Abstract
Background
Mounting evidence suggests that vitamin D deficiency is associated with a higher risk of many chronic non-skeletal, age-associated diseases as well as mortality.
Aim
To determine, in older patients aged ≥ 80, the prevalence of vitamin D deficiency and its association with comorbidity, laboratory tests, length of stay and mortality within one year from blood withdrawal on admission to acute geriatrics ward.
Methods
We retrospectively surveyed electronic hospital health records of 830 older patients. The recorded data included patient demographics (e.g., age, sex, stay duration, readmissions number, death within one year from blood withdrawal on admission), medical diagnoses, laboratory results, including 25-hydroxyvitamin D [25(OH)D], and medications. We compared the characteristics of the patients who survived to those who died within one year.
Results
On admission, in 53.6% patients, vitamin D levels were lower than 50 nmol/L, and in 32%, the levels were ≤ 35 nmol/L. Persons who died were likely to be older, of male sex, were likely to be admitted for pneumonia or CHF, were likely to have lower level of albumin or hemoglobin, lower level of vitamin D or higher vitamin B12 and higher level of creatinine, were also likely to have had a lengthier hospitalization stay, a greater number of hospitalizations in the last year, a higher number of comorbidities, to have consumption of ≥5 drugs or likely to being treated with insulin, diuretics, antipsychotics, anticoagulants or benzodiazepines. Higher age, male sex, on-admission CHF, higher number of drugs, lower albumin, higher vitamin B12, vitamin D < 50 nmol/L, and consumption of antipsychotics and anticoagulants – were predictors of mortality.
Conclusion
Hypovitaminosis D is predictive of mortality in older patients within one year from hospitalization in the acute geriatric ward, but a causal relationship cannot be deduced. Nevertheless, older patients in acute care settings, because of their health vulnerability, should be considered for vitamin D testing. In the acutely ill patients, early intervention with vitamin D might improve outcomes. Accurate evaluation of mortality predictors in this age group patients may be more challenging and require variables that were not included in our study.
Similar content being viewed by others
Background
Vitamin D is an essential nutrient and a pro-hormone that regulates and mediates many physiologic processes, including bone metabolism, calcium homeostasis, extra-skeletal metabolism, cardiovascular homeostasis as well as immune functions [1,2,3,4]. Low serum vitamin D levels are frequent in older adults [5]. A combination of inadequate exposure to solar radiation and less than optimal dietary intake results in vitamin D deficiency [6].
Hypovitaminosis D reduces formation of the active form of vitamin D (1,25-dihydroxyvitamin D) at the tissue level [7]. The vitamin D receptor is found in most body tissues, and 1,25-dihydroxyvitamin D has a diverse array of biological functions ranging from anti-proliferative and anti-angiogenic effects to modulation of the immune system [4, 8]. This may be critical in mediating the beneficial pleiotropic functions of vitamin D, involving innate immunity, mucosal barrier, and endothelial function [7].
Vitamin D deficiency has been related to inflammation and immune dysfunction, which may be the potential reason for the increased susceptibility of the individual to severe infection [2]. In hospitalized very old subjects, lower levels of serum 25-hydroxy vitamin D [25(OH)D] are associated with a higher comorbidity burden [9]. Since there are vitamin D receptors in most tissues and cells in the body [10], mounting evidence suggests that vitamin D deficiency is associated with a higher risk of many chronic non-skeletal, age-associated diseases, including cancer, heart disease, diabetes mellitus, cognitive dysfunction, and dementia [1] as well as mortality [4, 6, 11, 12]. Some studies have also found an association between lower levels of vitamin D and frailty [5].
A multitude of association studies and meta-analyses have demonstrated the potential protective effects of vitamin D in reducing risk of cardiometabolic disorders, several types of cancers, autoimmune disorders, all-cause mortality, and other acute and chronic illnesses [13] An inverse association was observed between 25(OH)D and cardiovascular diseases, infections, glucose metabolism, cognitive disorders, and all-cause mortality [14]. Whether 25(OH)D is a marker of organ diseases is still under debate [9]. Though epidemiological evidence suggests that vitamin D deficiency is associated with increased mortality [12], the evidence is inconclusive, and the possible pathways remain unresolved [8]. Also, it is unclear if there are specific causes of death for which vitamin D might be important [12]. In addition, it is unclear whether low vitamin D levels independently contribute to mortality [15].
Our study aimed to determine, in older patients aged ≥ 80, the prevalence of vitamin D deficiency and its association with comorbidity, laboratory tests, length of stay and mortality within one year from blood withdrawal on admission to the acute geriatric ward.
Methods
Participants, design and procedures
We retrospectively surveyed electronic hospital health records of 830 older patients, aged ≥ 80 years, admitted between January 2015 and December 2017 from the emergency room to the acute Geriatrics Department at Kaplan Medical Center (a large community-based general hospital), Rehovot, Israel.
The recorded data included patient demographics (e.g., age, sex, stay duration, readmissions number, death within one year from blood withdrawal on admission), medical diagnoses, laboratory results, including 25-hydroxyvitamin D [25(OH)D], and medications. We retrieved the following data: admission diagnoses as well as comorbidities, including pneumonia, ischaemic heart disease (IHD), congestive heart failure (CHF), cerebrovascular accident (CVA), atrial fibrillation (AF), acute renal failure (ARF), diabetes mellitus, chronic renal failure (CRF), chronic obstructive pulmonary disease (COPD), dementia, obesity, malignancy, and falls. The drug types we retrieved were: statins, β-blockers, benzodiazepines, antipsychotics, antiplatelets, anticoagulants, insulin, antidiabetics, and proton pump inhibitors (PPI). We compared the characteristics of the patients who survived to those who died within one year from blood withdrawal on admission.
The study was approved by the Institutional Ethics Committee of the Kaplan Medical Center, Rehovot, Israel.
Statistics
Statistical analysis was performed, using JMP 17.0 Pro software (SAS Institute Inc., Cary, NC). Patients who survived were compared to those who died within one year from on-admission blood withdrawal, for categorical and continuous characteristics. Univariate significance was established by Chi-Square tests for categorical characteristics and by t-tests for continuous characteristics. Variables with univariate significance of 0.10 or less were used for a stepwise logistic regression model using alpha = 0.10 to enter the model and alpha = 0.05 to leave the model. After employing this criterion, the association between the remaining variables and death were used in a multiple logistic regression model. Results are presented as odds ratios with 95% confidence limits and significance from the possibility OR = 1.
Results
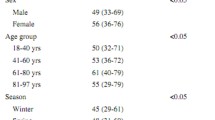
The mean age of the study population was 87.50 ± 4.87 years (range 80–112). Selected characteristics of the 830 older study subjects (61.4% females), divided according to vitamin D levels, are presented in Table 1. On admission, in 445 (53.6%) out of the 830 study subjects, vitamin D levels were lower than 50 nmol/L, and in 268 (32%) of the study subjects the levels were ≤ 35 nmol/L, 39% of the patients had low serum albumin, about 84% consumed ≥ 5 drugs, and about 52% consumed ≥ 10 drugs. Approximately 21% of the studied population were supplemented with vitamin D.
Within one year, 164 persons (19.8%) died, of whom 49.4% were women (Table 2). Compared with persons who survived, persons who died were likely to be older, of male sex, were likely to be admitted for pneumonia or CHF, were likely to have lower level of albumin or hemoglobin, lower level of vitamin D or higher vitamin B12 and higher level of creatinine, were also likely to have had a lengthier hospitalization stay, a greater number of hospitalizations in the last year, a higher number of comorbidities, to have consumption of ≥5 drugs or likely to be treated with insulin, diuretics, antipsychotics, anticoagulants or benzodiazepines. Mortality within one year from on-admission blood withdrawal, was higher among patients with low albumin levels as well as patients with lower vitamin D and lower or higher vitamin B12 levels.
According to multiple logistic regression analysis (Table 3), the independent variables – higher age, higher number of drugs, lower level of albumin, higher level of vitamin B12, vitamin D < 50 nmol/L, male sex, antipsychotics, anticoagulants, and on-admission diagnosed CHF – were predictors of mortality within one year. The significant mortality predictors, found in the study, explain about 21% of the possible predictors of mortality within one year from on-admission blood withdrawal.
Discussion
Our study deals with older adults ≥ 80 years old. We studied the risk factors of mortality within one year from blood withdrawal on admission to the acute geriatric ward. A higher percentage of men than women died, quite similarly to the findings of some other studies [16,17,18] and in contrast to other studies [19, 20]. Higher age was an independent risk factor of mortality. The risk of death was higher by about 5% in older subjects, although surprisingly, the mean age of the older adults, who survived was higher (93.13 ± 3.06) than that of those who died (87.96 ± 5.77). It can be explained by a higher proportion of women among the survivals (52% vs. 29%) in whom life expectancy is higher.
In our study, on-admission serum 25(OH)D levels below 50 nmol/L, were determined in 53.6% of the study population. Serum 25(OH)D is generally accepted as first choice measurement of vitamin D status, and it is used to classify vitamin D. The Endocrine Society Guidelines classify 25(OH)D levels below 50 nmol/L as deficient and levels of 75 nmol/L as sufficient, whereas the Institute of Medicine (IOM) suggested vitamin D deficiency to be indicated by 25(OH)D levels below 30 nmol/L and a level of 50 nmol/L to be sufficient [8].
Hypovitaminosis D is frequent in older subjects, ranging in occurrence from 50 to 90%, depending on the definition used and the setting [9]. Studies conducted in Australia revealed a higher risk of vitamin D deficiency in older people, who were hospitalized or residing in residential facilities [5].
Vitamin D is essential for bone mineralization, but a growing body of evidence points at a broader role [4, 8]. Vitamin D receptors are ubiquitous in the human body, and while the endocrine effects of vitamin D are well recognized, less appreciated are the autocrine and paracrine effects (antimicrobial and immunomodulatory) [6].
In hospitalized very old subjects, a higher comorbidity burden is associated with lower 25(OH)D serum levels [9]. Vitamin D deficiency has been found to be associated with mortality, and several diseases ranging from cardiovascular disease to autoimmune diseases and liver diseases [6, 8]. However, it is unclear whether this is explained by reverse causation, and if there are specific causes of death for which vitamin D might be important [12].
Despite an upsurge in medical research, the literature on determinants of survival in geriatric inpatients is scarce. Most of the studies, dealing with vitamin deficiency and its association with morbidity and mortality, have been conducted in older adults living in the community. In our study, vitamin D insufficiency (levels of < 50 nmol/L) was an independent risk factor of mortality, and increased mortality risk by 2.28. A retrospective study by Dudenkov et al. [14] reported a statistically significant inverse relationship between serum 25(OH)D levels and mortality in 11,022 white and nonwhite community patients registered in the Rochester Epidemiology Project. In an observational study of osteoporotic women aged 75 and older, 25(OH)D levels of less than 50 nmol/L were associated with greater all-cause mortality for up to 10 years. In that study, in women with vitamin D levels < 50 nmol/L, mortality risk in the low category was almost doubled twice than the high category, and remained higher even after adjustment for smoking and comorbidities, and was highest when additionally adjusted for osteoporosis, HR = 2.1 [15]. In a prospective cohort study of Australians older men, the risk of death was greater in those with vitamin D levels < 50 nmol/L than in those with a serum 25(OH)D level of 75 nmol/L or greater (adjusted HR = 1.42). In that study hypovitaminosis D is an independent predictor of all-cause mortality, regardless of frailty status or other comorbidities. The association between vitamin D and mortality is not solely dependent on the occurrence of frailty. Vitamin D may be a contributor in the development of frailty, but frailty is unlikely to play a major role in the association between vitamin D and all-cause mortality [5].
Very few studies have demonstrated the interaction between serum 25(OH)D and frailty in their association with mortality, and they were conducted in older adults in the community. One possible explanation for the relationship between serum 25(OH)D and frailty in their association with mortality is the fact that older adults are more likely to suffer from frailty, which increases their risk of falling, which in turn, might mediate between vitamin D deficiency and death. Since the study was performed in the oldest old patents, we presume that many of the study patients were frail. But no statement can be made about the frailty of these patients because no indicative data on frailty was found in the electronic hospital health records. A clear independent relationship between vitamin D status with frailty and mortality has yet to be established [5], through further future studies.
There are few studies on severely ill and hospitalized patients with malnutrition – a condition that puts patients at particular risk for adverse clinical outcomes. Vitamin D deficiency is highly prevalent in the population of malnourished inpatients and is negatively associated with mortality [21]. In a study in critically ill patients, a longer survival was observed in vitamin D sufficient patients [22]. A systematic review and meta-analysis, which investigated effects of vitamin D deficiency on adverse medical outcomes across different medical inpatient populations, found a stepwise increase in mortality of 3.4%, 5.6%, and 8.7% in patients with vitamin D sufficiency, insufficiency (25 to 50 nmol/L), and severe deficiency, respectively, and vitamin D deficiency increased 30-day mortality by 1.70 for vitamin D insufficient levels compared to sufficient levels (Vit D ≥ 50 nmol/L) [23]. In a prospective cohort Swiss study, inpatients with vitamin D levels, had an increased 180-day mortality rate of 29.9% compared to 23.1% in patients with no deficiency, and vitamin D deficiency increased mortality risk by 1.42 [21]. A comparison between mortality in deficient/insufficient subjects and in those with no deficiency emphasizes the importance of vitamin D in reducing mortality in the oldest old adults.
In the present study, additional factors were independent risk factors of mortality.
Hypoalbuminemia is a prognostic risk factor of mortality among older adults [10, 24]. Low levels of albumin are associated with worse recovery following acute pathologies [25]. Higher albumin levels, in our study, had a protective effect, correspondingly to other studies [24, 26]. Serum albumin plays a vital physiologic role in health maintenance for many organs. Hypoalbuminemia might be an indicator of malnutrition, which explains the bad prognosis [24, 27]. Hypoalbuminemia, in the present study, was associated with lower serum vitamin D levels, deficiencies that might eventually deteriorate to death, especially when being independent risk factors of mortality. Concomitant conditions of hypoalbuminemia and lower vitamin D levels may prompt to look for a high-risk group of geriatric patients, who could be targeted for more careful and closer follow-up and intervention for an extended time.
In our study, a higher rate of older adults with on-admission CHF died, and the risk of mortality among them was higher by about 1.9. In a study in hospitalized patients aged ≥ 80 years with acute myocardial infarction, on-admission left ventricular ejection fraction < 40% predicted 1-year mortality [28]. Comorbid CHF in patients aged ≥ 90 hospitalized in acute geriatric ward, was an independent risk factor of in-hospital mortality [29].
In the present study, a higher proportion of older adults with high vitamin B12 levels died, and high vitamin B12 level was a significant predictor of mortality. In many studies performed on the aged, the focus is usually on detecting vitamin B12 deficiency [30]. In contrast, less is known about the meaning of high vitamin B12 levels. High vitamin B12 levels, as a predictor of increased mortality in malignancies and liver disease, have been already documented [31, 32]. Likewise in our study, in several studies, high vitamin B12 levels, in older patients suffering from acute and chronic diseases except for malignancy, were associated with higher mortality [33,34,35,36,37,38,39].
Older people are prescribed a greater number of medications which may be inappropriate, fueling the cycle of comorbidity, disability, hospitalization, nursing home placement, and mortality [40]. In the present study, a higher percentage of older adults, who consumed ≥ 5 drugs, died, and a higher number of drugs consumed was found to be an independent risk factor of mortality.
In our study, the risk of mortality, in subjects who consumed antipsychotics, was higher by slightly more than twice. Antipsychotic use was an independent risk factor of mortality, correspondingly to Tal’s finding found in oldest old patients within one year after discharge from acute geriatric ward [41]. Also, in some other studies antipsychotics consumption enhanced mortality [42, 43]. Antipsychotic medications are used to treat and manage symptoms of many psychiatric disorders [44]. There are several likely mechanisms by which antipsychotics may increase the risk of death. Antipsychotics may prolong the QT interval, predisposing patients to arrhythmias and sudden cardiac death. Additionally, sedation and accelerated cognitive decline, caused by antipsychotics, may increase the risk of aspiration and choking, especially in patients with dementia [45].
In our study, a higher percentage of subjects, treated with anticoagulants, died, and anticoagulant treatment increased the risk of mortality by about 2.6. Although it was shown in several studies, that anticoagulant therapy clearly outweighs the risk of heavy bleeding, even in the older adults [46,47,48], the clinician should probably consider treating with caution older patients with many comorbidities, including falls.
Our study has all the disadvantages of a retrospective observational study. We did not have all the details that may have been influencing mortality in the older adults within one year after on-admission blood withdrawal, because they were not found in the patients’ electronic data. Consequently, the significant independent variables (age, male sex, number of drugs, on-admission CHF, low albumin, vitamin B12, vitamin D < 50, antipsychotics or anticoagulants use) comprise only part of mortality predictors. Some other unknown variables might explain the remainder.
Our study strength lies in its sample’s relatively large size. Since the study focuses on mortality predictors in the ≥ 80-year adults within one year from on-admission blood withdrawal, we would like to point out that we have contributed to the medical knowledge concerning this population of older adults, whose proportion in the geriatric population is recently significantly increasing.
Conclusion
Hypovitaminosis D is predictive of mortality in patients within one year from hospitalization in the acute geriatric ward. Although we have shown a significant association between the vitamin level and mortality, a causal relationship cannot be deduced. Nevertheless, older patients hospitalized in acute care settings, because of their health vulnerability, should be considered for vitamin D testing. In the acutely ill patients, early intervention with vitamin D might improve outcomes. Accurate evaluation of mortality predictors in this age group patients may be more challenging and require variables that were not included in our study. Future research is warranted.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 25(OH)D:
-
25-hydroxyvitamin D
- IHD:
-
Ischaemic heart disease
- CHF:
-
Congestive heart failure
- CVA:
-
Cerebrovascular accident
- AF:
-
Atrial fibrillation
- ARF:
-
Acute renal failure
- CRF:
-
Chronic renal failure
- COPD:
-
Chronic obstructive pulmonary disease
- PPI:
-
Proton pump inhibitors
- OR:
-
Odds Ratio
- HR:
-
Hazard Ratio
References
Wang Y, Wang Y, Zhang B, Lin Y, Tan S, Lu Z. Depressed serum 25-hydroxyvitamin D levels increase hospital stay and alter glucose homeostasis in first-ever ischemic stroke. Curr Neurovasc Res. 2019;16(4):340–7. https://doi.org/10.2174/1567202616666190924161947.
Li Y, Ding S. Serum 25-Hydroxyvitamin D and the risk of mortality in adult patients with Sepsis: a meta-analysis. BMC Infect Dis. 2020;20(1):189. https://doi.org/10.1186/s12879-020-4879-1.
Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020;12(7):2097. https://doi.org/10.3390/nu12072097.
Cherniack EP, Florez H, Roos BA, Troen BR, Levis S. Hypovitaminosis D in the elderly: from bone to brain. J Nutr Health Aging. 2008;12(6):366–73. https://doi.org/10.1007/BF02982668.
Wong YY, McCaul KA, Yeap BB, Hankey GJ, Flicker L. Low vitamin D status is an independent predictor of increased frailty and all-cause mortality in older men: the Health in men Study. J Clin Endocrinol Metab. 2013;98(9):3821–8. https://doi.org/10.1210/jc.2013-1702.
Youssef DA, El Abbassi AM, Cutchins DC, Chhabra S, Peiris AN. Vitamin D deficiency: implications for acute care in the elderly and in patients with chronic illness. Geriatr Gerontol Int. 2011;11(4):395–407. https://doi.org/10.1111/j.1447-0594.2011.00716.x.
de Haan K, Groeneveld AB, de Geus HR, Egal M, Struijs A. Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: systematic review and meta-analysis. Crit Care. 2014;18(6):660. https://doi.org/10.1186/s13054-014-0660-4.
Skaaby T. The relationship of vitamin D status to risk of cardiovascular disease and mortality. Dan Med J. 2015;62(2):B5008.
Boccardi V, Lapenna M, Gaggi L, Garaffa FM, Croce MF, Baroni M, Ercolani S, Mecocci P, Ruggiero C, Hypovitaminosis D. Hypovitaminosis D: a disease marker in hospitalized very old persons at risk of malnutrition. Nutrients. 2019;11(1):128. https://doi.org/10.3390/nu11010128.
Aronen M, Viikari L, Langen H, Kohonen I, Wuorela M, Vuorinen T, Söderlund-Venermo M, Viitanen M, Camargo CA Jr, Vahlberg T, Jartti T. The long-term prognostic value of serum 25(OH)D, albumin, and LL-37 levels in acute respiratory diseases among older adults. BMC Geriatr. 2022;22(1):146. https://doi.org/10.1186/s12877-022-02836-8.
Gaksch M, Jorde R, Grimnes G, Joakimsen R, Schirmer H, Wilsgaard T, Mathiesen EB, Njølstad I, Løchen ML, März W, Kleber ME, Tomaschitz A, Grübler M, Eiriksdottir G, Gudmundsson EF, Harris TB, Cotch MF, Aspelund T, Gudnason V, Rutters F, Beulens JW, van ‘t Riet E, Nijpels G, Dekker JM, Grove-Laugesen D, Rejnmark L, Busch MA, Mensink GB, Scheidt-Nave C, Thamm M, Swart KM, Brouwer IA, Lips P, van Schoor NM, Sempos CT, Durazo-Arvizu RA, Škrabáková Z, Dowling KG, Cashman KD, Kiely M, Pilz S. Vitamin D and mortality: individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium. PLoS ONE. 2017;12(2):e0170791. https://doi.org/10.1371/journal.pone.0170791.
Heath AK, Kim IY, Hodge AM, English DR, Muller DC. Vitamin D status and mortality: a systematic review of observational studies. Int J Environ Res Public Health. 2019;29(3):16. https://doi.org/10.3390/ijerph16030383.
Charoenngam N, Shirvani A, Holick MF. The ongoing D-lemma of vitamin D supplementation for nonskeletal health and bone health. Curr Opin Endocrinol Diabetes Obes. 2019;26(6):301–5. https://doi.org/10.1097/MED.0000000000000508.
Dudenkov DV, Mara KC, Petterson TM, Maxson JA, Thacher TD. Serum 25-hydroxyvitamin D values and risk of all-cause and cause-specific mortality: a population-based cohort study. Mayo Clin Proc. 2018;93(6):721–30. https://doi.org/10.1016/j.mayocp.2018.03.006.
Buchebner D, McGuigan F, Gerdhem P, Ridderstråle M, Akesson K. Association between hypovitaminosis d in elderly women and long- and short-term mortality-results from the osteoporotic prospective risk Assessment Cohort. J Am Geriatr Soc. 2016;64(5):990–7. https://doi.org/10.1111/jgs.14087.
Barba R, Martínez JM, Zapatero A, Plaza S, Losa JE, Canora J, Pérez A, García de Casasola G. Mortality and complications in very old patients (90+) admitted to departments of internal medicine in Spain. Eur J Intern Med. 2011;22(1):49–52. https://doi.org/10.1016/j.ejim.2010.11.001.
Ponzetto M, Maero B, Maina P, Rosato R, Ciccone G, Merletti F, Rubenstein LZ, Fabris F. Risk factors for early and late mortality in hospitalized older patients: the continuing importance of functional status. J Gerontol Biol Sci Med Sci. 2003;58(11):1049–54. https://doi.org/10.1093/gerona/58.11.m1049.
Rozzini R, Sleiman I, Maggi S, Noale M, Trabucchi M. Gender differences and health status in old and very old patients. Am Med Dir Assoc. 2009;10(8):554–8. https://doi.org/10.1016/j.jamda.2009.04.005.
Hwang LC, Hsu CP, Tjung JJ, Shih SC, Lin CH, Huang TH. Predictors of in-hospital mortality in oldest-old patients in Taiwan. Inter J Gerontol. 2013;7(1):22–6. https://doi.org/10.1016/j.ijge.2012.07.005.
Takahashi M, Okawa K, Morimoto T, Tsushima R, Sudo Y, Sakamoto A, Sogo M, Ozaki M, Doi M, Morita H, Okumura K, Ito H. Impact of direct oral anticoagulant use on mortality in very old patients with non-valvular atrial fibrillation. Age Ageing. 2022;51(7):afac146. https://doi.org/10.1093/ageing/afac146.
Merker M, Amsler A, Pereira R, Bolliger R, Tribolet P, Braun N, Hoess C, Pavlicek V, Bilz S, Sigrist S, Brändle M, Henzen C, Thomann R, Rutishauser J, Aujesky D, Rodondi N, Donzé J, Stanga Z, Mueller B, Schuetz P. Vitamin D deficiency is highly prevalent in malnourished inpatients and associated with higher mortality: a prospective cohort study. Med (Baltim). 2019;98(48):e18113. https://doi.org/10.1097/MD.0000000000018113.
Arnson Y, Gringauz I, Itzhaky D, Amital H. Vitamin D deficiency is associated with poor outcomes and increased mortality in severely ill patients. QJM. 2012;105(7):633–9. https://doi.org/10.1093/qjmed/hcs014.
Graedel L, Merker M, Felder S, Kutz A, Haubitz S, Faessler L, Kaeslin M, Huber A, Mueller B, Schuetz P. Vitamin D Deficiency strongly predicts adverse medical outcome across different medical inpatient populations: results from a prospective study. Med (Baltim). 2016;95(19):e3533. https://doi.org/10.1097/MD.0000000000003533.
Abe S. Prognostic factors for the survival of elderly patients who were hospitalized in the medical ward of our hospital in Japan. Geriatr (Basel). 2017;2(4):32. https://doi.org/10.3390/geriatrics2040032.
Cabrerizo S, Cuadras D, Gomez-Busto F, Artaza-Artabe I, Marín-Ciancas F. Malafarina Vm serum albumin and health in older people: review and meta analysis. Maturitas. 2015;81(1):17–27. https://doi.org/10.1016/j.maturitas.2015.02.009.
Corona LP, de Oliveira Duarte YA, Lebrão ML. Markers of nutritional status and mortality in older adults: the role of anemia and hypoalbuminemia. Geriatr Gerontol Int. 2018;18(1):177–82. https://doi.org/10.1111/ggi.13137.
Yildiz A, Yigit A, Benli AR. The impact of nutritional status and complete blood count parameters on clinical outcome in geriatric critically ill patients. J Clin Med Res. 2018;10(7):588–92. https://doi.org/10.14740/jocmr3461w.
Căruntu F, Bordejevic DA, Buz B, Gheorghiu A, Tomescu MC. Independent predictors of in-hospital and 1-year mortality rates in octogenarians with acute myocardial infarction. Rev Cardiovasc Med. 2021;22(2):489–97. https://doi.org/10.31083/j.rcm2202056.
Tal S. Mortality predictors in the Oldest-Old in an Acute Geriatric Ward. Isr Med Assoc J. 2022;24(10):638–42.
Dali-Youcef N, Andrès E. An update on cobalamin deficiency in adults. QJM. 2009;102(1):17–28. https://doi.org/10.1093/qjmed/hcn138.
Arendt JF, Pedersen L, Nexo E, Sørensen HT. Elevated plasma vitamin B12 levels as a marker for cancer: a population-based cohort study. J Nat Cancer Inst. 2013;105(23):1799–805. https://doi.org/10.1093/jnci/djt315.
Lin CY, Kuo CS, Lu CL, Wu MY, Huang RF. Elevated serum vitamin B(12) levels in association with tumor markers as the prognostic factors predictive for poor survival in patients with hepatocellular carcinoma. Nutr Cancer. 2010;62(2):190–7. https://doi.org/10.1080/01635580903305334.
Flores-Guerrero JL, Minovic I, Groothof D, Gruppen EG, Riphagen IJ, Kootstra-Ros J, Muller Kobold A, Hak E, Navis G, Gansevoort RT, de Borst MH, Dullaart RPF, Bakker SJL. Association of plasma concentration of vitamin B12 with all-cause mortality in the general population in the Netherlands. JAMA Netw Open. 2020;3(1):e1919274. https://doi.org/10.1001/jamanetworkopen.2019.19274.
Salles N, Herrmann F, Sakbani K, Rapin CH, Sieber C. High vitamin B12 level: a strong predictor of mortality in elderly inpatients. J Am Geriatr Soc. 2005;53(5):917–8. https://doi.org/10.1111/j.1532-5415.2005.53278_7.x.
Salles N, Herrmann F, Sieber C, Rapin C. High vitamin B12 level and mortality in elderly inpatients. J Nutr Health Aging. 2008;12(3):219–21. https://doi.org/10.1007/BF02982624.
Shahar A, Feiglin L, Shahar DR, Levy S, Seligsohn U. High prevalence and impact of subnormal serum vitamin B12 levels in Israeli elders admitted to a geriatric hospital. J Nutr Health Aging. 2001;5(2):124–7.
Tal S, Shavit Y, Stern F, Malnick S. Association between vitamin B12 levels and mortality in hospitalized older adults. J Am Geriatr Soc. 2010;58(3):523–6. https://doi.org/10.1111/j.1532-5415.2010.02721.x. Epub 2010 Feb 11.
Wolffenbuttel BHR, Heiner-Fokkema MR, Green R, Gans ROB. Relationship between serum B12 concentrations and mortality: experience in NHANES. BMC Med. 2020;18(1):307. https://doi.org/10.1186/s12916-020-01771-y.
Zeitlin A, Frishman WH, Chang CJ. The association of vitamin b 12 and folate blood levels with mortality and cardiovascular morbidity incidence in the old old: the Bronx aging study. Am J Ther. 1997;4(7–8):275–81. https://doi.org/10.1097/00045391-199707000-00008.
Bilek AJ, Levy Y, Kab H, Andreev P, Garfinkel D. Teaching physicians the GPGP method promotes deprescribing in both inpatient and outpatient settings. Ther Adv Drug Saf. 2019;27:10:2042098619895914. https://doi.org/10.1177/2042098619895914.
Tal S. Mortality in the oldest-old adults after Discharge from Acute Geriatric Ward. Gerontol Geriatr Med. 2023;9:23337214231156300. https://doi.org/10.1177/23337214231156300.
Bień B, Bień-Barkowska K, Wojskowicz A, Kasiukiewicz A, Wojszel ZB. Prognostic factors of long-term survival in geriatric inpatients. Should we change the recommendations for the oldest people? J Nutr Health Aging. 2015;19(4):481–8. https://doi.org/10.1007/s12603-014-0570-9.
Musicco M, Palmer K, Russo A, Caltagirone C, Adorni F, Pettenati C, Bisanti L. Association between prescription of conventional or atypical antipsychotic drugs and mortality in older persons with Alzheimer’s disease. Dement Geriatr Cogn Disord. 2011;31(3):218–24. https://doi.org/10.1159/000326213.
Ameer MA, Saadabadi A, Neuroleptic Medications. [Updated 2021 Dec 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK459150/.
Gurevich A, Guller V, Berner YN, Tal S. Are atypical antipsychotics safer than typical antipsychotics for treating behavioral and psychological symptoms of dementia? J Nutr Health Aging. 2012;16(6):557–61. https://doi.org/10.1007/s12603-012-0057-5.
Blacher J, Sorbets E, Guedj Meynier D, Huberman JP, Gauthier J, Cohen S, Hoffman O. Determinants of antithrombotic treatment for atrial fibrillation in octogenarians: results of the OCTOFA Study. Clin Drug Investig. 2019;39(9):891–8. https://doi.org/10.1007/s40261-019-00809-1.
Melkonian M, Jarzebowski W, Pautas E, Siguret V, Belmin J, Lafuente-Lafuente C. Bleeding risk of antiplatelet drugs compared with oral anticoagulants in older patients with atrial fibrillation: a systematic review and meta-analysis. J Thromb Haemost. 2017;15(7):1500–10. https://doi.org/10.1111/jth.13697.
Volgman AS, Nair G, Lyubarova R, Merchant FM, Mason P, Curtis AB, Wenger NK, Aggarwal NT, Kirkpatrick JN, Benjamin EJ. Management of Atrial Fibrillation in patients 75 years and older: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(2):166–79. https://doi.org/10.1016/j.jacc.2021.10.037. Erratum in: J Am Coll Cardiol. 2022;79(19):1967. https://doi.org/10.1016/j.jacc.2022.03.362.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Sari Tal and Felicia Stern contributed to study design, drafting, revision and finalization of the manuscript. Nadav Abel contributed to study data collection and study design.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Ethics Committee of the Kaplan Medical Center, Rehovot, Israel. Written informed consent was waived by the Kaplan Medical Center Ethics committee, since the study was performed on data retrospectively retrieved from the electronic hospital health records.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abel, N., Stern, F. & Tal, S. On-admission serum 25(OH)D level and mortality within one year in older patients. BMC Geriatr 24, 664 (2024). https://doi.org/10.1186/s12877-024-05166-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05166-z