retrospective study.
Methods
Patients with uveitic band keratopathy were submitted to PTK. The PTK was performed using Allegreto Wave EX500, with the ablation area of 6 mm.
Results
Twelve patients (13 eyes) diagnosed with band keratopathy secondary to chronic uveitis were analyzed. Of the 12 patients, 8 patients were female (66 %), aged 22 years (7–53 years). From the 12 patients (13 eyes) evaluated in this study, only one patient (one eye) did not have visual improvement, due to epithelial deposits 2 weeks after PTK, and all the others benefited with the procedure. In the children group, all eyes had visual improvement, and quantitatively speaking, the children had a more significant improvement than adults.
Conclusions
PTK is a safe and effective procedure even for children. However, the improvement in visual acuity was restricted due to other ocular changes secondary to uveitis, such as cataract and retinal changes, or even the corneal irregularity.
Similar content being viewed by others
Background
Calcified band keratopathy is a chronic degenerative disease characterized by the deposition of gray to white opacity in superficial layers of the cornea, more frequently at interpalpebral zone that typically develops over months or years. Although it can occur as an idiopathic form, it is associated with a variety of conditions, including chronic uveitis [1, 2, 3, 4].
Treatment includes removal of calcium deposits with either ethylenediaminetetraacetic (EDTA), superficial keratectomy or phototherapeutic keratectomy (PTK), indicated for improvement of visual acuity and ocular discomfort caused by band keratopathy [5, 6].
The phototherapeutic keratectomy is an effective treatment for various disorders of the corneal surface, among them the band keratopathy. Irregularity of the corneal surface, epithelial instability, and superficial opacification may benefit from the procedure [1, 5]. This study was to assess visual acuity and corneal changes in patients with band keratopathy secondary to uveitis who underwent PTK.
Methods
Retrospective study which analyzed patients with uveitic band keratopathy treated at the Uveitis Sector from the Department of Ophthalmology and Visual Sciences, Federal University of Sao Paulo, Paulista School of Medicine (São Paulo Hospital), between January and December 2013.
Patients underwent eye examination consisting of measuring visual acuity with pinhole, intraocular pressure (Goldmann tonometer), ectoscopy, biomicroscopy, and fundoscopy under mydriasis by indirect ophthalmoscopy lens of 20 diopters before and after 30 days of treatment. Those patients with a significant keratopathy in the visual axis, contributing to reduced vision, with pachymetry greater than 450 μm, with a maximum lesion depth of 100 μm, were chosen to undergo the PTK.
The PTK was the first option of treatment for these patients, all surgeries were performed under topical anesthesia, using Allegreto Wave EX500, with the ablation area of 6 mm. The procedure was performed aseptically. The corneal ablation is performed either by asking the patient to look at the light emitted by the device or manually focused laser. After using 70 to 80 % of the target ablation, the patient was examined at the slit lamp, to protect excess ablation of thin areas and decide on the need for additional treatment. At the end of the procedure, we put a bandage soft contact lens for 7 days and eye drops of antibiotic and corticosteroid [3, 5].
The protocol was approved by the Universidade Federal de São Paulo Research Ethics Committee and an informed consent was obtained.
Results
Twelve patients (13 eyes) diagnosed with band keratopathy secondary to chronic uveitis were analyzed. Of the 12 patients, 8 patients were female (69.2 %), aged 22 years (61.5 % less than 18 years old, 23.1 % between 18 and 40 years old, and 15.4 % more than 40 years old).
One patient had posterior uveitis secondary to acute retinal necrosis (7.7 %), four panuveitis secondary to Vogt Koyanagi Harada syndrome (30.8 %), one intermediate uveitis (7.7 %), seven had anterior uveitis, three of them secondary to juvenile idiopathic arthritis (23.1 %), and four idiopathic anterior uveitis (30.8 %).
Before PTK was performed, 38.5 % of the patients had visual acuity between 20/50 and 20/200, and the other 61.5 % had worse than 20/200. After the PTK, 23 % had visual acuity 20/40 or better, 31 % between 20/50 and 20/200, and 46 % had worse than 20/200 (Figs. 1, 2, 3, and 4).
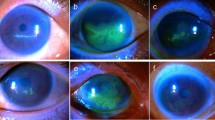
In the children group, all eyes had visual improvement. From the 12 patients (13 eyes) evaluated in this study, only 1 patient (one eye) did not have visual improvement, due to epithelial deposits 2 weeks after PTK (Figs. 5 and 6); all the others benefited with the procedure.
All the patients had central cornea involved and obtained central corneal clarity post treatment. Other relevant diseases detected were cataract and retinal changes.
Although the results were positive, there was no statistical significance between the variable final visual acuity and gender, age, or diagnosis (Tables 1 and 2).
Discussion
The mechanism of calcium deposition in the cornea is unknown, but it may result from precipitation left as tears evaporate, degeneration and necrosis from inflammatory diseases, changes in the pH, and the breakdown of phosphates [1, 2, 7]. This calcified material deposits at the Bowman’s membrane level [3, 4]. This study showed the benefits of excimer laser to achieve this layer, without manual error, in patients with chronic inflammatory diseases.
The excimer ablation allows precise tissue removal over wide areas of cornea without trauma to adjacent tissue, and this smoothing of the ocular surface after PTK may increase tear film stability, which may reduce the chances of recurrence and this regular tear film and cornea interface results in a better optical surface [2–4]. Stewart and colleagues showed that significant recurrence of band keratopathy was not seen in 2 years following PTK [5].
The main downside of the excimer laser ablation is that it does not discriminate between abnormalities, such as calcium, and normal stroma, and if the calcium deposits are not uniform, it can keep the irregular surface [2]. So, it is important to protect the healthy cornea of the laser and fill the irregularities with masking substances, such as balanced salt solution (BSS), avoiding this situation.
The main goal of PTK is to increase corneal transparency, providing visual rehabilitation, and prevent development of amblyopia in children [4].
The refractive changes after PTK can be variable, with myopic or hyperopic shifts, which can be corrected with spectacles or contact lenses [2, 6]. Other limit is the high cost of treatment [2].
Conclusions
In summary, the PTK is a safe and effective procedure even for children. However, the improvement in visual acuity was restricted due to other ocular changes secondary to uveitis, such as cataract and retinal changes, or even the corneal irregularity. And the challenge is to keep inflammation under control because this chronic stimulus is an important risk factor for recurrence of band keratopathy.
References
Moisseiev E, Gal A, Addadi L, Caspi D, Shemesh G, Michaeli A (2013) Acute calcific band keratopathy: case report and literature review. J Cataract Refract Surg 39:292–294
Jhanji V, Rapuano CJ, Vajpayee RB (2011) Corneal calcific band keratopathy. Curr Opin Ophthalmol 22:283–289
Stewart OG, Morrell AJ (2003) Management of band keratopathy with excimer phototherapeutic keratectomy: visual, refractive, and symptomatic outcome. Eye 17:233–237
Galor A, Leder HA, Thorne JE, Dunn JP (2008) Transient band keratopathy associated with ocular inflammation and systemic hypercalcemia. Clin Ophthalmol 2(3):645–647
Rathi VM, Vyas SP, Sangwan VS (2012) Phototherapeutic keratectomy. Indian J Ophthalmol 60:5
Rathi VM, Vyas SP, Vaddavalli PK, Sangwan VS, Murthy SI (2010) Phototherapeutic keratectomy in pediatric patients in India. Cornea 29:1109–1112
Kollias AN, Spitzlberge GM, Thurau S, Grüterich M, Lackerbauer CA (2007) Phototherapeutic keratectomy in children. J Refract Surg 23:703
Acknowledgements
We acknowledge Jacqueline Martins who helped during the procedures. There was no funding for this study.
The article has not been presented in a meeting. The authors did not receive any financial support from any public or private sources. The authors have no financial or proprietary interest in a product, method, or material described herein.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MKY, MCM, and DG followed patients and performed the procedures. HN, GHAS, CF, CM, and RBJ conceived of the study, participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nascimento, H., Yasuta, M.K., Marquezan, M.C. et al. Uveitic band keratopathy: child and adult. J Ophthal Inflamm Infect 5, 35 (2015). https://doi.org/10.1186/s12348-015-0062-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-015-0062-z