Abstract
Background
To date, the relationship between the Transesophageal Echocardiography (TEE) monitoring indicator tricuspid annular plane systolic excursion (TAPSE) and the incidence of postoperative acute kidney injury (AKI) in Coronary Artery Bypass Grafting(CABG) patients remains unknown. The main objective of this study was to explore the relationship between the TAPSE and the incidence of AKI in CABG patients.
Methods
This was a multicenter prospective cohort study was conducted between September 2021 and July 2022. Among 266 patients aged at least 18 years who underwent elective CABG, 140 were included.
Results
We measured TAPSE via M-mode TEE via the mid-esophageal (ME) right ventricle(RV) inflow-outflow view (60°). All echocardiographic measurements were performed three separate times at each time point: T0 (before the start of CABG), T2 (approximately 5 ∼ 10 min after neutralization of protamine) and T3 (before leaving the operating room), and then averaged. Serum creatinine was measured 1 day before and within 7 days after CABG. There was no statistically significant association between the TEE-monitoring indicator TAPSE and the incidence of postoperative AKI in patients who underwent CABG.
Conclusions
The TAPSE was not significantly correlated with postoperative AKI incidence and could not predict the early occurrence of postoperative AKI in CABG patients. TEE needs more evaluation for clinical efficacy of predicting the early occurrence of postoperative AKI in isolated CABG.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Acute kidney injury (AKI) is the most common major postoperative complication of CABG and is independently related to hospitalization and long-term mortality [1]. Therefore, early recognition of AKI is important for effectively improving the prognosis of CABG patients. In CABG patients, AKI is associated with renal hypoperfusion in addition to these surgery-related factors [2]. The condition of these patients is often complicated by myocardial infarction, severe multivessel coronary artery disease, or right heart insufficiency, which can cause venous congestion. Venous congestion and fluid overload may reduce renal blood flow and promote the occurrence of AKI [3]. Indicators of venous congestion, such as fluid balance and central venous pressure, have been shown to be correlated with AKI [4, 5]. At present, studies on the relationships between transesophageal echocardiography and postoperative clinical outcome and prognosis are rare, and the conclusions are unclear [6,7,8,9,10]. Although the TAPSE is an ideal indicator for assessing of right ventricular systolic insufficiency [11], its value in predicting the incidence of postoperative AKI in CABG patients remains unknown. Therefore, we designed a multicenter prospective cohort study [12] to explore the effectiveness and guiding role of the TAPSE in reducing the incidence of postoperative AKI and improving the clinical prognosis of CABG patients. The hypothesis of this study is that the TAPSE can predict AKI in CABG surgery patients. The main objective of this study was to investigate the relationship between the TAPSE and postoperative AKI in CABG patients.
Materials and methods
Study design
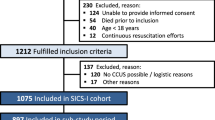
This was a multicenter prospective observational cohort study that was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of The First Affiliated Hospital of Shandong First Medical University, Jinan, and Zibo Central Hospital, Zibo, China. We have published our study protocol in the journal BMJ Open [12]. A total of 266 patients who underwent elective CABG at Qianfoshan Hospital in Shandong Province and Zibo Central Hospital in Shandong Province, China between September 6, 2021 and September 30, 2022, were enrolled. The inclusion criteria were as follows: patients ≥ 18 years who were scheduled to undergo CABG surgery and whose consent forms were signed by the patients themselves or their authorized family members. We interviewed the patients, and they signed the informed consent form 1 day before the procedure. Informed consent was obtained to publish the information/images in an online open access publication. The specific exclusion criteria are described in our protocol [12] that was published in BMJ Open. The clinical data of 140 patients were ultimately analyzed (Fig. 1).
Data collection
After the inclusion of patients, preoperative data on the following variables were collected: anthropomorphic data, risk factors for AKI, EuroSCORE II, preoperative left ventricular ejection fraction (LVEF), pulmonary arterial systolic pressure (PASP), tricuspid regurgitation pressure gradient (TRPG), preoperative Scr levels, preoperative estimation of the glomerular filtration rate (eGFR) and preoperative coexisting disease. Additionally, the following intraoperative data were collected: the type of CABG surgery, graft number, red blood cell (RBC) transfusion, bleeding volume, urine volume, total liquid input, total liquid excretion, operation time, cardiopulmonary bypass (CPB) time, aortic cross-clamp time, Systolic Blood Pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and serum lactate level. The postoperative data obtained in the intensive care unit (ICU) included the incidence of AKI, the incidence of major postoperative cardiovascular and cerebrovascular adverse events (MACCEs) within 30 days after surgery, the incidence of postoperative pulmonary complications (POPC), the duration of tracheal intubation in the ICU (EIT-ICU), the ICU length of stay (D-ICU), the length of stay (LOS), and the cost of hospitalization (HE) (Table 1).
The venous blood of patients was collected, and the Scr level was measured 1 day before and within 7 days after CABG. AKI was also diagnosed according to the Kidney Disease: Improving Global Outcomes (KDIGO) diagnostic guidelines [18, 19]. Patients were divided into the following two groups according to the occurrence of postoperative AKI: the acute kidney injury group (AKI group) and the nonacute kidney injury group (non-AKI group).
Anesthesia management
According to the American Society of Anesthesiologists (ASA) guidelines, continuous monitoring of parameters, including noninvasive blood pressure, heart rate, ECG, SpO2, bispectral index (BIS) and invasive blood pressure, is recommended following admission to the operating room. Midazolam (0.01–0.05 mg/kg), etomidate (0.2 mg/kg), sufentanil (1–3 µg/kg), and cisatracurium besylate (0.2–0.3 mg/kg) or rocuronium (0.6–0.8 mg/kg) were administered intravenously for general anesthesia induction. Combined intravenous and inhalational anesthesia was used to maintain general anesthesia. We adopted a low tidal volume ventilation strategy with the tidal volume set at 6 ml/kg and the PEEP set at 0 mmHg. After induction of general anesthesia, the right internal jugular vein was prepared for central venous pressure (CVP) monitoring and infusion. In the supine position, the central vein pressure sensor was zeroed at the level of the right atrium. We placed the TEE probe before the start of the CABG procedure.
Transesophageal echocardiography measurements
An anesthesiologist who is highly trained and experienced in the use of esophageal ultrasound performed a full TEE examination with a multiplanar TEE probe (Philips X7-2t) (Philips EPIQ 5, Washington, USA). Ultrasound measurements included measurements of inferior vena cava and right ventricular function. The detailed measurement methods and processes can be found in our research protocol (Fig. 2) [12]. All echocardiographic measurements were performed three separate times at each time point: T0 (before the start of coronary artery bypass graft), T2 (approximately 5 ∼ 10 min after neutralization of protamine) and T3 (before leaving the operating room after sternal closure), and the average values were calculated [12].
Outcome measures
The primary outcome was the incidence of postoperative AKI, which was diagnosed according to the KDIGO guidelines [13, 14].
The secondary outcomes included the incidence of MACCEs, the incidence of POPC, the duration of tracheal intubation in the ICU, the length of ICU stay, the LOS and the hospitalization expenses (Table 1) [12].
Statistical methods
Sample size
According to previous studies [2, 15], the incidence of AKI after CABG is approximately 5-57.7%. The sample size of this study was estimated on the basis of the Event Per Variable principle (EPV) in multivariate logistic regression analysis [16], and a total of 135 patients were needed. The minimum sample size is 150, which is based on a 10% loss rate. A total of 266 patients who met the test requirements were included in this study.
Statistical analysis
The statistical analysis was performed according to the prespecified protocol [12], with any deviations justified and conducted by R4.0.2 and Free V1.7 statistical software. All the data subjected to statistical analyses in this study were considered statistically significant if the two-tailed P value was < 0.05.
Baseline data were obtained throughout the cohort and stratified according to whether patients developed AKI. Depending on whether the data adhere to a normal distribution per the Shapiro‒Wilk test, continuous variables are expressed as the means and standard deviations (SDs) or medians and IQRs. Categorical variables are presented as counts (percentages) and were analyzed by means of Fisher’s exact test or the χ2 analysis.
Multivariate logistic regression analysis and smoothing function analysis (Fig. 3) were used to analyze the association between the TAPSE and the incidence of postoperative AKI in patients who underwent CABG. Adjustments were made for the following variables, which were important to the prognosis: age, sex, operation time, graft number, cardiopulmonary bypass condition, body mass index, cardiopulmonary bypass time, red blood cell count, high blood pressure, alcohol use, and aortic cross-clamp time. The associations between the TAPSE and the secondary outcomes were also analyzed via multivariate logistic regression analysis. In addition, we stratified patients with or without AKI after CABG descriptively according to sex, number of grafts, and cardiopulmonary bypass. A receiver operating characteristic (ROC) curve was generated for TAPSE at T0 (before the start of CABG). The area under the ROC curve (AUC) and 95% confidence interval (CI) of TAPSE0 were calculated to analyze its predictive ability.
Results
In the present study, 266 patients were included, and 126 were excluded for the following reasons: (a) patients for whom TEE examination could not be performed because the TEE probe was difficult to place or unavailable and (b) patients with too much gas in the stomach or an unclear ultrasonic image. Ultimately, 140 patients were analyzed (Fig. 1).
AKIs were diagnosed in 16.4% (23/140) of the patients. There were 23 patients with AKI (16.4%) and 117 patients without AKI (83.6%). The baseline characteristics of the two groups are shown in Table 1. There were no significant differences in sex, BMI, smoking status, alcohol consumption, EuroSCORE II, LVEF, comorbidities, type of CABG, graft number, RBC transfusion, urine volume, total liquid input, total liquid excretion, CPB time, aortic clamping time, POPC, EIT-ICU, D-ICU, LOS, or HE between the two groups; however, there were significant differences in age (62.7 ± 8.4 versus 66.7 ± 7.2, P = 0.032), bleeding volume (520.5 ± 153.4 versus 604.3 ± 302.2, P = 0.049), operation time (5.2 ± 0.9 versus 5.8 ± 1.6, P = 0.008) between the two groups. The incidence of MACCEs in the AKI group was higher than that in the non-AKI group(39.1% versus 10.3%, P = 0.002).
The smoothing function analysis(Fig. 3) and multivariate regression analysis (Table 2) revealed that the TEE monitoring index TAPSE at all three time points was not significantly associated with the incidence of postoperative AKI in patients who underwent CABG. Moreover, there was no statistically significant association between the TAPSE measured by TEE at any of the three time points and the secondary outcome of CABG (Table 3).
Discussion
In this prospective cohort study, we found that there was no statistically significant relationship between the TAPSE measured by TEE and the incidence of postoperative AKI. Cardiac surgery associated-acute kidney injury (CSA-AKI) is a major postoperative complication of CABG and is independently correlated with high morbidity and mortality rates. The incidence of CSA-AKI in this study was 16.4%, which was comparable to the results of several previous studies [15]. Traditional diagnostic indicators of AKI, such as serum creatinine (Scr) levels and urine volume, are time-delayed and influenced by many factors [2, 17, 20]. New biomarkers related to AKI, such as neutrophil gelatinase-associated lipoprotein (NGAL) and cystatin-C, are more sensitive for early detection but are not routinely used [2, 21]. Therefore, identifying a new indicator for the early prediction of postoperative AKI is highly important. However, no study has indicated that the TEE-monitoring indicator TAPSE can predict the occurrence of postoperative AKI in CABG patients.
According to the guidelines and previous literatures [11, 22], TAPSE is an ultrasound indicator that has a good correlation with right ventricular systolic function and a good reflection of right ventricular function. In clinical practice, TAPSE is one of the most frequent measures to assess RV function given its simplicity and reproducibility. Although the TAPSE is strongly correlated with global right ventricular function and has been routinely used to assess RV function [22,23,24], its value in predicting AKI after CABG surgery remains unclear. However, the relationship between intraoperative TAPSE and postcoronary bypass AKI remains to be verified in these patients. Wiersema and colleagues reported a statistically independent association between a lower TAPSE and the development of AKI in critically ill patients [3]. Shuangshuang Zhu et al. found that the TAPSE appears to be a reliable predictor of AKI after heart transplantation [25]. Guinot et al. showed that patients with RV dysfunction prior to surgery had a higher incidence of AKI after cardiac surgery [26].
However, a retrospective cohort study revealed that TEE was not associated with a reduced incidence of newly hospitalized AKI in adult patients undergoing isolated CABG surgery in the United States [8]. The results of our study revealed no statistically significant relationship between the TAPSE monitored by TEE and the incidence of postoperative AKI, which was similar to the findings of previous studies. We may consider this for several reasons as follows. First, the TAPSE in our study was derived from TEE measurements rather than from traditional transthoracic echocardiography (TTE), and this is different from the methods used in the above studies [3, 25, 26]. In previous studies, the TAPSE and other indicators reflecting right heart function were generally measured via TTE [3, 22,23,24,25,26]. Unlike the apical 4-chamber view in TTE, the ultrasound was not aligned with the lateral tricuspid annulus in TEE’s 4-chamber view. Mauermann E et al. reported that the TAPSE measured by the 4-chamber TEE view of the midesophagus was significantly lower than that measured by the reference standard TTE view [27]. Munaf and colleagues showed that high interobserver and intraobserver variability in both adult and pediatric patients warrant further studies to evaluate the feasibility of using transgastric RV inflow TAPSE in cardiac surgery [28]. Second, our study revealed a common problem with TEE: there are currently no guidelines comparing the gold standard for TEE measurements of right ventricular function in patients under anesthesia and ventilation [27]. Angle dependence is an important factor that severely hinders the measurement of the right ventricle. Third, longitudinal RV function may not reflect global performance. A study showed that right ventricular longitudinal strain reflects longitudinal myocardial tissue volume and accounts for 80% of the RV stroke volume [29]. Prior studies have shown that commonly used indices of RV function, such as the TAPSE, can be altered by pericardiotomy itself. Our results also revealed that the TAPSE was significantly reduced with sternotomy and pericardiotomy, which may also indicate deteriorated longitudinal RV function. A decrease in longitudinal shortening has been shown to result in gains in transverse shortening, which further limits traditional longitudinal measurements of RV performance, such as TAPSE [30]. Fourth, there are many influencing mechanisms and factors that cause AKI in CABG surgery [2, 8, 10], which also influences the ability of the TAPSE to predict the occurrence of postoperative AKI.
To our knowledge, this is a rare prospective multicenter cohort study examining the association between the TAPSE, an intraoperative TEE-monitoring indicator, and prognosis in patients with CABG. Furthermore, we registered the clinical study at ClinicalTrial.com and published the study protocol [12] in advance. Our study was designed in accordance with the strengthening the reporting of observational studies in epidemiology (STROBE) statement [31], and statistical analyses of the data and subject information were conducted in strict accordance with the research protocol, thereby increasing the transparency and internal validity of the research.
Our study has several limitations. First, the inherent limitation of this study was its observational design, which is well known to result in incomplete data collection and have an increased risk of missing data and follow-up information, which may introduce confounding bias and compromise the accuracy of the data. However, our study was implemented in strict accordance with the published research protocol [12], and multifactor logistic regression analysis was used to control for potential confounding factors. Second, the multifactorial nature of AKI makes the study susceptible to residual confounding factors, such as postoperative transient hypotension, pressor drug requirements and other influencing factors, which may lead to renal hypoperfusion, resulting in oliguria and acute kidney injury [33]. Third, according to the KDIGO guidelines, creatinine levels and urine volume are included in the diagnosis of AKI [13, 14]. However, we calculated the incidence of postoperative AKI on the basis of only blood creatinine levels, which may have led to the underestimation of AKI incidence in this study. Fourth, TAPSE is derived from the ME-RV inflow/outflow view, which is not one of the most commonly used methods and may affect results and repeatability. Although TAPSE measurements and analyses derived from TTE can more accurately assess right ventricular systolic function, it is less commonly used in open heart surgery and is more difficult to obtain. It has been reported that TEE values from the transgastric view RV-inflow view demonstrated high performance throughout surgery and a good agreement with TTE TAPSE measurements [33], which is similar and consistent with our research. The ME-RV inflow/outflow view(60°) avoids the simple evaluation of the longitudinal deep muscle systolic function of the right ventricular free wall, but more considers that the left and right ventricular muscle fibers combine the systolic function of the left and right ventricles through the fusion of the superficial muscle of the ring, taking into account the combined contraction function of the deep longitudinal muscle and the superficial muscle of the ring, which seems to better reflect the true right ventricular function [34].
In summary, the TAPSE, a TEE-based monitoring indicator, was not significantly correlated with postoperative AKI incidence and could not predict the early occurrence of postoperative AKI in CABG patients. These findings highlight the need for further and more significant additional studies to validate the clinical efficacy of TEE in isolated CABG surgery.
Data availability
The obtained data and other information from the included participants will be held in strict confidence by the investigators, research staff, and sponsoring institute. No information or data concerning the study will be released by any unauthoriszed third party, without a prior written approval of the sponsoring institution. Authorized representatives from the sponsoring institution may inspect all the documents and records required to be maintained by the investigator (Binghua Liu: liubinghua042525@126.com).
References
Brown JR, Cochran RP, MacKenzie TA, Furnary AP, Kunzelman KS, Ross CS, et al. Long-term survival after cardiac surgery is predicted by estimated glomerular filtration rate. Ann Thorac Surg. 2008;86(1):4–11.
Wang Y, Bellomo R. Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat Rev Nephrol. 2017;13(11):697–711.
Wiersema R, Koeze J, Hiemstra B, Pettilä V, Perner A, Keus F, et al. Associations between tricuspid annular plane systolic excursion to reflect right ventricular function and acute kidney injury in critically ill patients: a SICS-I sub-study. Ann Intensive Care. 2019;9(1):38.
Chen KP, Cavender S, Lee J, Feng M, Mark RG, Celi LA, et al. Peripheral edema, central venous pressure, and risk of AKI in critical illness. Clin J Am Soc Nephrol. 2016;11(4):602–8.
Vaara ST, Korhonen AM, Kaukonen KM, Nisula S, Inkinen O, Hoppu S, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care. 2012;16(5):R197.
Eltzschig HK, Rosenberger P, Löffler M, Fox JA, Aranki SF, Shernan SK. Impact of intraoperative transesophageal echocardiography on surgical decisions in 12,566 patients undergoing cardiac surgery. Ann Thorac Surg. 2008;85(3):845–52.
Klein AA, Snell A, Nashef SA, Hall RMO, Kneeshaw JD, Arrowsmith JE. The impact of intraoperative transoesophageal echocardiography on cardiac surgical practice. Anaesthesia. 2009;64(9):947–52.
MacKay EJ, Werner RM, Groeneveld PW, Desai ND, Reese PP, Gutsche JT, et al. Transesophageal echocardiography, acute kidney injury, and length of hospitalization among adults undergoing coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2020;34(3):687–95.
Sato K, Bainbridge D. Transesophageal echocardiography and outcomes in coronary artery bypass grafting surgery: dealing with confounders in observational studies. J Cardiothorac Vasc Anesth. 2020;34(3):696–7.
Metkus TS, Thibault D, Grant MC, Badhwar V, Jacobs JP, Lawton J, et al. Transesophageal Echocardiography in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol. 2021;78(2):112–22.
Olmos-Temois SG, Santos-Martinez LE, Alvarez-Alvarez R, Gutiérrez-Delgado LG, Baranda-Tovar LG. Interobserver agreement on the echocardiographic parameters that estimate right ventricular systolic function in the early postoperative period of cardiac surgery. Med Intensiva. 2016;40(8):491–8.
Liu B, Lv M, Wang H, Sun Y, Song X, Dong L, et al. Association between transoesophageal echocardiography monitoring indicators and the incidence of postoperative acute kidney injury in coronary artery bypass grafting: a study protocol for a prospective multicenter cohort study. BMJ Open. 2022;12(8):e059644.
Khwaja A. KDIGO clinical practice guideline for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–184.
Garg AX, Devereaux PJ, Yusuf S, Cuerden MS, Parikh CR, Coca SG, et al. Kidney function after off-pump or on-pump coronary artery bypass graft surgery: a randomized clinical trial. JAMA. 2014;311(21):2191–8.
Smeltz AM, Cooter M, Rao S, Karhausen JA, Stafford-Smith M, Fontes ML, et al. Elevated pulse pressure, intraoperative hemodynamic perturbations, and acute kidney injury after coronary artery bypass grafting surgery. J Cardiothorac Vasc Anesth. 2018;32(3):1214–24.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Zhang H, Zhou K, Wang D, Zhang N, Liu J. The predictive value of the intraoperative renal pulsatility index for acute kidney injury in patients undergoing cardiac surgery. Minerva Anestesiol. 2020;86(11):1161–9.
Romagnoli S, Ricci Z, Ronco C. Perioperative Acute kidney Injury: Prevention, Early Recognition, and supportive measures. Nephron. 2018;140(2):105–10.
Parida S, Badhe AS. Cardiac surgery–associated acute kidney injury. J Anesth. 2013;27(3):433–46.
Bragadottir G, Redfors B, Ricksten S-E. Assessing glomerular filtration rate (GFR) in critically ill patients with acute kidney injury - true GFR versus urinary creatinine clearance and estimating equations. Crit Care. 2013;17(3):1–30.
Fang F, Luo W, Yang M, Yang P, Yang X. Urinary Matrix Metalloproteinase-7 and Prediction of AKI Progression Post Cardiac Surgery. Dis Markers. 2019; 2019: 9217571.
Rudski LG, Lai WW, Afilalo J, Hua LQ, Handschumacher MD, Chandrasekaranet K. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–70.
Portnoy SG, Rudski LG. Echocardiographic evaluation of the right ventricle: a 2014 perspective. Curr Cardiol Rep. 2015;17(4):21.
Zhu S, Zhang Y, Qiao W, Wang Y, Xie Y, Zhang X, et al. Incremental value of preoperative right ventricular function in predicting moderate to severe acute kidney injury after heart transplantation. Front Cardiovasc Med. 2022;9:931517.
Guinot PG, Abou-Arab O, Longrois D, Dupont H. Right ventricular systolic dysfunction and vena cava dilatation precede alteration of renal function in adult patients undergoing cardiac surgery: an observational study. Eur J Anaesthesiol. 2015;32(8):535–42.
Mauermann E, Vandenheuvel M, François K, Bouchez S, Wouters P. Right ventricular systolic assessment by transesophageal versus transthoracic echocardiography: displacement, velocity, and myocardial deformation. J Cardiothorac Vasc Anesth. 2020;34(8):2152–61.
Munaf M, Suneel PR, Harikrishnan S, Koshy T. Tricuspid annular plane systolic excursion (TAPSE) for the Assessment of right ventricular function in Adult and Pediatric Cardiac surgery: modified Twodimensional and M-mode TAPSE by Transesophageal Echocardiography Compared to M-mode TAPSE by Transthoracic Echocardiography. J Cardiothorac Vasc Anesth. 2024;38(1):123–32.
Carlsson M, Ugander M, Heiberg E, Arheden H. The quantitative relationship between longitudinal and radial function in left, right, and total heart pumping in humans. Am J Physiol Heart Circ Physiol. 2007;293(1):H636–44.
Raina A, Vaidya A, Gertz ZM, Susan C, Forfia PR. Marked changes in right ventricular contractile pattern after cardiothoracic surgery: implications for post-surgical assessment of right ventricular function. J Heart Lung Transpl. 2013;32(8):777–83.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9.
Yue Z, Yan-Meng G, Ji-Zhuang L. Prediction model for acute kidney injury after coronary artery bypass grafting: a retrospective study. Int Urol Nephrol. 2019;51(9):1605–11.
Korshin A, Grønlykke L, Nilsson JC, Møller-Sørensen H, Ihlemann N, Kjøller M, et al. The feasibility of tricuspid annular plane systolic excursion performed by transesophageal echocardiography throughout heart surgery and its interchangeability with transthoracic echocardiography. Int J Cardiovasc Imaging. 2018;34(7):1017–28.
Cheng XS. Left and right ventricular interdependence and right ventricular myocardial mechanical pattern. Zhonghua Xin xue guan bing za zhi. 2020;48(10):814–22.
Acknowledgements
The authors would like to thank all the involved doctors and nurses of the Department of Anesthesia and Perioperative Medicine, The First Affiliated Hospital of Shandong First Medical University and the Department of Anesthesiology, Zibo Central Hospital for their great effort and support in this study. We also acknowledge to Professor Fang Tang and her team for assisting with the statistical analysis. The authors also thank all the participating patients.
Funding
This work was supported by the National Natural Science Foundation of China(82070078 to Yuelan Wang).
Author information
Authors and Affiliations
Contributions
Study design: Yuelan Wang, Binghua Liu. Screening, Enrolling participants, Data collection, Follow-up and Writing of the Report: Binghua Liu, Guoqing Zhang, Haiyan Wang, Hongyu Xu. Management and literature Search: Meng Lv, Xiumei Song, Ling Dong. Statistical analysis: Yongtao Sun, Hai Feng.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of The First Affiliated Hospital of Shandong First Medical University, Jinan, and Zibo Central Hospital, Zibo, China. Informed consent was obtained from all the subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Presentation
Our article has not been presented at any conference.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, B., Zhang, G., Lv, M. et al. The relationship between tricuspid annular plane systolic excursion on transesophageal echocardiography and the incidence of postoperative acute kidney injury in patients undergoing coronary artery bypass grafting surgery: a multicenter prospective cohort study. BMC Anesthesiol 24, 328 (2024). https://doi.org/10.1186/s12871-024-02709-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-024-02709-0