Abstract
Background
The accelerated growth of older individuals worldwide has increased the number of patients presenting with fragility hip fractures. Having a hip fracture can cause excess mortality, and patients with hip fracture have a higher risk of death than those without hip fracture. Most studies have treated hip fracture as a single, homogeneous condition, but hip fracture includes two major anatomic types: intertrochanteric fracture and femoral neck fracture. Few studies have specifically evaluated 1-year mortality risk in older individuals with femoral intertrochanteric fracture. The aim of this study was to evaluate 1-year mortality and factors associated with mortality in older individuals with femoral intertrochanteric fracture.
Methods
A retrospective review was conducted of 563 patients ≥ 65 years old who underwent surgery for femoral intertrochanteric fractures at our institution between January 2010 and August 2018. Patient demographics, comorbidities, and treatment were collected by retrospective chart review. Age, sex, Body Mass Index (BMI), American Society of Anesthesiologists (ASA) classification, Charlson comorbidity index (CCI), Arbeitsgemeinschaft Für Osteosynthesefragen (AO) fracture classification, haemoglobin value at admission, time to surgery, operation time, and intraoperative blood loss were risk factors to be tested. Multivariable logistic regression was used to evaluate associations between variables and death.
Results
Among the 563 patients, 49 died within 1 year after surgery, and the 1-year mortality rate was 8.7%. Multivariate analysis identified age > 80 years (OR = 4.038, P = 0.011), haemoglobin < 100 g/l (OR = 2.732, P = 0.002), ASA score ≥ 3 (OR = 2.551, P = 0.005), CCI ≥ 3 (OR = 18.412, P = 0.018) and time to surgery > 14 d (OR = 3.907, P = 0.030) as independent risk factors for 1-year mortality. Comorbidities such as myocardial infarction and chronic pulmonary disease were associated with 1-year mortality after adjusting for age > 80 years and time to surgery > 14 days.
Conclusions
Patients over 80 years old with haemoglobin < 100 g/l, ASA score ≥ 3, CCI ≥ 3, and multiple comorbidities, especially myocardial infarction and chronic pulmonary disease before surgery, are at a higher risk of 1-year mortality. Doctors should pay more attention to these vulnerable patients, and a surgical delay greater than 14 days should be avoided.
Similar content being viewed by others
Background
Osteoporotic fractures pose an important economic and health burden in China and worldwide. Hip fracture is one of the most devastating consequences of osteoporosis [1] and is becoming one of the most important public health problems in the world [2]. Femoral intertrochanteric fracture and femoral neck fracture are its two main types. Although hip fracture is discussed as a unified entity, there are significant differences in the incidence rate and mortality after operation for femoral intertrochanteric fracture and femoral neck fracture. According to our previous systematic analysis, the pooled estimate of the 1-year mortality rate was 17.47% after femoral intertrochanteric fracture and 9.83% after femoral neck fracture between 2000 and 2018 [3]. Many studies [4,5,6] on hip fractures have described high mortality rates. Most studies document an increase in mortality lasting for 6 to 12 months [7, 8]. Identifying predictors of 1-year mortality could help discriminate between those at higher risk of adverse outcomes and facilitate targeted interventions [9]. Here we report the results of a consecutive population of femoral intertrochanteric fracture patients from our hospital. We reviewed the patient admission data and identified any predictors of patients at high risk of mortality not only during the immediate perioperative period but also over the year after discharge.
Methods
Patient data
The medical records of patients who underwent surgery for femoral intertrochanteric fractures at our institution between January 2010 and August 2018 were retrospectively reviewed. Inclusion criteria: (1) fresh closed femoral intertrochanteric fracture (≤ 3 weeks) and (2) age ≥ 65 years. Exclusion criteria: (1) pathological fracture, open fracture or periprosthetic fracture; and (2) poly-trauma.
Operative protocol
Five experienced orthopaedic surgeons performed all of the surgeries. Spinal anaesthesia or general anaesthesia was used. Reduction and internal fixation were performed with the patients in the supine position on a fracture table using an image intensifier. After closed manipulation, intraoperative images were taken to evaluate the reduction quality of the fracture. Patients then underwent routine surgical procedures for internal fixation according to the manufacturer’s protocol.
Time to mobilization after surgery
All patients commenced the routine rehabilitation treatment post-operation, which included immediate ankle pump training. On the first postoperative day, non-weight bearing joint mobility training was conducted, and patients were motivated to ambulate with assistance. Partial weight bearing was initiated once radiographic evidence of fracture healing appeared, progressing to full weight bearing upon clinical confirmation of fracture healing.
Follow-up method
Patients were asked to return to hospital 1 month, 2 months, 3 months, 6 months, and 1 year after surgery. If the patients did not return on time, then a phone call or a video call was made to record their status. Patients who could not be reached after discharge were counted as lost to follow-up. Time to death (in months) was calculated from the date of surgery.
Risk factors
The following general data were collected from medical records: age, sex, Body Mass Index (BMI), American Society of Anesthesiologists (ASA) classification, Charlson comorbidity index (CCI) [10] and age-adjusted CCI (aCCI) [11].
The following surgical data were also collected: the Arbeitsgemeinschaft Für Osteosynthesefragen (AO) classification [12] of the fracture, haemoglobin value (g/l) at admission, time to surgery (≤ 2 d, 2 d to 14 d, or > 14 d, time from injury to surgery), operation time (min), and intraoperative blood loss (ml).
Statistical analysis
The chi-squared test was used to compare categorical variables between groups. For quantitative data, the one-sample Kolmogorov‒Smirnov test was used to test the normality of the distribution. Student’s t test or the Mann‒Whitney test was used to compare continuous variables, as appropriate. All variables were evaluated using unconditional univariate logistic regression analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. All variables with P < 0.05 in the univariate analysis were included in a multivariate model. Statistical significance was defined as P < 0.05. All statistical analyses were performed using SPSS 22.0 (SPSS, Chicago, IL, USA).
Results
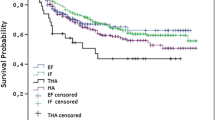
According to the inclusion criteria and exclusion criteria, 688 femoral intertrochanteric fractures were included in this study. There were 125 patients lost to follow-up. Therefore, a total of 563 patients were analysed. They were 175 (31.1%) males and 388 (68.9%) females. The patients were aged from 65 to 97 years, with an average of 80.1 ± 6.4 years. Among the 563 patients, 49 died within 1 year after surgery, for a 1-year mortality rate of 8.7%. Five patients died in hospital, for a nosocomial mortality rate of 0.9%.
The general and surgical data of living and dead patients were compared (Table 1). There were no significant differences in sex, BMI, AO classification, operation time, or intraoperative blood loss between groups (P > 0.05). The average age of patients in the deceased group was higher than that of patients in the alive group (P = 0.002). The 1-year mortality was higher in patients with ASA score ≥ 3 (51.0% versus 25.9% in survivors, P < 0.001). The results also showed differences in haemoglobin (P < 0.001), CCI (P = 0.07), aCCI (P = 0.016), and time to surgery (P = 0.029) between the two groups. To further analyse the differences between the two groups, a univariate analysis was conducted.
Univariate analysis identified age > 80 years (P = 0.013), haemoglobin < 100 g/l (P = 0.001), ASA score ≥ 3 (P < 0.001), CCI ≥ 3 (P = 0.005), aCCI ≥ 7 (P = 0.009) and time to surgery > 14 d (P = 0.012) as risk factors for 1-year mortality (Table 2).
After controlling for confounding variables, multivariate analysis identified age > 80 years (P = 0.011), haemoglobin < 100 g/l (P = 0.002), ASA score ≥ 3 (P = 0.005), CCI ≥ 3 (P = 0.018) and time to surgery > 14 d (P = 0.030) as independent risk factors for 1-year mortality (Table 2). In femoral intertrochanteric fracture patients, those over 80 years had a 4.038-fold higher risk of 1-year morality than the younger elderly. Patients with haemoglobin < 100 g/l had 2.732 times the risk of 1-year morality of those with haemoglobin ≥ 100 g/l. Patients with ASA score ≥ 3 had 2.551 times the risk of 1-year morality of those with a score < 3. Patients with CCI ≥ 3 had 18.412 times the risk of 1-year mortality of those with CCI = 0. Patients who underwent surgery more than 14 days after fracture had 3.907 times the risk of 1-year mortality of those who underwent surgery within 2 days.
Of the pathologies evaluated by the CCI, diabetes mellitus was the most common condition, being found in 17.1% (n = 96) of the cases, followed by cerebrovascular disease at 8.2% (n = 46), myocardial infarction at 5.5% (n = 31), any tumour at 3.0% (n = 17) and chronic pulmonary disease (chronic obstructive pulmonary disease (COPD) and asthma) at 2.0% (n = 11). Other diseases, such as dementia, connective tissue disease, renal disease, congestive heart failure, peripheral vascular disease, and metastatic solid tumours, were also present in the patients, but in fewer than 10 patients. Ulcer disease; mild, moderate or severe liver disease; leukaemia; lymphoma; and AIDS were not found in this study (Table 3).
Comorbidities such as myocardial infarction and chronic pulmonary disease were associated with mortality during the first post-operative year after adjusting for age > 80 years and time to surgery > 14 days (Table 3).
Discussion
The accelerating growth of the global elderly population has increased the number of patients with fragile hip fractures [13, 14]. Hip fractures are among the fractures with the highest risk of death [15]. Hip fractures can lead to excess mortality, and patients with hip fractures have a higher risk of death than those without hip fractures [16, 17]. Results for 1-year mortality after hip fracture have been reported to vary. Abrahamsen et al. [18] performed a meta-analysis and found a 1-year mortality rate of 5.9 to 59%. In 2008 and 2009, the 1-year mortality rate after hip fractures among nursing home residents in Canada was approximately 45% [19]. Among Asian populations, the 1-year mortality rates were also different: 17.8% for Korean women [20], 18.65% for Hong Kong [21], and 13.5% for Taiwanese women [22]. In mainland China, a study showed the 1-year mortality in Beijing was approximately 23.44% [17]. Most studies have treated hip fracture as a single, uniform condition, but it includes two major anatomic types: intertrochanteric fractures and femoral neck fractures. The former is an extracapsular fracture, and the latter is an intracapsular fracture. A previous study showed that the 90-day mortality rate after intertrochanteric fracture of the femur was 12.1% and 9.6% after femoral neck fracture [23]. Another study showed that fracture type is an independent predictor of mortality in patients with hip fractures at 1 month and 1 year after injury [24]. Therefore, we should treat intertrochanteric fractures and femoral neck fractures differently and analyse their mortality rates separately.
In the present study of 563 patients who underwent surgery for femoral intertrochanteric fractures, 49 (8.7%) died within one year of surgery. Age, haemoglobin value at admission, ASA score, CCI and time to surgery were associated with 1-year mortality after surgery.
The present study showed that individuals over 80 years had a risk of 1-year morality 4.038 times that of younger individuals. Advanced age and male sex are known risk factors for mortality after hip fracture [25, 26]. Most previous studies have emphasized advanced age as the main cause of mortality and morbidity after hip fracture [27,28,29], but the relationship between sex and mortality remains controversial. Mariconda et al. [27] found that the 1-year mortality rate after a hip fracture was lower for patients aged > 80 years than for those aged < 80 years. Kim et al. [30] also found that age over 80 years was a predictor of 1-year mortality. Ferris et al. [8] found that male sex significantly predicted increased mortality, while other authors found that sex has no effect on mortality [29, 30]. In the present study, age was a significant predictor of 1-year mortality, but sex was not.
Nutritional status stands as a potential factor linked to 1-year mortality. Prior research has established a correlation between a low BMI and increased mortality rates [31]. Specifically, one study revealed that individuals with a BMI below 22 kg/m2 faced an almost seven-fold increase in 1-year mortality compared to those with a BMI exceeding 25 kg/m2 [32]. Another study echoed these findings, noting that obese patients (with a BMI of 30 kg/m2 or higher) exhibited the lowest risk of 1-year mortality, whereas those with a BMI less than 22 kg/m2 demonstrated the highest risk [33]. In our current study, although BMI served as a proxy for patients’ nutritional status, our analysis did not reveal a statistically significant difference in BMI between the survivors and the deceased (P > 0.05). Consequently, the impact of BMI on 1-year mortality warrants further examination.
Hip fracture patients, particularly those suffering from intertrochanteric fractures, frequently exhibit comorbid anemia. However, the degree of anemia and its association with 1-year mortality remain unclear. Espinosa et al. [34] found that haemoglobin values at the moment of hospital admission were associated with increased mortality, and the study showed that patients with haemoglobin < 10 g/dl had an increase of 1.51 times the mortality at 1 year, as compared to those with haemoglobin ≥ 10 g/dl. The present study showed same outcome, individuals with haemoglobin < 100 g/l had a risk of 1-year morality 2.732 times those haemoglobin ≥ 100 g/l. The result suggests that we should pay attention to the adverse effects of anemia, especially in individuals with haemoglobin less than 100 g/l.
The ASA score is based on a subjective assessment of patients’ health status before surgery. It was evaluated immediately prior to surgery. Liu et al. [14] found that ASA grading was significantly correlated with the incidence of postoperative complications and 1-year mortality in nonagenarians undergoing hip fracture surgery. Daugaard et al. [35] showed that increasing ASA score would significantly increase the mortality rate. Pugely et al. [36] also found that age greater than 80 years, male sex, declining functional status, ASA grade 3 or 4, and a history of cancer were independent risk factors for 30-day mortality. As in other studies [37,38,39], increasing ASA grade has independent deleterious effects on mortality and complications. This is consistent with the findings of our study, where an ASA score ≥ 3 was strongly associated with mortality. Patients with an ASA score ≥ 3 had a risk of 1-year mortality 2.551 times that of patients with an ASA score < 3.
Many studies have shown that comorbidities are associated with increased mortality or poor functional outcomes [16, 25, 29]. The CCI was developed by Charlson and colleagues in 1987 to classify comorbidities that may affect the risk of death [10]. The CCI considers 19 medical conditions, with the resulting score rising with their severity. The CCI is the most widely used comorbidity index for predicting survival rate (1 year and 10 years) in patients with multiple comorbidities. We hypothesized that multiple comorbidities (CCI ≥ 3) would be associated with a higher mortality, which was supported by our results. Patients with CCI ≥ 3 had a 18.412-fold risk of 1-year morality compared to those with CCI = 0.
In the present study, among various kinds of comorbidities, myocardial infarction and chronic pulmonary disease were found to be associated with 1-year mortality. These findings were mostly consistent with published papers. Espinosa et al. [29] found that diseases such as myocardial infarction, chronic pulmonary disease and hemiplegia caused by stroke were associated with increased 1-year mortality. Chang et al. [28] found that malignant tumor, cardiovascular disease and pulmonary disease were risk factors for mortality after hip fracture surgery. Friesendorff et al. [40] found that cardiovascular disease and pneumonia were the leading causes of death in both men and women of all age groups. Specifically, both myocardial infarction and cardiac failure are considered to be common determinants of death after hip fracture surgery [41]. Another study reported that patients with COPD had a 60–70% higher risk of death after hip fracture surgery than those without COPD [42]. In short, common comorbidities were associated with a higher risk of death after hip fracture surgery. The speculated reason is that patients with high mortality are often affected by postoperative complications such as infection, myocardial ischaemia, and thromboembolism. Given these findings, patients with these comorbidities require extra attention to reduce the risk of postoperative death.
Clinical guidelines recommend that elderly patients receive surgery within 48 h after hospital admission [43, 44]. However, in developing countries, there may be greater uncertainty about the effects of early surgery, as some studies have shown that postoperative mortality is similar in patients with short and long preoperative delays [29]. In contrast, in developed countries, patients may be admitted to hospital within 6 h after the trauma and receive surgical treatment within 24 h after the fracture, with similar mortality rates at one year after surgery [45]. In the present study, patients who underwent surgery after 14 days had a risk of 1-year mortality 3.907 times that of patients who underwent surgery within 2 days. However, the difference in 1-year mortality was not significant between patients who underwent surgery after 2 days but within 14 days and patients who underwent surgery within 2 days. In fact, immediate surgery can reduce immobilization time, the risk of bedsores, infections and thromboembolic complications. Some delays in surgery may be due to the severity of the patient’s health condition, which requires adequate treatment. A delay of more than 14 days should be avoided.
This study has several limitations. First, it was a retrospective observational study, and some patients were lost to follow-up. Second, it was a single-centre study, so there might have been selection bias. Third, some patients died in the community or other medical institutions, and we could not obtain the accurate causes of death from their family members, so the cause of death was not analyzed in this study.
Conclusions
This study identified risk factors for 1-year mortality in older individuals with femoral intertrochanteric fracture. Patients over 80 years old with haemoglobin < 100 g/l, ASA score ≥ 3, CCI ≥ 3, and multiple comorbidities, especially myocardial infarction and chronic pulmonary disease before surgery, are at a higher risk of 1-year mortality. These results help identify vulnerable patients whom doctors should pay more attention to. As time to surgery is another factor associated with 1-year mortality, a surgical delay greater than 14 days should be avoided.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- ASA:
-
American Society of Anesthesiologists
- CCI:
-
Charlson comorbidity index
- AO:
-
Arbeitsgemeinschaft Für Osteosynthesefragen
- OR:
-
odds ratio
- CI:
-
confidence interval
- COPD:
-
chronic obstructive pulmonary disease
References
Tosteson AN, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ 3rd. Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18(11):1463–72.
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23(9):2239–56.
Cui Z, Feng H, Meng X, Zhuang S, Liu Z, Ye K, et al. Age-specific 1-year mortality rates after hip fracture based on the populations in mainland China between the years 2000 and 2018: a systematic analysis. Arch Osteoporos. 2019;14(1):55.
Li XP, Zhang P, Zhu SW, Yang MH, Wu XB, Jiang XY. All-cause mortality risk in aged femoral intertrochanteric fracture patients. J Orthop Surg Res. 2021;16(1):727.
Gasparik AI, Lorenzovici L, Pașcanu IM, Csata Z, Poiană C, Dobre R, et al. Predictors of mortality for patients with hip fracture: a study of the nationwide 1-year records of 24,950 fractures in Romania. Arch Osteoporos. 2023;18(1):69.
Nishimura Y, Inagaki Y, Noda T, Nishioka Y, Myojin T, Ogawa M, et al. Risk factors for mortality after hip fracture surgery in Japan using the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Arch Osteoporos. 2023;18(1):91.
Yoo J, Lee JS, Kim S, Kim BS, Choi H, Song DY, et al. Length of hospital stay after hip fracture surgery and 1-year mortality. Osteoporos Int. 2019;30(1):145–53.
Ferris H, Merron G, Coughlan T. 1 year mortality after hip fracture in an Irish urban trauma centre. BMC Musculoskelet Disord. 2023;24(1):487.
Hjelholt TJ, Johnsen SP, Brynningsen PK, Knudsen JS, Prieto-Alhambra D, Pedersen AB. Development and validation of a model for predicting mortality in patients with hip fracture. Age Ageing. 2022;51(1):afab233.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51.
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium – 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–133.
Melton LJ 3rd, Gabriel SE, Crowson CS, Tosteson AN, Johnell O, Kanis JA. Cost-equivalence of different osteoporotic fractures. Osteoporos Int. 2003;14(5):383–8.
Liu Y, Peng M, Lin L, Liu X, Qin Y, Hou X. Relationship between American Society of Anesthesiologists (ASA) grade and 1-year mortality in nonagenarians undergoing hip fracture surgery. Osteoporos Int. 2015;26(3):1029–33.
Smith T, Pelpola K, Ball M, Ong A, Myint PK. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43(4):464–71.
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90.
Li S, Sun T, Liu Z. Excess mortality of 1 year in elderly hip fracture patients compared with the general population in Beijing, China. Arch Osteoporos. 2016;11(1):35.
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633–50.
Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR. Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: prospective cohort study. J Am Geriatr Soc. 2012;60(7):1268–73.
Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011;26(8):1087–92.
Man LP, Ho AW, Wong SH. Excess mortality for operated geriatric hip fracture in Hong Kong. Hong Kong Med J. 2016;22(1):6–10.
Wang CB, Lin CF, Liang WM, Cheng CF, Chang YJ, Wu HC, et al. Excess mortality after hip fracture among the elderly in Taiwan: a nationwide population-based cohort study. Bone. 2013;56(1):147–53.
Frisch NB, Wessell N, Charters M, Greenstein A, Shaw J, Peterson E, et al. Hip fracture mortality: differences between intertrochanteric and femoral Neck fractures. J Surg Orthop Adv. 2018;27(1):64–71.
Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S, et al. Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007;41(6):958–64.
Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374.
Söderqvist A, Miedel R, Ponzer S, Tidermark J. The influence of cognitive function on outcome after a hip fracture. J Bone Joint Surg Am. 2006;88(10):2115–23.
Mariconda M, Costa GG, Cerbasi S, Recano P, Aitanti E, Gambacorta M, et al. The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Joint J. 2015;97–B(3):383–90.
Chang W, Lv H, Feng C, Yuwen P, Wei N, Chen W, et al. Preventable risk factors of mortality after hip fracture surgery: systematic review and meta-analysis. Int J Surg. 2018;52:320–8.
Espinosa KA, Gélvez AG, Torres LP, García MF, Peña OR. Pre-operative factors associated with increased mortality in elderly patients with a hip fracture: a cohort study in a developing country. Injury. 2018;49(6):1162–8.
Kim SM, Moon YW, Lim SJ, Yoon BK, Min YK, Lee DY, et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone. 2012;50(6):1343–50.
Malafarina V, Reginster JY, Cabrerizo S et al. Nutritional Status and Nutritional Treatment are related to outcomes and mortality in older adults with hip Fracture[J]. Nutrients,2018,10(5).
Schaller F, Sidelnikov E, Theiler R, et al. Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after hip fracture. Bone. 2012;51(3):347–52.
Modig K, Erdefelt A, Mellner C et al. Obesity Paradox holds true for patients with hip fracture: a Registry-based cohort Study[J]. J Bone Joint Surg Am 2019,101(10):888–95.
Espinosa KA, Gelvez AG, Torres LP, et al. Pre-operative factors associated with increased mortality in elderly patients with a hip fracture: a cohort study in a developing country[J]. Volume 49. Injury; 2018. pp. 1162–8. 6.
Daugaard CL, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, van der Mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83(6):609–13.
Pugely AJ, Martin CT, Gao Y, Klocke NF, Callaghan JJ, Marsh JL. A risk calculator for short-term morbidity and mortality after hip fracture surgery. J Orthop Trauma. 2014;28(2):63–9.
Smektala R, Endres HG, Dasch B, Maier C, Trampisch HJ, Bonnaire F, et al. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord. 2008;9:171.
Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ. Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma. 2005;19(1):29–35.
Buecking B, Eschbach D, Koutras C, Kratz T, Balzer-Geldsetzer M, Dodel R, et al. Re-admission to Level 2 unit after hip-fracture surgery - risk factors, reasons and outcome. Injury. 2013;44(12):1919–25.
von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg AH, Woolf AD, et al. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int. 2016;27(10):2945–53.
Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007;17(7):514–9.
de Luise C, Brimacombe M, Pedersen L, Sørensen HT. Chronic obstructive pulmonary disease and mortality following hip fracture: a population-based cohort study. Eur J Epidemiol. 2008;23(2):115–22.
Ftouh S, Morga A, Swift C, Guideline Development Group. Management of hip fracture in adults: summary of NICE guidance. BMJ. 2011;342:d3304.
Roberts KC, Brox WT, AAOS Clinical Practice Guideline. Management of hip fractures in the Elderly. J Am Acad Orthop Surg. 2015;23(2):138–40.
Muhm M, Arend G, Ruffing T, Winkler H. Mortality and quality of life after proximal femur fracture-effect of time until surgery and reasons for delay. Eur J Trauma Emerg Surg. 2013;39(3):267–75.
Acknowledgements
Not applicable.
Funding
This study was funded by the Innovation & Transfer Fund of Peking University Third Hospital (BYSYZHKC2021106).
Author information
Authors and Affiliations
Contributions
FZ designed the study. YH and RW were responsible for the data collection and analysis and wrote the manuscript. ZZ, HJ, YT and YG were responsible for the data collection and analysis. ZC, YL, ZY and GH were responsible for follow-up. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Peking University Third Hospital. Written informed consent was obtained from all the participants included in the manuscript.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hao, Y., Wang, R., Chen, Z. et al. One-year mortality risk in older individuals with femoral intertrochanteric fracture: a tertiary center in China. BMC Geriatr 24, 544 (2024). https://doi.org/10.1186/s12877-024-05159-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05159-y