Abstract
Background
In developing nations, myocardial infarction (MI) remains a significant contributor to deaths from sudden cardiac arrest, with diet playing a key role in its incidence through oxidative stress mechanisms. Although the connection between the Dietary Antioxidant Index (DAI) and cardiovascular diseases has been demonstrated in some studies, the relationship between DAI and MI has not been extensively explored. Therefore, this research aims to investigate this association.
Methods
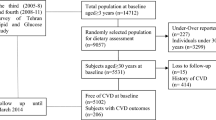
We conducted a nested case-control study involving 156 MI cases and 312 healthy controls, utilizing data from the Fasa Adults Cohort Study (FACS), a population-based study of individuals aged 35–70 residing in Fasa, Iran, with 11,097 participants included at baseline. The DAI was determined by normalizing the intake values of six dietary vitamins and minerals, adjusting by subtracting the global mean, and then dividing by the global standard deviation. MI diagnosis was established by an experienced cardiologist using electronic medical records. Conditional logistic regression was employed to examine the association between DAI and MI.
Results
There were no significant differences between the case and control groups in terms of age (P = 0.96), gender distribution (P = 0.98), and education level (P = 0.38). In a multiple conditional logistic regression analysis, after adjusting for key variables—including body mass index (BMI), smoking status, education level, and serum levels of triglycerides (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), total cholesterol (TC), fasting blood sugar (FBS), saturated fatty acids (SFA), and polyunsaturated fatty acids (PUFA)—an inverse association was found between DAI and the risk of myocardial infarction (MI) [adjusted Odds Ratio (Adj OR) = 0.88, 95% Confidence Interval (CI): 0.85–0.92; P < 0.001].
Conclusions
This study highlights the crucial role of the DAI in reducing the risk of myocardial infarction. Promoting diets rich in antioxidants presents a straightforward and effective strategy for MI prevention and the promotion of cardiovascular health, underscoring the novelty and significance of this research in dietary approaches to disease prevention.
Similar content being viewed by others
Introduction
Myocardial Infarction (MI), also referred to as a heart attack, is a critical coronary event that can result in sudden cardiac death and represents the most severe clinical presentation of coronary artery disease (CAD) [1, 2]. The incidence of MI is approximately 15.9 million cases annually, imposing a significant economic burden; however, effective preventive measures can lead to cost savings and increased productivity [3, 4]. Although reperfusion therapy reduces adverse outcomes, survivors often face challenges such as heart failure, which significantly impacts health outcomes [5,6,7]. MI occurs due to the narrowing of coronary arteries, which restricts blood flow to the myocardial tissue [8]. Inflammation and inflammatory conditions, such as chronic low-grade inflammation (CLE), play a crucial role in the development of atherosclerotic plaques within the arterial walls, further impeding blood flow to the heart [9,10,11].
The development and progression of atherosclerosis are promoted by the presence of reactive oxygen species (ROS) and reactive nitrogen species (RNS). Antioxidants have shown potential in mitigating atherosclerosis by neutralizing these harmful species [12,13,14,15]. A diet rich in fruits and vegetables, which are high in antioxidants, has been linked to a reduced risk of CAD [16]. Additionally, some medications used in CAD treatment, including aspirin, statins, and angiotensin-converting enzyme inhibitors, possess antioxidant properties [17, 18].
Studies have demonstrated that adhering to a Mediterranean dietary pattern is associated with a lower risk of MI and other cardiovascular diseases [19, 20]. The Dietary Antioxidant Index (DAI), developed to assess a person’s overall antioxidant capacity, considers dietary intake of vitamins A, C, and E, along with the minerals including manganese, selenium, and zinc. These antioxidants have been proven to lower cardiovascular disease and mortality rates while also enhancing the body’s endogenous antioxidant mechanisms [21,22,23].
Previous research, including a prospective cohort study utilizing data from the US National Health and Nutrition Examination Survey (NHANES), has identified a correlation between a higher DAI and lower risks of all-cause and cardiovascular mortality [24, 25]. To further explore the relationship between DAI and MI, and to potentially reduce the mortality rates and economic impacts associated with MI, we conducted a nested case-control study using data from the Fasa Cohort Study (FACS), a population-based study.
Materials and methods
Study population and setting
This nested case-control study utilized data collected within the framework of the FACS [26, 27]. FACS is part of the larger PERSIAN Cohort Study, a comprehensive longitudinal investigation designed to explore the factors contributing to the development of noncommunicable diseases among the residents of Sheshdeh, a rural area in Fasa, Iran. Sheshdeh has a population of approximately 41,000 individuals.
The study cohort consisted of individuals aged 35–70 residing in Sheshdeh, totaling 11,097 participants. Data collection took place between 2015 and 2016, following a documented informed consent process. This investigation was a matched case-control study, with participants in the case and control groups matched based on age, sex, and the time of the event. The study’s primary outcome of interest was the incidence of a confirmed first-time myocardial infarction (MI), classified by the International Classification of Diseases, Tenth Revision (ICD-10) codes I21.0 through I21.9 [28]. The incident cases included 156 patients with confirmed MI based on their electronic medical records, and controls were frequency-matched to cases by sex, age (± 5 years), and time of event, with a control-to-case ratio of 2:1.
The inclusion criteria for the study included individuals who had been permanent residents of the area for at least one year, demonstrated willingness to participate by providing informed consent via a signed agreement, and were within the age range of 35 to 70 years. Participants were excluded from the analysis if they had autoimmune diseases, certain types of cancers, were using nutritional supplements with antioxidant properties (such as vitamin E, selenium, vitamin A, zinc, vitamin C, or omega-3 fatty acids), were pregnant or lactating, adhered to a strict dietary regimen, or had gastrointestinal disorders, including irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or celiac disease. Additionally, individuals with incomplete nutritional intake questionnaires or abnormal caloric intake (exceeding 4500 kcal or below 700 kcal) were excluded from the study.
Baseline characteristics
Demographic data, including age, level of education, smoking status, and gender, were recorded using a survey instrument. The instrument also collected medical histories related to cardiovascular diseases (CVD), including coronary heart disease, myocardial infarction, and stroke. A trained professional measured participants’ heights with a stadiometer accurate to 0.1 cm (SECA 222, Germany), while weights were recorded using a calibrated digital scale accurate to 0.1 kg (SECA 888 Digital Scale, Germany).
MI assessment
The assessment of MI in our population was conducted in two phases: First, through patient self-reporting of the disease, and second, by evaluating medical records. Two experienced physicians reviewed these records using the latest guidelines for evaluating cardiovascular diseases, including MI.
Dietary assessment
At the start of the study, dietary information was obtained using a semi-quantitative food frequency questionnaire (FFQ) that included 168 items, depending on the year of assessment. Participants reported their consumption frequency, which ranged from “never” to “daily.” Food portion sizes were converted from common household units (e.g., cups, spoons) to grams per day for standardized analysis. The dietary data in grams per day was then uploaded into Nutritionist IV software to generate detailed nutrient profiles and assess total daily calorie intake.
Biochemical and physical activity evaluation
Serum levels of total cholesterol, triglycerides, HDL cholesterol, and glucose were measured using the enzymatic colorimetric technique. Blood pressure was assessed with a validated monitor manufactured by Omron, Japan. Measurements were taken after a resting period of at least 10 min following recent activity. Participants were instructed to sit in a relaxed position with their left arm exposed and supported on a stable surface at heart level. Blood pressure readings were obtained from the left arm using an appropriately sized cuff.
To assess physical activity levels, the study employed the 20-item International Physical Activity Questionnaire (IPAQ). This tool quantified the routine physical activities of participants residing in rural Iran. The IPAQ collected data on activity duration (recorded in hours and minutes) for various activities. By multiplying these durations by their corresponding metabolic equivalent (MET) values, researchers calculated a total MET score, which reflects overall activity intensity.
DAI calculation
For each participant, dietary data obtained through the FFQ were used to compute their DAI score. To estimate the DAI, the intake values for each of the six dietary vitamins and minerals were normalized by subtracting the global mean and then dividing by the global standard deviation. The DAI was calculated by summing the normalized intakes of these vitamins and minerals, with each component given equal weight, as outlined below [22]:
Finally, to eliminate the effect of energy, the DAI score was adjusted to energy.
Statistical analysis
This study employs descriptive statistics to present the findings. For continuous variables that follow a normal distribution, the mean and standard deviation are reported. Categorical variables are described using frequencies and percentages. The Kolmogorov-Smirnov test was used to assess the normality of continuous variables. To compare average nutrient intake across quartiles of the DAI, a one-way ANOVA test was conducted. Conditional logistic regression was applied across various models to explore the relationship between DAI and myocardial infarction (MI) risk, adjusting for relevant variables.
Initially, adjustments were made for body mass index (BMI) and smoking status. The second model included additional adjustments for educational level and serum concentrations of triglycerides (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), and total cholesterol. A further model accounted for fasting blood sugar (FBS), saturated fatty acids (SFA), and polyunsaturated fatty acids (PUFA). All statistical analyses were performed using IBM® SPSS® Statistics version 18.0 software. A significance level of p < 0.05 was adopted for all statistical tests.
Results
An overview of the participants’ demographics is provided in Table 1. The case and control groups exhibited no statistically significant differences in age (P = 0.96), gender distribution (P = 0.98), or education level (P = 0.38). However, a significant difference in weight was observed between the MI and control groups, with the MI group exhibiting a higher mean weight (P = 0.03). Additionally, our analysis revealed significant differences between the case and control groups in terms of BMI, WC, and physical activity levels (P < 0.05).
In terms of biochemical variables, participants in the MI group had significantly higher levels of FBS (112.38 ± 56.08 mg/dL vs. 93.12 ± 27.99 mg/dL; P < 0.001), SBP (123.76 ± 23.11 mmHg vs. 113.82 ± 20.94 mmHg; P < 0.001), and DBP (79.26 ± 14.75 mmHg vs. 74.79 ± 12.95 mmHg; P < 0.001). Interestingly, no significant differences were observed in TG (P = 0.21), LDL (P = 0.74), cholesterol (P = 0.41), or HDL (P = 0.67) levels between the case and control groups. Additionally, we did not observe any significant differences between the two groups in terms of dietary intake (P > 0.05).
In Table 2, we explore the distribution of baseline characteristics and dietary intakes categorized by quartiles of DAI scores. No significant differences were observed across quartiles of the DAI in terms of anthropometric and biochemical variables (P > 0.05). However, there was a significant difference across quartiles of the DAI in terms of energy intake and other macro- and micronutrients (P < 0.001).
We assessed the relationship between DAI and the odds of developing MI. In the crude model, we identified a significant inverse relationship between DAI and the odds of MI (odds ratio (OR) = 0.81, CI: 0.78–0.83; P < 0.001). After full adjustment for confounding factors (adjusted for BMI, smoking, educational degree, LDL, HDL, cholesterol, FBS, SFA, and PUFA), this level of significance did not change in the fully adjusted model (Adj OR = 0.88, CI: 0.85–0.92; P < 0.001).
Discussion
In our nested case-control study using data from the Fasa Adults Cohort Study, we found that DAI was inversely associated with MI risk after adjusting for potential confounding factors, suggesting that DAI may act as a protective factor against myocardial infarction.
Poor dietary choices are often linked to chronic low-grade inflammation, a key factor contributing to the development of various metabolic diseases [29]. Diets high in pro-inflammatory components can intensify the inflammatory response through mechanisms such as increased oxidative stress and immune system dysregulation, thereby contributing to the onset of atherosclerosis [30, 31]. Evidence shows that inflammatory cytokines, such as interleukin-1 (IL-1) and IL-6, can destabilize atherosclerotic plaques and cause myocardial damage [32,33,34]. Elevated levels of inflammatory cytokines, commonly associated with unhealthy eating patterns, further reinforce this connection. Chronic low-grade inflammation triggered by pro-inflammatory diets can lead to the production of reactive oxygen species (ROS). These ROS, in turn, contribute to endothelial dysfunction, chronic vascular inflammation, and cardiomyocyte death [35, 36].
Studies suggest that a diet rich in antioxidants may be associated with a substantial reduction in overall mortality rates within the general U.S. population [24].
Supporting our observations, a previous cross-sectional analysis of NHANES data identified a similar inverse, non-linear association between dietary antioxidant intake, measured by the DAI, and CHD risk in the U.S. adult population [37]. Additionally, results from another cohort suggested a preventive relationship between dietary total antioxidant capacity (DTAC) and MI [38]. An analysis of Iranian individuals aged 40–70 also demonstrated that DAI had a protective effect against cardiovascular disease [39]. Another cross-sectional study of a sample of U.S. adults revealed a negative, non-linear association between DAI and depression [40]. Interestingly, some studies suggest that a diet lower in antioxidants might be associated with a reduced risk of type 2 diabetes, particularly in middle-aged women [41]. Increasing dietary antioxidant intake has also been shown to protect against various other diseases, such as papillomavirus infection, cancer, depression, and osteoporosis [42].
Evidence shows that MI activates the immune system and increases pro-inflammatory cytokines in the blood [4]. Previous research has demonstrated that DTAC is inversely related to MI and specific oxidative stress biomarkers [38, 43]. The imbalance between oxidative stress and antioxidant defense, leading to the production of ROS, has been linked to atherosclerosis. Dietary antioxidants are believed to help prevent coronary heart disease by scavenging ROS [14, 44]. Non-enzymatic antioxidants, including vitamins A, C, and E, along with minerals such as zinc, selenium, and manganese, are essential in combating oxidative stress [45,46,47,48,49].
Several studies have identified low blood zinc concentrations as a potential independent risk factor for the development of CHD, while selenium’s role in interacting with selenoproteins helps protect against oxidative stress-induced cell damage and lipid peroxidation [50, 51]. A nested case-control study involving 1,621 individuals with incident CHD and 1,621 control subjects without CHD found an inverse association between incident CHD and selenium levels [52]. Additionally, a separate study utilizing multivariable logistic regression analysis of blood parameters from 3,541 participants identified low zinc concentration in blood as an independent predictor of CHD in a cohort consisting of 1,253 CHD patients and 2,288 healthy controls [51, 53].
While previous research has examined the association between DAI and cardiovascular disease, our study is the first to explore its connection to MI. By integrating various antioxidants into the DAI, our study provides a unique perspective on the potential protective effects of a diverse range of dietary antioxidants [24, 37]. This study represents the initial examination of the association between DAI and MI among the Iranian population, offering valuable insights into the protective role of dietary antioxidants.
One of the strengths of our study is the consideration of the synergistic effects of combining antioxidants in the DAI, which reflects the realistic dietary intake of individuals consuming a variety of foods with diverse antioxidants. The use of a FFQ allowed for a comprehensive assessment of participants’ dietary habits.
However, there are limitations to consider. First, while this nested case-control design efficiently explores the association between DAI and MI risk, it is inherently observational and cannot definitively establish causality. Reverse causation is a possibility, where pre-existing MI might influence dietary choices. Lastly, although the study accounted for various confounding factors, there may still be unmeasured variables influencing both DAI and MI risk, potentially introducing bias into the results.
The significant inverse relationship observed between DAI and the risk of MI in our study highlights the potential importance of dietary antioxidants in cardiovascular health. While this finding underscores the benefits of consuming a diet rich in antioxidants, it is essential to consider how this might influence clinical practice and treatment approaches. Based on our findings, incorporating dietary strategies that enhance antioxidant intake could be an effective supplementary approach in the prevention of MI. Healthcare providers might consider recommending diets rich in antioxidants—such as those abundant in vitamins A, C, and E, and essential minerals like zinc, manganese, and selenium—as part of a comprehensive strategy to reduce cardiovascular risk. This dietary approach could be integrated with existing treatment modalities, such as pharmacological therapies and lifestyle modifications, to offer a holistic preventive strategy for MI.
It is crucial to acknowledge that while our study demonstrates an association, it does not establish causality. Therefore, future research should focus on clinical trials to investigate the direct impact of dietary antioxidants on MI risk reduction. Such trials could help determine the optimal levels and sources of antioxidants required for significant cardiovascular benefits and provide more robust evidence to inform clinical guidelines.
Conclusion
In conclusion, our nested case-control study revealed a significant inverse relationship between DAI and the risk of MI in the adult population, even after adjusting for potential confounders. Incorporating foods rich in DAI components, such as vitamins A, C, and E, along with essential minerals like zinc, manganese, and selenium, into one’s diet may be an effective strategy for reducing the risk of MI. These findings underscore the importance of maintaining a well-rounded diet abundant in antioxidants to promote heart health and overall well-being.
Future prospective cohort studies with extended follow-up periods could provide stronger evidence for a causal relationship between DAI and MI risk. Additionally, investigating the specific mechanisms by which dietary antioxidants exert their protective effects, such as reducing oxidative stress and inflammation, would be valuable for developing targeted dietary recommendations to enhance cardiovascular health.
Data availability
The data that was used in this study are not publicly available due to confidentiality of information; however the data is available from the corresponding author on a reasonable request basis.
Abbreviations
- DAI:
-
Dietary Antioxidant Index
- MI:
-
Myocardial infarction
- BMI:
-
Body mass index
- TG:
-
Triglycerides
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- TC:
-
Total cholesterol
- FBS:
-
Fasting blood sugar
- SFA:
-
Saturated fatty acids
- PUFA:
-
Polyunsaturated fatty acids
- ROS:
-
Reactive oxygen species
- RNS:
-
Reactive nitrogen species
- CAD:
-
Coronary artery disease
- NHANES:
-
National Health and Nutrition Examination Survey
- FACS:
-
Fasa Cohort Study
- IBS:
-
Irritable bowel syndrome
- IBD:
-
Inflammatory bowel disease
- CVD:
-
Cardiovascular diseases
- FFQ:
-
Food frequency questionnaire
- IPAQ:
-
International Physical Activity Questionnaire
- MET:
-
Metabolic equivalent of task
- CHD:
-
Coronary heart disease
- DTAC:
-
Dietary total antioxidant capacity
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Hahla MS, Saeed Y, Razieh H. Comparison of risk factors & clinical and angiographic characterization of STEMI in young adults with older patients. Research journal of pharmaceutical biological and chemical sciences; 2016;7(6):2013–6.
Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–65.
Bishu KG, Lekoubou A, Kirkland E, Schumann SO, Schreiner A, Heincelman M, et al. Estimating the economic burden of acute myocardial infarction in the US: 12 year national data. Am J Med Sci. 2020;359(5):257–65.
Vanherle L, Lidington D, Uhl FE, Steiner S, Vassallo S, Skoug C, et al. Restoring myocardial infarction-induced long-term memory impairment by targeting the cystic fibrosis transmembrane regulator. EBioMedicine. 2022;86:104384.
Zhuang L, Zong X, Yang Q, Fan Q, Tao R. Interleukin-34-NF-κB signaling aggravates myocardial ischemic/reperfusion injury by facilitating macrophage recruitment and polarization. EBioMedicine. 2023;95:104744.
Hayward CJ, Batty JA, Westhead DR, Johnson O, Gale CP, Wu J, Hall M. Disease trajectories following myocardial infarction: insights from process mining of 145 million hospitalisation episodes. EBioMedicine. 2023;96:104792.
Lan C, Chen C, Qu S, Cao N, Luo H, Yu C, et al. Inhibition of DYRK1A, via histone modification, promotes cardiomyocyte cell cycle activation and cardiac repair after myocardial infarction. EBioMedicine. 2022;82:104139.
Gao J, Zhang X, Xu M, Deng S, Chen X. The efficacy and safety of sacubitril/valsartan compared with ACEI/ARB in the treatment of heart failure following acute myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Front Pharmacol. 2023;14:1237210.
McCullough PA. Coronary artery disease. Clin J Am Soc Nephrol. 2007;2(3):611–6.
Olbrich H, Kridin K, Zirpel H, Sadik CD, Terheyden P, Thaçi D, et al. Cutaneous lupus erythematosus is associated with an increased risk of cardiac and vascular diseases: a large-scale, propensity-matched global retrospective cohort study. EBioMedicine. 2023;93:104639.
Ghanavati M, Rahmani J, Clark CC, Hosseinabadi SM, Rahimlou M. Pistachios and cardiometabolic risk factors: a systematic review and meta-analysis of randomized controlled clinical trials. Complement Ther Med. 2020;52:102513.
Darley-Usmar V, Halliwell B. Blood radicals: reactive nitrogen species, reactive oxygen species, transition metal ions, and the vascular system. Pharm Res. 1996;13(5):649–62.
Patel RP, Moellering D, Murphy-Ullrich J, Jo H, Beckman JS, Darley-Usmar VM. Cell signaling by reactive nitrogen and oxygen species in atherosclerosis. Free Radic Biol Med. 2000;28(12):1780–94.
Thomson MJ, Puntmann V, Kaski JC. Atherosclerosis and oxidant stress: the end of the road for antioxidant vitamin treatment? Cardiovasc Drugs Ther. 2007;21(3):195–210.
Rahimlou M, Morshedzadeh N, Karimi S, Jafarirad S. Association between dietary glycemic index and glycemic load with depression: a systematic review. Eur J Nutr. 2018;57:2333–40.
Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136(10):2588–93.
Kattoor AJ, Pothineni NVK, Palagiri D, Mehta JL. Oxidative stress in atherosclerosis. Curr Atheroscler Rep. 2017;19:1–11.
Morvaridzadeh M, Sepidarkish M, Fazelian S, Rahimlou M, Omidi A, Ardehali SH, et al. Effect of calcium and vitamin D co-supplementation on blood pressure: a systematic review and meta-analysis. Clin Ther. 2020;42(3):e45–63.
Tektonidis TG, Åkesson A, Gigante B, Wolk A, Larsson SC. A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: a population-based cohort study. Atherosclerosis. 2015;243(1):93–8.
Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, Trichopoulos D. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6):S1402–6.
Jenkins DJ, Kitts D, Giovannucci EL, Sahye-Pudaruth S, Paquette M, Mejia SB, et al. Selenium, antioxidants, cardiovascular disease, and all-cause mortality: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2020;112(6):1642–52.
Wright ME, Mayne ST, Stolzenberg-Solomon RZ, Li Z, Pietinen P, Taylor PR, et al. Development of a comprehensive dietary antioxidant index and application to lung cancer risk in a cohort of male smokers. Am J Epidemiol. 2004;160(1):68–76.
Rahimlou M, Mirzaei K, Keshavarz SA, Hossein-Nezhad A. Association of circulating adipokines with metabolic dyslipidemia in obese versus non-obese individuals. Diabetes Metab Syndr. 2016;10(1 Suppl 1):S60–5.
Wang L, Yi Z. Association of the Composite dietary antioxidant index with all-cause and cardiovascular mortality: a prospective cohort study. Front Cardiovasc Med. 2022;9:993930.
Karakayali M, Omar T, Artac I, Ilis D, Arslan A, Altunova M, et al. The prognostic value of HALP score in predicting in-hospital mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2023;34(7):483–8.
Farjam M, Bahrami H, Bahramali E, Jamshidi J, Askari A, Zakeri H, et al. A cohort study protocol to analyze the predisposing factors to common chronic non-communicable diseases in rural areas: Fasa Cohort Study. BMC Public Health. 2016;16:1–8.
Homayounfar R, Farjam M, Bahramali E, Sharafi M, Poustchi H, Malekzadeh R, et al. Cohort Profile: the Fasa adults Cohort Study (FACS): a prospective study of non-communicable diseases risks. Int J Epidemiol. 2023;52(3):e172–8.
Anderson RN, Rosenberg HM. Disease classification: measuring the effect of the Tenth Revision of the International classification of diseases on cause-of‐death data in the United States. Stat Med. 2003;22(9):1551–70.
Maiuolo J, Gliozzi M, Carresi C, Musolino V, Oppedisano F, Scarano F et al. Nutraceuticals and Cancer: potential for natural polyphenols. Nutrients. 2021;13(11).
Younossi ZM, Corey KE, Lim JK. AGA clinical practice update on Lifestyle Modification using Diet and Exercise to achieve weight loss in the management of nonalcoholic fatty liver disease. Expert Rev Gastroenterol. 2021;160(3):912–8.
Ignarro LJ, Balestrieri ML, Napoli C. Nutrition, physical activity, and cardiovascular disease: an update. Cardiovasc Res. 2007;73(2):326–40.
Huse C, Anstensrud AK, Michelsen AE, Ueland T, Broch K, Woxholt S, et al. Interleukin-6 inhibition in ST-elevation myocardial infarction: Immune cell profile in the randomised ASSAIL-MI trial. EBioMedicine. 2022;80:104013.
Wang S, Hu S, Luo X, Bao X, Li J, Liu M, et al. Prevalence and prognostic significance of DNMT3A- and TET2- clonal haematopoiesis-driver mutations in patients presenting with ST-segment elevation myocardial infarction. EBioMedicine. 2022;78:103964.
Yin X, Yin X, Pan X, Zhang J, Fan X, Li J, et al. Post-myocardial infarction fibrosis: pathophysiology, examination, and intervention. Front Pharmacol. 2023;14:1070973.
Wanschel A, Guizoni DM, Lorza-Gil E, Salerno AG, Paiva AA, Dorighello GG et al. The Presence of Cholesteryl Ester Transfer Protein (CETP) in endothelial cells generates vascular oxidative stress and endothelial dysfunction. Biomolecules. 2021;11(1).
Shi HT, Huang ZH, Xu TZ, Sun AJ, Ge JB. New diagnostic and therapeutic strategies for myocardial infarction via nanomaterials. EBioMedicine. 2022;78:103968.
Ma R, Zhou X, Zhang G, Wu H, Lu Y, Liu F, et al. Association between composite dietary antioxidant index and coronary heart disease among US adults: a cross-sectional analysis. BMC Public Health. 2023;23(1):2426.
Rautiainen S, Levitan EB, Orsini N, Åkesson A, Morgenstern R, Mittleman MA, Wolk A. Total antioxidant capacity from diet and risk of myocardial infarction: a prospective cohort of women. Am J Med. 2012;125(10):974–80.
Parisa K, Maryam J, Masoumeh Ghoddusi J, Ramin R, Seyed Vahid H, Abbas R. The Association between Dietary antioxidant indices and Cardiac Disease: Baseline Data of Kharameh Cohort Study. J Biostatistics Epidemiol. 2022;8(4).
Zhao L, Sun Y, Cao R, Wu X, Huang T, Peng W. Non-linear association between composite dietary antioxidant index and depression. Front Public Health. 2022;10:988727.
Mancini FR, Affret A, Dow C, Balkau B, Bonnet F, Boutron-Ruault MC, Fagherazzi G. Dietary antioxidant capacity and risk of type 2 diabetes in the large prospective E3N-EPIC cohort. Diabetologia. 2018;61(2):308–16.
Yang C, Yang Q, Peng X, Li X, Rao G. Associations of composite dietary antioxidant index with cardiovascular disease mortality among patients with type 2 diabetes. Diabetol Metab Syndr. 2023;15(1):131.
Frijhoff J, Winyard PG, Zarkovic N, Davies SS, Stocker R, Cheng D, et al. Clinical relevance of biomarkers of oxidative stress. Antioxid Redox Signal. 2015;23(14):1144–70.
Griendling KK, FitzGerald GA. Oxidative stress and cardiovascular injury: part II: animal and human studies. Circulation. 2003;108(17):2034–40.
An L, Zhang T, Vitamins C. E reverse melamine-induced deficits in spatial cognition and hippocampal synaptic plasticity in rats. Neurotoxicology. 2014;44:132–9.
Fraga DB, Camargo A, Olescowicz G, Azevedo Padilha D, Mina F, Budni J, et al. A single administration of ascorbic acid rapidly reverses depressive-like behavior and hippocampal synaptic dysfunction induced by corticosterone in mice. Chem Biol Interact. 2021;342:109476.
Klotz LO, Kröncke KD, Buchczyk DP, Sies H. Role of copper, zinc, selenium and tellurium in the cellular defense against oxidative and nitrosative stress. J Nutr. 2003;133(5 Suppl 1):s1448–51.
Mezzaroba L, Alfieri DF, Colado Simão AN, Vissoci Reiche EM. The role of zinc, copper, manganese and iron in neurodegenerative diseases. Neurotoxicology. 2019;74:230–41.
O’Reilly K, Bailey SJ, Lane MA. Retinoid-mediated regulation of mood: possible cellular mechanisms. Exp Biol Med (Maywood). 2008;233(3):251–8.
Barchielli G, Capperucci A, Tanini D. The role of Selenium in pathologies: an updated review. Antioxid (Basel). 2022;11(2).
Meng H, Wang Y, Zhou F, Ruan J, Duan M, Wang X, et al. Reduced serum zinc Ion Concentration is Associated with Coronary Heart Disease. Biol Trace Elem Res. 2021;199(11):4109–18.
Yuan Y, Xiao Y, Feng W, Liu Y, Yu Y, Zhou L, et al. Plasma metal concentrations and Incident Coronary Heart Disease in Chinese adults: the Dongfeng-Tongji Cohort. Environ Health Perspect. 2017;125(10):107007.
Karabağ Y, Çınar T, Çağdaş M, Rencüzoğulları İ, Tanık VO. In-hospital and long-term prognoses of patients with a mid-range ejection fraction after an ST-segment myocardial infarction. Acta Cardiol. 2019;74(4):351–8.
Acknowledgements
Our study was supported by the Fasa University of Medical Sciences (approval number: 401013), and the authors would like to thank the staff for their support and data sharing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
R.T, Z.N, M.R and MR.M worked on conception or design of the work and Z.N and M.R cooperated in data collection. R.T, M.R, MR.M, S.K and M.R analyzed and interpreted the data and R.T, M.R, S.K, MS.N and Z.N drafted the manuscript and all authors read and approved the final version of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research methodology and ethical consideration of this study was approved by the ethical committee of FASA university of medical sciences (approval code: IR.FUMS.REC.1401.195).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Naziri, Z., Rahimlou, M., Rezaei, M. et al. High dietary antioxidant intake linked to lower risk of myocardial infarction: a nested case-control study. BMC Cardiovasc Disord 24, 485 (2024). https://doi.org/10.1186/s12872-024-04158-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-04158-6