Abstract
Background
Family caregivers of persons with dementia are faced with complex caregiving management needs. This study had two aims: (1) to identify caregiving management needs of family caregivers of persons with dementia and (2) identify any variables that might influence these needs.
Methods
This cross-sectional study recruited family caregivers of persons with dementia (N = 250) through referrals from clinicians at a dementia outpatient clinic in Northern Taiwan. Data were collected with a 32-item researcher-developed instrument, the Caregiving Management Needs Scale (CMNS), to identify management needs specific to family caregivers of persons with dementia. The CMNS was comprised of questions about the types of assistance or support family caregivers would like to receive to facilitate caregiving.
Results
CMNS scores indicated caregivers had moderate management needs. Caregivers of relatives with a moderate severity of dementia had significantly higher scores on the CMNS compared with caregivers of persons with very mild dementia (p < 0.01). Linear regression analysis indicated significant predictors of high caregiving management needs were caregivers who were female (p < 0.01), and persons with dementia with behavioral problems (p < 0.01), low scores for Activities of Daily Living (p < 0.01), regular medication adherence (p < 0.01), and use of long-term care services (p < 0.001) were significant (F[13, 236] = 7.12; p < 0.001; R2 = 28.2%).
Conclusions
Understanding variables and predictors of caregiving management needs for family caregivers could reduce the complexity of caregiving.
Trial Registration
ClinicalTrials.gov NCT05151185
Similar content being viewed by others
Background
The global prevalence of dementia is increasing especially for individuals over 65 years of age [1]. The proportion of Taiwan’s population aged ≥ 65 years is 18.02%, which is expected to enter the era of an ultra-aged society by 2025 [2]. This increase in the population of older adults underscores the urgency of addressing the challenges of caring for persons with dementia.
Family caregivers of persons with dementia invest more time in caregiving than their counterparts caring for individuals without dementia [3, 4] and also experience a greater caregiving burden compared with caregivers of individuals with other health conditions due to greater levels of stress [4, 5]. Stress results in perceptions of caregiving burden, which can affect caregivers’ social, emotional, and financial wellbeing [6]. Caregiver burden can be exacerbated by high levels of unmet caregiver needs, which result from the caregiver prioritizing the needs of the person with dementia over their own needs [7]. Therefore, identifying and understanding specific unmet needs is one means of reducing caregiver burden.
The disease trajectory of dementia, which includes an increase in cognitive decline over time, requires ongoing changes in caregiving management, which results in changes in caregiving management needs. Caregiving management needs for family caregivers of persons with dementia encompass the ability to obtain dementia-related information, including strategies for providing assistance with activities of daily living (ADLs), caregiving specific that addresses memory loss and behavioral changes [8], and the provision of timely and individualized information to enable them to access the appropriate support services [8,9,10]. However, one qualitative study reported that caregivers felt service providers did not fully comprehend the range of unmet needs, which impacted their ability to fulfill their caregiving responsibilities [11]. Another study suggested that surveys of caregivers’ unmet needs focused more on caregiver burden rather than assessing practical unmet caregiving management needs that could be addressed with targeted, individualized interventions [7].
Management of the needs of persons with dementia and their caregivers can be achieved immediately following a diagnosis of dementia by identifying a person to act as a case manager and provide long-term support. This allows for timely identification of care services, interventions, and support services specific the diagnosis of the person with dementia as well as the needs of the caregiver, which is not only applicable to individuals with early onset dementia [12], but also for older adults with mild to severe dementia [13]. Including case managers and specialists in dementia clinic can address complex needs of persons with dementia associated by the unpredictable trajectory of the disease progression and the long duration of the illness [13]. Throughout the illness trajectory, case managers can integrate necessary services that are needed not only by the person with dementia but also the caregiver [12,13,14]. However, studies identifying the caregiving management needs of family caregivers of persons with dementia are limited.
Caregiving for persons with dementia in Taiwan is primarily provided by family caregivers with adult children representing over 70% of these caregivers [15,16,17,18]. Thus, the National Ten-year Long-term Care Plan 2.0, initiated in 2017, involves home-based dementia care. Dementia care resources were expanded in 2018 by implementing the Integrated Dementia Care Center, which advocates for a community care service model for persons with dementia and their caregivers that is reinforced by professional case managers who are available to assist with navigating access to support services over the course of dementia. The anticipated goal is that by 2025, over 80% of persons with dementia will receive care management services, 40% will access long-term care services, and support will be provided for at least 70% of family caregivers of persons with dementia, which will significantly alleviate caregiver burden [19]. Therefore, assessing caregiving management needs and providing strategies to meet these needs could be incorporated into the long-term plan model for dementia care.
Survey questionnaires frequently used to assess the needs of family caregivers. The Carers’ Needs Assessment for Dementia (CNA-D) is a qualitative interview-based survey about 18 problem areas to identify unmet needs of caregivers in Germany. The CNA-D had concurrent validity with the Zarit Burden Inventory, indicating it was a reliable for assessing caregiver burden for caregivers of persons with dementia [20]. A second scale evaluates family caregivers’ competence, knowledge, and preparedness in caregiving for persons with dementia to assess “caregiver activation”, which does not generate a list of needs but identifies caregivers needs for education and caregiving behaviors to better participate in the care of their relative [21]. The assessment tool for Family Care Needs of Person with Dementia, developed for family caregivers of persons with dementia in Taiwan, focuses on physical and behavioral functions of the care receiver to evaluate the needs of the caregiver relative to the severity the caregiving burden and care resources that could reduce caregiving burden [22]. However, similar to the CAN-D and the assessment of “caregiver activation” this survey does not provide information about the specific needs, the level of these needs, or the desire for a care specialist to provide assistance. Thus, there is a gap in the literature on available assessment tools that comprehensively address caregiving management needs of family caregivers of persons with dementia [23].
Unmet needs are common among family caregivers of persons with dementia [24], however needs will not only differ with the severity of their relative’s cognitive impairment but for caregivers in Eastern countries such as Taiwan, cultural influences will also shape caregiving needs and how caregivers express them [8, 25, 26]. Therefore, this study aimed to expand the dementia care resources available through Taiwan’s Integrated Dementia Care Center, by evaluating the caregiving management needs of family caregivers of persons with dementia. To address the gap in the literature about specific caregiver needs as well as care management needs for family caregivers in Taiwan, we developed a survey questionnaire which not only evaluates family caregivers’ needs for educational information about dementia, caregiving strategies, and personal needs but also includes questions about care management needs, which distinguishes it from other survey instruments. The scores on the researcher-developed Care Management Needs Scale (CMNS) were used to determine the overall level of caregiving management needs and examine if any specific needs were associated with personal characteristics of the caregivers or demographic and clinical characteristics of the person with dementia. Identification of the caregiving management needs of these family caregivers and any predictor variables could serve as a reference for developing targeted support interventions for individualized, person-centered care for reducing caregiver burden.
Methods
Study design and participants
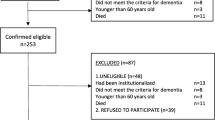
This cross-sectional study was conducted from August 2020 to January 2022 at dementia outpatient clinics in Northern Taiwan. Inclusion criteria for persons with dementia were as follows: (1) had received a score ≥ 0.5 on the Clinical Dementia Rating (CDR) scale by a neurologist [27] and (2) not residing in a long-term care institution or nursing home. Inclusion criteria for family caregivers were as follows: (1) age ≥ 20 years, (2) the family member who provided at least 5 h of daily caregiving and/or supervised the daily care provided by a hired caregiver and was designated as the decision-maker for medical care and treatment of the person with dementia, and (3) proficient in Mandarin or Taiwanese. The study was approved by the Chang Gung Medical Foundation Institutional Review Board (No.202000902B0). Written informed consent was obtained from caregivers prior to enrollment in the study.
Measures
Characteristics of caregivers and persons with dementia
Data were collected when the person with dementia was visiting the clinic at a time convenient for the family caregiver. Demographic and clinical characteristics for persons with dementia were collected from their medical charts and included age, gender, educational level, marital status, duration and type of dementia, and scores on the Mini-Mental State Examination (MMSE), CDR, Activities of Daily Living (ADL) [28], Instrumental Activities of Daily Living (IADL) [29], and comorbidities. The number of behavioral problems was obtained by providing caregivers with a list of common disruptive behaviors and asking them to check any that had frequently occurred in the past month; an open-ended question allowed them to add any behaviors not listed. We also provided caregivers with a list of resources for long-term care services for persons with dementia and ask them to check any that had been used in the last six months; an open-ended question allowed them to add any additional information.
Demographic and clinical characteristics of family caregivers were collected with a researcher-developed survey instrument, which included age, gender, educational level, marital status, relationship to care receiver, perceived current economic status (1 = very unsatisfied to 5 = very satisfied), perceived health status (1 = very poor to 5 = very good), caregiving duration (months), daily caregiving time (hours), and the use of hired foreign caregiving helpers.
Caregiving Management needs scale
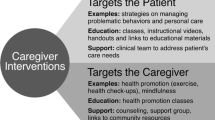
Caregiving management needs of family caregivers of persons with dementia were assessed with a researcher-developed Caregiving Management Needs Scale (CMNS). A total of 33 items about caregiving management needs were generated based on the literature regarding caregiving for persons with dementia [23,24,25], consultations with experts in dementia, and discussions with 10 family caregivers of persons with dementia. Each item is a question about what type of assistance the caregiver believes would facilitate better management of caregiving and would result in reduced stress experienced by trying to balance their personal needs and the needs of the person with dementia. The goal of the CMNS is to identify the most significant needs of family caregivers of persons with dementia, which can be used to create a whole-system model of dementia support that is readily accessible [13], which can reduce management needs and improve quality of life [14]. Questions focus on sources of assistance and needs such as a dementia specialist and improving communication with healthcare providers, such as, “Do you need a dementia specialist, such as a case manager, to facilitate communication between you and members of the healthcare team?” or a member of a dementia support service that can provide more information about dementia and caring for a person with dementia, such as, “Do you need someone to provide you with information about dementia, such as how the disease progresses and approaches to caregiving?”
Content validity of the 33 items was assessed by five experts in dementia care: a researcher, a nurse practitioner, a case manager, an occupational therapist and a social worker with more than 10 years of experience in the field. Each item was assessed for relevance using a 4-point Likert scale from 1 (not relevant) to 4 (extremely relevant). Mean scores for all items were ≥ 3, thus, all items were retained. The content validity index (CVI) was 0.98.
Principal component analysis resulted in a Kaiser-Meyer-Olkin index of 0.94 and Bartlett’s test of sphericity was significant (χ2 = 6925.31, df = 528, p < 0.001); indicating the scale was suitable for conducting factor analysis. Confirmatory factor analysis (CFA) examined construct validity of the 33-item CMNS [30] using data provided by 250 family caregivers. Maximum likelihood extraction with orthogonal varimax rotation was performed with factor extraction based on eigenvalues > 1 and factor loadings ≥ 0.4. CFA extracted six factors, which explained 71.33% of the total variance. One item was excluded (Item 6: “Do you need caregiving assistance during the daytime to provide you with a short break?”) due cross-factor loading (loading < 0.4), indicating it did not align with any of the factors. The six factors were labeled as follows: Individual Case Management Services (ICMS, 7 items); Immediate Information (I-Info, 8 items); Care Services (CS, 7 items); Anticipated Information (A-Info, 5 items); Psychological Support (PS, 3 items); and Referral and Tracking of Long-term Care Services (RTLCS, 2 items).
The scale was demonstrated to have good reliability and validity. Composite reliability (CR) for Factors 1–5 ranged from 0.702 to 0.880, CR for Factor 6 was 0.592. With the exception of Factor 4, Average Variance Extracted (AVE) ranged from 0.423 to 0.607; Factor 4 was 0.335, which is considered acceptable. Cronbach’s α for the total scale was 0.96; the six subscales ranged from 0.84 to 0.94, demonstrating good internal consistency. Details of the CFA are shown in Additional file 1.
Statistical analysis
Statistical analysis was performed using SPSS Software version 28 (SPSS Inc., Chicago, IL, USA). Descriptive statistics for characteristics of family caregivers and persons with dementia included frequency and percentage (n, %) for categorical variables; mean and standard deviation (SD) for continuous variables. All p values were two-tailed, with significance at p < 0.05. Characteristics among caregivers and persons with dementia were examined based on CDR scores for dementia severity of the care receiver: 0.5 = very mild; 1 = mild; 2 = moderate; and 3 = severe. Differences among caregivers and care receivers across care receivers grouped by dementia severity were examined with Chi-square test or one-way ANOVA with Bonferroni’s post hoc comparisons, or Fisher’s exact text. Differences in caregiving management needs for categorical characteristics of caregivers and care receivers were examined with independent samples t-test or one-way ANOVA with Bonferroni’s post hoc comparison; Spearman’s rank correlation coefficient examined continuous variables. Multiple linear regression analysis was conducted to identify predictors for high caregiving management needs as the dependent variable among family caregivers. Independent variables included marital status, dementia severity, MMSE score, medication adherence, number of behavioral problems, ADL and IADL scores, and utilization of long-term care services for care receivers and caregiver variables of gender and perceived economic and health status. Prior to linear regression analysis, the variance inflation factor (VIF) for each variable was calculated to examine if there was multicollinearity. A VIF > 10 indicates the existence of significant multicollinearity that needs to be corrected [31]. VIF values for our predictor variables in all regression analyses ranged from 1.034 to 3.080, indicating variables were moderately correlated and no correction was required.
Results
Characteristics of family caregivers and persons with dementia
Characteristics for all family caregivers, persons with dementia, and grouped by the severity of dementia of the care receiver are shown in Table 1. The mean age of caregivers was 56.22 years (SD = 11.01; range = 22–85 years), most were female (62.4%), and married (71.6%). Most caregivers lived with the person with dementia fulltime or on a rotating basis (82. 8%). The mean number of daily caregiving hours was 14.29 (SD = 9.23) and number of months of caregiving was 54.87 (SD = 41.03). The mean age of the persons with dementia was 80.75 years (SD = 8.09), most were female (65.6%), married (58.8%), and lived with their spouse or an adult child (91.2%). The mean duration of dementia was 58.20 months (SD = 43.26) and most had been diagnosed with Alzheimer’s disease (72.4%).
Caregivers and persons with dementia were grouped by dementia severity based on the CDR score of the care receiver. The four dementia severity groups were very mild (36.8%, n = 92), mild (37.6%, n = 94), and moderate (19.6%, n = 49) and severe (n = 15, 6.0%). When characteristics of caregiver groups were examined, there were no differences among groups for age, gender, marital or employment status, educational level, presence of chronic disease, or relationship to the care receiver. Significantly more caregivers lived with the care receiver for all levels of severity compared with those who did not (p < 0.05), caregivers of persons with very mild and mild dementia had a higher perceived economic status than caregivers of persons with moderate dementia severity (p < 0.01). The mean duration of caregiving differed between dementia severity groups (p < 0.001), with more months of caregiving for caregivers of persons with moderate or severe dementia, compared with those caring for persons with very mild dementia; and more months of caregiving for caregivers of persons with severe dementia compared with those caring for persons with mild dementia.
When persons with dementia were grouped by dementia severity, care receivers with moderate severity were significantly older than those with severe dementia (p < 0.01); more care receivers with very mild dementia lived with a spouse or adult child compared with care receivers with mild dementia (p < 0.05); and duration of dementia was greatest for care receivers with severe dementia (p < 0.001). Significantly more care receivers with severe dementia had no behavioral problems compared with care receivers with mild or moderate dementia; more care receivers with moderate dementia had ≥ 4 behavioral problems (46.9%) compared with very mild (22.8%) and severe (0%), and more care receivers with mild dementia had ≥ 4 behavioral problems compared with those with severe dementia (p < 0.001). Characteristics of comorbidities, ADL scores, IADL scores, and previous use of long-term care services also differed significantly with severity of dementia.
CMNS scores for family caregivers and variations across dementia severity of care receivers
We examined CMNS scores for all family caregivers and grouped by dementia severity of the care receiver (Table 2). The mean total score on the CMNS for all 250 family caregivers was 93.29 (SD = 27.79), indicating family caregivers had a moderate overall level of caregiving management needs. Mean scores for all six subscales indicated specific caregiving management needs were also moderate; the highest mean subscale score was immediate information (3.15, SD = 1.20) and the lowest was for care services (2.56, SD = 1.10).
We examined if management needs of caregivers varied across different dementia severity levels of the person with dementia. Total scores on the CMNS were significantly greater for caregivers of a person with moderate dementia compared with persons with very mild dementia (F = 3.91, p < 0.01), suggesting dementia severity influenced care management needs. Subscale scores for care services and psychological support also differed significantly for caregivers across levels of dementia severity of the care receiver. Caregivers of persons with mild, moderate, and severe dementia had significantly higher scores for care services compared with caregivers of persons with very mild dementia (F = 17.72, p < 0.001); and scores differed significantly between caregivers of persons with moderate dementia and mild dementia (p < 0.001). Caregivers of persons with moderate dementia had significantly higher scores for psychological support compared with caregivers of persons with very mild dementia (F = 2.67, p < 0.05). These findings suggest dementia severity had a significant impact on caregiving management needs.
Relationships between CMNS scores and characteristics of family caregivers and the person with dementia
We examined relationships between mean total scores for family caregivers on the CMNS and characteristics of family caregivers and persons with dementia (Table 3). Family caregivers who were female had significantly higher scores for total caregiving management needs (t = − 3.56, p < 0.001), compared with males. Additionally, family caregivers with a lower perceived economic status and poorer perceived health status had significantly higher scores compared with caregivers who perceived their status was higher (rs[248] = − 0.192, p < 0.01; and (rs[248] = − 0.148, p < 0.05; respectively), suggesting greater caregiving management needs. The mean total CMNS score was significantly higher for family caregivers of a person with dementia who was unmarried/widowed/divorced compared with scores for caregivers of a married care receiver (t = 2.17, p < 0.05). Other characteristics of care receivers resulting in higher CMNS scores having a lower score for MMSE (rs = − 0.140, p < 0.05), ADL (rs = − 0.283, p < 0.01), and IADL (rs = − 0.251, p < 0.01). The total number of behavioral problems exhibited by persons with dementia was also related to higher scores on the CMNS (F = 4.11, p < 0.05), with post hoc analysis indicating that scores were significantly higher if the person with dementia had ≥ 4 behavioral problems compared with those who had from 1 to 3. Finally, caregivers of a person with dementia who used long-term care services had significantly higher scores on the CMNS (t = -6.05, p < 0.01) compared with caregivers whose care receivers did not use these services, suggesting use of long-term care services did not reduce caregiving management needs.
We also examined if there were relationships between subscale scores and characteristics of the caregiver. Similar to the total score, compared with male caregivers, female caregivers had significantly higher scores for all six subscales, with the greatest difference in scores for immediate information (t = -3.45, p < 0.01) and individual case management services (t = -3.37, p < 0.01). Relationships were also seen for low economic status and care services, psychological support, anticipated information, and referral and tracking of long-term care resources. There were also significant relationships between the characteristic of poor health status and subscales of case services and immediate information; daily caregiving hours and the subscales of immediate information and referral and tracking of long-term care resources. Details of the relationships between caregiver characteristics and CMNS subscales scores are available in Additional file 2.
When we examined relationships between subscale scores and characteristics of the person with dementia, seven characteristics were associated with high subscale scores: residential status, MMSE score, medication adherence, number of behavioral problems, ADL and IADL status, and use of long-term care services. Caregivers with a care receiver using long-term care services had significantly higher scores for all six subscales compared with caregivers of a person who did not receive any assistance (p < 0.01 and p < 0.001). Other significant relationships were seen between caregivers of a person needing more assistance with ADLs, more assistance with IADLs and four subscales: care services, psychological support, immediate information, and referral and tracking of long-term care resources; persons with behavioral problems and subscales for care services, psychological support, anticipated information, and referral and tracking of long-term care resources. Other significant relationships included medication adherence and subscales for care services, psychological support, immediate information, and referral and tracking of long-term care resources. Details about these relationships and other significant characteristics are described in Additional file 2.
Predictors of caregiving management needs of family caregivers
We examined if any characteristics of caregivers or the person with dementia were predictors of total caregiving management needs using a linear regression model. The regression model identified five predictors of caregiving management needs for family caregivers of persons with dementia (Table 4). The variable of gender (female) was the only caregiver characteristic that was a predictor of high caregiving management needs (B = 9.49, 95% CI = 2.86, 16.11, p < 0.01). However, four characteristics of persons with dementia were predictors of caregivers with high caregiving management needs: adherence to medication (B = -17.13, 95% CI = -29.43, -4.82, p < 0.01); number behavioral problems (B = 1.87, 95% CI = 0.76, -2.99, p < 0.01); a low ADL score (B = -0.23, 95% CI = -0.39, -0.08, p < 0.01); and use of long-term care services (B = 16.27, 95% CI = 9.34, 23.20, p < 0.001). Use of long-term care services and a higher number of behavioral problems had the highest explanatory power (β = 0.282 and β = 0.199, respectively).
We also examined if any caregiver or care receiver characteristics that were significantly related to subscale scores of the CMNS were predictors of specific caregiving management needs. The linear regression models included caregiver variables of gender, perceived economic status, health status, and the seven care receiver variables shown to be significantly related to specific management needs. All models were significant, with explanatory variance ranging from 10.5 to 41.9%. The greatest needs for female caregivers were seen for case services (B = 0.24, p < 0.05), psychological support (B = 0.46, p < 0.01), and immediate information (B = 0.34, p < 0.01), and individual case management services (B = 0.36, p < 0.01). Persons with dementia who used long-term care services were significant predictors of caregivers who had a need for psychological support (B = 0.61, p < 0.001), anticipated information (B = 0.31, p < 0.05), RTLCS (B = 0.48, p < 0.01), as well as individual case management services (B = 0.61, p < 0.001). Details of the regression models for each subscale are available in Additional file 3.
Discussion
Caregivers of persons with dementia in our study had a moderate level of overall caregiving management needs. The caregiver characteristic of gender (female), perceived economic status, and perceived health status were associated with higher caregiver management needs. Whereas the level of dementia severity of the care receiver as well as characteristics of residential status, MMSE score, medication adherence, number of behavioral problems, ADL and IADL status, and use of long-term care services were associated with higher needs. When we examined if any significant variables were predictors of caregiving management needs, analysis identified one caregiver characteristic (gender, female) and four care receiver characteristics: adherence to medication, number of behavioral problems, a low ADL score, and use of long-term care services.
Our initial linear regression analysis focused on total CMNS scores, which indicated only one of the five predictors of caregiving management needs was related to a characteristic of family caregivers. This finding is similar to a study conducted in Germany that reported female caregivers of persons with dementia experienced a higher perceived caregiving burden compared with male family caregivers [32]. Taiwan is strongly influenced by the Chinese cultural expectations of filial piety, where women are expected to balance caring for parents and young children, even while employed [33]. Therefore, our finding may be related to the societal influences of Taiwan. Although not examined as a predictive factor for caregiving management needs, a study reported that most family caregivers of persons with dementia with at least one unmet need were female [7].
However, linear analysis of the six subscales and caregiver variables demonstrated that gender (female) was a predictor of four specific needs (case services, psychological support, immediate information, and individual case management services) and the characteristic of perceived low economic status was also a significant predictor of psychological support needs in addition to anticipated information and referral and tracking of long-term care services. These findings are in contrast to studies that have suggested higher unmet needs are associated with caregiver characteristics of age, educational level, caregiving hours, and symptoms of depression [24, 26].
The care receiver characteristic of dementia severity was associated with significantly higher CMNS scores for family caregivers of persons with moderate dementia compared with caregivers of persons with very mild dementia. When we examined relationships between all care receiver characteristics and caregiver needs, this finding was supported by the significant relationship between caregivers of a person with a lower MMSE score and higher total caregiving management needs. When specific needs were examined, dementia severity was associated with higher specific needs of case services and psychological support. Two scoping reviews have suggested support for emotional distress resulting from caregiving is one of the most frequently mentioned needs for caregivers of persons with dementia [8, 34]. When all care receiver characteristics and subscale scores were examined, only the relationship between MMSE scores and case services remained significant. However, a care receivers’ MMSE score was not a predictor of any of the six specific needs. Lower MMSE scores have been demonstrated to be a predictor of greater caregiving needs for persons with dementia [35]. Increased cognitive impairment has also been shown to cause family caregivers in Taiwan to consider long-term care resources [36]. Our findings suggest this may be the result of a failure to obtain caregiving management services.
In addition to dementia severity, other predictors of caregiving management needs were high medication adherence, number of behavioral problems, ADLs, and the use of long-term care services. When we examined all care receiver characteristics that were significantly related to specific caregiver needs, regression analysis identified high medication adherence, number of behavioral problems, ADLs, IADLs, and the use of long-term care services as predictors of specific needs. High medication adherence was a predictor for three caregiving needs: psychological support, immediate information, and referral and tracking of long-term care services. The number of behavioral problems and the use of long-term care services were both predictors for five needs: case services, psychological support, immediate information, anticipated information, and referral and tracking services.
Two scenarios might explain high medication adherence as a predictor of caregiving needs. Adherence may have been the result of the family caregiver being more vigilant about monitoring the daily regimen of the person with dementia, leading to higher caregiving management needs. However, the person with dementia may have adhered to their medications because their cognitive abilities had declined, which would have also increased caregiving management needs. Whether these are influencing variables warrant further exploration.
The five characteristics identified as predictors of specific caregiving needs are variables that should be discussed with family caregivers of persons with dementia when attempting to determine what care management needs should be provided to reduce caregiver burden. Use of long-term care services [36] and the numbers of behavioral problems for persons with dementia [37] have been demonstrated to be predictors of unmet needs and increased caregiver burden and these two characteristics were predictors of five of the six specific needs. In addition, we did not collect data types of behaviors. Descriptions of types and frequency of disruptive behaviors should be explored in future studies to better understand their impact on caregiving management needs. Although a low MMSE score was not a predictor of total care management needs or any specific need, more behavioral problems, the use of long-term care, and a decrease in independence, as measured by ADLs and IADLs, are all associated an increase in severity of dementia, which often require additional care services beyond those that a family caregiver can provide [38]. Our findings suggest that family caregivers caring for a person with dementia with four or more behavioral problems, low ADL or IADL scores, or use long-term care services may have a high need for additional care management services. Caregivers who engage providers of long-term care services are more likely to experience a more satisfactory health status and lower caregiver burden compared with caregivers who do not use any care resources [39]. The CMNS could be used to proactively identify family caregivers in need of long-term care services as a means of providing additional care and reducing caregiver burden.
Limitations
The study had several limitations. First, although the researcher developed CMNS evaluated caregiving management needs, it did not include a ranking of needs in order of importance. Including ranking in future studies could provide more information about prioritizing intervention strategies. Second, we did not survey the care management needs of the persons with dementia. Understanding caregiving management needs from the perspectives of persons with dementia has been demonstrated to be an important variable for helping caregivers provide quality care [27]. Finally, most family caregivers lived with the person with dementia, which prevents generalizing our findings to family caregivers who provide a significant amount of care without residing the care receiver.
Conclusion
The CMNS can be used to evaluate caregiving management needs for family caregivers of persons with dementia. Our findings indicated that caregiving management needs were primarily influenced by four characteristics of the person living with dementia: ≥ 4 behavioral problems, dependency for assistance with ADLs, dementia medication adherence, and use of long-term care services. The CMNS can also guide case managers in providing caregiving support and resources that are tailored to the specific needs of the family caregiver, which could reduce caregiver burden and improve quality of life for both the caregiver and the persons with dementia.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADL:
-
Activities of Daily Living
- MMSE:
-
Mini-Mental State Examination
- CDR:
-
Clinical Dementia Rating
- IADL:
-
Instrumental Activities of Daily Living
- CMNS:
-
Caregiving Management Needs Scale
- CVI:
-
Content validity index
- CFA:
-
Confirmatory factor analysis
References
Gale SA, Acar D, Daffner KR, Dementia. Am J Med. 2018;131(10):1161–9. https://doi.org/10.1016/j.amjmed.2018.01.022.
Analysis of household census data in August of the 112th year of the Republic of China. Ministry of Interior.https://www.moi.gov.tw/News_Content.aspx?n=9&sms=9009&s=295989. (Original work published in Chinese)(2023) Accessed 22 Jan. 2024.
2022 Alzheimer’s disease facts and figures. Alzheimer’s Association.https://www.alz.org/media/documents/alzheimers-facts-and-figures.pdf.(2022).
Sheehan OC, Haley WE, Howard VJ, Huang J, Rhodes JD, Roth DL. Stress, burden, and well-being in dementia and nondementia caregivers: insights from the caregiving transitions study. Gerontologist. 2021;61(5):670–9. https://doi.org/10.1093/geront/gnaa108.
Bertrand RM, Fredman L, Saczynski J. Are all caregivers created equal? Stress in caregivers to adults with and without dementia. J Aging Health. 2006;18(4):534–51. https://doi.org/10.1177/0898264306289620.
Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist. 1986;26(3):260–6. https://doi.org/10.1093/geront/26.3.260.
Zwingmann I, Michalowsky B, Esser A, Kaczynski A, Monsees J, Keller A, Hertel J, Wucherer D, Thyrian JR, Eichler T, Kilimann I, Teipel S, Dreier Wolfgramm A, Hoffmann W. Identifying unmet needs of family dementia caregivers: results of the baseline assessment of a cluster-randomized controlled intervention trial. J Alzheimers Dis. 2019;67(2):527–39. https://doi.org/10.3233/JAD-180244.
Queluz FNFR, Kervin E, Wozney L, Fancey P, McGrath PJ, Keefe J. Understanding the needs of caregivers of persons with dementia: a scoping review. Int Psychogeriatr. 2020;32(1):35–52. https://doi.org/10.1017/S1041610219000243.
Bressan V, Visintini C, Palese A. What do family caregivers of people with dementia need? A mixed-method systematic review. Health Soc Care Community. 2020;28(6):1942–60. https://doi.org/10.1111/hsc.13048.
Steenfeldt VØ, Aagerup LC, Jacobsen AH, Skjødt U. Becoming a family caregiver to a person with dementia: a literature review on the needs of family caregivers. SAGE Open Nurs. 2021;7:23779608211029073. https://doi.org/10.1177/23779608211029073.
Gibson AK, Anderson KA, Acocks S. Exploring the service and support needs of families with early-onset Alzheimer’s disease. Am J Alzheimers Dis. 2014;29(7):596–600. https://doi.org/10.1177/1533317514558160.
Bakker C, Verboom M, Koopmans R. Reimagining postdiagnostic care and support in Young-Onset Dementia. J Am Med Dir Assoc. 2022;23(2):261–5. https://doi.org/10.1016/j.jamda.2021.12.008.
Low LF, Gresham M, Phillipson L. Further development needed: models of post-diagnostic support for people with dementia. Curr Opin Psychiatry. 2023;36(2):104–11. https://doi.org/10.1097/YCO.0000000000000848.
MacNeil Vroomen J, Bosmans JE, van de Ven PM, et al. Community-dwelling patients with dementia and their informal caregivers with and without case management: 2-year outcomes of a pragmatic trial. J Am Med Dir Assoc. 2015;16(9):e8001–8008008. https://doi.org/10.1016/j.jamda.2015.06.011.
Caregiving for Person with Alzheimer’s Disease or a related Dementia. 2022. Centers Disease Control Prev https://www.cdc.gov/aging/caregiving/alzheimer.htm
Huang HL, Shyu YI, Chen MC, Huang CC, Kuo HC, Chen ST, Hsu WC. Family caregivers’ role implementation at different stages of dementia. Clin Interv Aging. 2015;10:135–46. https://doi.org/10.2147/CIA.S60574.
Huang HL, Shyu YL, Hsu WC, Liao YT, Huang HL, Hsieh SH. Effectiveness of a health education program for people with dementia and their family caregivers: an intervention by nurse practitioners. Arch Psychiatr Nurs. 2024;50:147–59. https://doi.org/10.1016/j.apnu.2024.03.018.
Kuo LM, Huang HL, Liang J, Kwok YT, Hsu WC, Su PL, Shyu YL. A randomized controlled trial of a home-based training programme to decrease depression in family caregivers of persons with dementia. J Adv Nurs. 2017;73(3):585–98. https://doi.org/10.1111/jan.13157.
Dementia prevention and care policy. and action plan 2.0. Ministry of Health and Welfare.https://1966.gov.tw/LTC/cp-6572-69818-207.html. (Original work published in Chinese) (2023) Accessed 23 Jan. 2024.
Wancata J, Krautgartner M, Berner J, et al. The Carers’ needs Assessment for Dementia (CNA-D): development, validity and reliability. Int Psychogeriatr. 2005;17(3):393–406. https://doi.org/10.1017/s1041610205001699.
Sadak T, Korpak A, Borson S. Measuring caregiver activation for health care: validation of PBH-LCI:D. Geriatr Nurs. 2015;36(4):284–92. https://doi.org/10.1016/j.gerinurse.2015.03.003.
Chiang KY, Fan SY, Chang LH, Chang WY, Pai MC, Wang JY. Development and psychometric validation of a tool for assessing the care needs of families of patients with dementia. J Nuring. 2020;67(4):39–49. https://doi.org/10.6224/JN.202008_67(4. (Original published in Chinese).
Kinchin I, Edwards L, Adrion E, Chen Y, Ashour A, Leroi I, Brugulat-Serrat A, Phillips J, Masterson F, Kochovska S. Care partner needs of people with neurodegenerative disorders: what are the needs, and how well do the current assessment tools capture these needs? A systematic meta-review. Int J Geriatr Psychiatr. 2022;37(7):1–18. https://doi.org/10.1002/gps.5764.
Black BS, Johnston D, Leoutsakos J, Reuland M, Kelly J, Amjad H, Davis K, Willink A, Sloan D, Lyketsos C, Samus QM. Unmet needs in community-living persons with dementia are common, often non-medical and related to patient and caregiver characteristics. Int Psychogeriatr. 2019;31(11):1643–54.
Richardson VE, Fields N, Won S, Bradley E, Gibson A, Rivera G, Holmes SD. At the intersection of culture: ethnically diverse dementia caregivers’ service use. Dementia. 2019;18(5):1790–809. https://doi.org/10.1177/1471301217721304.
Tapia Muñoz T, Slachevsky A, León-Campos MO, et al. Predictors of unmet needs in Chilean older people with dementia: a cross-sectional study. BMC Geriatr. 2019;19(1):106. https://doi.org/10.1186/s12877-019-1131-1.
Morris JC. The clinical dementia rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412–4. https://doi.org/10.1212/wnl.43.11.2412-a.
Mahoney FI. Functional evaluation: the Barthel Index. Md State Med J. 1965;14(2):61–5.
Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52–63. https://doi.org/10.1097/01.NAJ.0000314810.46029.74.
Kline R. Exploratory and confirmatory factor analysis. Applied quantitative analysis in education and the social sciences. Routledge; 2013. pp. 171–207.
Akinwande MO, Dikko HG, Samson A. Variance inflation factor: as a condition for the inclusion of suppressor variable(s) in regression analysis. OPEN J Stat. 2015;5(7):754. https://doi.org/10.4236/ojs.2015.57075.
Seidel D, Thyrian JR. Burden of caring for people with dementia - comparing family caregivers and professional caregivers. A descriptive study. J Multidiscip Healthc. 2019;12:655–63. https://doi.org/10.2147/JMDH.S209106.
Macleod A, Tatangelo G, McCabe M, You E. There isn’t an easy way of finding the help that’s available. Barriers and facilitators of service use among dementia family caregivers: a qualitative study. Int Psychogeriatr. 2017;29(5):765–76. https://doi.org/10.1017/S1041610216002532.
Clemmensen HT, Lauridsen HH, Andersen-Ranberg K, Kristensen HK. Informal carers’ support needs when caring for a person with dementia - A scoping literature review. Scand J Caring Sci. 2021;35(3):685–700. https://doi.org/10.1111/scs.12898.
Tobis S, Wieczorowska-Tobis K, Talarska D, Pawlaczyk M, Suwalska A. Needs of older adults living in long-term care institutions: an observational study using Camberwell Assessment of need for the Elderly. Clin Interv Aging. 2018;13:2389–95. https://doi.org/10.2147/CIA.S145937.
Shih PY, Ku LJE, Pai MC, Liu LF. Long-term care services use and reasons for non-use by elders with dementia and their families. Taiwan J Public Health. 2017;36(4):375–85. https://doi.org/10.6288/TJPH201736106026. (Original work published in Chinese).
Cheng ST. Dementia caregiver burden: a research update and critical analysis. Curr Psychiatry Rep. 2017;19(9):64. https://doi.org/10.1007/s11920-017-0818-2.
Wang WF, Su YY, Jhang KM, Chen CM. Patterns of home- and community-based services in older adults with dementia: an analysis of the long-term care system in Taiwan. BMC Geriatr. 2021;21(1):290. https://doi.org/10.1186/s12877-021-02231-9.
Chang CH, Ming Y, Chang TH, Yen YY, Lan SJ. The needs and utilization of long-term care service resources by dementia family caregivers and the affecting factors. Int J Environ Res Public Health. 2020;17(16):6009. https://doi.org/10.3390/ijerph17166009.
Funding
This work was supported by the National Science and Technology Council, Taiwan (grant numbers: 109-2511-H-255-004 -; MOST 110-2511-H-255-003-MY2). and Geriatric and Long-Term Care Research Center, Chang Gung University of Science and Technology (grant numbers: ZRRPF3K0071).
Author information
Authors and Affiliations
Contributions
HLH contributed to the conception, design, and supervision of the study. YTL, WCH and JLH acquired the data. HLH, YTL, and PCK contributed to the statistical analysis and interpretation of the data. HLH and YTL contributed to the draft and revision of the manuscript. YILS contributed to the conceptualization of the study and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Chang Gung Medical Foundation Institutional Review Board (No.202000902B0). Written informed consent was obtained from caregivers prior to enrollment in the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, HL., Liao, YT., Kung, PC. et al. Caregiving management needs and predictors for family caregivers of persons with dementia: a cross-sectional study. BMC Geriatr 24, 724 (2024). https://doi.org/10.1186/s12877-024-05316-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05316-3