Abstract
Background
The escalating global prevalence of polypharmacy presents a growing challenge to public health. In light of this issue, the primary objective of our study was to investigate the status of polypharmacy and its association with clinical outcomes in a large sample of hospitalized older patients aged 65 years and over.
Methods
A two-year prospective cohort study was carried out at six tertiary-level hospitals in China. Polypharmacy was defined as the prescription of 5 or more different medications daily, including over-the-counter and non-prescription medications. Baseline polypharmacy, multimorbidity, and other variables were collected when at admission, and 2-year outcomes were recorded by telephone follow-up. We used multivariate logistic regression analysis to examine the associations between polypharmacy and 2-year outcomes.
Results
The overall response rate was 87.2% and 8713 participants were included in the final analysis. The mean age was 72.40 years (SD = 5.72), and women accounted for 42.2%. The prevalence of polypharmacy among older Chinese inpatients is 23.6%. After adjusting for age, sex, education, marriage status, body mass index, baseline frailty, handgrip strength, cognitive impairment, and the Charlson comorbidity index, polypharmacy is significantly associated with frailty aggravation (OR 1.432, 95% CI 1.258–1.631) and mortality (OR 1.365, 95% CI 1.174–1.592), while inversely associated with readmission (OR 0.870, 95% CI 0.764–0.989). Polypharmacy was associated with a 35.6% increase in the risk of falls (1.356, 95%CI 1.064–1.716). This association weakened after adjustment for multimorbidity to 27.3% (OR 1.273, 95%CI 0.992–1.622).
Conclusions
Polypharmacy was prevalent among older inpatients and was a risk factor for 2-year frailty aggravation and mortality. These results highlight the importance of optimizing medication use in older adults to minimize the risks associated with polypharmacy. Further research and implementing strategies are warranted to enhance the quality of care and safety for older individuals exposed to polypharmacy.
Trial registration
Chinese Clinical Trial Registry, ChiCTR1800017682, registered 09/08/2018.
Similar content being viewed by others
Background
As the technical report from the World Health Organization [1] states, polypharmacy is the concurrent use of multiple medications. Although there is no standard definition of polypharmacy, it is often defined as the routine use of five or more medications, including over-the-counter, prescription, and/or traditional and complementary medicines use [2]. Polypharmacy is a significantly increasing threat to global health as a result of multimorbidity and the consequent associated use of various medicines [3, 4]. At least one-third (33.7%) of people who developed a non-communicable disease (NCD), such as diabetes, chronic lung disease, or heart failure, were diagnosed with multiple NCDs in their lifetime [5]. It was estimated that the prevalence of 2 or more chronic diseases among Chinese older people aged 60 and above reached 31.8% [6]. Evidence-based clinical guidelines and care pathways [7] commonly recommend the simultaneous use of multiple drugs for treatment and prevention in older patients with multimorbidity. It is estimated that the prevalence of polypharmacy among hospitalized olders was 56.32% [8], and higher than that of nursing home residents and community-dwelling older people [9, 10]. These statistics highlight the need for multiple medications use in patient care. However, it is crucial to recognize that the appropriateness of polypharmacy should be carefully evaluated in this population. The older are at greater risk of adverse effects due to decreased renal and hepatic function, lower lean body mass, and reduced hearing, vision, cognition, and mobility [11]. For instance, decreased liver and kidney function leads to a decline in the elimination of several drugs. Therefore, a comprehensive assessment of polypharmacy is essential to ensure optimal treatment while minimizing potential harm.
It is paramount to thoroughly consider the risks and benefits of polypharmacy in the context of managing multimorbidity. Some studies [12,13,14,15,16] have examined that polypharmacy is linked to negative clinical outcomes such as adverse drug reactions, drug-related events, physical and cognitive functions, healthcare utilization outcomes, or mortality. However, the literature examining the adverse outcomes of polypharmacy in older people is complex, extensive, and conflicting [17]. These findings emphasize the need to address the appropriateness of polypharmacy specifically in the inpatient setting and explore its association with adverse outcomes. In this report, we aimed to determine the association between polypharmacy and clinical outcomes through adjusting multimorbidity, considered as significant confounding, in a prospective cohort study. We sought to add more evidence for a better understanding of polypharmacy and clinically relevant consequences in the face of rising multimorbidity and population ageing.
Methods
Study design and participants
We performed a prospective cohort study to investigate older inpatients aged 65 years and over. To ensure nationally representative samples, we selected one tertiary-level hospital from each of the six administration regions of China, taking into account the geographical distribution and economic level. Within each selected hospital, all older inpatients in the included Internal Medicine, Surgical, Neurology, Orthopedics departments and Intensive Care Units of these hospitals that met the criterion were continuously enrolled from October 2018, through February 2019. The inclusion criteria for participants were as follows: Age ≥ 65 years; Willingness to provide informed consent and actively participate in this study. Patients who exhibited persistent impairment of consciousness or communication, rendering them unable to effectively communicate, along with their caregivers who were unable to provide necessary information, were excluded from the study. Both the baseline survey and telephone follow-up after two years were carried out by 589 well-trained registered nurses. In total, 9996 older inpatients completed the baseline survey and 1283 persons were removed for failure to follow up at 2 years. The overall response rate was 87.2% and 8713 participants were included in the final analysis (Fig. 1). The trial is registered at the Chinese Clinical Trial Registry with registration number ChiCTR1800017682 on 09/08/2018.
The Ethics Committee of Peking Union Medical College Hospital approved the study protocol(SK-400). Written informed consent was obtained from each participant (when collection started) before data collection.
Measurement instruments
Assessment of polypharmacy
Polypharmacy was defined as the prescription of 5 or more different medications daily. The types of polypharmacy included over-the-counter and non-prescription medicines, and we excluded Chinese herbal medicines and health products. The number of medication use was investigated at baseline survey when at admission, which collected patients’ recent drug use through the medical orders list.
Assessment of multimorbidity
Multimorbidity was defined as the coexistence of 2 or more chronic conditions [18]. In our study, multimorbidity was assessed according to the list of diagnoses at admission based on the 10th International Statistical Classification of Diseases (ICD-10). We determined the Charlson Comorbidity Index (CCI) to serve as proxies of participants’ chronic disease statuses. The Charlson Comorbidity Index employs a systematic assignment method for each type of disease to quantify comorbidities in patients [19]. The total score of the CCI consists of a simple sum of the weights, with higher scores indicating more severe comorbidity conditions and greater mortality risk [20].
Association between polypharmacy and health outcomes
Our outcomes of interest were 2-year falls, frailty aggravation, all-cause readmission, and mortality.
-
1.
Falls.
The well-trained nurses completed telephone follow-ups according to a standard procedure. We recorded patients’ falls by self-reported “Yes/No” without times.
-
2.
Frailty aggravation.
Baseline and 2-year frailty status were assessed according to our protocol by using the FRAIL scale [21], which consists of 5 simple self-reported questions, including fatigue, resistance, ambulation, illness, and loss of weight. Baseline assessment was completed by face-to-face interview, 2-year frailty status of participants was accessed through telephone follow-up. For fatigue, investigators asked, “Did you (all or most of the time) feel tired in the past 4 weeks?”. If the answer was “yes”, then they scored 1 point, otherwise, they scored 0 points. For resistance, “Did you feel difficult to walk 10 steps without aid?” (“yes” = 1, “no” = 0). For illness, “Has the doctor ever told you that you have more than five illnesses?” (“yes” = 1, “no” = 0). For ambulation, “Did you feel difficult to walk a quarter of a mile by yourself?” (“yes” = 1, “no” = 0). Weight loss: “Did you lose 5% of your total weight in the past 6 months?” (“yes” = 1, “no” = 0). The FRAIL scale scores ranged from 0 to 5, which represent frail (3–5), pre-frail (1–2), and robust (0). Frailty aggravation included inpatients who transitioned from robust to pre-frail or frail, and from pre-frail to frail over a 2-year follow-up period.
-
3.
Readmission.
The investigators asked patients to recall readmissions in the previous 2 years and recorded “Yes/No” without times.
-
4.
Mortality.
The investigators got in contact with inpatients or their families, and if their family informed that the patient had died, then they recorded it as mortality and ended the investigation. Specific times of death were not obtained due to online data collection constraints and limited access to detailed medical records.
Other covariates
In addition to sociodemographic data including age, sex, education, ethnicity, BMI, marital status, smoking, and alcohol consumption, we assessed other geriatric syndromes including baseline frailty status, cognitive impairment and handgrip strength. Of sociodemographics, levels of education were classified as illiterate, primary school, middle school and diploma and above. Ethnicity included two categories as the Han nationality and other nationalities. Body mass index (BMI, weight divided by the square of height) was categorized as underweight (BMI < 18.5 kg/m2), normal (18.5 ≤ BMI < 24 kg/m2), overweight (24 ≤ BMI < 28 kg/m2) and obesity (≥ 28 kg/m2) [22]. Martial status included married and divorced or widowed. Smoking and alcohol consumption were grouped as non-smoker, current smoker and former smoker, and non-drinker, current drinker and former drinker, respectively. The baseline frailty status was assessed as described earlier. As for covariate, pre-frail and frail were grouped into frailty, and robust was grouped into non-frailty. We used the Mini-Cog Scale to assess cognitive function and recognized cognitive impairment by Mini-Cog Scale score < 2 [23]. Handgrip strength with the dominant hand was measured by using a dynamometer while sitting, and low handgrip strength was defined as a two-categorical variable with cut-points of 28 kg in men and 18 kg in women [24].
Statistical analysis
Continuous variables were expressed as means (standard deviations, SD), categorical variables as frequencies (percentages), and non-normally distributed covariates as median and interquartile range. We used χ2 tests to compare categorical variables and t tests or analyses of variance (ANOVA) to compare continuous variables. To examine the associations between polypharmacy and 2-year outcomes, we employed multivariate logistic regression analysis in three models: an unadjusted model, an adjusted model 1, and an adjusted model 2. Model 1 adjusted for demographic and baseline health variables, including age, sex, education, marriage status, BMI, baseline frailty, handgrip strength, and cognitive impairment, based on existing literature and professional judgment. Model 2 included all variables from Model 1 and additionally adjusted for the Charlson comorbidity index to account for the overall comorbidity burden. When examining the association between polypharmacy and 2-year frailty aggravation, we adjusted all variables except baseline frailty in model 1 and 2. We determined the association with a binomial distribution presented as the Odds ratio (OR) and 95% confidence interval (95% CI). A two-sided p < 0.05 is considered as a statistically significant result. All the statistical analyses were carried out by SAS® Proprietary Software version 9.4 (SAS Institute, Cary, NC, USA).
Results
Characteristics of study participants
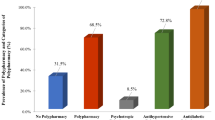
Table 1 shows the baseline characteristics of the study population. We identified 8713 hospitalized patients (2055 [23.6%] polypharmacy, 6658 [76.4%] non-polypharmacy). The mean age of this sample was 72.40 years (SD = 5.72), women accounted for 42.25%, and the prevalence of underweight and obesity was 6.70% and 9.85%, respectively. 52.08% of the older inpatients had low handgrip strength, and 19.04% presented cognitive impairment.
At baseline, the incidence of polypharmacy increases with age. The proportion of inpatients with polypharmacy was highest in the 85 + age group (39.51%). Older people with higher levels of education were more likely to experience polypharmacy (18.69% of illiterate, 22.49% of middle school, 25.61% of middle school, 25.56% of diploma and above, P < 0.0001, Supplementary Table 1). Current smokers and former smokers had a higher prevalence of polypharmacy than non-smokers, while the only significant difference is between former smokers (27.44%) and current/non-smokers (22.77% and 22.39%, respectively, P < 0.0001). No differences in medication use were found concerning alcohol consumption. In addition, inpatients with polypharmacy were more likely to have low handgrip strength(26.29%, P < 0.0001) and cognitive impairment (26.64%, P = 0.0015) compared to inpatients without polypharmacy. Older patients with a higher disease burden have a higher incidence of polypharmacy.
Association between polypharmacy and health outcomes
As of the two-year date at follow-up, 1510 (17.33%) older inpatients had died, 2071 (23.77%) inpatients reported all-cause readmissions, 366 (4.20%) and 708(8.13%) inpatients experienced falls and frailty aggravation respectively (Table 2). We also conducted a sensitivity analysis dividing “polypharmacy” into 3 groups (< 3 drugs; 3 ∼ 4 drugs; ≥5 drugs). The results and discussion were presented in the supplementary materials (Supplementary Table 2).
Falls
For the unadjusted model of self-reported falls, polypharmacy was associated with a 35.6% increase in the risk of falls (OR 1.356, 95%CI 1.064–1.716). This association was not statistically significant after fully adjusting for covariates including multimorbidity (OR 1.273, 95%CI 0.992–1.622; Table 3). The non-significant finding may be due to insufficient statistical power, as the sample size (n = 366 with 2-year falls; Table 2) may not have been large enough to detect a significant difference.
Frailty aggravation
Older patients with polypharmacy had significantly higher odds of frailty aggravation in two years compared with those who did not receive polypharmacy (OR 1.367, 95%CI 1.114–1.676). Multimorbidity is strongly associated with frailty deterioration [25], after adjusting for the CCI, this association slightly increased (OR 1.432, 95%CI 1.258–1.631; Table 3). As for this outcome, we created a new variable for frailty status transition as a four-categorical variable, including frailty aggravation, consistent frailty, frailty improvement, and consistent non-frailty. The association between polypharmacy and other frailty status transition or 2-year frailty status were presented in Supplementary Tables 3 and 4.
Readmission
The association between polypharmacy and all-cause readmission was not statistically significant (OR 0.996, 95% CI 0.855–1.091). After adjusting for covariates, inpatients with polypharmacy had a lower risk of readmission compared to inpatients without multiple drug use (OR 0.870, 95% CI 0.764–0.989; Table 3).
Mortality
As shown in Table 3, inpatients with polypharmacy had slightly higher odds of mortality in the unadjusted model (OR 1.162, 95%CI 1.012–1.337). We then adjusted sex, age, education, marital status, BMI, frailty, handgrip strength, and cognition impairment, this association still existed (OR 1.322, 95%CI 1.141–1.536). After fully adjusting variables by adding the CCI score, this association significantly increased (OR 1.365, 95%CI 1.174–1.592).
Discussion
This cohort study demonstrates that polypharmacy is highly prevalent (23.6%) among older inpatients, while this prevalence is relatively low compared to other studies of hospitalized patients [26, 27]. Since the study included hospitals from various regions of China, with diverse geographical and economic backgrounds, this prevalence could reflect general medicine use conditions. Some regions may have strict prescribing practices, contributing to the lower observed prevalence. Correlation analysis indicated that polypharmacy is significantly associated with frailty aggravation and mortality among older inpatients (P < 0.0001), while it is not related to falls and is inversely associated with readmission within two years. However, it is worth noting that regarding the sample size of deaths, which accounted for 17.33% of total cases, we were unable to obtain outcome ratings for their falls, frailty, and readmission. It is necessary to consider that a higher number of adverse outcomes may have occurred in those inpatients who died. Therefore, the role of polypharmacy in our results may have been underestimated.
Falls
This study illustrated that compared to inpatients who did not experience multiple drug use, inpatients with polypharmacy had a higher risk of falls. Polypharmacy increases the incidence of drug-drug interactions and drug-disease interactions and its adverse effects lead to an increased risk of falls. Gait disturbance mediates the relationship between medication quantity and incidence of falls [28], e.g., polypharmacy may cause reduced walking speed and shortened stride length in older adults, which directly affects their gait stability and thus increases the incidence of falls. Furthermore, polypharmacy (taking four or more prescription medications daily) was positively associated with recurrent falls, particularly psychotropic drugs. Recurrent fallers demonstrate less confidence in their ability to perform daily activities and have an increasing likelihood of admission [29]. In addition to the number of medications being a critical factor for falls among older people, the types or quality indicators of medication use are associated with the risk of fall occurrence. The presence of multiple fall risk-increasing drugs (FRIDs) in prescription is an independent risk factor for falls, even in patients with few medications [30]. FRIDs can also contribute to falls by causing gait disturbances, especially drugs with sedative properties [31]. Of all the deprescribing tools, potentially inappropriate medications (PIMs) have been independently associated with inpatient falls [32].
In summary, polypharmacy is a critical indicator of falls among older patients. However, falls in the older are multifactorial and may be a direct result of physical illness or frailty [33]. Recurrent fallers have a greater need to prevent falls, and medications are considered modifiable risk factors [29]. Currently, there is insufficient evidence on the risk-benefit ratio of prescribing multiple medications versus the potential benefits of preventive deprescribing [34, 35]. More evidence is needed to clarify the effectiveness of reducing the number of FRIDs or medicines in reducing the incidence of falls and to inform the management of polypharmacy.
Frailty aggravation
Polypharmacy has a persistent and negative effect on the overall health of older persons, leading to exacerbation of frailty. Polypharmacy increases the risk of drug-drug interactions and side effects, which can lead to a decline in body functions and the development of frailty. There is a complex interplay between polypharmacy, multimorbidity, and frailty. While polypharmacy is entangled with several geriatric syndromes including frailty, falls, and cognitive impairment [36], the causal relationship between these factors has not been determined. Even with cohort studies where polypharmacy is measured at baseline and frailty aggravation is tracked over time, it remains unclear what is the original cause and what are the consequences. Polypharmacy may lead to increased frailty, but it is also plausible that frail individuals are more likely to be prescribed multiple medications due to their complex health needs.
Polypharmacy is associated with a wide range of adverse health outcomes, especially amplified in those individuals with frailty [37]. In addition to frailty aggravation, frail older patients with polypharmacy are less likely to experience improvement in their frail status compared to patients without polypharmacy [37]. Healthcare providers should conduct thorough pharmaceutical reviews for frail older adults to reduce unnecessary drug use and minimize side effects [38]. This approach can help prevent more severe adverse outcomes and promote the restoration of physical condition.
In patients with comorbidities and frailty, the risk-benefit ratio of specific drugs tends to increase due to reduced functional reserve and impaired compensatory mechanisms [39]. As frailty is a dynamic syndrome [40], it should be noted that the relationship between polypharmacy and frailty is complex and influenced by various factors, such as mobility levels, appropriateness of medication selection, and accuracy of dosage management may impact this association. Further research is needed to explore the roles of underlying factors and provide more specific guidance and intervention measures.
Readmission
Polypharmacy does not show a positive relationship with 2-year readmission. Previous studies have shown that potentially inappropriate medication use, not polypharmacy, was associated with readmission [41]. However, Lu et al. analyzed medication use by measuring it quarterly and incorporating it as time-varying variables in their model analysis, both polypharmacy and potentially inappropriate medication use were associated with fracturespecific admissions with dose-response relations [42]. Drug-related readmission (DRA) is defined as readmission due to an adverse drug reaction as a primary or significant cause, for which polypharmacy is a significant predictor [43]. These findings might suggest that medication use, frailty and comorbidity each act on adverse health outcomes through their parallel pathophysiological mechanism. This result also might suggest that inpatients with polypharmacy may reflect a higher degree of concern about health conditions, leading to polypharmacy as a protective factor for readmission statistically. In conclusion, measurement of drug exposure may lead to different conclusions on study outcomes, while the role of polypharmacy on patient readmission cannot be ignored, and high-level medication review interventions reduce hospitalization rates and improve outcomes more significantly in hospitalized patients [44]. Interventions such as comprehensive clinical evaluation for disease management in hospitalized patients on multiple medications are necessary.
Mortality
This study also confirmed the polypharmacy-mortality association, which has been controversial. Zhao et al. [8] conducted a retrospective cross-sectional study and revealed that polypharmacy was associated with a reduction in mortality. Pozzi et al. [41] showed that in univariate analysis, mortality was two-fold higher in participants with polypharmacy, while when performing multivariable Cox regression analysis models, polypharmacy was no longer associated with an increased risk of mortality. However, a dose-response relationship exists between polypharmacy and all-cause mortality in longer-term longitudinal studies [45]. Chang et al. [46] adjusted for age, sex, residential area, and CCI score in the multivariate Cox models and reported that polypharmacy was associated with significantly a higher risk of mortality. The present study adequately adjusted for baseline frailty, multimorbidity and other confoundings, and the association remained. The result indicated that polypharmacy and the range of medicine use problems that arise from it, including potential inappropriate prescribing, adverse drug-drug interactions and adverse drug-disease interactions, prescribing cascades [45,46,47,48], increase the risk of death in hospitalized patients. Some studies have been carried out to examine the effectiveness of medication review [49] or non-pharmacological interventions [50] for older patients to minimise the exposure of older inpatients to medication-related harm.
Limitations
Several limitations of this study have to be addressed. First, the calculation of multiple drugs use in this study was based on the self-reported number of medications counted by the inpatients at the time of admission, which may cause recollection bias. Second, we did not collect and analyze specific information on drug prescriptions, such as types of drugs or potentially inappropriate medications, anticholinergic burden, and the efficacy of polypharmacy may be overestimated based on the number of drugs rather than quality. Third, the outcomes were reported by patients through dial follow-up, resulting in possible subjective recollection bias. Furthermore, by only considering fall occurrence, rather than the number of falls experienced by participants, the current analysis may fail to capture the full extent of the relationship between polypharmacy and fall risk. The frequency of falls can provide a more comprehensive understanding of developing targeted interventions and understanding the clinical implications of polypharmacy in the context of falls among older adults. Patients who died within two years after the baseline investigation were likely to have been readmitted to the hospital before their death, and only the outcome, mortality, was recorded through telephone follow-up with their families. These cases were not included in the analyses of polypharmacy with other health outcomes, and as mentioned above, the impact of polypharmacy may have been underestimated. For future research, time-to-event analysis methods such as Cox proportional hazards models and Kaplan-Meier curves are particularly useful for analyzing the timing and probability of events over a period. These methods could provide more nuanced insights into the dynamics between polypharmacy and outcomes like mortality.
Conclusion
Polypharmacy and multimorbidity were prevalent among hospitalized patients aged ≥ 65 years. Polypharmacy (≥ 5 medications) had an increased risk of 2-year frailty aggravation and mortality, showing that a re-evaluation of polypharmacy may be warranted and inpatients with polypharmacy still require more attention for adverse outcomes.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- ORs:
-
Odds ratios
- SD:
-
Standard deviation
- NCD:
-
Non-communicable disease
- BMI:
-
Body mass index
- CCI:
-
Charlson Comorbidity Index
- FRID:
-
Fall risk-increasing drug
- PIM:
-
Potentially inappropriate medication
- DRA:
-
Drug-related readmission
References
Medication safety in polypharmacy: technical report. Accessed December 23. 2023. https://www.who.int/publications-detail-redirect/WHO-UHC-SDS-2019.11
Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. 2021;12(3):443–52. https://doi.org/10.1007/s41999-021-00479-3
Mr M, Sg M, Km J, et al. Association of polypharmacy and potential drug-drug interactions with adverse treatment outcomes in older adults with advanced cancer. Cancer. 2023;129(7). https://doi.org/10.1002/cncr.34642
G K. Polypharmacy: the challenge for nurses. Nurs Stand R Coll Nurs G B 1987. 2016;30(39). https://doi.org/10.7748/ns.30.39.52.s45
Licher S, Heshmatollah A, van der Willik KD, et al. Lifetime risk and multimorbidity of non-communicable diseases and disease-free life expectancy in the general population: a population-based cohort study. PLoS Med. 2019;16(2):e1002741. https://doi.org/10.1371/journal.pmed.1002741
Z JF, C S. Multimorbidity patterns and association with mortality in 0.5 million Chinese adults. Chin Med J (Engl). 2022;135(6). https://doi.org/10.1097/CM9.0000000000001985
As B, Nk C. Evidence-based prescribing and polypharmacy for patients with heart failure. Ann Intern Med. 2021;174(8). https://doi.org/10.7326/M21-1427
Y Z. Multimorbidity and polypharmacy in hospitalized older patients: a cross-sectional study. BMC Geriatr. 2023;23(1). https://doi.org/10.1186/s12877-023-04109-4
D M, M L, J B, et al. Prevalence and factors associated with polypharmacy: a systematic review and Meta-analysis. BMC Geriatr. 2022;22(1). https://doi.org/10.1186/s12877-022-03279-x
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65. https://doi.org/10.1517/14740338.2013.827660
Andres TM, McGrane T, McEvoy MD, Allen BFS. Geriatric pharmacology: an update. Anesthesiol Clin. 2019;37(3):475–92. https://doi.org/10.1016/j.anclin.2019.04.007
AM, MW, TD. Addressing the challenge of Polypharmacy. Annu Rev Pharmacol Toxicol. 2020;60. https://doi.org/10.1146/annurev-pharmtox-010919-023508
Ra KRKB. Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults. Age Ageing. 2015;44(1). https://doi.org/10.1093/ageing/afu141
Rawle MJ, Cooper R, Kuh D, Richards M. Associations between Polypharmacy and cognitive and physical capability: a British birth Cohort Study. J Am Geriatr Soc. 2018;66(5):916–23. https://doi.org/10.1111/jgs.15317
Saum KU, Schöttker B, Meid AD, et al. Is Polypharmacy Associated with Frailty in Older people? Results from the ESTHER Cohort Study. J Am Geriatr Soc. 2017;65(2):e27–32. https://doi.org/10.1111/jgs.14718
Huang YT, Steptoe A, Wei L, Zaninotto P. Dose–response relationships between Polypharmacy and all-cause and cause-specific mortality among older people. J Gerontol Ser A. 2022;77(5):1002–8. https://doi.org/10.1093/gerona/glab155
Le D, A GSAK. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc. 2020;21(2). https://doi.org/10.1016/j.jamda.2019.10.022
Organization WH. The World Health Report 2008: Primary Health Care Now More than Ever. World Health Organization; 2008. Accessed January 13, 2024. https://iris.who.int/handle/10665/43949
Me C, Kl PP, Cr A. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5). https://doi.org/10.1016/0021-9681(87)90171-8
C VSTH, Wa PAMHQ. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12). https://doi.org/10.1016/j.jclinepi.2004.03.012
van Abellan G, Rolland Y, Bergman H, Morley JE, Kritchevsky SB, Vellas B. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12(1):29–37. https://doi.org/10.1007/BF02982161
The Chinese National Health Commission Health Industry Standards of the People’s Republic of China—Criteria of Weight for Adults.pdf. Accessed February 5. 2024. http://www.nhc.gov.cn/ewebeditor/uploadfile/2013/08/20130808135715967.pdf
Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive vital signs measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15(11):1021–7. https://doi.org/10.1002/1099-1166(200011)15:11%3C1021::aid-gps234%3E3.0.co;2-6
Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–e3072. https://doi.org/10.1016/j.jamda.2019.12.012
Doi T, Makizako H, Tsutsumimoto K, et al. Transitional status and modifiable risk of frailty in Japanese older adults: a prospective cohort study. Geriatr Gerontol Int. 2018;18(11):1562–6. https://doi.org/10.1111/ggi.13525
Lai X, Zhu H, Huo X, Li Z. Polypharmacy in the oldest old (≥ 80 years of age) patients in China: a cross-sectional study. BMC Geriatr. 2018;18. https://doi.org/10.1186/s12877-018-0754-y
Tao L, Qu X, Gao H, Zhai J, Zhang Y, Song Y. Polypharmacy and potentially inappropriate medications among elderly patients in the geriatric department at a single-center in China: a retrospective cross-sectional study. Med (Baltim). 2021;100(42):e27494. https://doi.org/10.1097/MD.0000000000027494
Montero-Odasso M, Sarquis-Adamson Y, Song HY, Bray NW, Pieruccini-Faria F, Speechley M, Polypharmacy. Gait Performance, and Falls in Community-Dwelling older adults. Results from the Gait and Brain Study. J Am Geriatr Soc. 2019;67(6):1182–8. https://doi.org/10.1111/jgs.15774
Ming Y, Zecevic A. Medications & polypharmacy influence on recurrent fallers in Community: a systematic review. Can Geriatr J. 2018;21(1):14–25. https://doi.org/10.5770/cgj.21.268
K I EC, Rd B, Sm A. Fall risk-increasing drugs, polypharmacy, and Falls among Low-Income Community-Dwelling older adults. Innov Aging. 2021;5(1). https://doi.org/10.1093/geroni/igab001
Osman A, Kamkar N, Speechley M, Ali S, Montero-Odasso M. Fall risk-increasing drugs and gait performance in community-dwelling older adults: a systematic review. Ageing Res Rev. 2022;77:101599. https://doi.org/10.1016/j.arr.2022.101599
Ba DV, K R. Potentially inappropriate medications and their effect on falls during hospital admission. Age Ageing. 2022;51(1). https://doi.org/10.1093/ageing/afab205
Bennett A, Gnjidic D, Gillett M, et al. Prevalence and impact of fall-risk-increasing drugs, polypharmacy, and drug-drug interactions in robust versus frail hospitalised falls patients: a prospective cohort study. Drugs Aging. 2014;31(3):225–32. https://doi.org/10.1007/s40266-013-0151-3
Jm P et al. S D, R S,. Deprescribing electronic case reviews for older veterans at risk for falls: Effects on drug burden and falls. J Am Geriatr Soc. Published online August 11, 2023. https://doi.org/10.1111/jgs.18650
Ekc JLANRP. Deprescribing fall-risk increasing drugs (FRIDs) for the prevention of falls and fall-related complications: a systematic review and meta-analysis. BMJ Open. 2021;11(2). https://doi.org/10.1136/bmjopen-2019-035978
Rs M, Bd K, K K, Me E, At C. Emerging approaches to polypharmacy among older adults. Nat Aging. 2021;1(4). https://doi.org/10.1038/s43587-021-00045-3
Toh JJY, Zhang H, Soh YY, Zhang Z, Wu XV. Prevalence and health outcomes of polypharmacy and hyperpolypharmacy in older adults with frailty: a systematic review and meta-analysis. Ageing Res Rev. 2023;83:101811. https://doi.org/10.1016/j.arr.2022.101811
Tt H, C D. Association of Polypharmacy and potentially inappropriate medications with Frailty among older adults with blood cancers. J Natl Compr Cancer Netw JNCCN. 2022;20(8). https://doi.org/10.6004/jnccn.2022.7033
C. M. How polypharmacy affects frailty. Expert Rev Clin Pharmacol. 2020;13(11). https://doi.org/10.1080/17512433.2020.1829467
Kutner NG, Zhang R. Frailty as a dynamic process in a diverse cohort of older persons with dialysis-dependent CKD. Front Nephrol. 2023;3. https://doi.org/10.3389/fneph.2023.1031338
C P. Is suboptimal prescribing a risk factor for poor health outcomes in community-dwelling elders? The ICARe Dicomano study. Pharmacoepidemiol Drug Saf. 2010;19(9). https://doi.org/10.1002/pds.1997
Wh L, Yw W, Lk C, Fy H. Effect of polypharmacy, potentially inappropriate medications and anticholinergic burden on clinical outcomes: a retrospective cohort study. CMAJ Can Med Assoc J J Assoc Medicale Can. 2015;187(4). https://doi.org/10.1503/cmaj.141219
Bmg S, Tgh K, Ce A, et al. Drug-related readmissions in older hospitalized adults: external validation and updating of OPERAM DRA prediction tool. J Am Geriatr Soc. 2023;71(12). https://doi.org/10.1111/jgs.18575
Mizokami F, Mizuno T, Kanamori K, et al. Clinical medication review type III of polypharmacy reduced unplanned hospitalizations in older adults: a meta-analysis of randomized clinical trials. Geriatr Gerontol Int. 2019;19(12):1275–81. https://doi.org/10.1111/ggi.13796
Petrovic M, O’Mahony D, Cherubini A. Inappropriate prescribing: hazards and solutions. Age Ageing. 2022;51(2):afab269. https://doi.org/10.1093/ageing/afab269
B I, E J, E J, B O, H T. Fatal adverse drug events: the paradox of drug treatment. J Intern Med. 2001;250(4). https://doi.org/10.1046/j.1365-2796.2001.00892.x
Pallesen AVJ, Kristiansen M, Westendorp RGJ, Mortensen LH. Polypharmacy occurrence and the related risk of premature death among older adults in Denmark: a nationwide register-based cohort study. PLoS ONE. 2022;17(2):e0264332. https://doi.org/10.1371/journal.pone.0264332
Sternberg SA, Guy-Alfandary S, Rochon PA. Prescribing cascades in older adults. CMAJ Can Med Assoc J. 2021;193(6):E215. https://doi.org/10.1503/cmaj.201564
Rankin A, Cadogan CA, Patterson SM, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2018;9(9):CD008165. https://doi.org/10.1002/14651858.CD008165.pub4
Daunt R, Curtin D, O’Mahony D. Polypharmacy stewardship: a novel approach to tackle a major public health crisis. Lancet Healthy Longev. 2023;4(5):e228–35. https://doi.org/10.1016/S2666-7568(23)00036-3
Acknowledgements
The authors appreciate all the participants for their voluntary participation, and thanks for all the investigators for their work.
Funding
This work was supported by the Fundamental Research Funds for the Central Universities (3332020007); Project of Peking Union Medical College Hospital (ZC201910578). The funding bodies had no specific role in study design or data collection, analysis, and interpretation, or manuscript conception and writing.
Author information
Authors and Affiliations
Contributions
WX and JJ designed the study; XT and YM analysed and interpreted the data; LX and JJ designed the study and drafted the paper. ZR, ZX, ZX, WX, JJ, WH, LD, ZS carried out data acquisition and patient interview. The authors read approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Peking Union Medical College Hospital (S-K540). All included subjects gave their written informed consent forms to participate in the study.
Consent for publication
All subjects gave written consent for their accounts to be anonymously published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, X., Zhao, R., Zhou, X. et al. Association between polypharmacy and 2-year outcomes among Chinese older inpatients: a multi-center cohort study. BMC Geriatr 24, 748 (2024). https://doi.org/10.1186/s12877-024-05340-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05340-3