Abstract
Background
Theoretically, a rapid urease test (RUT) using a swab of the gastric wall (Swab-RUT) for Helicobacter pylori (H. pylori) is safe. However, the validity and utility of Swab-RUT remain unclear. Therefore, we assessed the validity and utility of Swab-RUT compared to RUT using mucosal forceps of the gastric wall (Forceps-RUT) and 13C-urea breath test (UBT).
Methods
This study was a multicenter prospective observational study. When the examinees were suspected of H. pylori infection during esophagogastroduodenoscopy, we performed Swab-RUT and Forceps-RUT continuously. When the examinees were not suspected of H. pylori infection, we performed Swab-RUT alone. We validated the status of H. pylori infection using UBT.
Results
Ninety-four examinees were enrolled from four institutions between May 2016 and December 2020 (median age [range], 56.5 [26–88] years). In this study, the sensitivity, specificity, and accuracy of Swab-RUT to UBT were 0.933 (95% confidence interval: 0.779–0.992), 0.922 (0.827–0.974), and 0.926 (0.853–0.970), respectively. The Kappa coefficient of Swab-RUT to UBT was 0.833, and that of Swab-RUT to forceps-RUT was 0.936. No complications were observed in this study.
Conclusions
Swab-RUT is a valid examination for the status of H. pylori infection compared to the conventional Forceps-RUT.
Similar content being viewed by others
Background
Gastric cancer (GC) is the sixth most common cancer and the third most common cause of cancer-related deaths [1]. The incidence and mortality rates of GC are expected to increase worldwide [2]. Helicobacter pylori (H. pylori) is an established risk factor for GC, occupying 65–80% of all GC cases [3, 4], with an odds ratio of 21 for H. pylori infection in patients with GC [5]. Its eradication is a robust measure to reduce the incidence of GC and GC-related deaths [6,7,8]. Moreover, H. pylori is related to other diseases, including peptic ulcer, gastric mucosa-associated lymphoid tissue lymphoma and Idiopathic thrombocytopenic purpura, and H. pylori eradication therapy is also a strong treatment for them [9,10,11]. Therefore, the diagnosis of H. pylori is indispensable as a first step to eradicate H. pylori infection and reduce H. pylori-related diseases.
Diagnostic methods for H. pylori infection include serum antibody, urinary antibody, stool antigen test, incubation, and rapid urease test (RUT) [12]. Although RUT is inexpensive, rapid, widely available, and highly specific, it inevitably requires forceps specimens through esophagogastroduodenoscopy (EGD). There is a considerably low risk (0.0016–0.07%), but not never, of post-biopsy bleeding in the stomach [13,14,15]. Since RUT is not a treatment but a diagnostic measure for asymptomatic examinees, it should comply with safety standards at an extremely high level.
A previous report showed that urease from gastric mucus matches RUT from the gastric mucosa using forceps [13]. Accordingly, we developed a new method for retrieving gastric mucus using a small swab for RUT (Swab-RUT). Although a previous report claimed that Swab-RUT provided higher sensitivity and accuracy for H. pylori infection, the study was performed at a single institution [14, 15]. Therefore, a validation study in multicenter from a different country was required.
This study aimed to assess the validity and usefulness of gastric mucus by Swab-RUT compared with conventional gastric mucosa using forceps for RUT (Forceps-RUT) as a multicenter study.
Methods
Study design and examinees
This prospective cross-sectional study was conducted at four institutions. we recruited examinees who underwent EGD at the Medical Research Institute KITANO HOSPITAL (Osaka, Japan), Kawasaki Medical School Hospital (Okayama, Japan), Medical Check Center of Kawasaki Medical School (Okayama, Japan), and Hyogo Prefectural Awaji Medical Center (Hyogo, Japan) between March 2016 and December 2020. First, we performed EGD on the examinees who provided informed consent and underwent H. pylori infection assessment according to the Kyoto classification [16]. When we suspected H. pylori infection, we sequentially performed Swab-RUT and Forceps-RUT. 13C-urease breath test (UBT) was performed on the same day but more than 2 h after EGD was completed. When we assessed negatively for H. pylori infection, we performed only Swab-RUT and did not perform Forceps-RUT. UBT was performed on the same day but more than 2 h after EGD was completed.
The primary outcomes were the true positive rate, true negative rate, accuracy rate of Swab-RUT compared to Forceps-RUT, and the accuracy rate of Swab-RUT compared to UBT. All endoscopists were board-certified fellows of the Japan Gastroenterological Endoscopy Society.
The inclusion criteria for this study were as follows: ≥20 years of age, Eastern Cooperative Oncology Group Performance Status Scale 0 and provision of written informed consent. The exclusion criteria were as follows: ≤19 years of age, history of H. pylori eradication, within 4 weeks after H. pylori eradication, prescribing or stopping within 2 weeks of H2-blocker and proton pump inhibitors including potassium-competitive acid blocker, antithrombotic drugs use, overt bleeding in the stomach, strong vomiting reflex during EGD, American Society of Anesthesiologists physical status ≥ 3, doctors judged that the examinees were inappropriate. Ninety-four patients were enrolled, and 41 underwent Forceps-RUT simultaneously.
The following variables were collected from medical records: age, sex, and complications. The following variables were collected during EGD: sodium bicarbonate use. Sodium bicarbonate use depended on the endoscopists’ intention.
RUT
For Swab-RUT, we prepared small or large (1-mm or 3-mm in original compressed form, around 5-mm or 7-mm in expanded form just before examination) cotton in advance (Fig. 1A). We swabbed the anterior wall of the gastric antrum with one absorbent cotton grasped with forceps and retrieved the cotton throw from the channel (Fig. 1B). The anterior wall of the upper corpus was swabbed with another piece of cotton and was retrieved (Fig. 1C). These two pieces of cotton were embedded in separate RUT kits and were judged positive for H. pylori when the color of at least one kit changed in 2 h. The cotton size (small or large) was recorded for analysis. For Forceps-RUT, we obtained one biopsy sample from the mucosa of the anterior wall of the gastric antrum, and another from the anterior wall of the upper corpus by forceps. Sodium bicarbonate has a pH of 8.5, which may affect the RUT results; therefore, we carefully cleaned the channel and stomach with water if sodium bicarbonate was used. RUT was performed by urease test tubes (Helicocheck®, Otsuka Pharmaceutical, Tokyo, Japan), and each RUT sample was blinded.
UBT
UBT was performed more than 2 h after EGD was finished. UBT was performed using 100 mg of Urea (13C) (UBIT®, Otsuka Pharmaceutical, Tokyo, Japan). We collected exhaled breath 20 min after the examinees took 13C-Urea.
Statistics
We had estimated that the accuracy rate of Forceps- RUT and Swab-RUT to UBT was 0.70 and 0.80, respectively. Non-inferiority margin was set to 0.15 with alpha value of 0.05 and a power of 80%. Calculation estimated that ideal sample size was 48. The Kappa coefficient was used to compare the match rates of the different tests. The magnitudes of the kappa coefficient were assessed as follows: ≤0 = poor, 0.01–0.20 = slight, 0.21–0.40 = fair, 0.41–0.60 = moderate, 0.61–0.80 = substantial, and 0.81–1 = almost perfect [17]. Logistic regression analysis was performed to predict the association of categorized explanatory variables with the binary group. The McNemar’s test was performed to determine the differences in paired binary data. The kappa coefficient, logistic regression analysis, and the McNemar’s test were performed using EZR (version 1.51; Jichi Medical University, Saitama, Japan) [18]. P values of < 0.05 were considered statistically significant.
Study approval
This study was approved by the Ethics Committees of Kitano Hospital (1601004, 04/17/16), Kawasaki Medical School (2529, 10/17/16), and Hyogo Prefectural Awaji Medical Center (30 − 15, 08/02/18), and written informed consent was obtained from all the participants. The study was conducted in accordance with the Declaration of Helsinki.
Results
Examinees’ characteristics
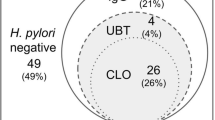
A flowchart of the study is shown in Fig. 2, and the examinees’ characteristics are summarized in Table 1. The mean age (range) was 56.5 (26–88) years, and 52 (57.3%) examinees were men. Sixty-seven (71.3%) examinees had atrophic gastritis. Sodium bicarbonate was used in 60 (63.8%) cases. Thirty (31.9%) tested positive for UBT. No complications were observed in this study.
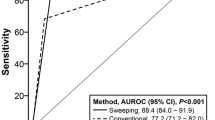
Swab-RUT
The results relating Swab-RUT to UBT are listed in Table 2. The positive rate for Swab-RUT was 35.1% (33/94). The sensitivity, specificity, and accuracy of Swab-RUT to UBT were 0.933 (95%CI: 0.779–0.992), 0.922 (0.827–0.974), and 0.926 (0.853–0.970), respectively. The positive predictive value (PPV) and negative predictive value (NPV) of Swab-RUT to UBT were 0.848 (0.681–0.949) and 0.967 (0.887–0.996). The Kappa coefficient was 0.833 (0.714–0.952). A mismatch between the result of each RUT acquired from the antrum and the corpus occurred in 1/94 (1.1%) examinee.
In addition, we analyzed the influence of sodium bicarbonate on Swab-RUT (Table 3). The sensitivity, specificity, and accuracy of Swab-RUT to UBT with sodium bicarbonate were 0.952 (0.762–0.999), 0.872 (0.726–0.957) and 0.900 (0.795–0.962), respectively. The PPV and NPV of Swab-RUT to UBT with sodium bicarbonate were 0.800 (0.593–0.932) and 0.971 (0.851–0.999), respectively. The Kappa coefficient was 0.789 (0.630–0.949).
Logistic regression analysis showed that the cotton size used for Swab-RUT did not affect the accuracy of UBT (OR:6.270 [0.279–141], p = 0.248).
Next, we compared the accordance of Swab-RUT with that of Forceps-RUT (Table 4). The sensitivity and specificity of Swab-RUT for Forceps-RUT were 0.967 (0.828–1.000) and 1.000 (0.615–1.000), respectively. The accuracy of Swab-RUT was 0.976 (0.871–0.999). The kappa coefficient of Swab-RUT to Forceps-RUT was 0.936 (0.823–1.057). The McNemar’s test showed no difference between Swab-RUT and Forceps-RUT groups (p = 1.000).
These findings showed that Swab-RUT has a good accordance with Forceps-RUT and UBT.
Discussion
In this study, we confirmed that Swab-RUT harbored good agreement with UBT at the multicenter level. Swab-RUT was compatible with Forceps-RUT. The accuracy of Swab-RUT maintained by the use of sodium bicarbonate, which are commonly used during EGD. Swab-RUT was proved to be safe, and small cotton pieces were sufficient to obtain accurate results.
RUT has been conventionally assessed using forceps specimen. Forceps damage the gastric mucosa and bear the risk of post-forceps bleeding. In contrast, Swab-RUT do not damage the mucosa and cause post-examination bleeding because Swab-RUT only rubs the mucosa. Although this study excluded examinees with antithrombotic drugs or poor PS, Swab-RUT may be performed safely for such examinees. Moreover, the conventional forceps method can only reflect H. pylori status within the forceps cup. However, Swab-RUT can integrate H. pylori status from a broader area of the gastric mucosa.
Small pieces of cotton were used in this study. The diameter of the cotton varied as small or large (1–3 mm). However, the cotton size did not affect the accuracy rate of H. pylori infection. Even 1-mm cotton could collect enough H. pylori to obtain a positive result. Such a small size of cotton allows us to use the commercially available RUT kit for forceps specimens. There is no need to prepare special equipment to perform Swab-RUT.
In this study, specificity of Swab-RUT to UBT with sodium bicarbonate was lower than Swab-RUT to UBT in total. False positive cases affected the result, and limited the Kappa coefficient of Swab-RUT to UBT with sodium bicarbonate to substantial. Sodium bicarbonate has a pH of 8.5 and is often used for the stability of pronase to liquefy mucins in the stomach. In addition, RUT utilizes a ph-dependent indicator and color of RUT kit changes from negative to positive by alkalization. However hard the channel and the stomach were cleaned with water, the remaining sodium bicarbonate might contribute on false positive.
This study has some limitations. First, the sample size was relatively small. Second, we validated the status of H. pylori infection using only one method (UBT) and we did not verify the status of H. pylori infection by histological analysis, H. pylori polymerase chain reaction or 16 S rRNA sequencing. Although UBT is a well-accepted method for diagnosing H. pylori infection, false positives and negatives sometimes occur. However, PCR or 16 S rRNA sequencing is not a gold standard in busy daily clinical situations. Therefore, the validation by UBT matches the real-world practice. Third, we did not regulate the number and extent of sweeps during Swab-RUT. The number and extent of sweeping depended on the facility and the endoscopist. In addition, cotton is not approved within insurance coverage in Japan. Fourth, no complications occurred in this study for both Swab-RUT and Forceps-RUT, partially because the examinees taking antithrombotic drugs were excluded. Therefore, we could not analyze the superiority of Swab-RUT to Forceps-RUT regarding safety. Finally, forceps-RUT was not performed in all cases. In this study, the examinees did not undergo forceps-RUT if they were not suspected of H. pylori infection thought EGD. The accuracy, mainly NPV, of swab-RUT to forceps-RUT might be underestimated.
Conclusions
In conclusion, Swab-RUT has a good accuracy rate for H. pylori infection with high safety. Since Swab-RUT is a convenient, universal, safe, and inexpensive method, it is suitable for screening for H. pylori infection during EGD. Swab-RUT could be a reliable option to Forceps-RUT, when biopsy samples are not available or not preferred.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
- EGD:
-
Esophagogastroduodenoscopy
- GC:
-
Gastric Cancer
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PS:
-
Performance status
- RUT:
-
Rapid Urease Test
- UBT:
-
Urea Breath Test
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Morgan E, Arnold M, Camargo MC, Gini A, Kunzmann AT, Matsuda T, Meheus F, Verhoeven RHA, Vignat J, Laversanne M, et al. The current and future incidence and mortality of gastric cancer in 185 countries, 2020-40: a population-based modelling study. EClinicalMedicine. 2022;47:101404.
Helicobacter C, Collaborative G. Gastric cancer and Helicobacter pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut. 2001;49(3):347–53.
de Martel C, Ferlay J, Franceschi S, Vignat J, Bray F, Forman D, Plummer M. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13(6):607–15.
Gonzalez CA, Megraud F, Buissonniere A, Lujan Barroso L, Agudo A, Duell EJ, Boutron-Ruault MC, Clavel-Chapelon F, Palli D, Krogh V, et al. Helicobacter pylori infection assessed by ELISA and by immunoblot and noncardia gastric cancer risk in a prospective study: the Eurgast-EPIC project. Ann Oncol. 2012;23(5):1320–4.
Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, Graham DY. Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology. 2016;150(5):1113–e11241115.
Tsuda M, Asaka M, Kato M, Matsushima R, Fujimori K, Akino K, Kikuchi S, Lin Y, Sakamoto N. Effect on Helicobacter pylori eradication therapy against gastric cancer in Japan. Helicobacter. 2017;22(5).
Chiang TH, Chang WJ, Chen SL, Yen AM, Fann JC, Chiu SY, Chen YR, Chuang SL, Shieh CF, Liu CY, et al. Mass eradication of Helicobacter pylori to reduce gastric cancer incidence and mortality: a long-term cohort study on Matsu Islands. Gut. 2021;70(2):243–50.
Thiede C, Morgner A, Alpen B, Wundisch T, Herrmann J, Ritter M, Ehninger G, Stolte M, Bayerdorffer E, Neubauer A. What role does Helicobacter pylori eradication play in gastric MALT and gastric MALT lymphoma? Gastroenterology. 1997;113(6 Suppl):S61–64.
Suzuki T, Matsushima M, Masui A, Watanabe K, Takagi A, Ogawa Y, Shirai T, Mine T. Effect of Helicobacter pylori eradication in patients with chronic idiopathic thrombocytopenic purpura-a randomized controlled trial. Am J Gastroenterol. 2005;100(6):1265–70.
Chan FK, Sung JJ, Chung SC, To KF, Yung MY, Leung VK, Lee YT, Chan CS, Li EK, Woo J. Randomised trial of eradication of Helicobacter pylori before non-steroidal anti-inflammatory drug therapy to prevent peptic ulcers. Lancet. 1997;350(9083):975–9.
Garza-Gonzalez E, Perez-Perez GI, Maldonado-Garza HJ, Bosques-Padilla FJ. A review of Helicobacter pylori diagnosis, treatment, and methods to detect eradication. World J Gastroenterol. 2014;20(6):1438–49.
Matsumoto H, Shiotani A, Nishibayashi H, Kamada T, Kimura T, Fujimura Y, Nakato R, Murao T, Fujita M, Haruma K. Molecular detection of H. Pylori using adherent gastric mucous to biopsy forceps. Helicobacter. 2016;21(6):548–53.
Noh CK, Lee GH, Park JW, Roh J, Han JH, Lee E, Park B, Lim SG, Shin SJ, Cheong JY, et al. Diagnostic accuracy of sweeping method compared to conventional sampling in rapid urease test for Helicobacter pylori detection in atrophic mucosa. Sci Rep. 2020;10(1):18483.
Soh H, Kim N, Moon J, Lee HM, Kim B, Cho SJ, Kim SG, Chung H. Gastric mucosal swab as an alternative to biopsy for Helicobacter pylori detection. Helicobacter. 2023;28(3):e12980.
Kamada T, Haruma K, Inoue K, Shiotani A. [Helicobacter pylori infection and endoscopic gastritis -Kyoto classification of gastritis]. Nihon Shokakibyo Gakkai Zasshi. 2015;112(6):982–93.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48(3):452–8.
Acknowledgements
None.
Funding
This research received external funding from the Institute of Immunology Co., Ltd. (Tokyo, Japan).
Author information
Authors and Affiliations
Contributions
Conceptualization: AY, KK; data curation: AY, KK, TM, TK, MS; investigation: TY; methodology: TY; supervision: AYi, TM, TK, MS, KK, KH, TK, SY; writing-original draft: TK.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committees of Kitano Hospital (1601004, 04/17/16), Kawasaki Medical School (2529, 10/17/16), and Hyogo Prefectural Awaji Medical Center (30 − 15, 08/02/18), and written informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yoshikawa, T., Yamauchi, A., Kou, T. et al. Validity of rapid urease test using swab of gastric mucus to mucosal forceps and 13 C-urease breath test: a multicenter prospective observational study. BMC Gastroenterol 24, 258 (2024). https://doi.org/10.1186/s12876-024-03344-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03344-2