Abstract
Background
Adverse effects of rigorously lowering low-density lipoprotein cholesterol on cognition have been reported; therefore, we aimed to study the contribution of serum cholesterol in cognitive decline in older people with or without dementia.
Methods
Cognitive function was assessed by the Cognitive Abilities Screening Instrument (CASI). We investigated associations between serum cholesterol with cognitive decline using multiple regressions controlling for the effects of demographics, vascular risk factors, and treatments.
Results
Most associations between cholesterol and CASI scores could be explained by non-linear and inverted U-shaped relationships (R2 = 0.003–0.006, p < 0.016, Šidákcorrection). The relationships were most evident between changes in cholesterol and CASI scores in older people at the preclinical or prodromal stages of dementia (R2 = 0.02–0.064, p values < 0.016). There were no differences in level of changes in CASI scores between individuals in 1st decile and 10th decile groups of changes in cholesterol (p = 0.266–0.972). However, individuals in the 1st decile of triglyceride changes and with stable and normal cognitive functions showed significant improvement in CASI scores compared to those in the 10th decile (t(202) = 2.275, p values < 0.05).
Conclusion
These findings could implicate that rigorously lowering cholesterol may not be suitable for the prevention of cognitive decline among older people, especially among individuals in preclinical or prodromal stages of dementia.
Similar content being viewed by others
Introduction
Previous studies have suggested that midlife elevated serum total cholesterol (TC) may be associated with cognitive decline [1,2,3,4,5]. Previous studies revealed associations between high midlife TC and an increased risk of Alzheimer’s dementia (AD) or all-cause dementia [6]. However, there was no evidence supporting an association between all-cause dementia including AD and late-life TC [6,7,8].
Recent guidelines have suggested a rigorous management of cholesterol, especially low-density lipoprotein cholesterol (LDL-c), among people with cerebrovascular disease (CVD) risks [9,10,11]. However, there is no consensus on whether the rigorous management has protective effects on cognitive function [10,11,12,13]. In addition, optimal levels of TC, triglycerides (TG), and high-density lipoprotein (HDL) remain to be determined. Several recent studies have reported that relationship between circulating cholesterol and cognitive function may conform to an inverted U-shaped function [1, 14, 15].
Researchers have recently addressed importance of brain health in relationship between CVD risk and cognitive decline [16, 17], such that effects of serum cholesterol on cognitive function might be different in the course of dementia [5]. According to demyelination hypothesis of AD, reduction in integrity of axons in the brain may be an early sign of AD [18, 19]. Cholesterol is a major component of axons and cholesterol level has been reported to be associated with normal functioning and repairment of axons [20, 21]. In addition, recent studies have revealed the role of cholesterol in preventing the migration of tauopathies in the brain [22,23,24,25]. Thus, cholesterol might play a more important role in early stages of dementia as compared to its role in later stages. To the best of our knowledge, no studies have investigated the role of cognitive states among older people in relationship between serum cholesterol and cognitive function.
In this study, we longitudinally investigated individuals with subjective and/or objective cognitive decline as well as patients with dementia. We analyzed association between serum cholesterol and cognitive function at baseline and at approximately 2.5 years after the first examination. We hypothesized that (1) relationship between cholesterol and cognitive function was non-linear and inverted U-shaped, (2) drastic changes in serum cholesterol were associated with cognitive decline, and (3) relationship between serum cholesterol and cognitive function was different across individuals with different cognitive states.
Methods
Participants
The participants were selected from a dataset built for the “History-Based Artificial Intelligent Clinical Dementia Diagnostic System (HAICDDS) Project” [26]. HAICDDS aims to have participants longitudinally receive regular serum laboratory examinations and cognitive assessments at each time of evaluation at the Neurology outpatient clinics across Taiwan to facilitate early management of dementia. Individuals with no difficulties in understanding the instructions of cognitive assessment and blood sampling were included in the dataset. Currently, 10,526 participants have been included. Among them, 3,703 have been assessed at least twice. Data from 2,134 participants with at least two assessments in serum total cholesterol and cognitive function and aged over 50 years were extracted and analyzed in this study after excluding individuals aged under 50 years or with missing data in terms of demographics, serum total cholesterol levels, cerebrovascular diseases (CVD) and their risk factors, and drug treatment for the CVD (Fig. 1). The samples exclude from this study were younger (72.4 ± 13.7 years), more educated (6.5 ± 5.7 years), and more prone to be male (47%) as compared to the samples included in the analysis. In addition, they had higher cognitive (score on the Cognitive Abilities Screening Instrument [CASI]: 59.6 ± 30.3, maximum score = 100) and daily (score on the History-based Artificial Intelligent ADL questionnaire [HAI-ADL]: 9.9 ± 10.2, maximum score = 43) functions, lower levels of frailty (score on the Clinical Frailty Scale: 3.2 ± 2.7, maximum score = 7), and lower levels of vascular risks (hypertension: 44.6%; diabetes mellitus: 27.4%; coronary artery disease: 4.7%; arrhythmia: 6.6%) (absolute values of t = 3.73–14.71, df = 10,524; \({\chi }_{n=\text{10,526}, df=1}^{2}\) = 23.91–1189.00; all p values < 0.001). No difference in levels psychiatric symptoms (p = 0.38) was observed between individuals included in or excluded from the analysis. Data concerning HDL-c and LDL-c were available among 1,571 (73.6%) and 2,130 (99.9%) individuals, respectively, due to staff error. Neuroimaging studies were used to exclude marked etiologies other than degenerative or cerebrovascular. Participants who did not complete the assessment of cognitive functions were excluded. Data were analyzed retrospectively and anonymously. The study was approved by Committee for Medical Research Ethics of Show Chwan Memorial Hospital and the need for informed consent was waived (SCMH_IRB No: IRB1081006).
Cognitive assessment
Global cognitive function among participants was assessed by clinical neuropsychologists using Cognitive Assessment Screening Instrument (CASI) [27]. CASI is a widely used tool assessing cognitive function with tasks evaluating memory, orientation, attention and concentration, language abilities, abstract thinking and judgment, and visuospatial abilities. Activities of daily living (ADL) of participants were assessed using History-based Artificial Intelligent ADL questionnaire (HAI-ADL) [28]. For diagnosing subjective cognitive decline (SCD), the individual should have a global Clinical Dementia Rating (CDR) score of 0 or 0.5 and perform normally on CASI with normal score HAI-ADL (< 8.5) [28]. Mild cognitive impairment (MCI) was diagnosed according to criteria proposed by previous studies [29], and an operational determination of MCI was made if the individual displayed a performance on CASI that was below cutoff score adjusted for age and educational level, a performance on HAI-ADL that was within normal range, and a CDR score was 0.5 with a CDR-sum of boxes < 4.5 [30,31,32]. Dementia was diagnosed according to NIA-AA criteria [33], and an operational determination of impaired cognitive function or ADL was made if the individual displayed performances below cutoffs of CASI and HAI-ADL with a CDR score of \(\ge\) 0.5.
Participants with subjective or MCI (SMCI) at baseline assessment were further classified as following: (1) Individuals with incident dementia: Having SMCI at baseline assessment, displaying deterioration in ADL at follow-up assessment (i.e., from CDR = 0 or 0.5 to higher than or equal to 1), and without ‘reverse’ in cognitive function (i.e., from below the cutoff score to above or equal to the cutoff score) or ADL at any follow-up assessment (SMCI-D); or (2) Individuals without incident dementia (SMCI-stable, SMCI-S): Having SMCI at baseline assessment and without deterioration in ADL at follow-up assessment. Similarly, patients with dementia at baseline assessment were classified as following: (1) Patients with a functional deterioration (Dementia-D): Having prevalent dementia at baseline assessment and displaying a deterioration in ADL at follow-up assessment (i.e., from CDR = 1 to higher than or equal to 2); or (2) Patients without functional deterioration (Dementia-S): Having prevalent dementia at baseline assessment without a deterioration in ADL at follow-up assessment.
Serum cholesterol
Serum TC and TG were directly measured using enzymatic methods. HDL-c was measured by the Roche HDL-c 3rd generation direct method. LDL-c was calculated by formula of Friedewald: LDL-c = TC – HDL-c – TG/5.0 (mg/dL) [34]. For individuals with TG \(\ge\) 400 mg/dL, a revised Friedwald formula was used to better estimate LDL-c: LDL-c = TC – HDL-c – TG/8.0 (mg/dL) [35]. History of hypertension, diabetes mellitus, coronary artery disease, arrhythmia, and hypercholesterolemia as well as whether the patients were taking anti-hypertensives, anti-diabetics, and statins were collected through a structural interview or a review of medical charts.
Statistical analysis
Statistical analyses were accomplished using SPSS 22.0 (IBM Corp., Armonk, NY) and R [36]. Longitudinal changes in serum TC, TG, HDL-c, and LDL-c levels as well as CASI scores were calculated as average in the difference in each pair of proximate follow-up examinations.
We established three models using multiple regressions that controlled for covariates (i.e., age, educational levels, sex, follow-up duration, hypertension, diabetes mellitus, coronary artery disease, cerebrovascular disease, arrhythmia, hypercholesterolemia, taking anti-hypertensive, taking anti-diabetics, taking anti-coagulants, taking statins, and frailty [37]) to investigate relationship between baseline cholesterol levels and CASI score (model 1), between baseline cholesterol levels and longitudinal changes in CASI score (model 2), and between longitudinal changes in cholesterol levels and in CASI score (model 3). Goodness of fit among functions describing relationships between cholesterol levels and CASI score was assessed by calculating R-squared values. There is currently no definite threshold for R-squared values in the evaluation of models; however, it is a method to evaluate the significance of explanatory variables on the dependent variable [38]. We also compared the non-linear functions and linear functions in explaining the relationship between serum cholesterol and cognitive functions by comparing the generalized additive models introducing the restricted cubic spline terms (knots = 3) for serum cholesterol levels or not using splines function package of R. The significance of the regression models was evaluated using F-tests. We categorized longitudinal changes in TC, TG, HDL-c, and LDL-c into deciles and compared changes in CASI scores between individuals in first and tenth deciles (TC: 1st decile: over 35 mg/dL decrease, 10th decile: over 24 mg/dL increase; TG: 1st decile: over 47 mg/dL decrease, 10th decile: over 39.50 mg/dL increase; HDL-c: 1st decile: over 9 mg/dL decrease, 10th decile: over 10.00 mg/dL increase; LDL-c: 1st decile: over 30 mg/dL decrease, 10th decile: over 22.50 mg/dL increase) in order to assess effects of extreme increases and decreases in these parameters on cognitive function. Demographic and clinical characteristics were compared across subgroups (i.e., SMCI-S, SMCI-D, Dementia-S, Dementia-D) using one-way ANOVAs or chi-square tests. Multiple regression models were applied and compared across the subgroups. In sensitivity analysis, we repeated main analyses after excluding 357 individuals with SCD. The \(\alpha\) levels were set as 0.016 according to Šidák correction for multiple comparisons. We did not correct the \(\alpha\) levels for prediction using each variable in this study due to the explorative nature of the study [39, 40].
Results
Participants
Demographics and clinical characteristics of participants are presented in Table 1. Changes in cholesterol levels of participants are presented in Supplementary Table 1.
Association of serum cholesterol and cognitive function
Baseline serum TC levels were linearly associated with maintenance or increase in CASI scores after controlling for covariates (b = 0.025, 95% confidence interval [CI] = 0.008–0.092, standard error [SE] = 0.01, t = 3.376, p < 0.01). Other linear relationships between serum cholesterol and CASI score were not significant (p = 0.162–0.994) (supplementary Table 2). Non-linear and quadratic inverted U-shaped functions could be used to describe the relationships between cholesterol parameters and cognitive function in all models (baseline: TC: baseline CASI, R2 = 0.003, | residuals | [1st quartile to 3rd quartile] = 10.12–29.01, F = 3.801, p < 0.016; change in CASI, R2 = 0.011, | residuals | = 11.90–30.24, F = 13.025, p < 0.001; HDL-c: baseline CASI, R2 = 0.008, | residuals | = 11.68–20.12, F = 6.342, p < 0.01; LDL-c: baseline CASI, R2 = 0.003, | residuals | = 13.14–20.26, F = 3.910, p < 0.050.016; change in CASI, R2 = 0.008, | residuals | = 11.23–17.10, F = 8.882, p < 0.001; longitudinal: TC: R2 = 0.003, | residuals | = 14.42–23.37, F = 3.923, p < 0.01 (Figs. 2 and 3), with the exceptions of relationship between HDL-c and changes in CASI (baseline: R2 = 0.005, | residuals | = 10.98–26.25, F = 3.331, p = 0.042; longitudinal: R2 = 0.006, | residuals | = 14.42–23.37, F = 4.460, p = 0.026) (supplementary Fig. 1), between TG and cognitive function (baseline: baseline CASI, R2 = 0.001, | residuals | = 10.32–30.11, F = 0.946, p = 0.381; change in CASI, R2 = 0.002, | residuals | = 10.63–21.49, F = 1.720, p = 0.198; longitudinal: R2 = 0.006, | residuals | = 8.26–19.19, F = 2.533, p = 0.102) (supplementary Fig. 2), and between changes in LDL-c and changes in CASI (R2 = 0.002, | residuals | = 15.32–22.38, F = 2.212, p = 0.146). The associations become insignificant after removing the cubic terms of serum cholesterol parameters in the models (p = 0.32–0.89), with the exceptions of the associations of baseline TC level and maintenance or increase of CASI scores and of baseline HDL-c and LDL-c and baseline CASI scores.
Relationship between serum TC levels and CASI scores. The upper panel denotes the relationship between baseline cholesterol levels and baseline CASI scores. The lower left plot denotes the relationship between baseline cholesterol levels and changes in CASI score. The lower right plot denotes the relationship between changes in cholesterol levels and CASI scores. Asterisk sign denotes a significant quadratic relationship. Abbreviations are the same as those used in Fig. 1
Relationship between serum LDL-c levels and CASI scores. LDL-c: Low-density lipoprotein cholesterol. Note and other abbreviations are the same as those used in Fig. 1
Subgroup analyses
Serum cholesterol levels did not significantly nor linearly correlate with changes in CASI scores in each of the subgroups after controlling for covariates (TC: SMCI-S: p = 0.082–0.623; SMCI-D: p = 0.372–0.954; Dementia-S: p = 0.517–0.903; Dementia-D: p = 0.107 − 0.524; HDL-c: SMCI-S: p = 0.084–0.461; SMCI-D: p = 0.023–0.762; Dementia-S: p = 0.419–0.870; Dementia-D: p = 0.021–0.058; LDL-c: SMCI-S: p = 0.040–0.551; SMCI-D: p = 0.397–0.773; Dementia-S: p = 0.735–0.961; Dementia-D: p = 0.110–0.657; TG: SMCI-S: p = 0.036–0.130; SMCI-D: p = 0.062–0.314; Dementia-S: p = 0.822–0.995; Dementia-D: p = 0.084–0.862) (supplementary Tables 3–6). Relationships between changes in TC and changes in CASI scores (R2 = 0.064, | residuals | = 5.23–10.01, F = 13.706, p < 0.001) as well as between changes in TG and changes in CASI scores (R2 = 0.020, | residuals | = 9.71–17.20, F = 4.165, p < 0.016) could be explained by inverted U-shaped functions in the SMCI-D group (supplementary Figs. 3 and 4). Changes in LDL-c were also non-linearly and quadratically associated with changes in CASI scores with an inverted U-shaped relationship in SMCI-S (R2 = 0.059, | residuals | = 9.98–17.20, F = 12.447, p < 0.001) and SMCI-D (R2 = 0.059, | residuals | = 10.23–18.33, F = 12.447, p < 0.001) groups (Fig. 4). The relationship between changes in HDL-c and changes in CASI scores can also be explained by an inverted U-shaped function in Dementia-S group (R2 = 0.020, | residuals | = 10.10–18.23, F = 3.263, p < 0.016) (supplementary Fig. 5). The associations become insignificant after removing the cubic terms of serum cholesterol in the models (p = 0.21–0.78).
Relationship between serum LDL-c levels and CASI scores across individuals with different cognitive states. Note and abbreviations are the same as those used in Fig. 3
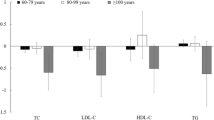
Effects of extreme changes in cholesterol
There were no differences in level of changes in CASI scores between individuals in 1st decile and 10th decile groups of changes in cholesterol (TC, p = 0.266–0.73 L; HDL-c, p = 0.207–0.645; LDL-c, p = 0.355–0.972), with the exception of individuals with SMCI-S in 1st decile of TG changes displaying a slight but significant improvement in CASI scores over individuals with SMCI-S in 10th decile (1.438 vs. -1.154, t(202) = 2.275, p < 0.05) (total sample: p = 0.440; other subgroups: p = 0.420–0.823) (supplementary Fig. 6).
Sensitivity analyses
Sensitivity analysis excluding individuals with SCD in the SMCI-S and SMCI-D groups revealed very similar results except for the results in terms of taking statins become insignificant (p = 0.302) and males were associated with a higher baseline CASI scores (p < 0.016) in model 1 for LDL-c in the SMCI-D group. All other sensitivity analyses for fitting the quadratic functions remained the same for delineated relationships between cholesterol and cognitive function in the groups and individuals with extreme changes in cholesterol (p < 0.016).
Discussion
In this study, we retrospectively investigated associations between serum cholesterol and cognitive function among individuals with different cognitive states. Baseline TC and LDL-c levels were linearly associated with maintenance or improvement in cognitive function after controlling for covariates. However, most associations between baseline or changes in cholesterol with cognitive function could be explained by non-linear, quadratic, and inverted U-shaped functions. The inverted U-shaped relationships were most evident between changes in TC, TG, and LDL-c in SMCI-D group and between HDL-c and cognitive function in Dementia-D group. No differences were observed in cognitive decline between individuals with drastic changes in serum cholesterol, with the exception of a mild improvement in cognitive function with an extreme TG decline in the SMCI-S group.
Guidelines for lipid control in CVD have mainly focused on lowering LDL-c [10, 11], however, associations between cholesterol and cognitive function have remained controversial [7, 12, 13, 41,42,43]. Previous research has reported deleterious effects of LDL-c on cognitive function [41, 44]. It appears that oxidized LDL-c promotes the development of atherosclerosis and chronic inflammation in the intima of arteries [45]. For example, one study reported that compared with LDL-c levels at 70.0–99.9 mg/dL, low LDL-c levels (< 70 mg/dL, especially < 55 mg/dL) were associated with significantly slower cognitive decline in a population-based setting [44]. There was, however, a non-linear trend for the effects of LDL-c on cognitive function in this study (i.e., a worse prognosis for cognitive function was observed among individuals with LDL-c levels between 70.0 and 99.9 mg/dL rather than higher or lower levels) [44].
Previous studies have focused on individuals with normal cognitive states and emphasized the importance of lowering LDL-c on health [46, 47]. Although this may be true among middle-aged individuals [48], our results indicate that decreases in LDL-c were only linearly associated with maintenance or improvement of cognition among older people with SMCI-S. Similarly, aggressively lowering TG appeared to cause a favorable effect on cognitive function for individuals with SMCI-S only, due perhaps to the fact that negative impacts of increases in LDL-c and TG on cognitive function are relatively more evident in early stages of cognitive decline. Furthermore, participants in this study were older than those in many previous studies. Protective effect of serum cholesterol on the preservation of cognitive decline might be more marked among older people than among younger people.
Consistent with other studies [1, 14, 15], we found that a non-linear and inverted U-shaped relationship could explain most of the relationships between serum cholesterol and cognitive function among older people, including the relationship between LDL-c and cognitive function. A recent study suggested that longitudinal increases in non-HDL-c may be protective for cognitive function among females or individuals without cardiovascular disease [43]. Similarly, a study reported that the risk for a decline in global cognitive (OR = 0.50) and memory function (OR = 0.45) was remarkably lower among older people with long-term increases in non-HDL-c than those in the consistently low level group [42]. Our results revealing an inverted U-shaped relationship between cholesterol and cognitive function might reflect the fact that cholesterol is important for myelination in the brain [49, 50]. Individuals with a low level or drastic decrease in cholesterol might suffer from reduced levels of myelination in the brain, especially in the early stages of cognitive decline.
Demyelination and axonal damage have recently been considered an important and potentially treatable neuropathology in AD [18, 51]. Previous studies have proposed complex interactive relationships between damage in myelin and amyloid in gray matter. Some studies have reported that demyelination occurs in the preclinical stages of AD, at a time when neurodegeneration is not apparent [25, 51, 52]. The findings of a more pronounced inverted U-shaped relationship between cholesterol and cognitive function in the SMCI-D group might reflect the fact that cholesterol plays a role in the process of demyelination in the early stages of AD. In addition, studies have found that sufficient levels of cholesterol may also prevent transmission or generation of AD pathologies [23, 25].
We found a non-linear and inverted-U relationship between changes in HDL-c and cognitive decline in Dementia-D group. Researchers have recently suggested that cholesterol also plays a role in preventing inflammation [45]. HDL-c may facilitate cholesterol efflux and inhibit the process of molecular adhesion during the formation of atherosclerotic plaques [45]. Previous studies have reported that cholesterol levels are correlated with cognitive decline during middle adulthood [48]. By contrast, cholesterol levels are negatively correlated with cognitive decline in late adulthood. The older age of the Dementia-D individuals in this study might be associated with the impacts of cholesterol changes in these individuals, especially changes in HDL-c and TG. The sensitivity of individuals in the Dementia-D group could be due to the fact that they are more prone to suffer from damage to blood vessels associated with atherosclerotic plaques [45]. In addition, the potentially poor brain state of these individuals may also contribute to sensitivity to HDL-c and TG changes [16].
This study shed new light on the relationship between cholesterol and cognitive function among older people. However, this study is subject to several limitations. First, the follow-up duration was relatively short; the full impact of changes in cholesterol levels on cognitive function could be better elucidated with longer follow-ups in future studies. Second, we did not collect information regarding treatment doses for CVD risks. Thus, the optimal level of cholesterol on cognitive function could be a result of proper pharmacological control of CVD risks [53, 54]. Third, the sample size in this study was relatively small whereby some of the subgroups may have been too small to detect any effects of cholesterol on cognitive function. Fourth, the present study could not completely exclude reverse causality. Individuals with cognitive decline could have exhibited changes in several factors that may have been associated with poor brain health (e.g., dietary habit, microbiota, or exercise habit) [55]. The possibility could cause the low explaining ability of the models in this study. Fifth, the prevalence of CVD risks among the excluded individuals was lower in this study. The relationship between serum cholesterol and cognitive functions may not be necessarily the same among individuals with better CVD risk management than current samples. Similarly, the current study included only the clinical samples. Baseline conditions, including the cognitive conditions, among the samples might be poorer than general population. Future studies could investigate these issues with a randomized control design and larger samples to further unravel the mechanisms of effects of cholesterol on brain and cognitive functions.
Most relationships between cholesterol and cognitive function conform to an inverted U-shaped function among older people. The inverted U-shaped relationship between cognitive function and cholesterol may be most evident in the early stages of cognitive decline. A balance between reducing CVD risks and preserving cognitive function should always be taken into consideration in clinical practice. It is merited to consider for effects of cholesterol reduction on cognitive decline among older people.
Data availability
Data available on request due to privacy/ethical restrictions. Requests to access these datasets should be directed to H-T C, changht@cycu.edu.tw.
References
An Y, Zhang X, Wang Y, Wang Y, Liu W, Wang T, Qin Z, Xiao R. Longitudinal and nonlinear relations of dietary and serum cholesterol in midlife with cognitive decline: results from EMCOA study. Mol Neurodegener. 2019;14(1):51.
Kivipelto M, Helkala EL, Hänninen T, Laakso MP, Hallikainen M, Alhainen K, Soininen H, Tuomilehto J, Nissinen A. Midlife vascular risk factors and late-life mild cognitive impairment: a population-based study. Neurology. 2001;56(12):1683–9.
Li X-Y, Zhang M, Xu W, Li J-Q, Cao X-P, Yu J-T, Tan L. Midlife modifiable risk factors for dementia: a systemic review and meta-analysis of 34 prospective cohort studies. Curr Alzheimer Res. 2019;16(14):1254–68.
Ranson JM, Rittman T, Hayat S, Brayne C, Jessen F, Blennow K, van Duijn C, Barkhof F, Tang E, Mummery CJ, et al. Modifiable risk factors for dementia and dementia risk profiling. A user manual for Brain Health services—part 2 of 6. Alzheimer’s Res Ther. 2021;13(1):169.
Licher S, Ahmad S, Karamujić-Čomić H, Voortman T, Leening MJG, Ikram MA, Ikram MK. Genetic predisposition, modifiable-risk-factor profile and long-term dementia risk in the general population. Nat Med. 2019;25(9):1364–9.
Anstey KJ, Lipnicki DM, Low LF. Cholesterol as a risk factor for dementia and cognitive decline: a systematic review of prospective studies with meta-analysis. Am J Geriatr Psychiatry. 2008;16(5):343–54.
Mielke MM, Zandi PP, Shao H, Waern M, Östling S, Guo X, Björkelund C, Lissner L, Skoog I, Gustafson DR. The 32-year relationship between cholesterol and dementia from midlife to late life. Neurology. 2010;75(21):1888–95.
Liang J-h, Lu L, Li J-y, Qu X-y, Li J, Qian S, Wang Y-q, Jia R-x, Wang C-s, Xu Y. Contributions of modifiable risk factors to dementia incidence: a Bayesian network analysis. J Am Med Dir Assoc. 2020;21(11):1592–e913.
Spencer-Bonilla G, Chung S, Sarraju A, Heidenreich P, Palaniappan L, Rodriguez F. Statin use in older people with stable atherosclerotic cardiovascular disease. J Am Geriatr Soc. 2021;69(4):979–85.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;139(25):e1082–e143.
Raygor V, Khera A. New recommendations and revised concepts in recent guidelines on the management of dyslipidemias to prevent cardiovascular disease: the 2018 ACC/AHA and 2019 ESC/EAS guidelines. Curr Cardiol Rep. 2020;22(9):87.
Zhang X, Wen J, Zhang Z. Statins use and risk of dementia: a dose-response meta analysis. Medicine. 2018;97(30):e11304.
Lu G, Li Z. Statin therapy on cognitive decline and incident dementia. J Am Coll Cardiol. 2021;78(14):e101.
Yang FN, Stanford M, Jiang X. Low cholesterol level linked to reduced semantic fluency performance and reduced gray matter volume in the medial temporal lobe. Front Aging Neurosci. 2020;12.
Wendell CR, Waldstein SR, Zonderman AB. Nonlinear longitudinal trajectories of cholesterol and neuropsychological function. Neuropsychology. 2014;28(1):106–12.
Chen C-L, Kuo M-C, Chen P-Y, Tung Y-H, Hsu Y-C, Huang C-WC, Chan WP, Tseng W-YI. Validation of neuroimaging-based brain age gap as a mediator between modifiable risk factors and cognition. Neurobiol Aging. 2022;114:61–72.
Marebwa BK, Adams RJ, Magwood GS, Basilakos A, Mueller M, Rorden C, Fridriksson J, Bonilha L. Cardiovascular risk factors and brain health: impact on long-range cortical connections and cognitive performance. J Am Heart Assoc. 2018;7(23):e010054.
Nasrabady SE, Rizvi B, Goldman JE, Brickman AM. White matter changes in Alzheimer’s disease: a focus on myelin and oligodendrocytes. Acta Neuropathol Commun. 2018;6(1):22.
Morrison C, Dadar M, Villeneuve S, Ducharme S, Collins DL. White matter hyperintensity load varies depending on subjective cognitive decline criteria. GeroScience. 2023;45(1):17–28.
Tang BL. Cholesterol synthesis inhibition or depletion in axon regeneration. Neural Regeneration Res. 2022;17(2):271–6.
Shabanzadeh AP, Charish J, Tassew NG, Farhani N, Feng J, Qin X, Sugita S, Mothe AJ, Wälchli T, Koeberle PD, et al. Cholesterol synthesis inhibition promotes axonal regeneration in the injured central nervous system. Neurobiol Dis. 2021;150:105259.
Szabo L, Cummins N, Paganetti P, Odermatt A, Papassotiropoulos A, Karch C, Götz J, Eckert A, Grimm A. ER-mitochondria contacts and cholesterol metabolism are disrupted by disease-associated tau protein. EMBO Rep. 2023;24(8):e57499.
Varma VR, Büşra Lüleci H, Oommen AM, Varma S, Blackshear CT, Griswold ME, An Y, Roberts JA, O’Brien R, Pletnikova O, et al. Abnormal brain cholesterol homeostasis in Alzheimer’s disease—a targeted metabolomic and transcriptomic study. Npj Aging Mech Disease. 2021;7(1):11.
Dimou E, Katsinelos T, Meisl G, Tuck BJ, Keeling S, Smith AE, Hidari E, Lam JYL, Burke M, Lövestam S, et al. Super-resolution imaging unveils the self-replication of tau aggregates upon seeding. Cell Rep. 2023;42(7):112725.
Tuck BJ, Miller LVC, Katsinelos T, Smith AE, Wilson EL, Keeling S, Cheng S, Vaysburd MJ, Knox C, Tredgett L et al. Cholesterol determines the cytosolic entry and seeded aggregation of tau. Cell Rep. 2022;39(5).
Wang C-T, Hung G-U, Wei C-Y, Tzeng R-C, Chiu P-Y. An informant-based simple questionnaire for visuospatial dysfunction assessment in dementia. Front Neurosci. 2020;14:44.
Lin KN, Wang PN, Liu CY, Chen WT, Lee YC, Liu HC. Cutoff scores of the cognitive abilities screening instrument, Chinese version in screening of dementia. Dement Geriatr Cogn. 2002;14(4):176–82.
Hung C-H, Hung G-U, Wei C-Y, Tzeng R-C, Chiu P-Y. Function-based dementia severity assessment for vascular cognitive impairment. J Formos Med Assoc. 2021;120(1, Part 2):533–41.
Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, Nordberg A, Bäckman L, Albert M, Almkvist O, et al. Mild cognitive impairment – beyond controversies, towards a consensus: report of the international working group on mild cognitive impairment. J Intern Med. 2004;256(3):240–6.
Yang YW, Hsu KC, Wei CY, Tzeng RC, Chiu PY. Operational determination of subjective cognitive decline, mild cognitive impairment, and dementia using sum of boxes of the clinical dementia rating scale. Front Aging Neurosci. 2021;13:705782.
Tzeng R-C, Yang Y-W, Hsu K-C, Chang H-T, Chiu P-Y. Sum of boxes of the clinical dementia rating scale highly predicts conversion or reversion in predementia stages. Front Aging Neurosci. 2022;14:1021792.
O’Bryant SE, Lacritz LH, Hall J, Waring SC, Chan W, Khodr ZG, Massman PJ, Hobson V, Cullum CM. Validation of the new interpretive guidelines for the clinical dementia rating scale sum of boxes score in the national Alzheimer’s coordinating center database. Arch Neurol. 2010;67(6):746–9.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr., Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Ageing-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Tsai C-H, Su J-L, Wu M-H, Huang C-J, Lin J-L. Estimating low density lipoprotein-cholesterol by a new formula instead of the Friedwald formula in adult Taiwanese. Taiwan J Family Med. 2013;2(1):10–9.
Team. RC. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014.
Luo C-M, Hsieh M-Y, Cheng C-H, Chen C-H, Liao M-T, Chuang S-Y, Wu C-C. Association of frailty with thrombosis of hemodialysis vascular access: a prospective Taiwanese cohort study. Am J Kidney Dis. 2022;80(3):353–e631.
Ozili PK. The acceptable R-square in empirical modeling for social science research. Social research methodology and publishing results: a uide to non-native English speakers. Edited by Saliya CA: IGI Global; 2023.
Menyhart O, Weltz B, Győrffy B. MultipleTesting.com: a tool for life science researchers for multiple hypothesis testing correction. PLoS ONE. 2021;16(6):e0245824.
Shaffer JP. Multiple hypothesis testing. Annu Rev Psychol. 1995;46:561–84.
Iwagami M, Qizilbash N, Gregson J, Douglas I, Johnson M, Pearce N, Evans S, Pocock S. Blood cholesterol and risk of dementia in more than 1·8 million people over two decades: a retrospective cohort study. Lancet Healthy Longev. 2021;2(8):e498–506.
Liu H, Zou L, Zhou R, Zhang M, Gu S, Zheng J, Hukportie DN, Wu K, Huang Z, Yuan Z, et al. Long-term increase in cholesterol is associated with better cognitive function: evidence from a longitudinal study. Front Aging Neurosci. 2021;13:691423.
Pang K, Liu C, Tong J, Ouyang W, Hu S, Tang Y. Higher total cholesterol concentration may be associated with better cognitive performance among elderly females. Nutrients. 2022;14(19):4198.
Hua R, Ma Y, Li C, Zhong B, Xie W. Low levels of low-density lipoprotein cholesterol and cognitive decline. Sci Bull. 2021;66(16):1684–90.
Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat Rev Immunol. 2015;15(2):104–16.
Anstey KJ, Ashby-Mitchell K, Peters R. Updating the evidence on the association between serum cholesterol and risk of late-life dementia: review and meta-analysis. J Alzhermers Dis. 2017;56(1):215–28.
Sáiz-Vazquez O, Puente-Martínez A, Ubillos-Landa S, Pacheco-Bonrostro J, Santabárbara J. Cholesterol and Alzheimer’s disease risk: a meta-meta-analysis. Brain Sci. 2020;10(6):386.
Shepardson NE, Shankar GM, Selkoe DJ. Cholesterol level and statin use in Alzheimer disease: I. Review of epidemiological and preclinical studies. JAMA Neurol. 2011;68(10):1239–44.
Yi SW, Yi JJ, Ohrr H. Total cholesterol and all-cause mortality by sex and age: a prospective cohort study among 12.8 million people. Sci Rep. 2019;9(1):1596.
Douaud G, Groves AR, Tamnes CK, Westlye LT, Duff EP, Engvig A, Walhovd KB, James A, Gass A, Monsch AU, et al. A common brain network links development, aging, and vulnerability to disease. Proc Natl Acad Sci U S A. 2014;111(49):17648–53.
Morrison C, Dadar M, Villeneuve S, Ducharme S, Collins DL. White matter hyperintensity load varies depending on subjective cognitive decline criteria. GeroScience. 2022.
Fischer FU, Wolf D, Scheurich A, Fellgiebel A. Altered whole-brain white matter networks in preclinical Alzheimer’s disease. NeuroImage Clin. 2015;8:660–6.
Olmastroni E, Molari G, De Beni N, Colpani O, Galimberti F, Gazzotti M, Zambon A, Catapano AL, Casula M. Statin use and risk of dementia or Alzheimer’s disease: a systematic review and meta-analysis of observational studies. Eur J Prev Cardiol. 2022;29(5):804–14.
Torrandell-Haro G, Branigan GL, Vitali F, Geifman N, Zissimopoulos JM, Brinton RD. Statin therapy and risk of Alzheimer’s and age-related neurodegenerative diseases. Alzheimers Dement. 2020;6(1):e12108.
Claesson MJ, Jeffery IB, Conde S, Power SE, O’Connor EM, Cusack S, Harris HM, Coakley M, Lakshminarayanan B, O’Sullivan O, et al. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;488(7410):178–84.
Acknowledgements
We would like to thank the members of History-Based Artificial Intelligent Clinical Dementia Diagnostic System (HAICDDS) Project for their help in completing this research.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, formal analysis and investigation, writing (original draft preparation): H.-T.C. Writing (review and editing): P.-C.C. Conceptualization, methodology, writing (review and editing), supervision: P.-Y.C.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the Show Chwan Memorial Hospital (SCMH_IRB1081006) and informed consent was waived by the Institutional Review Board of the Show Chwan Memorial Hospital (SCMH_IRB1081006) because of the retrospective nature of the study design and data were processed anonymously.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chang, HT., Chan, PC. & Chiu, PY. Non-linear relationship between serum cholesterol levels and cognitive change among older people in the preclinical and prodromal stages of dementia: a retrospective longitudinal study in Taiwan. BMC Geriatr 24, 474 (2024). https://doi.org/10.1186/s12877-024-05030-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05030-0