Abstract
Purpose
Systemic inflammation and nutrition are vital for tumor progression. This study aimed to identify prognostic inflammation nutrition markers and develop a predictive nomogram for gallbladder cancer (GBC).
Methods
A total of 123 patients with GBC who underwent surgical resection at the First Affiliated Hospital of Soochow University and Suzhou Kowloon Hospital were included in our study. The final prognostic variables were identified using univariate and multivariate analyses. A nomogram model was then established, and the consistency index (C-index), calibration curves, and Kaplan–Meier analysis were performed to evaluate the accuracy and discrimination of the nomogram. The area under the receiver operating characteristic curve (AUC) and decision curve analysis (DCA) suggested that our nomogram had better predictive ability and clinical feasibility than a published model.
Results
The cox regression analysis showed that carcinoembryonic antigen (CEA) > 4.580, albumin-bilirubin (ALBI) > –2.091, geriatric nutritional risk index (GNRI) < 90.83, T3–T4, and N2 are independent prognostic factors. A predictive nomogram was constructed with a C-index of 0.793. In the calibration curves, the nomogram-predicted 1-, 3-, and 5-year survival matched well with the actual survival. Kaplan–Meier analysis showed that the high-risk group had worse survival than the low-risk group (P < 0.001). Finally, our nomogram achieved better 1-, 3- and 5-year AUCs than an established model (0.871, 0.844, and 0.781 vs. 0.753, 0.750, and 0.693). DCA also confirmed that our model outperformed the established model.
Conclusions
In conclusion, our study revealed that CEA > 4.580, GNRI < 90.83, ALBI > –2.091, T3–T4 stage, and N2 were related to clinical outcomes of patients with GBC after surgical resection. The constructed nomogram has superior predictive ability and clinical practicality.
Similar content being viewed by others
Introduction
Gallbladder cancer (GBC) is a rare but highly malignant tumor with a 2.3 per 100,000 incidence rate [10]. The overall survival rate of patients with GBC is typically poor, with less than 10% surviving beyond five years [4]. Hence, developing appropriate parameters or models to enhance treatment optimization and prognosis prediction for patients with GBC is essential.
Previous studies have reported that inflammation is closely associated with cancer development and patient outcomes [2, 6, 25]. The preoperative systemic immune and nutritional status is a critical part of the inflammatory response, which can be reflected by serum inflammatory-nutritional markers, like prognostic nutritional index (PNI), albumin-bilirubin (ALBI), geriatric nutritional risk index (GNRI) and modified Glasgow prognostic score (mGPS). Recent evidence has indicated that immune and nutritional statuses are effective biomarkers for predicting the prognosis of various patients with cancer [16, 18, 30, 42]. For example, in hepatocellular carcinoma (HCC), ALBI can predict the overall survival (OS) of patients after radiofrequency ablation [20] and provide valuable insights for assessing hepatotoxicity risk during SBRT treatment [29]. The nomogram is a graphical tool that can predict the likelihood of clinical events in patients with cancer. It has been found to outperform traditional tumor, node, and metastasis (TNM) staging systems. It may serve as an alternative or a new standard for assessing cancer prognosis across different malignancies. Many GBC-related nomogram prediction models have been developed [26, 39, 41, 49]. However, they mainly focused on some basic characteristics of tumors (tumor size, TNM staging, differentiation, lymph node metastasis, and live infiltration), and none of them considered systemic immune and nutritional status. Therefore, it is necessary to identify independent inflammatory nutritional markers involved in GBC survival and establish a reliable nomogram model to predict GBC OS.
In this study, we retrospectively analyzed the clinicopathological data and inflammatory nutrition markers of 123 patients who underwent surgical resection for GBC at two medical facilities. Using univariate and multivariate analyses, we identified carcinoembryonic antigen (CEA) > 4.580, ALBI > –2.091, GNRI < 90.83, T3–T4, and N2 stage as independent prognostic factors for GBC. We constructed a nomogram to predict OS and evaluated its clinical practicality and accuracy using the consistency index (C-index), calibration curves, and Kaplan–Meier analysis. Using the area under the receiver operating characteristic (ROC) curve (AUC) analysis and decision curve analysis (DCA), we also compared the novel nomogram with another established one, and the results disclosed that our prediction model outperformed the established one.
Methods
Study population
The present study conducted a retrospective analysis of 123 patients diagnosed with GBC who underwent surgical resection at the First Affiliated Hospital of Soochow University and Suzhou Kowloon Hospital. The data collection period spanned from March 2013 to December 2022, and the follow-up deadline was March 2023. Ethical approval for this research was obtained from the ethics committee of the First Affiliated Hospital of Soochow University, and all participants provided informed consent. The process diagram was shown in Fig. 1.
The inclusion criteria were as follows: (1) pathologically diagnosed as GBC; (2) patients underwent surgical resection; (3) complete clinicopathological and blood examinations data one week before surgery; (4) regular follow-up data.
The exclusion criteria were as follows: (1) history of other tumors; (2) concurrent other infectious diseases and systemic diseases like autoimmune diseases, hematological diseases, or inflammatory diseases; (3) underwent neoadjuvant therapy; (4) incidental gallbladder cancer; (5) incomplete clinical data or missed follow-up.
The patients in this study underwent various surgical procedures according to their TNM stage. Surgery 1, cholecystectomy + liver resection + lymph node dissection; surgery 2, extended resection including peripheral organ resection; surgery 3, palliative tumor resection.
Serum inflammatory-nutritional markers
All patients underwent routine blood and blood biochemical tests within one week of surgical resection. The PNI was computed as albumin concentration (g/L) + 5 × lymphocyte count (109/L). The systemic immune-inflammation index (SII) was calculated as platelet × neutrophil/lymphocyte count. Systemic inflammation response index (SIRI) was defined as neutrophil × monocyte/lymphocyte. The ALBI score was computed using the formula –0.085 × albumin (g/L) + 0.66 × log bilirubin (µmol/L). GNRI was defined as 1.487 × albumin concentration (g/L) + 41.7 × preoperative weight/ideal weight (kg). The ideal weight was defined as = 22 × height2 (m). The mGPS was calculated using the following method: mGPS = 2 means albumin concentration (g/L) < 35 (g/L) and blood C-reactive protein (CRP) > 1.0 (mg/dL); mGPS = 1 means albumin concentration (g/L) < 35 (g/L) or blood C-reactive protein (CRP) > 1.0 (mg/dL); mGPS = 0 means albumin concentration (g/L) > 35 (g/L) and blood C-reactive protein (CRP) < 1.0 (mg/dL).
Statistical analysis and nomogram construction
The median [IQR] was used to present quantitative data, while counts and percentages were used for categorical variables. To define the optimal cutoff values for age, body mass index (BMI), carbohydrate antigen 19–9 (CA19-9), carbohydrate antigen 12–5 (CA12-5), CEA, tumor size, and all serum inflammatory markers, we performed ROC analysis using the GraphPad Prism 8 software. Univariate Cox proportional hazards regression was conducted to identify potential prognostic indicators, and covariates at P < 0.05 were selected for further multivariable Cox regression analyses. Likelihood ratio test, Wald test and Score (log-rank) test were performed to evaluate the fitting effect of Cox regression model. Cox proportional hazards regression was used to evaluate potential risk factors of prognosis. The nomogram prediction model was constructed based on variables with P < 0.05, using univariate and multivariable models. Next, we evaluated the nomogram's ability to discriminate and accurately predict outcomes using AUC analysis, C-index calculation, DCA, and the calibration curve. All patients were categorized into high- and low-risk cohorts based on the median cutoff risk score. The method for calculating the risk score is presented in the supplementary materials. The survival disparities between these two groups were assessed using Kaplan–Meier analysis and evaluated using the log-rank test. P < 0.05 was deemed as statistically significant.
Results
Basic characteristics of patients
Following applying our inclusion and exclusion criteria, 123 patients with GBC were successfully enrolled in our study. The median follow-up time for all patients was 22.7 month; 65 patients survived (52.85%), and 58 patients died (47.15%). The clinical features of 123 patients diagnosed with GBC are shown in Table 1. The GBC cohort comprised 53 (43.09%) men and 70 (56.91%) women. The median age of the patients was 66 years; the median BMI was 22.86; 60 (48.78%) had gallbladder stones, and 20 (16.26%) had diabetes. After surgical resection, a pathological examination was performed to determine the histological characteristics of all tumors. The median tumor size was 3.0 cm, and according to the American Joint Committee on Cancer (AJCC) 8th edition, 11 (8.94%) patients were stage I, 32 (26.02%) were stage II, 61 (49.59%) were stage III, and 19 (15.45%) were stage IV. Additionally, 65 (52.85%) patients presented with low differentiated adenocarcinoma, while 43 (34.96%) and 15 (12.19%) patients presented with medium and highly differentiated adenocarcinoma, respectively. The perineural invasion has been reported to contribute to a poor prognosis in patients with GBC [26]. In this population, 35 (28.46%) patients had perineural invasion. A total of 100 patients (81.30%) underwent cholecystectomy + liver resection + lymph node dissection, 17 patients (13.82%) underwent extended resection, including peripheral organ resection, six patients (4.88%) underwent palliative tumor resection, and 115 (93.50%) had an R0 resection margin. The median operation time was 195 min, and the median blood loss was 200 mL.
The best cutoff values of age, BMI, CA199, CA125, CEA, tumor size, SIRI, SII, PNI, ALBI, GNRI, mGPS, blood loss and operation time were 73, 23.28, 51.15, 24.50, 4.58, 3.45, 1.691 × 109, 829.2 × 109, 44.88, –2.091, 90.83, 2, 125 and 118 respectively, and AUCs were 0.514, 0.514, 0.578, 0.606, 0.603, 0.664, 0.631, 0.638, 0.653, 0.661, 0.581, 0.615, 0.591, and 0.505, respectively.
Identification of prognostic factors for OS in patients with GBC
Cox regression analysis was performed to ascertain potential variables linked to GBC development. Table 1 lists the detailed results of univariate and multivariate analyses. Univariate analysis indicated that CA125, CA199, CEA, SIRI, SII, PNI, ALBI, GNRI, mGPS, tumor size, T stage, AJCC stage, grade, lymph node metastasis, perineural invasion, and surgery were potential prognostic factors. Variables that exhibited P < 0.05 were defined as statistically significant. Subsequently, these significant predictors were further enrolled in a multivariate Cox regression analysis. CEA > 4.580, ALBI > –2.091, GNRI < 90.83, T3-T4, and N2 were finally considered independent prognostic factors for GBC patients after surgery, with a P value < 0.05. A forest plot was used to visually display the independent predictors of poor prognosis (supplementary Fig. S1). Likelihood ratio test (p = 2.35 × 109), Wald test (p = 2.68 × 108) and Score (log-rank) test (p = 5.92 × 1014) were performed to comprehensively evaluate the model, and the results indicated that the Cox regression model had a good fitting effect. Further, we performed the Schoenfeld residuals analysis to evaluate whether the proportional hazards assumption was valid. The results showed that the p-values for CEA, ALBI, GNRI, T stage, and lymph node metastasis were 0.4738, 0.5247, 0.9755, 0.3249 and 0.6719 separately and the p-value for global test was 0.6608 (supplementary Fig. S2). These results suggested that CEA, ALBI, GNRI, T stage, and lymph node metastasis were satisfied for the proportional hazards assumption.
Construction and validation of the nomogram prediction model
We then developed a predictive nomogram for estimating 1-, 3-, and 5-year OS in patients with GBC, incorporating the above five independent risk factors: CEA > 4.580, ALBI > –2.091, GNRI < 90.83, T3-T4, and N2 (Fig. 2). After performing internal validation with 1000 bootstrap samples, we obtained the bias-corrected C-index (0.793), demonstrating the nomogram's good predictive power. The calibration curves for the 1-, 3-, and 5-year OS rates also confirmed the high accuracy of the model, as they all matched well with the standard lines (Fig. 3).
Each factor within the nomogram was assigned a certain point according to its risk contribution to the OS of patients with GBC. We calculated the total points of all patients with GBC and separated them into high- or low-risk groups using the optimal cutoff value (65.84). The survival rate of the low-risk group was better than that of the high-risk group, as indicated by Kaplan–Meier analysis (Fig. 4). We also divided all patients into high-, medium-, and low-risk groups based on their nomogram scores. The Kaplan–Meier analysis and survival rate are presented in supplementary Fig. S3 and Table S1.
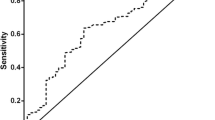
The total points of all patients obtained in our nomogram were compared with those calculated from another reported GBC nomogram [26]. In our prediction model, the 1-, 3-, and 5-year AUC were 0.871, 0.844, and 0.781, respectively (Fig. 5A), which were higher than those of the reported nomogram (0.753, 0.750, and 0.693, respectively) (Fig. 5B). DCA is often utilized to assess the net clinical benefit of prediction models. In our study, the DCA curve showed that the net benefit of our nomogram was better than that of the established model for a risk threshold between 0 and 1, implying that our prediction model outperformed the established model (Fig. 6A–C).
Discussion
GBC has been linked to a significant increase in cancer-related mortality. The accurate prediction of mortality after surgical resection can aid doctors and patients in making clinical choices and predicting survival. Malnutrition is a prevalent and severe issue among patients with cancers, negatively affecting their life quality and survival time [34, 45]. Systemic inflammation, vital for cancer progression, leads to disturbances in hematological elements like white blood cells (monocytes, lymphocytes, and neutrophils) and platelets [7]. Although previous studies have constructed nomograms to predict OS in different populations of patients with GBC, no study has integrated inflammatory-nutritional markers with clinical characteristics into a predictive nomogram.
In this study, we developed and verified a nomogram model for predicting OS in patients with GBC who underwent surgical resection by combining inflammatory-nutritional markers and clinical parameters. Our results showed that CEA, GNRI, ALBI, T3–T4, and N2 are independent prognostic factors for GBC. We further constructed a nomogram, for which the C-index and calibration curves suggested good predictive power and clinical utility. Kaplan–Meier analysis revealed that patients in the high-risk group had significantly worse OS than those in the low-risk group. Furthermore, compared with the established model, our prediction model had a higher AUC value (sensitivity and specificity) and a better DCA curve.
Patients with cancer, including GBC, are prone to malnutrition. Our study found two nutrition-related indicators, ALBI and GNRI, which can function as reliable prognostic biomarkers for patients with GBC. The ALBI score, calculated based on serum albumin and bilirubin levels, was originally developed to evaluate liver function and OS in individuals diagnosed with HCC [17]. Recent investigations have shown that ALBI is a promising predictor of postoperative liver failure and mortality in HCC patients after hepatic resection [11, 17]. Since the original reports, there has been evidence of a strong relationship between ALBI and mortality in many non-hepatic tumors, including pancreatic cancer [40], colon cancer [19], intrahepatic and extrahepatic bile duct cancer [37, 38], and even brain cancer [46, 48]. However, no reports have suggested the prognostic value of ALBI in patients with GBC undergoing surgical resection. The link between the ALBI score and patient survival across these cancers can be partially explained by impaired nutritional status [13]. Albumin production in the liver is responsible for maintaining optimal nutritional status, and a reduction in serum albumin levels may indicate impaired nutritional status or liver dysfunction. An impaired nutritional status has been reported to enhance cancer progression by reducing macrophage activation and suppressing antitumor immunity [36]. Albumin also acts as a negative acute phase reactant and its levels can be influenced by cancer-related inflammation. In conditions such as malnutrition and cachexia, cytokines affect its blood concentration, making albumin a marker for inflammatory and immune states as well as nutritional status [9]. Bilirubin, a product of heme metabolism, play an important role in the antioxidant activity, intestinal homeostasis and host defense. Therefore, it also involves in shaping the intestinal microbiota. Changes in the intestinal microbiota significantly affect carcinogenesis, development and prognosis of various cancers, including GBC [14, 22, 24]. Additionally, bilirubin levels in the blood can be indicative of tumor progression invading the bile ducts. Overall, ALBI > –2.091 indicates worse liver function and inflammatory-nutritional status. These characteristics suggest that the ALBI score has the potential to be a significant biomarker for forecasting GBC advancement.
The GNRI was first established to prognosticate the morbidity and mortality of hospitalized elderly patients [3]. Since then, the index has been developed for its applicability to various diseases, including cancers [12, 27, 33]. However, no studies have indicated the relationship between GNRI and clinical outcomes in patients with GBC. The high predictive value of the GNRI is attributable to integrating two readily available and critical indicators of malnutrition: body weight and serum albumin. A low BMI has been widely accepted as an indicative factor for cancer progression and unfavorable prognosis [5]. Calculating the GNRI while considering the current body weight to the ideal body weight ratio adds the BMI component to the index, which may provide a more objective reflection of weight changes in cancer patients due to tumor consumption.
In our study, we demonstrated that ALBI > –2.091 (HR, 3.301; 95% CI: 1.049–10.381; p = 0.041) and GNRI < 90.83 (HR, 2.461; 95% CI: 1.026–5.903; p = 0.044) were poor independent prognostic factors for 123 patients with GBC after surgical resection. For the GNRI to be routinely used by clinicians, setting a definite cutoff to stratify patients into low and high GNRI groups is necessary. Although the majority of included studies and literature have reached a consensus on setting 98 as the cutoff point, this value is not sacrosanct, and various alternative thresholds have also been employed based on receiver operating curve analysis of specific cohort data [27, 43]. Nevertheless, a well-defined GNRI cutoff should be explored further. Multiple meta-analyses have demonstrated that a decreased GNRI is associated with poorer overall survival, with an HR range of 1.75 to 1.96, indicating that a low GNRI typically corresponds to a two-fold increase in mortality rate across various types of cancer [23, 35, 47]. Contrarily, our findings revealed an approximate 2.5-fold rise in mortality rate among patients with GBC exhibiting a low GNRI. This suggests that GNRI, when used as a prognostic indicator for GBC, is more effective than its application in other malignancies. In our study, GNRI < 90.83 indicates relatively malnutrition of GBC patients, which can lead to a weakened immune system, reduced tolerance to treatments, and overall poorer prognosis. The association of low GNRI with worse outcomes in GBC patients underscores the critical role of maintaining adequate nutrition and body weight in managing cancer patients.
Except for ALBI and GNRI, another three commonly used GBC prognostic indicators, namely CEA (HR, 2.253; 95% CI: 1.133–4.479; p = 0.021), T3–T4 stage (HR, 3.487; 95% CI: 1.039–11.704; p = 0.043) and N2 (HR, 2.843; 95% CI: 1.018–7.942; p = 0.046), were also included in our novel nomogram. CEA is a widely-used, non-specific cancer biomarker valuable for early detection of malignancies [31]. It plays a crucial role in evaluating treatment effectiveness and monitoring for tumor recurrence and metastasis. Elevated levels of CEA are often associated with various cancers, including GBC [8, 28]. In this study, CEA > 4.580 correlates with poorer survival outcomes of GBC patients. This suggests that patients with higher preoperative CEA levels may have more aggressive or advanced disease, warranting closer monitoring and potentially more aggressive treatment. The T stage of GBC describes its size and extent of invasion into surrounding tissues, while the N stage describes the extent of regional lymph node involvement. T3–T4 stages indicate advanced local disease, with the tumor invading beyond the gallbladder into the liver or other nearby organs, and N2 stage indicates more than four regional lymph node metastasis. As a result, they are naturally associated with a worse prognosis due to the increased difficulty of achieving complete surgical resection and the higher likelihood of metastasis. The presence of T3–T4 stages or N2 stage often necessitates more extensive surgical procedures and may limit the effectiveness of local treatments [1, 15, 21]. Although the TNM staging system is the most widely used system for GBC prognostics and treatment planning, its focus on the anatomical features of tumors suggests that it might not fully encompass other factors that impact survival. Adding CEA and two nutrition-related indicators to GBC risk stratification beyond the TNM staging system makes our nomogram more comprehensive. Previous studies have reported that elevated CEA levels are significantly associated with metastasis and poor survival in patients undergoing surgical resection [32, 44, 49]. The optimal cutoff value of CEA derived from other studies was 5.000 IU/mL [32, 49], similar to that in our study (4.580 IU/mL).
Our study has some limitations. Initially, we collected retrospective data without any prospective elements, which may pose challenges if similar factors are included in the multivariable analyses. The study was conducted using data from two institutions and had a relatively small sample size. Future validation studies should include more independent cohorts from other centers. Additionally, it is worth mentioning that the focus of this study was on mortality, and due to various factors, there was no follow-up regarding the time until recurrence. This study did not provide information on tumor-free or tumor-specific survival.
Conclusions
In conclusion, our study revealed that CEA > 4.580, GNRI < 90.83, ALBI > –2.091, T3-T4 stage, and N2 were related to clinical outcomes of patients with GBC after surgical resection. Based on these factors, a novel nomogram was developed to predict the prognosis of patients with GBC, which could help develop a rational and individualized treatment strategy.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GBC:
-
Gallbladder cancer
- C-index:
-
The consistency index
- AUC:
-
The area under the receiver operating characteristic curve
- DCA:
-
Decision curve analysis
- CEA:
-
Carcinoembryonic antigen
- ALBI:
-
Albumin-bilirubin
- GNRI:
-
Geriatric nutritional risk index
- PNI:
-
Prognostic nutritional index
- GNRI:
-
Geriatric nutritional risk index
- mGPS:
-
Modified Glasgow prognostic score
- HCC:
-
Hepatocellular carcinoma
- OS:
-
Overall survival
- ROC:
-
The receiver operating characteristic
- SII:
-
The systemic immune-inflammation index
- SIRI:
-
Systemic inflammation response index
- CRP:
-
C-reactive protein
- BMI:
-
Body mass index
- CA19-9:
-
Carbohydrate antigen 19–9
- CA12-5:
-
Carbohydrate antigen 12–5
- AJCC:
-
The American Joint Committee on Cancer
References
Amini N, Spolverato G, Kim Y, Gupta R, Margonis GA, Ejaz A, Pawlik TM. Lymph node status after resection for gallbladder adenocarcinoma: prognostic implications of different nodal staging/scoring systems. J Surg Oncol. 2015;111(3):299–305. https://doi.org/10.1002/jso.23813.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–45. https://doi.org/10.1016/S0140-6736(00)04046-0.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L, Aussel C. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–83. https://doi.org/10.1093/ajcn/82.4.777.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Caan BJ, Meyerhardt JA, Kroenke CH, Alexeeff S, Xiao J, Weltzien E, Feliciano EC, Castillo AL, Quesenberry CP, Kwan ML, Prado CM. Explaining the obesity paradox: the association between body composition and colorectal cancer survival (C-SCANS Study). Cancer Epidemiol Biomarkers Prev. 2017;26(7):1008–15. https://doi.org/10.1158/1055-9965.EPI-17-0200.
Castillo-Martinez L, Castro-Eguiluz D, Copca-Mendoza ET, Perez-Camargo DA, Reyes-Torres CA, Avila EA, Lopez-Cordova G, Fuentes-Hernandez MR, Cetina-Perez L, Milke-Garcia MDP. Nutritional assessment tools for the identification of malnutrition and nutritional risk associated with cancer treatment. Rev Invest Clin. 2018;70(3):121–5. https://doi.org/10.24875/RIC.18002524.
Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13(11):759–71. https://doi.org/10.1038/nrc3611.
Fletcher RH. Carcinoembryonic antigen. Ann Intern Med. 1986;104(1):66–73. https://doi.org/10.7326/0003-4819-104-1-66.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69. https://doi.org/10.1186/1475-2891-9-69.
Henley SJ, Weir HK, Jim MA, Watson M, Richardson LC. Gallbladder Cancer Incidence and Mortality, United States 1999–2011. Cancer Epidemiol Biomarkers Prev. 2015;24(9):1319–26. https://doi.org/10.1158/1055-9965.EPI-15-0199.
Ho SY, Liu PH, Hsu CY, Hsia CY, Su CW, Lee YH, Huang YH, Lee FY, Hou MC, Huo TI. Comparison of twelve liver functional reserve models for outcome prediction in patients with hepatocellular carcinoma undergoing surgical resection. Sci Rep. 2018;8(1):4773. https://doi.org/10.1038/s41598-018-22923-4.
Iguchi T, Sugimachi K, Mano Y, Motomura T, Sugiyama M, Ota M, Ikebe M, Esaki T, Yoshizumi T, Morita M, Mori M, Toh Y. Prognostic impact of geriatric nutritional risk index in patients with synchronous colorectal liver metastasis. Anticancer Res. 2020;40(7):4165–71. https://doi.org/10.21873/anticanres.14416.
Imamura T, Okamura Y, Sugiura T, Ito T, Yamamoto Y, Ashida R, Ohgi K, Otsuka S, Uesaka K. Clinical significance of preoperative albumin-bilirubin grade in pancreatic cancer. Ann Surg Oncol. 2021;28(11):6223–35. https://doi.org/10.1245/s10434-021-09593-9.
Inoguchi T, Nohara Y, Nojiri C, Nakashima N. Association of serum bilirubin levels with risk of cancer development and total death. Sci Rep. 2021;11(1):13224. https://doi.org/10.1038/s41598-021-92442-2.
Ito H, Ito K, D’Angelica M, Gonen M, Klimstra D, Allen P, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. Accurate staging for gallbladder cancer: implications for surgical therapy and pathological assessment. Ann Surg. 2011;254(2):320–5. https://doi.org/10.1097/SLA.0b013e31822238d8.
Jiang YT, Wang TC, Zhang W. Preoperative systemic immune-inflammation index is a potential biomarker in adult patients with high-grade gliomas undergoing radical resection. J Inflamm Res. 2023;16:3479–90. https://doi.org/10.2147/JIR.S423488.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O’Beirne J, Fox R, Skowronska A, Palmer D, Yeo W, Mo F, Lai P, Inarrairaegui M, Chan SL, Sangro B, Miksad R, Tada T, Kumada T, Toyoda H. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–8. https://doi.org/10.1200/JCO.2014.57.9151.
Kang X, Wang J, Kang X, Bai L. Predictive value of prognostic nutritional index (PNI) in recurrent or unresectable hepatocellular carcinoma received anti-PD1 therapy. BMC Cancer. 2023;23(1):787. https://doi.org/10.1186/s12885-023-11166-w.
Koh HH, Cho ES, Lee JH, Shin SJ, Lee HS, Park EJ, Baik SH, Lee KY, Kang J. Association of albumin-bilirubin grade and myosteatosis with its prognostic significance for patients with colorectal cancer. Ann Surg Oncol. 2022;29(6):3868–76. https://doi.org/10.1245/s10434-022-11445-z.
Kuo YH, Huang TH, Yen YH, Lu SN, Wang JH, Hung CH, Chen CH, Tsai MC, Kee KM. Nomogram to predict the long-term overall survival of early-stage hepatocellular carcinoma after radiofrequency ablation. Cancers (Basel) 2023;15(12) https://doi.org/10.3390/cancers15123156.
Lee AJ, Chiang YJ, Lee JE, Conrad C, Chun YS, Aloia TA, Vauthey JN, Tzeng CD. Validation of American Joint Committee on Cancer eighth staging system for gallbladder cancer and its lymphadenectomy guidelines. J Surg Res. 2018;230:148–54. https://doi.org/10.1016/j.jss.2018.04.067.
Lee HG, Lim SB, Lee JL, Kim CW, Yoon YS, Park IJ, Kim JC. Preoperative albumin-bilirubin score as a prognostic indicator in patients with stage III colon cancer. Sci Rep. 2022;12(1):14910. https://doi.org/10.1038/s41598-022-19329-8.
Li L, He J. Prognostic role of geriatric nutritional risk index in patients with pancreatic cancer: a meta-analysis. Nutr Cancer. 2023;75(7):1531–40. https://doi.org/10.1080/01635581.2023.2209345.
Liu S, Li W, Chen J, Li M, Geng Y, Liu Y, Wu W. The footprint of gut microbiota in gallbladder cancer: a mechanistic review. Front Cell Infect Microbiol. 2024;14:1374238. https://doi.org/10.3389/fcimb.2024.1374238.
Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006;4(4):221–33. https://doi.org/10.1158/1541-7786.MCR-05-0261.
Ma Z, Dong F, Li Z, Zheng Z, Zhou Z, Zhuang H, Liu C, Huang B, Huang S, Zou Y, Yang L, Gong Y, Zhang C, Hou B. A novel prognostic nomogram for gallbladder cancer after surgical resection: a single-center experience. J Oncol. 2021;2021:6619149. https://doi.org/10.1155/2021/6619149.
Matsuura S, Morikawa K, Ito Y, Kubota T, Ichijo K, Mochizuki E, Akiyama N, Uehara M, Harada M, Tsukui M, Koshimizu N. The geriatric nutritional risk index and prognostic nutritional index predict the overall survival of advanced non-small cell lung cancer patients. Nutr Cancer. 2022;74(5):1606–13. https://doi.org/10.1080/01635581.2021.1960387.
Ono T, Komatsu M, Hoshino T, Ishii T, Fujii T, Oshima S, Mikami K, Umeki Y, Enomoto K, Masamune O. Alpha-fetoprotein, carcinoembryonic antigen, and carbohydrate antigen 19–9-producing gallbladder cancer. J Gastroenterol. 1996;31(5):742–6. https://doi.org/10.1007/BF02347628.
Prehn LM, Kojima A. Paradoxical effect of three-day thymectomy on sarcogenesis in the mouse with different dosages of methylcholanthrene. Cancer Res. 1986;46(10):4971–2.
Qiu J, Yang J, Yu Y, Wang Z, Lin H, Ke D, Zheng H, Li J, Yao Q. Prognostic value of pre-therapeutic nutritional risk factors in elderly patients with locally advanced esophageal squamous cell carcinoma receiving definitive chemoradiotherapy or radiotherapy. BMC Cancer. 2023;23(1):597. https://doi.org/10.1186/s12885-023-11044-5.
Rizeq B, Zakaria Z, Ouhtit A. Towards understanding the mechanisms of actions of carcinoembryonic antigen-related cell adhesion molecule 6 in cancer progression. Cancer Sci. 2018;109(1):33–42. https://doi.org/10.1111/cas.13437.
Sachan A, Saluja SS, Nekarakanti PK, Nimisha B, Mahajan HH, Nag and P. K. Mishra,. Raised CA19-9 and CEA have prognostic relevance in gallbladder carcinoma. BMC Cancer. 2020;20(1):826. https://doi.org/10.1186/s12885-020-07334-x.
Sakamoto T, Yagyu T, Uchinaka E, Miyatani K, Hanaki T, Kihara K, Matsunaga T, Yamamoto M, Tokuyasu N, Honjo S, Fujiwara Y. The prognostic significance of combined geriatric nutritional risk index and psoas muscle volume in older patients with pancreatic cancer. BMC Cancer. 2021;21(1):342. https://doi.org/10.1186/s12885-021-08094-y.
Schwegler I, von Holzen A, Gutzwiller JP, Schlumpf R, Muhlebach S, Stanga Z. Nutritional risk is a clinical predictor of postoperative mortality and morbidity in surgery for colorectal cancer. Br J Surg. 2010;97(1):92–7. https://doi.org/10.1002/bjs.6805.
Shen F, Ma Y, Guo W, Li F. Prognostic Value of Geriatric Nutritional Risk Index for Patients with Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Lung. 2022;200(5):661–9. https://doi.org/10.1007/s00408-022-00567-6.
Thurnham DI. Interactions between nutrition and immune function: using inflammation biomarkers to interpret micronutrient status. Proc Nutr Soc. 2014;73(1):1–8. https://doi.org/10.1017/S0029665113003662.
Tsilimigras DI, Hyer JM, Moris D, Sahara K, Bagante F, Guglielmi A, Aldrighetti L, Alexandrescu S, Marques HP, Shen F, Koerkamp BG, Endo I, Pawlik TM, G. other members of the International Intrahepatic Cholangiocarcinoma Study. Prognostic utility of albumin-bilirubin grade for short- and long-term outcomes following hepatic resection for intrahepatic cholangiocarcinoma: A multi-institutional analysis of 706 patients. J Surg Oncol. 2019;120(2):206–13. https://doi.org/10.1002/jso.25486.
Wang Y, Pang Q, Jin H, Zhou L, Hu X, Qian Z, Man Z, Yang S, Liu H. Albumin-bilirubin grade as a novel predictor of survival in advanced extrahepatic cholangiocarcinoma. Gastroenterol Res Pract. 2018;2018:8902146. https://doi.org/10.1155/2018/8902146.
Xie ZH, Shi X, Liu MQ, Wang J, Yu Y, Zhang JX, Chu KJ, Li W, Ge RL, Cheng QB, Jiang XQ. Development and validation of a nomogram to predict overall survival in patients with incidental gallbladder cancer: A retrospective cohort study. Front Oncol. 2022;12:1007374. https://doi.org/10.3389/fonc.2022.1007374.
Yagyu T, Saito H, Sakamoto T, Uchinaka EI, Morimoto M, Amisaki M, Watanabe J, Tokuyasu N, Honjo S, Ashida K, Fujiwara Y. Preoperative albumin-bilirubin grade as a useful prognostic indicator in patients with pancreatic cancer. Anticancer Res. 2019;39(3):1441–6. https://doi.org/10.21873/anticanres.13260.
Yin Z, Chen T, Shu Y, Li Q, Yuan Z, Zhang Y, Xu X, Liu Y. A gallbladder cancer survival prediction model based on multimodal fusion analysis. Dig Dis Sci. 2023;68(5):1762–76. https://doi.org/10.1007/s10620-022-07782-4.
Ying HQ, Deng QW, He BS, Pan YQ, Wang F, Sun HL, Chen J, Liu X, Wang SK. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol. 2014;31(12):305. https://doi.org/10.1007/s12032-014-0305-0.
Yu J, Zhang W, Wang C, Hu Y. The prognostic value of pretreatment geriatric nutritional risk index in esophageal cancer: a meta-analysis. Nutr Cancer. 2022;74(9):3202–10. https://doi.org/10.1080/01635581.2022.2069273.
Yu T, Yu H, Cai X. Preoperative prediction of survival in resectable gallbladder cancer by a combined utilization of CA 19–9 and carcinoembryonic antigen. Chin Med J (Engl). 2014;127(12):2299–303.
Yugawa K, Itoh S, Kurihara T, Yoshiya S, Mano Y, Takeishi K, Harada N, Ikegami T, Soejima Y, Mori M, Yoshizumi T. Skeletal muscle mass predicts the prognosis of patients with intrahepatic cholangiocarcinoma. Am J Surg. 2019;218(5):952–8. https://doi.org/10.1016/j.amjsurg.2019.03.010.
Zhang J, Xu Q, Zhang H, Zhang Y, Yang Y, Luo H, Lin X, He X, Mou Y, Zhou Z, He Z. High preoperative albumin-bilirubin score predicts poor survival in patients with newly diagnosed high-grade gliomas. Transl Oncol. 2021;14(4):101038. https://doi.org/10.1016/j.tranon.2021.101038.
Zhou J, Fang P, Li X, Luan S, Xiao X, Gu Y, Shang Q, Zhang H, Yang Y, Zeng X, Yuan Y. Prognostic value of geriatric nutritional risk index in esophageal carcinoma: a systematic review and meta-analysis. Front Nutr. 2022;9:831283. https://doi.org/10.3389/fnut.2022.831283.
Zhu S, Cheng Z, Hu Y, Chen Z, Zhang J, Ke C, Yang Q, Lin F, Chen Y, Wang J. Prognostic value of the systemic immune-inflammation index and prognostic nutritional index in patients with medulloblastoma undergoing surgical resection. Front Nutr. 2021;8:754958. https://doi.org/10.3389/fnut.2021.754958.
Zhu Z, Luo K, Zhang B, Wang G, Guo K, Huang P, Liu Q. Risk factor analysis and construction of prediction models of gallbladder carcinoma in patients with gallstones. Front Oncol. 2023;13:1037194. https://doi.org/10.3389/fonc.2023.1037194.
Acknowledgements
No.
Funding
This study was supported by grants from the National Nature Science Foundation of China (No.82203735).
Author information
Authors and Affiliations
Contributions
Xueqing Yin, Danyang Shen and Zuxiong Tang designed the work and wrote the manuscript. Xueqing Yin, Xinren Ma and Pu Sun collected the GBC patients clinical data, and completed the follow-up examinations of GBC patients after surgery. Xueqing Yin and Danyang Shen analyzed the data. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study is in accordance with the Declaration of Helsinki and has been approved by the ethical committee of the First Affiliated Hospital of Soochow University and Suzhou Kowloon Hospital. All research procedures were in compliance with the relevant guideline and regulations. Informed consent was obtained from all patients prior to being included.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yin, X., Ma, X., Sun, P. et al. A novel nomogram based on inflammatory-nutritional biomarkers for gallbladder cancer after surgical resection. BMC Gastroenterol 24, 289 (2024). https://doi.org/10.1186/s12876-024-03374-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03374-w