Abstract
Background
Creatinine-to-cystatin C ratio (CCR) has been associated with multiple adverse outcomes. However, little is known about its relationship with frailty. We aimed to explore the association between CCR and frailty among older adults.
Methods
A total of 2599 participants aged ≥ 60 years (mean age 67.9 ± 6.0 years, 50.4% males) were included from the China Health and Retirement Longitudinal Study (2011–2015). Baseline CCR was calculated as plasma creatinine (mg/dL) / cystatin C (mg/L) × 10 and was grouped by quartiles. Frailty was evaluated by the validated physical frailty phenotype (PFP) scale and was defined as PFP score ≥ 3. The generalized estimating equations model was used to explore the relationship between CCR and frailty.
Results
The frailty risk decreased gradually with increasing CCR in the quartiles (P for trend = 0.002), and the fourth CCR quartile was associated with a significantly lower risk of frailty compared with the lowest quartile (odds ratio [OR] 0.37, 95% confidence interval [CI] 0.19–0.70). When modeling as a continuous variable, per 1-unit increase in CCR was related to 17% decreased odds of frailty (OR 0.83, 95% CI 0.74–0.93). The association was consistent in male and female participants (P for interaction = 0.41). Poisson models revealed that frailty score was negatively associated with CCR (β= -0.11, 95% CI= -0.19 to -0.04), and sex did not significantly moderate the associations (P for interaction = 0.22). The results were not affected by further adjusting for high-sensitivity C-reactive protein. Similar results were observed by analyses with multiple imputation technique and analyses excluding participants with baseline frailty.
Conclusions
Higher CCR was associated with a lower frailty risk. CCR may be a simple marker for predicting frailty in older adults.
Similar content being viewed by others
Background
Frailty is a common geriatric syndrome characterized by diminished functioning across multiple physiological systems along with an elevated vulnerability to stressors [1], which is associated with numerous adverse outcomes (e.g., falls, fractures, disability, and mortality) [1,2,3,4,5]. It is estimated to occur in 10% of older community-dwellers [6] and is more prevalent in other settings like hospitals [5] and nursing homes [7]. As the population ages, the number of older adults with frailty is expected to increase substantially. Frailty is emerging as a global health burden, with important implications for clinical practice and public health. However, to date, the underlying mechanisms of frailty are still far from being understood, and effective interventions are also lacking [1]. A better knowledge of the underlying risk factors of frailty is thus imperative, which may not only help to accurately characterize individual risk profiles but may also provide potential targets for frailty-modifying interventions.
Sarcopenia, marked by loss of skeletal muscle mass and function [8], is proposed as the biological substratum of frailty [9]. It has been considered a precursor syndrome or a major component of frailty [10], and growing studies have confirmed sarcopenia in relation to frailty [11,12,13]. Interventions targeting skeletal muscle can provide preventive and therapeutic benefits against frailty [9], and people with sarcopenia have been established as a special target group for frailty prevention [1, 14]. Thus, early identification of sarcopenia is important for the implementation of early interventions in clinic, but it often requires quantification of muscle mass with specific devices (e.g., bioelectrical impedance analysis, dual-energy X-ray absorptiometry, or computed tomography) and assessment of muscle function by grip strength and gait speed, which may be costly, time-consuming, and more often than not, impossible in the busy clinical setting.
Recently, creatinine-to-cystatin C ratio (CCR), an easily available, economical biomarker, has been suggested as a reliable surrogate indicator of sarcopenia [15, 16]. Serum creatinine and cystatin C are commonly used markers for evaluating kidney function. Creatinine is mainly produced by skeletal muscle cells, and its circulating level is not only influenced by kidney function but also by muscle mass. Contrarily, cystatin C is less affected by skeletal muscle as it is excreted by all nucleated cells. Hence, the relative concentration of creatinine to cystatin C can reflect muscle mass [17]. Increasing studies have found that CCR is strongly related to skeletal muscle mass and strength [17,18,19], and its diagnostic accuracy and prognostic value for sarcopenia have been validated in many diseases [15, 16, 20, 21]. Previous research has reported the association of sarcopenia with frailty [11,12,13], however, evidence regarding the link between CCR and frailty is limited.
Therefore, in this study, we aimed to explore the relationship between CCR and frailty. As lower CCR is associated with sarcopenia and other negative health events, we speculated that participants with lower CCR were at greater risk of frailty. Given the reported sex differences in CCR [15, 19], a sex-specific subgroup analysis was further conducted.
Methods
Study population
This cohort study was performed based on the China Health and Retirement Longitudinal Study (CHARLS), which is a prospective population-based survey of middle-aged and older adults (≥ 45 years) from 28 provinces in China. CHARLS baseline survey was conducted in 2011, with subsequent follow-ups held biennially. Details of the CHARLS study have been described previously [22]. The Ethics Review Committee of Peking University (IRB00001052-11015) approved CHARLS. All participants signed written informed consent. More details are available on its website (http://charls.pku.edu.cn/).
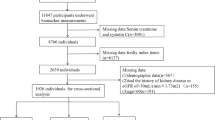
In the current study, three waves of CHARLS data (2011, 2013, and 2015) were used. Eligible participants were those aged ≥ 60 years in 2011. Participants were excluded if they: (1) had missing data on age; (2) had no baseline data on creatinine or cystatin C levels; (3) with kidney disease or estimated glomerular filtration rate (eGFR) < 30 mL/(min×1.73 m2) based on the Chinese based equation [23]; (4) without sufficient information on baseline frail status; (5) without complete frailty data at any of the two subsequent follow-up surveys. The flowchart of the participants’ selection was detailed in Fig. 1.
Creatinine-to-cystatin C ratio
Venous blood samples were collected by medically-trained staff from each respondent after fasting overnight. After collection, the blood samples were transported to the local laboratory at 4 ◦C and then were separated into plasma and buffy coat, frozen at -20 ◦C, which were finally transported to the Chinese Center for Disease Control and Prevention in Beijing within 2 weeks, where they were placed in a deep freezer and stored at -80 ◦C until assayed.
Plasma creatinine was analyzed using the rate-blanked and compensated Jaffe creatinine method (within-assay coefficients of variation [CVs] < 1.6%, between-assay CVs < 2.1%, and detection limits: 0.1–25 mg/dL), while cystatin C was measured by the particle-enhanced turbimetric assay (within-assay CVs < 5%, between-assay CVs < 5%, and detection limits: 0.5-8 mg/L). Creatinine-to-cystatin C ratio (CCR) was calculated as creatinine (mg/dL) / cystatin C (mg/L) × 10 [17, 24], and was classified into four groups by quartiles (Q1-Q4).
Frailty assessment
Frailty was determined by the modified physical frailty phenotype (PFP) scale [25], which was constructed and validated using CHARLS data [26]. The PFP scale contains five components: weakness, slowness, exhaustion, inactivity, and shrinking, totaling a score of 5. Consistent with the previous study [26], weakness was defined as the maximal handgrip strength of either hand (twice for each hand, measured in a standing position) ≤ 20% of the weighted population distribution, after adjusting for sex and body mass index (BMI). Slowness was identified as gait speed (measured as the average of two trials of walking tests over a 2.5-meter course) ranking in the slowest 20% of the weighted population distribution, after adjustment for sex and height [26]. Exhaustion was defined if participants answered “Moderate amount of time: 3–4 days” or “Most or all of the time: 5–7 days” to either of the following two questions: “I could not get going” and “I felt everything I did was an effort” [26]. Inactivity was evaluated by asking participants if they were able to walk continuously for at least 10 min during a usual week, and participants were determined to be inactive if they answered “no”. Shrinking was defined as having a current BMI ≤ 18.5 kg/m2 or having lost at least 5 kg in the last year. Those scoring ≥ 3 out of the 5 points were considered as having frailty, 1–2 as prefrailty, and 0 as robustness. If ≥ 2 PFP components were missing, frailty status was treated as missing [27].
Covariates
The following covariates were included: age, sex, marital status (married/partnered, unmarried/others), educational level (illiterate, primary school or below, middle school, high school or above), residence area (urban, rural), geographical region, household income per capita (yuan), current working status (working, non-working). Consistent with previous studies [26, 28], we classified investigated provinces into nine geographical regions: (1) Northwest, including Shaanxi, Gansu, Qinghai, and Xinjiang; (2) Northern, including Beijing, Tianjin, Hebei, Shanxi, and Inner Mongolia; (3) Central, including Shandong, Henan, and Anhui; (4) Southwest, including Chongqing, Sichuan, Guizhou, and Yunnan; (5) South, including Guangdong and Guangxi; (6) Northeast, including Heilongjiang, Jilin, and Liaoning; (7) East, including Shanghai and Jiangsu; (8) South Central, including Hubei, Hunan, and Jiangxi; and (9) Southeast, including Zhejiang and Fujian. Smoking status was measured by asking participants if they had ever smoked and if they were currently smoking, and was classified as never smoking, past smoking, and current smoking. Drinking status was determined by asking respondents the frequency of alcoholic beverages during the past year and was categorized into never drinking, drinking ≤ 1 time/month, and drinking > 1 time/month. Social activities were identified if the subject engaged in at least one of the following activities: (1) interacting with friends; (2) playing mahjong, chess, cards, or going to a community club; (3) going to a sport, social, or other kinds of clubs; (4) participating in community-related organizations; (5) doing voluntary or charity work; or (6) attending an educational or training course. The number of comorbidities was assessed based on the presence of 13 self-reported chronic conditions (hypertension, heart problems, stroke, diabetes, dyslipidemia, cancer [excluding minor skin cancers], chronic lung disease, digestive disease, liver disease, arthritis/rheumatism, emotional/nervous/psychiatric problems, memory-related disease, and asthma), and was classified into three categories: 0, 1, and ≥ 2 diseases. Self-reported health status was categorized into three groups: good, fair, and poor. BMI was calculated as weight divided by the square of height (kg/m2).
Statistical analysis
Continuous variables were presented as mean with standard deviation (SD) or median with interquartile range (IQR), and were assessed by t-test, analysis of variance, Mann-Whitney U test, or Kruskal-Wallis H test, as appropriate. Categorical variables were expressed as frequencies with percentages, and were evaluated via χ2 or Fisher’s exact test.
The generalized estimating equations (GEE) model was adopted to examine the association between baseline CCR and frailty in the following several years, where the results were expressed as odds ratio (OR) with 95% confidence intervals (CI). CCR was first analyzed as a continuous variable (per 1-unit increase), and then was included as a categorical variable to detect possible curvilinear associations between CCR and frailty. As there were no established thresholds for CCR [29] and given the sample size of this study, we divided the participants into four categories based on CCR quartiles (Q1 was set as the reference). Three models were fitted: (1) Model 1: age and sex adjusted; (2) Model 2: additionally adjusted for marital status, educational level, residence, geographical region, household income, working status, smoking and drinking status, social activities, number of chronic diseases, and self-reported health status; (3) Model 3: further adjusted for BMI, eGFR, and baseline frailty score. All covariates were measured in each wave and included as time-dependent covariates, except for age and sex, which were measured only at baseline. Trends in ORs across CCR quartiles were estimated by using the median within each quartile as the predictor.
Given the sex difference in CCR [15, 19, 24], subgroup analysis by sex was further conducted, and the interaction between CCR and sex was tested by including a multiplicative term in the model. Four sensitivity analyses were performed to evaluate the robustness of our findings: (1) we repeated the analyses treating the outcome measure as continuous PFP scores, using Poisson models with Poisson family and log link; (2) high-sensitivity C-reactive protein (hs-CRP) was additionally adjusted in the multivariate model to control the potential confounding of inflammation, as inflammation may potentially affect CCR level [30]; (3) we performed multiple imputations with 10 replications using chained equations procedure to impute missing data, which were assumed to be missing at random, and the results were pooled by Rubin’s rule [31]; (4) to rule out the potential reverse causality, we reanalyzed the data after excluding baseline frail population (n = 181). As CCR was closely correlated to age (Spearman’s rank correlation = -0.20, P < 0.001) in this study, which may potentially bias the relationship between CCR and frailty, we performed additional stratified analysis by age groups (60–69, 70–79, and ≥ 80 years) to explore the possible heterogeneous effects of age.
In addition, the multinomial logistic regression models were used to examine the association between CCR and the risk of prefrailty and frailty in baseline robust participants (n = 919). Finally, to evaluate the predictive ability of CCR for frailty, we further conducted the receiver operating characteristic (ROC) curve analysis and the optimal cutoff threshold was determined by Youden’s index.
All analyses were conducted using Stata version 15.0 (StataCorp, College Station, TX, USA). A two-sided P-value < 0.05 was considered to be statistically significant.
Results
Baseline characteristics
Among the 17,708 participants initially recruited in 2011, we screened 3873 older adults with CCR. After excluding those without baseline frailty data (n = 804) and those without complete frailty data at any of the two follow-up surveys (n = 470), 2599 participants were finally included (Fig. 1). Compared with the excluded subjects, those included were older, more likely to be male, unmarried, had lower socioeconomic status, higher comorbidity burden, lower eGFR, and lower CCR level (all P < 0.05, Table A1 in the Additional file 1).
The baseline characteristics of the participants were depicted in Table 1. Overall, the average age of the 2599 participants was 67.9 ± 6.0 years, and 1310 (50.4%) were males. The median value of CCR was 7.37 (IQR 6.40–8.43). All participants were classified into four groups by the quartiles of CCR (Q1 < 6.397, Q2 6.397–7.370, Q3 7.371–8.430, and Q4 > 8.430). Subjects in the highest quartile were younger, more likely to be male, married/partnered, higher educated, urban residents, smokers, drinkers, and had a higher household income per capita, higher social activity participation, lower eGFR, higher creatinine, and lower cystatin C level (all P < 0.05, Table 1); whereas no significant difference was found in working status, comorbidity burden, and BMI among CCR quartiles.
Association between CCR and frailty
Figure 2 and Table A2 showed the association of CCR with frailty based on GEE models. We found that the ORs for frailty were significantly lower in groups with higher CCR than those in Q1, and the frailty risk decreased successively with increasing CCR in the quartiles (P for trend = 0.002, Fig. 2). After adjusting for potential confounders (in Model 3), the fourth quartile showed a significant decrease in frailty compared to the first quartile (OR 0.37, 95% CI 0.19–0.70). When modeling CCR as a continuous variable, per 1-unit increase in CCR was associated with 17% decreased odds of frailty (95% CI 7%-26%, Fig. 2; Table A2).
The association of CCR with (A) frailty and (B) frailty score. Adjusted for age, sex, marital status, educational level, residence, geographical region, household income per capita, working status, smoking and drinking status, social activities, number of chronic diseases, self-reported health status, BMI, eGFR, and frailty score at baseline. CCR, creatinine-to-cystatin C ratio; OR, odds ratio; CI, confidence interval. ***, P < 0.001; **, P < 0.01; *, P < 0.05
Subgroup analysis revealed that the association between CCR and frailty was consistent across sex-based subgroups (P for interaction = 0.41). In males, per 1-unit increase in CCR was related to a 22% lower risk of frailty (OR 0.78, 95% CI 0.63–0.96, Fig. 2 and Model 3 in Table A2). A similar tendency of association between CCR and frailty was observed in females (Fig. 2 and Table A2). Results of analyses treating the outcome as continuous frailty scores were shown in Fig. 2. Frailty score was negatively associated with CCR (β= -0.11, 95% CI= -0.19 to -0.04), and sex did not modify the associations (P for interaction = 0.22). The results were not affected by further adjustment for hs-CRP (Fig. 3). Analyses using dataset with multiple imputation techniques yielded similar associations between CCR and frailty (Fig. 4). To avoid the influence of possible reverse causation, we repeated the analyses after excluding 181 participants with baseline frailty, and the associations of CCR with frailty were not significantly changed (Fig. 5). Age did not significantly modify the relationships between CCR and frailty (all P for interaction > 0.05, Table A3).
Sensitivity analysis of the association of CCR with (A) frailty and (B) frailty score, after further adjusting for hs-CRP. Adjusted for age, sex, marital status, educational level, residence, geographical region, household income per capita, working status, smoking and drinking status, social activities, number of chronic diseases, self-reported health status, BMI, eGFR, frailty score at baseline, and hs-CRP. CCR, creatinine-to-cystatin C ratio; hs-CRP, high-sensitivity C-reactive protein; OR, odds ratio; CI, confidence interval. ***, P < 0.001; **, P < 0.01; *, P < 0.05
The association of CCR with (A) frailty and (B) frailty score, using dataset with multiple imputation techniques. Adjusted for age, sex, marital status, educational level, residence, geographical region, household income per capita, working status, smoking and drinking status, social activities, number of chronic diseases, self-reported health status, BMI, eGFR, and frailty score at baseline. CCR, creatinine-to-cystatin C ratio; OR, odds ratio; CI, confidence interval. ***, P < 0.001; **, P < 0.01; *, P < 0.05
The association of CCR with (A) frailty and (B) frailty score, after excluding frail population at baseline (N = 2418). Adjusted for age, sex, marital status, educational level, residence, geographical region, household income per capita, working status, smoking and drinking status, social activities, number of chronic diseases, self-reported health status, BMI, eGFR, and frailty score at baseline. CCR, creatinine-to-cystatin C ratio; OR, odds ratio; CI, confidence interval. ***, P < 0.001; **, P < 0.01; *, P < 0.05
The multinomial regression analysis confirmed the association of CCR with frailty, but not with prefrailty (Table A4). The ROC analysis showed that the predictive ability of CCR for frailty was moderate, and CCR higher than the optimal cut-off (7.66) was associated with a significantly reduced risk of frailty (OR 0.54, 95% CI 0.35–0.82, Table A5).
Discussion
The present study revealed that higher CCR was independently associated with a lower risk of frailty, and the association was consistent among male and female participants. Our results offer evidence of the association between CCR and frailty, suggesting that CCR may serve as a simple, practical marker for predicting frailty in older adults.
Although the relationship between sarcopenia and frailty has been reported [11,12,13], few studies have evaluated whether CCR, a marker of sarcopenia, is related to frailty. A recent cross-sectional study, focusing on 1208 subjects without advanced cirrhosis from the Framingham Heart Study, found that CCR was inversely related to physical frailty as measured by the Liver Frailty Index [13], which was partially in agreement with our current results. Different from the above study [13], we conducted a prospective cohort and extended our analysis to the Chinese population, by using data from a large longitudinal population-based survey with multiple repeated frailty measurements. The participants included in our study were recruited from 2127 households and 391 communities within 28 provinces in China, constituting a nationally representative sample, and the sample size was twice larger than the previous research [13]. Moreover, we chose the most widely used and well-validated instrument (i.e., the PFP scale) to measure frailty, which strengthened the reliability of our results.
Creatinine is produced by skeletal muscle cells, and its circulating level is generally higher in men than that in women. A clear sex difference in CCR has been reported [16, 19], thus a sex-specific subgroup analysis is required. In our sex-stratified analysis, as expected, males had a significantly higher CCR than females (median [IQR] 7.88 [6.97–8.95] vs. 6.86 [5.99–7.81], P < 0.001, Table A6). After adjusting for all covariates in the multivariate analysis, similar associations between CCR and frailty were observed in both sex groups. The results suggest that CCR may provide important predictive information for frailty, regardless of sex. As the measurement of creatinine and cystatin C is inexpensive and easily available in clinic, CCR may be a promising and time-efficient marker for identifying individuals at risk of frailty.
There are several possible explanations for the observed relationship between CCR and frailty. First, CCR is a reliable marker of skeletal muscle mass and strength [17,18,19], with lower CCR indicating reduced muscle mass and weak muscle strength. The core feature of frailty is physical function impairment [1, 32]. Advancing age combined with physical decay, especially a loss of skeletal muscle mass, would contribute to frailty. Furthermore, skeletal muscle is important to maintain metabolic homeostasis [33], and reduced muscle mass may confer an increased risk of comorbidities [34, 35], the cumulation of which may drive people to be frail. It has been reported that CCR was associated with the disorders of multiple physiological systems like endocrine, cardiovascular, and nervous systems, and could predict a range of negative health outcomes. For example, accumulating clinical evidence has indicated the associations of low CCR with osteoporosis [36], diabetes [37], atherosclerosis [38, 39], cardiovascular events [40], depressive symptoms [41], and cognitive impairment [42]. The compromise of multisystemic homeostasis and resilience may eventually result in the occurrence of frailty.
Apart from reflecting skeletal muscle, CCR may also be indicative of inflammatory status, which is a well-known risk factor for frailty onset or progression [1]. Inflammation is associated with lower creatinine and higher cystatin C levels [30], and increases in CCR are found to be related to the amelioration of inflammation [43]. These data imply that the noted association between CCR and frailty may be mediated through inflammation. However, in the sensitivity analysis, CCR remained significantly associated with frailty even after adjustment for hs-CRP, which suggests that the association with frailty is independent of inflammatory status.
The strengths of this study included the prospective study design and population-based setting. Besides, GEE models were used to investigate the longitudinal associations, which enabled us to obtain robust estimates taking into account the within-participant association across repeated measurements. The sensitivity analyses further confirmed the robustness of our findings. However, some limitations must be acknowledged. First, this study focused mainly on older adults in China, and the generalizability to young persons and other populations may be limited. Second, selection bias may be introduced, as participants with missing creatinine and cystatin C values and those without complete data on frailty were excluded. Frailty may be common in people with severely impaired kidney function. However, given that serum cystatin C doesn’t increase in individuals with severe renal impairment as serum creatinine does [44], we eliminated participants with eGFR < 30 mL/ (min×1.73 m2) from this study, which may also have introduced bias. Third, residual confounding from unmeasured and unreported variables cannot be ruled out, despite that we have adjusted for multiple covariates in the multivariate analysis. For example, dietary intake and nutritional status were not assessed in CHARLS, whereas they can affect the level of creatinine [45], which may potentially bias our results. Finally, CCR was measured only once during the study period, and the effect of changes in CCR over time on frailty remains uncertain and requires further study.
Conclusions
Higher CCR was significantly associated with lower frailty in older adults. As creatinine and cystatin C are routinely available in clinical practice, CCR may be used as a promising cost-effective marker to identify individuals at risk of frailty for prompting the implementation of early interventions to postpone the frailty progression. More studies are warranted to verify our results and to evaluate its generalized application.
Data availability
The datasets used and/or analysed during the current study are available from the website of China Health and Retirement Longitudinal Study at http://charls.pku.edu.cn/en.
Abbreviations
- CCR:
-
Creatinine-to-cystatin C ratio
- PFP:
-
Physical frailty phenotype
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- CHARLS:
-
The China Health and Retirement Longitudinal Study
- eGFR:
-
Estimated glomerular filtration rate
- CVs:
-
Coefficients of variation
- BMI:
-
Body mass index
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- GEE:
-
Generalized estimating equations
- hs-CRP:
-
High-sensitivity C-reactive protein
References
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394:1365–75.
Kojima G. Frailty as a predictor of Future Falls among Community-Dwelling Older people: a systematic review and Meta-analysis. J Am Med Dir Assoc. 2015;16:1027–33.
Kojima G. Frailty as a predictor of disabilities among community-dwelling older people: a systematic review and meta-analysis. Disabil Rehabil. 2017;39:1897–908.
Mousa A, Savva GM, Mitnitski A, Rockwood K, Jagger C, Brayne C, et al. Is frailty a stable predictor of mortality across time? Evidence from the cognitive function and ageing studies. Age Ageing. 2018;47:721–7.
Cunha AIL, Veronese N, de Melo Borges S, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: a systematic review and meta-analysis. Ageing Res Rev. 2019;56:100960.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60:1487–92.
Kojima G. Prevalence of Frailty in nursing homes: a systematic review and Meta-analysis. J Am Med Dir Assoc. 2015;16:940–5.
Larsson L, Degens H, Li M, Salviati L, Lee YI, Thompson W, et al. Sarcopenia: aging-related loss of muscle Mass and function. Physiol Rev. 2019;99:427–511.
Landi F, Calvani R, Cesari M, Tosato M, Martone AM, Bernabei R, et al. Sarcopenia as the Biological substrate of physical Frailty. Clin Geriatr Med. 2015;31:367–74.
Wilson D, Jackson T, Sapey E, Lord JM. Frailty and Sarcopenia: the potential role of an aged immune system. Ageing Res Rev. 2017;36:1–10.
Feng H, Wang X, Mao L, Yu Z, Cui B, Lin L, et al. Relationship between sarcopenia/myosteatosis and frailty in hospitalized patients with cirrhosis: a sex-stratified analysis. Ther Adv Chronic Dis. 2021;12:20406223211026996.
Laskou F, Fuggle NR, Patel HP, Jameson K, Cooper C, Dennison E. Associations of osteoporosis and sarcopenia with frailty and multimorbidity among participants of the Hertfordshire Cohort Study. J Cachexia Sarcopenia Muscle. 2022;13:220–9.
Mehta M, Louissaint J, Parikh NS, Long MT, Tapper EB. Cognitive function, Sarcopenia, and inflammation are strongly Associated with Frailty: a Framingham Cohort Study. Am J Med. 2021;134:1530–8.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Biol Sci Med Sci. 2004;59:255–63.
Tang T, Xie L, Hu S, Tan L, Lei X, Luo X, et al. Serum creatinine and cystatin C-based diagnostic indices for Sarcopenia in advanced non-small cell lung cancer. J Cachexia Sarcopenia Muscle. 2022;13:1800–10.
Osaka T, Hamaguchi M, Hashimoto Y, Ushigome E, Tanaka M, Yamazaki M, et al. Decreased the creatinine to cystatin C ratio is a surrogate marker of Sarcopenia in patients with type 2 diabetes. Diabetes Res Clin Pract. 2018;139:52–8.
Kashani KB, Frazee EN, Kukralova L, Sarvottam K, Herasevich V, Young PM, et al. Evaluating muscle Mass by using markers of kidney function: development of the Sarcopenia Index. Crit Care Med. 2017;45:e23–9.
Kusunoki H, Tabara Y, Tsuji S, Wada Y, Tamaki K, Nagai K, et al. Estimation of muscle Mass using Creatinine/Cystatin C ratio in Japanese Community-Dwelling Older people. J Am Med Dir Assoc. 2022;23:902. e921-902 e931.
Lin YL, Chen SY, Lai YH, Wang CH, Kuo CH, Liou HH, et al. Serum creatinine to cystatin C ratio predicts skeletal muscle mass and strength in patients with non-dialysis chronic kidney disease. Clin Nutr. 2020;39:2435–41.
Ding P, Guo H, Sun C, Chen S, Yang P, Tian Y, et al. Serum creatinine/cystatin C ratio is a systemic marker of Sarcopenia in patients with gastrointestinal stromal tumours. Front Nutr. 2022;9:963265.
Hirai K, Tanaka A, Homma T, Goto Y, Akimoto K, Uno T, et al. Serum creatinine/cystatin C ratio as a surrogate marker for Sarcopenia in patients with chronic obstructive pulmonary disease. Clin Nutr. 2021;40:1274–80.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43:61–8.
Li D, Yin W, Yi Y, Zhang B, Zhao J, Zhu C, et al. Development and validation of a more accurate estimating equation for glomerular filtration rate in a Chinese population. Kidney Int. 2019;95:636–46.
Okubo N, Yoshida T, Tanaka K, Okada N, Hosoi K, Ohara M, et al. Serum creatinine to cystatin C ratio reflects preoperative and early postoperative walking ability in older patients with hip fracture. J Cachexia Sarcopenia Muscle. 2022;13:945–54.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Biol Sci Med Sci. 2001;56:M146–156.
Wu C, Smit E, Xue QL, Odden MC. Prevalence and correlates of Frailty among Community-Dwelling Chinese older adults: the China Health and Retirement Longitudinal Study. J Gerontol Biol Sci Med Sci. 2017;73:102–8.
Li Y, Xue QL, Odden MC, Chen X, Wu C. Linking early life risk factors to frailty in old age: evidence from the China Health and Retirement Longitudinal Study. Age Ageing. 2020;49:208–17.
Xu W, Li YX, Wu C. Incidence of frailty among community-dwelling older adults: a nationally representative profile in China. BMC Geriatr. 2019;19:378.
Lin T, Jiang T, Huang X, Xu P, Liang R, Song Q et al. Diagnostic test accuracy of serum creatinine and cystatin C-based index for Sarcopenia: a systematic review and meta-analysis. Age Ageing. 2024;53.
Stevens LA, Schmid CH, Greene T, Li L, Beck GJ, Joffe MM, et al. Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int. 2009;75:652–60.
Aloisio KM, Swanson SA, Micali N, Field A, Horton NJ. Analysis of partially observed clustered data using generalized estimating equations and multiple imputation. Stata J. 2014;14:863–83.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62.
Collins KH, Herzog W, MacDonald GZ, Reimer RA, Rios JL, Smith IC, et al. Obesity, metabolic syndrome, and Musculoskeletal Disease: common inflammatory pathways suggest a Central Role for loss of muscle Integrity. Front Physiol. 2018;9:112.
Yeung CHC, Au Yeung SL, Fong SSM, Schooling CM. Lean mass, grip strength and risk of type 2 diabetes: a bi-directional mendelian randomisation study. Diabetologia. 2019;62:789–99.
Kim SR, Lee G, Choi S, Oh YH, Son JS, Park M, et al. Changes in predicted lean body mass, appendicular skeletal muscle mass, and body fat mass and cardiovascular disease. J Cachexia Sarcopenia Muscle. 2022;13:1113–23.
Dai H, Xu J. Creatinine-to-cystatin C ratio as a marker of Sarcopenia for identifying osteoporosis in male patients with type 2 diabetes mellitus. BMC Musculoskelet Disord. 2022;23:672.
Qiu S, Cai X, Xie B, Yuan Y, Sun Z, Wu T. Normalized creatinine-to-cystatin C ratio and risk of diabetes in Middle-aged and older adults: the China Health and Retirement Longitudinal Study. Diabetes Metab J. 2022;46:476–85.
Hashimoto Y, Takahashi F, Okamura T, Osaka T, Okada H, Senmaru T, et al. Relationship between serum creatinine to cystatin C ratio and subclinical atherosclerosis in patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2022;10:e002910.
Shin JY. Low serum creatinine to cystatin C ratio is independently associated with Sarcopenia and high carotid plaque score in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2022;32:1454–62.
Lu YW, Tsai YL, Chou RH, Kuo CS, Chang CC, Huang PH, et al. Serum creatinine to cystatin C ratio is associated with major adverse cardiovascular events in patients with obstructive coronary artery disease. Nutr Metab Cardiovasc Dis. 2021;31:1509–15.
Zhu Y, Guo X, Zhang X, Shi X, Yang Y, Zhang Q. Sex differences in the relationship of serum creatinine to cystatin C ratio and depressive symptoms among middle-aged and older adults in China. J Affect Disord. 2022;319:57–61.
Zhu Y, Tan Z, Li S, Zhu F, Qin C, Zhang Q, et al. Serum creatinine to cystatin C ratio and cognitive function among middle-aged and older adults in China. Front Aging Neurosci. 2022;14:919430.
Qiu S, Cai X, Yuan Y, Xie B, Sun Z, Wu T. Changes in creatinine-to-cystatin C ratio over 4 years, risk of diabetes, and cardiometabolic control: the China Health and Retirement Longitudinal Study. J Diabetes. 2021;13:1025–33.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Performance of serum cystatin C versus serum creatinine as a marker of glomerular filtration rate as measured by inulin renal clearance. Clin Exp Nephrol. 2011;15:868–76.
Patel SS, Molnar MZ, Tayek JA, Ix JH, Noori N, Benner D, et al. Serum creatinine as a marker of muscle mass in chronic kidney disease: results of a cross-sectional study and review of literature. J Cachexia Sarcopenia Muscle. 2013;4:19–29.
Acknowledgements
We thank all participants and staff for their great contributions. We also sincerely appreciate the China Health and Retirement Longitudinal Study team for providing data.
Funding
This work was supported by grants from Sichuan Science and Technology Program (2022ZDZX0021, 2023ZYD0173, 2024YFHZ0072, 2022YFS0294), 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC21005), National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z2023LC006), and Health Research of Cadres in Sichuan province (SCR2022-101).
Author information
Authors and Affiliations
Contributions
QS: conceptualization, data acquisition, data curation, data analysis and interpretation, writing the original draft, and review and editing of the manuscript. TL: data curation, data analysis and interpretation, and review and editing of the manuscript. RL: data analysis and interpretation, and review and editing of the manuscript. YZ: data interpretation, and review and editing of the manuscript. NG: conceptualization, interpretation, and review and editing of the manuscript. JY: conceptualization, and critical revision of the manuscript.All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conformed to the ethical guidelines of the Declaration of Helsinki. The Ethics Review Committee of Peking University (IRB00001052-11015) approved CHARLS. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Song, Q., Lin, T., Liang, R. et al. Creatinine-to-cystatin C ratio and frailty in older adults: a longitudinal cohort study. BMC Geriatr 24, 753 (2024). https://doi.org/10.1186/s12877-024-05326-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05326-1