Abstract
Background
This study aimed to develop a tool for predicting the early occurrence of acute kidney injury (AKI) in ICU hospitalized cirrhotic patients.
Methods
Eligible patients with cirrhosis were identified from the Medical Information Mart for Intensive Care database. Demographic data, laboratory examinations, and interventions were obtained. After splitting the population into training and validation cohorts, the least absolute shrinkage and selection operator regression model was used to select factors and construct the dynamic online nomogram. Calibration and discrimination were used to assess nomogram performance, and clinical utility was evaluated by decision curve analysis (DCA).
Results
A total of 1254 patients were included in the analysis, and 745 developed AKI. The mean arterial pressure, white blood cell count, total bilirubin level, Glasgow Coma Score, creatinine, heart rate, platelet count and albumin level were identified as predictors of AKI. The developed model had a good ability to differentiate AKI from non-AKI, with AUCs of 0.797 and 0.750 in the training and validation cohorts, respectively. Moreover, the nomogram model showed good calibration. DCA showed that the nomogram had a superior overall net benefit within wide and practical ranges of threshold probabilities.
Conclusions
The dynamic online nomogram can be an easy-to-use tool for predicting the early occurrence of AKI in critically ill patients with cirrhosis.
Graphical Abstract

Similar content being viewed by others
Background
Acute kidney injury (AKI) is characterized by a swift and pronounced decline in renal function, making it one of the most prevalent complications among patients with severe cirrhosis, particularly those admitted to the intensive care unit (ICU) [1]. It is reported that AKI occurs in approximately 20-50% of hospitalized patients with cirrhosis and is associated with a high risk of death during hospitalization and after discharge, as well as higher length of hospital stay (LOS) and higher resource utilization [2, 3]. A previous study showed that AKI markedly increased mortality in ICU patients with cirrhosis, the 15-day and 30-day cumulative mortality can be 22.5% and 42.1%, respectively [4]. AKI develops rapidly in ICU patients with cirrhosis, with a median time of occurrence of 2–4 days, and the in-hospital mortality rate is extremely high, which can reach 29.8% [5, 6]. Early diagnosis and treatment of AKI are essential for reducing mortality and improving prognosis. Therefore, early identification of cirrhotic ICU patients at high risk for AKI is crucial for timely intervention and improved prognosis.
In the past decade, a number of studies have focused on identifying the risk factors for the development of AKI in patients with cirrhosis [7,8,9] and other specific clinical situations (such as after cardiac surgery, hospital acquisition, contrast exposure, general surgery, high-risk surgery, etc.) [10,11,12,13,14]. Some studies have also investigated the risk of AKI in ICU patients, however, these studies have not fully considered the competitive risk of death for AKI, and have not constructed a short-term mortality risk after admission [5, 6, 15]. Given the high incidence, rapid progression, and high short-term mortality rate of AKI in ICU hospitalized patients with cirrhosis, we believe that developing a simple short-term predictive model is crucial.
Multiparameter Intelligent Monitoring in Intensive Care Database IV (MIMIC-IV) is a large public relations database. It collected the clinical data of more than 380,000 patients admitted to the Beth Israel Deaconess Medical Center in Boston, Massachusetts, from 2008 to 2019, including demographic information, laboratory examination, medication, vital signs, surgical procedures, disease diagnosis, drug management, survival status, and other details. Using the MIMIC database, researchers have analyzed the relationship between AKI and mortality in critically ill sepsis patients [16], established a prediction model for the risk of AKI in septic patients [17], and created a prognostic model for diabetic patients with AKI [18]. However, there is no relevant research or clinical prediction model for the risk assessment of AKI within 7 days after admission in ICU patients with liver cirrhosis. Therefore, we conducted this analysis with the aim of developing a simple and clinically useful dynamic nomogram that includes the most prominent parameters to predict the early occurrence of AKI in critically ill patients with cirrhosis. We believe that it is necessary to develop an improved AKI early clinical risk prediction tool in the ICU to provide doctors with practical information about precautions, early diagnosis, and targeted intervention.
Methods
Source of data
The MIMIC database was created by the Massachusetts Institute of Technology (MIT) and approved by the Institutional Review Board (IRB) of the Beth Israel Deaconess Medical Center (No. 2001-P-001699/15). We applied the version of MIMIC-IV v2.0 released on June 12, 2022. This retrospective observational study used database management software and structured query language (SQL) to extract the clinical data of patients. All relevant data were exported, processed, and analyzed using data analysis software. Such an analysis has no impact on the treatment of patients and is safe. The author Tu. H obtained the Collaborative Institutional Training Initiative (CITI) license (certification No. 51704839) and the right to use the MIMIC-IV v2.0 database according to the relevant regulations. The work described has been carried out following The Code of Ethics of the World Medical Association (Declaration of Helsinki). Since all protected private information had been identified and deleted, informed consent from patients was no longer required.
Population selection criteria
All patients with cirrhosis who were hospitalized for the first time in the MIMIC IV v2.0 database were screened. If there were multiple ICU stays during hospitalization, the data from the first ICU admission were used. The diagnosis of cirrhosis was combined with histological diagnosis or imaging findings with clinical manifestations (such as ascites, esophageal varices, sepsis, gastrointestinal bleeding, progressive jaundice, hepatic encephalopathy, or spontaneous bacterial peritonitis). The diagnosis and staging of AKI referred to the standard of Kidney Disease Improving Global Outcomes (KDIGO): Stage I: Increase in serum Cr (sCr) of 0.3 mg/dl within 48 h, increase of 1.5-2×baseline Cr in the last 7 d, or urine output (UOP) < 0.5 ml/kg/h for 6–12 h; Stage 2: 2–3×baseline sCr or UOP < 0.5 ml/kg/h for at least 12 h; Stage 3: 3×baseline sCr, increase of 0.5 mg/dl above the absolute level of 4.0 mg/dl, on renal replacement therapy (RRT), UOP < 0.3 ml/kg/h for 24 h, or 12 h of anuria. The baseline creatinine for this study is defined as the most recent creatinine value before admission to the ICU. If the patient’s creatinine value was not measured before admission to the ICU, the first creatinine value measured after admission to the ICU is used as the baseline creatinine.
In order to reduce the competitive risk of death for AKI, we have implemented stricter inclusion of patients to minimize patient deaths caused by other serious extrahepatic events. The exclusion criteria were as follows: (1) length of stay in the ICU was less than 48 h or died within 48 h after ICU admission; (2) age < 18 and > 80 years; (3) liver cancer or other malignant tumors; (4) complications such as myocardial infarction, congestive heart failure, cerebrovascular disease, chronic complications of diabetes, AIDS, and other life-threatening extrahepatic organ diseases; (5) liver transplantation performed before admission or during the hospital stay; (6) diagnosis of chronic kidney disease (CKD); and (7) occurrence of AKI before admission. CKD diagnosis refers to the KDIGO guidelines, defined as sustained renal structural or functional abnormalities (GFR < 60 ml/min/1.72 m2) > 90 days [19].
Research variables
As our goal is to construct the probability of AKI occurring within 7 days after ICU admission, patients with AKI after 7 days of admission were further excluded. Data on each patient, including demographic characteristics, vital signs, comorbidities and complications, laboratory examinations, and interventions, were obtained from MIMIC-IV 2.0. Demographic characteristics including age and sex were collected from the original database. Vital signs, including respiratory rate (RR, beats/min), heart rate (HR, beats/min), temperature (Temp, °C), mean arterial pressure (MAP), and arterial oxygen saturation (SpO2) upon ICU admission, were collected from charting at CHARTERS. Laboratory parameters, including WBC count, hemoglobin (Hb), platelet count (PLT), INR, BUN, creatinine (Cr), sodium (Na), chloride (Cl), potassium (K), calcium (Ca), total bilirubin (TB), ALT, AST, albumin (Alb) level, and blood glucose (Glu) were recorded in the table of laboratory events. Hospital interventions, including mechanical ventilation, RRT, and the use of vasoactive drugs and antibiotics were recorded. Model for End-Stage Liver Disease score (MELD), systemic inflammatory response syndrome (SIRS) score, Glasgow Coma Score (GCS), and urine volume (UV) were calculated using the data from the first 24 h of ICU stay. All comorbidities and complications were identified according to the ICD-9 or ICD-10 code records. The length of hospitalization, in-hospital mortality, and mortality at 28 days, 90 days, and 1 year after discharge were calculated using the original database.
Missing data handling
Missing data is widespread in the MIMIC database. The missing values of the variables included in this study are all < 20%. When filling in missing data, continuous variables with a normal distribution are supplemented with the mean, while variables with a skewed distribution are supplemented with the median. Besides, there are no missing values in the binary variables we included.
Statistical analysis
Eligible patients were divided into training and validation cohorts with a split ratio of 2: 1. Data from the training cohort were used to construct the dynamic nomogram, whereas data from the validation cohort were used to validate the model. Continuous variables were expressed as the mean (SD) or median and interquartile range and analyzed using the unpaired t-test or Wilcoxon rank-sum test, as appropriate. Categorical variables are presented as frequencies and percentages and were analyzed using Fisher’s exact test. Independent risk factors for predicting the occurrence of AKI in patients with cirrhosis were screened using a training cohort based on the least absolute shrinkage and selection operator (LASSO) logistic regression [20], which is a shrinkage method that can actively select from a large and potentially multicollinear set of variables in the regression, resulting in a more relevant and interpretable set of predictors. A nomogram model was established using the screened independent risk factors as variables, and an interactive web-based dynamic nomogram application was built using Shiny. The nomogram performance was assessed using discrimination and calibration. The discriminative ability of the model was determined using the area under the receiver operating characteristic curve [21]. The prediction model was calibrated using a visual calibration plot comparing the predicted and actual probabilities of AKI. A decision curve analysis was also performed to determine the net benefit threshold of prediction [22]. All the above analyses were repeated 1000 times using bootstrap to reduce the deviation.
The statistical significance of all analyses was set at P level less than 0.05. IBM SPSS Statistics (version 22.0; IBM Corporation, Armonk, New York, USA) and R version 4.2.2 (The R Foundation for Statistical Computing, Austria, and Vienna) were used as the analysis software in this study.
Results
Baseline characteristics
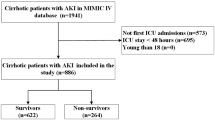
The procedure for patient selection is illustrated in Fig. 1. A total of 1254 patients with liver cirrhosis were included in the analysis. Among them, 745 patients (59.4%) developed AKI within 7 days of entering the ICU. The characteristics of the eligible patients are shown in Table 1. Subsequently, these 1254 patients were randomly divided into the training and validation cohorts with a split ratio of 2: 1. Baseline clinical data were similar between the training and validation cohorts (Table 2). AKI was detected in 58.9% (492/836) and 60.5% (253/418) of the patients in the training and validation sets, respectively.
As shown in Table 1, there was no significant difference in age and sex between patients with AKI and those without AKI. Patients without AKI had a higher proportion of hypertension [190 (37.3%) vs. 236 (31.7%), P = 0.038], but there was no significant difference in the incidence of diabetes and COPD. 62.0% of the enrolled population had alcohol related cirrhosis was the cause of cirrhosis, but there was no difference between the AKI and non-AKI group. In terms of liver cirrhosis complications, the people with AKI were more likely to have hydrothorax, ascites, jaundice, hepatic encephalopathy, and infection than those without AKI. The admission risk score was higher in the MELD score [22.67 ± 9.75 vs. 16.58 ± 8.35, P < 0.001] and SIRS score [3 (2–3) vs. 2 (2–3), P < 0.001] in the AKI group than that in the non-AKI group. The GCS score [13 (9–15) vs. 15 (14–15), P < 0.001] in the AKI group was lower than that in the non-AKI group. In addition, the usage proportions of renal replacement therapy, mechanical ventilation, vasoactive drugs, and antibiotics in AKI group were higher than those in non-AKI group, the length of hospitalization were also longer. From the perspective of prognosis, the hospital mortality [168 (22.6%) vs. 9 (1.8%), P < 0.001], 28 day mortality [220 (29.5%) vs. 22 (4.3%), P < 0.001], 90 day mortality [255 (34.2%) vs. 43 (8.4%), P < 0.001] and one-year mortality [309 (41.5%) vs. 95 (18.7%), P < 0.001] of patients with AKI were significantly higher than those without AKI.
Factor associated with AKI development and nomogram development
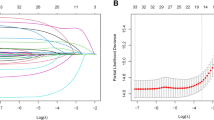
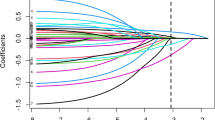
Twenty-six variables, including age, sex, vital signs, comorbidities, and laboratory tests, were measured at hospital admission in the training cohort (Table 3). In the comparison between the AKI and non-AKI groups, variables with P < 0.1 were included in the LASSO regression. Nineteen variables (Temp, HR, RR, MAP, GCS, WBC, Hb, PLT, INR, BUN, Cr, Na, Cl, Ca, TB, ALT, AST, Glu and Alb) were included in the original model and were later reduced to eight potential predictors (MAP, WBC, TB, GCS, Cr, Alb, HR and PLT) using the LASSO regression model. A coefficient profile plot and cross-validated error plot of the LASSO regression model are shown in Fig. 2A and B. The most regularized and parsimonious model, included eight variables, as shown by the left vertical dashed line in Fig. 2B. The final logistic model incorporated eight independent predictors (Fig. 2C) and was developed as a simple-to-use nomogram, as shown in Fig. 2D, and available online (https://yixueliexiantumoxing.shinyapps.io/AKIprediction/), as shown in Fig. 2E.
Factors associated with AKI development and Nomogram Development. (A) LASSO coefficient profiles of the 19 baseline features. (B) Tuning parameter (λ) selection in the LASSO model used 1000-fold cross-validation via minimum criteria. (C) Predictors of AKI obtained by LASSO regression analysis in the training cohort. (D) Established nomogram for the early prediction of AKI in critically ill patients with cirrhosis. (E) Online dynamic nomogram accessible at https://yixueliexiantumoxing.shinyapps.io/AKIprediction/
Nomogram validation
After constructing the model, the area under the receiver operating characteristic curve (AUC) was used to assess the accuracy of the model. The receiver operating characteristic (ROC) curves are shown in Fig. 3A and B, which show that the model has a good ability to differentiate AKI from non-AKI among critically ill patients with cirrhosis, with AUCs of 0.797 and 0.750 in the training and validation cohorts, respectively. To further verify the validity of the model, a calibration curve was constructed using R software (Fig. 3C and D). The predictive probabilities of the model were consistent with the observation results in both the training and validation cohorts, suggesting good calibration. Finally, DCA curve analysis (Fig. 3E and F) visually showed that the nomogram had superior overall net benefit within the wide and practical ranges of threshold probabilities, thereby indicating that the nomogram had significant predictive value.
The AUC of the nomogram for the early prediction of AKI in critically ill patients with cirrhosis was 0.797 in the training cohort (A) and 0.750 in the validation cohort (B). Calibration curves of the predicted nomogram in the training cohort (C) and validation cohort (D). Decision curve analysis of the nomogram in the training cohort (E) and the validation cohort (F). AUC: area under the receiver operating characteristic curve
Discussion
To the best of our knowledge, this is the first study to develop and validate a convenient and practical dynamic nomogram for detecting the risk of AKI occurring within 7 days after admission to the ICU in patients with cirrhosis using the MIMIC IV 2.0 database. Short-term AKI risk prediction models facilitate medical decision-making when critically ill patients with cirrhosis are admitted to the ICU and facilitate early identification or implementation of preventive measures to improve the prognosis of AKI. Multiple studies have reported prediction models for AKI in different clinical settings [10, 17, 23, 24]. However, the number of cases in these studies was small, and a short-term prediction model for AKI in critically ill patients with cirrhosis after admission to the ICU is lacking. The increase in the computerization of ICU has generated large electronic databases that are suitable for “big data” research. Using machine learning algorithms to analyze large datasets and develop models for prognostication or decision support in critical care could be a cost-effective alternative to biomarkers for AKI prognostication.
In recent years, a specific modern technique, the least absolute shrinkage and selection operator (LASSO), has attracted much attention [25]. Traditional regression techniques are limited in the analysis and synthesis of large numbers of covariates, including multicollinear variables, but thus far, the majority of the data on AKI and cirrhosis have utilized traditional statistical techniques [5]. LASSO is a regression-based methodology that allows for a large number of covariates in a model. Importantly, it has the unique characteristic of penalizing the absolute value of a regression coefficient; thus, regulating the influence a coefficient may have on the overall regression. The greater the penalization, the greater the coefficient shrinkage, with some coefficients reaching zero, thus automatically removing unnecessary/uninfluential covariates [26]. The logistic LASSO model can actively select from a large and potentially multicollinear set of variables in the regression, resulting in a more relevant and interpretable set of predictors [27]. Therefore, in the present study, we aimed to investigate the relationship between baseline characteristics, vital signs, laboratory test results, and other risk factors on the early occurrence of AKI in critically ill patients with cirrhosis.
Our study has several strengths. Most of the major risk variables associated with AKI were included in the study, and the risk model development was based on parameters available to clinicians, thereby providing clinically relevant information in the management of patients with cirrhosis. MAP, WBC, TB, GCS, Cr, Alb, HR and PLT were included in this nomogram, making it an objective and simple-to-use tool to screen patients for AKI in a dynamic online manner. The proposed dynamic nomogram showed good performance in discrimination, calibration, and clinical application, providing valuable information for the decision-making of appropriate therapy options for individual patients. Moreover, it fills the gap between the high incidence and rapid development of AKI in ICU cirrhosis patients and the lack of a reliable clinical predictive model. Our findings also confirm that the mortality of AKI patients in the ICU is high, and the length of hospital stay (LOS) is increasing, which supports the necessity of identifying high-risk patients. These patients could benefit from monitoring and primary prevention strategies to reduce the incidence of AKI.
Our model showed that lower MAP, GCS, PLT and Alb; higher WBC, HR, TB and Cr were related to the early occurrence of AKI in patients with cirrhosis. The risk factors we used for the identification of AKI were consistent with previous AKI literature. Rise in sCr is the cornerstone of AKI diagnosis, consistent with other studies, our study also found that sCr levels upon admission can identify patients with cirrhosis at risk of developing AKI during hospitalization [5]. The kidneys account for less than 5% of our body weight but receive approximately 25% of our cardiac output. Therefore, targeting adequate renal perfusion is considered a potential factor in changing the risk of AKI [28]. MAP is widely used as an index for optimal blood pressure, and previous studies have shown that the incidence of serious renal adverse events is higher in patients with lower blood pressure [29, 30]. Increased HR is the primary mechanism for compensatory adaptation to low blood volume [31]. In the ICU, the GCS scoring system is commonly used to evaluate the severity of a patient’s condition. Our results revealed that patients with a low GCS score were more likely to develop AKI, which is consistent with previous studies [32, 33]. Infection, particularly sepsis, is the most important risk factor for renal function [34]. A high WBC count, a surrogate of systemic inflammation, is a known independent predictor of mortality in patients with advanced cirrhosis and is a driver for the development of AKI [35]. Elevated WBC count has also been found to be associated with renal dysfunction in patients with spontaneous bacterial peritonitis (SBP) [15] and alcoholic hepatitis [36]. Hyperbilirubinemia can be found in 60% of AKI patients. Elevated serum bilirubin levels are an independent risk factor for AKI [37]. An increase in bilirubin can induce oxidative stress in renal tubular cells, induce apoptosis, aggravate renal ischemia-reperfusion injury, and lead to AKI [38, 39]. A decrease in PLT count in critically ill patients is a sign of severe clinical condition, and there is a research indicating a significant association between the reduction in PLT count and major adverse renal events in AKI patients [40]. Hypoalbuminemia is an important independent predictor of AKI occurrence and mortality in critically ill patients [41, 42]. The measurement of serum Alb has a positive significance in assessing AKI risk and predicting mortality after AKI.
This study has several limitations. First, although it was performed in a large cohort, selection bias might be unavoidable because this study was a retrospective analysis of secondary data. Second, the model was constructed based on a US population and developed and validated using the same database. Thus, its generalizability to the global population remains unclear. It was more reliable to validate it prospectively or at least in another database. Third, we only established a short-term prediction model for AKI after admission, but a recent study shows that longitudinal AKI development is also important issue [43]. Therefore, in the future, we can further study the impact of AKI development on the long-term prognosis of patients, which may be a direction worthy of further research. In addition, this study did not delve into the etiology of AKI (Supplementary Table 1), so in the future, we can conduct in-depth research on AKI, which is crucial for timely and accurate identification of AKI and better understanding of the pathophysiological mechanisms that lead to renal dysfunction [44].
Conclusions
Through filtering by LASSO, eight independent predictive factors of early occurrence of AKI in ICU cirrhosis patients were selected to construct a dynamic online nomogram, including MAP, WBC, TB, GCS, Cr, Alb, HR and PLT. The proposed model exhibited good performance in terms of discrimination, calibration, and clinical applications. Through early assessment of the risk of AKI development, clinicians can implement measures that are beneficial for ICU patients with cirrhosis. Further studies are needed to externally validate our model using a large-sample prospective cohort study.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AKI:
-
Acute kidney injury
- ICU:
-
Intensive care unit
- MIMIC:
-
Medical Information Mart for Intensive Care
- LASSO:
-
Least absolute shrinkage and selection operator
- LOS:
-
Length of hospital stay
- CKD:
-
Chronic kidney disease
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CRP:
-
C-reactive protein
- INR:
-
International normalized ratio
- BUN:
-
Blood urea nitrogen
- RRT:
-
Renal replacement therapy
- MELD:
-
Model for End-Stage Liver Disease score
- SIRS:
-
Systemic inflammatory response syndrome score
- GCS:
-
Glasgow Coma Score
- UV:
-
Urine volume
- COPD:
-
Chronic Obstructive Pulmonary Disease
- HE:
-
Hepatic encephalopathy
- UGIB:
-
Upper gastrointestinal bleeding
- HR:
-
Heart rate; RR: respiratory rate
- MAP:
-
Mean arterial pressure
- SpO2:
-
Arterial oxygen saturation
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the receiver operating characteristic curve
- DCA:
-
Decision curve analysis
References
Zhou XD, Chen QF, Sun DQ, Zheng CF, Liang DJ, Zhou J, et al. Remodeling the model for end-stage liver disease for predicting mortality risk in critically ill patients with cirrhosis and acute kidney injury. Hepatol Commun. 2017;1(8):748–56.
Gupta K, Bhurwal A, Law C, Ventre S, Minacapelli CD, Kabaria S, et al. Acute kidney injury and hepatorenal syndrome in cirrhosis. World J Gastroenterol. 2021;27(26):3984–4003.
Angeli P, Gines P, Wong F, Bernardi M, Boyer TD, Gerbes A, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of ascites. Gut. 2015;64(4):531–7.
Liao T, Lu Y, Su T, Bei L, Li X, Lu Y, et al. Development and validation of prognostic nomogram for cirrhotic patients with acute kidney injury upon ICU admission. Intern Emerg Med. 2024;19(1):49–58.
Patidar KR, Xu C, Shamseddeen H, Cheng YW, Ghabril MS, Mukthinuthalapati V, et al. Development and validation of a model to Predict Acute kidney Injury in hospitalized patients with cirrhosis. Clin Translational Gastroenterol. 2019;10(9):e00075.
Li X, Li X, Zhao W, Wang D. Development and validation of a nomogram for predicting in-hospital death in cirrhotic patients with acute kidney injury. BMC Nephrol. 2024;25(1):175.
Karagozian R, Bhardwaj G, Wakefield DB, Verna EC. Acute kidney injury is associated with higher mortality and healthcare costs in hospitalized patients with cirrhosis. Ann Hepatol. 2019;18(5):730–5.
Vaz NF, da Cunha VNR, Cunha-Silva M, Sevá-Pereira T, de Souza Almeida JR, Mazo DF. Evolution of diagnostic criteria for acute kidney injury in patients with decompensated cirrhosis: a prospective study in a tertiary university hospital. Clin Res Hepatol Gastroenterol. 2020;44(4):551–63.
Khatua CR, Sahu SK, Meher D, Nath G, Singh SP. Acute kidney injury in hospitalized cirrhotic patients: risk factors, type of kidney injury, and survival. JGH open: Open Access J Gastroenterol Hepatol. 2021;5(2):199–206.
Malhotra R, Kashani KB, Macedo E, Kim J, Bouchard J, Wynn S, et al. A risk prediction score for acute kidney injury in the intensive care unit. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association -. Eur Ren Association. 2017;32(5):814–22.
Palomba H, de Castro I, Neto AL, Lage S, Yu L. Acute kidney injury prediction following elective cardiac surgery: AKICS score. Kidney Int. 2007;72(5):624–31.
Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44(7):1393–9.
Kheterpal S, Tremper KK, Heung M, Rosenberg AL, Englesbe M, Shanks AM, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology. 2009;110(3):505–15.
Grimm JC, Lui C, Kilic A, Valero V 3rd, Sciortino CM, Whitman GJ, et al. A risk score to predict acute renal failure in adult patients after lung transplantation. Ann Thorac Surg. 2015;99(1):251–7.
Navasa M, Follo A, Filella X, Jiménez W, Francitorra A, Planas R, et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology (Baltimore MD). 1998;27(5):1227–32.
Wang Z, Weng J, Yang J, Zhou X, Xu Z, Hou R, et al. Acute kidney injury-attributable mortality in critically ill patients with sepsis. PeerJ. 2022;10:e13184.
Yue S, Li S, Huang X, Liu J, Hou X, Wang Y, et al. Construction and validation of a risk prediction model for acute kidney Injury in patients suffering from septic shock. Dis Markers. 2022;2022:9367873.
Mo M, Pan L, Huang Z, Liang Y, Liao Y, Xia N. Development and validation of a Prediction Model for Survival in Diabetic patients with acute kidney Injury. Front Endocrinol. 2021;12:737996.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–84.
Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized Linear models via Coordinate Descent. J Stat Softw. 2010;33(1):1–22.
Zhou ZR, Wang WW, Li Y, Jin KR, Wang XY, Wang ZW, et al. In-depth mining of clinical data: the construction of clinical prediction model with R. Annals Translational Med. 2019;7(23):796.
Vickers AJ, Holland F. Decision curve analysis to evaluate the clinical benefit of prediction models. Spine Journal: Official J North Am Spine Soc. 2021;21(10):1643–8.
Feng LH, Lu Y, Ren S, Liang H, Wei L, Jiang J. Development and validation of a dynamic online nomogram for predicting acute kidney injury in cirrhotic patients upon ICU admission. Front Med. 2023;10:1055137.
Lu J, Qi Z, Liu J, Liu P, Li T, Duan M, et al. Nomogram Prediction Model of serum chloride and sodium ions on the risk of Acute kidney Injury in critically ill patients. Infect drug Resist. 2022;15:4785–98.
Hu JY, Wang Y, Tong XM, Yang T. When to consider logistic LASSO regression in multivariate analysis? Eur J Surg Oncology: J Eur Soc Surg Oncol Br Association Surg Oncol. 2021;47(8):2206.
McEligot AJ, Poynor V, Sharma R, Panangadan A. Logistic LASSO regression for dietary intakes and breast Cancer. Nutrients. 2020;12(9).
Wu Q, Jiang S, Cheng T, Xu M, Lu B. A Novel pyroptosis-related Prognostic Model for Hepatocellular Carcinoma. Front cell Dev Biology. 2021;9:770301.
Forni LG, Joannidis M. Blood pressure deficits in acute kidney injury: not all about the mean arterial pressure? Critical care (London. England). 2017;21(1):102.
Alrahbi S, Alaraimi R, Alzaabi A, Gosselin S. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. Cjem. 2018;20(2):256–9.
Panwar R, Lanyon N, Davies AR, Bailey M, Pilcher D, Bellomo R. Mean perfusion pressure deficit during the initial management of shock–an observational cohort study. J Crit Care. 2013;28(5):816–24.
Marzuillo P, Di Sessa A, Iafusco D, Capalbo D, Polito C, Nunziata F, et al. Heart rate cut-offs to identify non-febrile children with dehydration and acute kidney injury. Eur J Pediatrics. 2022;181(5):1967–77.
Wang RR, He M, Ou XF, Xie XQ, Kang Y. The predictive value of serum uric acid on acute kidney Injury following traumatic Brain Injury. Biomed Res Int. 2020;2020:2874369.
Moore EM, Bellomo R, Nichol A, Harley N, Macisaac C, Cooper DJ. The incidence of acute kidney injury in patients with traumatic brain injury. Ren Fail. 2010;32(9):1060–5.
Gomez H, Ince C, De Backer D, Pickkers P, Payen D, Hotchkiss J, et al. A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock (Augusta Ga). 2014;41(1):3–11.
Clària J, Stauber RE, Coenraad MJ, Moreau R, Jalan R, Pavesi M, et al. Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology (Baltimore MD). 2016;64(4):1249–64.
Altamirano J, Fagundes C, Dominguez M, García E, Michelena J, Cárdenas A, et al. Acute kidney injury is an early predictor of mortality for patients with alcoholic hepatitis. Clin Gastroenterol Hepatology: Official Clin Pract J Am Gastroenterological Association. 2012;10(1):65–e713.
Mohammadi Kebar S, Hosseini Nia S, Maleki N, Sharghi A, Sheshgelani A. The incidence rate, risk factors and clinical outcome of Acute kidney Injury in critical patients. Iran J Public Health. 2018;47(11):1717–24.
Yuan L, Liao PP, Song HC, Zhou JH, Chu HC, Lyu L. Hyperbilirubinemia induces Pro-apoptotic effects and aggravates renal Ischemia Reperfusion Injury. Nephron. 2019;142(1):40–50.
Rafat C, Burbach M, Brochériou I, Zafrani L, Callard P, Rondeau E, et al. Bilirubin-associated acute tubular necrosis in a kidney transplant recipient. Am J Kidney Diseases: Official J Natl Kidney Foundation. 2013;61(5):782–5.
Medina-González R, Zaragoza JJ, Hernández-Barajas EM, Correa-de Leon J, Claure-Del Granado R, Vazquez-Rangel A, et al. Decrease in platelet count in patients with AKI and its association with major adverse kidney events. Ren Fail. 2024;46(1):2359643.
Kellum JA, Prowle JR. Paradigms of acute kidney injury in the intensive care setting. Nat Rev Nephrol. 2018;14(4):217–30.
Wiedermann CJ, Wiedermann W, Joannidis M. Hypoalbuminemia and acute kidney injury: a meta-analysis of observational clinical studies. Intensive Care Med. 2010;36(10):1657–65.
Miwa T, Utakata Y, Hanai T, Aiba M, Unome S, Imai K et al. Acute kidney injury development is associated with mortality in Japanese patients with cirrhosis: impact of amino acid imbalance. J Gastroenterol. 2024.
Nadim MK, Kellum JA, Forni L, Francoz C, Asrani SK, Ostermann M, et al. Acute kidney injury in patients with cirrhosis: Acute Disease Quality Initiative (ADQI) and International Club of ascites (ICA) joint multidisciplinary consensus meeting. J Hepatol. 2024;81(1):163–83.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Key Research and Development Program of China (No.2022YFC2304501, No.2021YFC2301800), Chinese National Natural Science Foundation (No.81870425), the Fundamental Research Funds for the Central Universities (2021FZZX001-41,226-2023-00127) and Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (No.2022RC141).
Author information
Authors and Affiliations
Contributions
HLT, YS, and JFS conceived and designed the study; HLT, JWS, KG and ZWL collected data; XY and XBX analyzed the data; HLT and JWS wrote the manuscript; and YS and JFS revised the manuscript. All authors have approved the final version of the manuscript, including the authorship list.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tu, H., Su, J., Gong, K. et al. A dynamic model to predict early occurrence of acute kidney injury in ICU hospitalized cirrhotic patients: a MIMIC database analysis. BMC Gastroenterol 24, 290 (2024). https://doi.org/10.1186/s12876-024-03369-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03369-7