Abstract
Background
Older adults with hearing impairments are vulnerable to cognitive impairment. Although previous reports suggest a correlation between widowhood and cognitive impairment, further investigation is needed to elucidate the effect of widowhood on cognitive function and the moderating effects of social support and participation on widowhood-related cognitive impairment in this vulnerable demographic.
Methods
The study’s data were sourced from the nationally representative Chinese Longitudinal Healthy Longevity Survey (CLHLS) for the years 2011, 2014, and 2018. Multiple linear regression was used to analyze the association between widowhood and cognitive function among older adults. Multivariate logistic regression examined the effect of widowhood on the likelihood of experiencing various levels of cognitive impairment in older adults with hearing impairments. A moderating effect model explored the roles of social support and participation in mitigating widowhood-related cognitive impairment.
Results
The cognitive function of older adults with hearing impairment was found to be lower than that of those without hearing impairment. Widowhood was significantly negatively correlated with Mini-Mental State Examination (MMSE) scores in older adults, both with (Coef. = -0.898) and without (Coef.: = -0.680) hearing impairments. A stronger association was observed between widowhood and declining cognitive function among older adults with hearing impairment. Specifically, widowhood may be more likely to significantly increase the likelihood of moderate and severe cognitive impairment (RRR = 1.326, 1.538) among older adults with hearing impairments. Social support and social participation significantly moderated the cognitive impairment associated with widowhood among hearing-impaired older adults. These forms of support and engagement are buffers against the risk of widowhood-related cognitive impairment among this demographic.
Conclusions
Our findings indicate that widowhood is significantly associated with cognitive impairment in older adults with hearing impairment. Social support and participation help mitigate this risk. Strategies should prioritize early screening, specialized cognitive rehabilitation, comprehensive care, and enhancing social support and participation to maintain cognitive health in this vulnerable population following widowhood.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Cognitive impairment is characterized by a decline, loss, or difficulty in memory, attention, language, executive function, calculation, and other cognitive capacities. As the aging population continues to expand, cognitive impairment among older adults has emerged as a significant health concern in numerous countries and regions. It is estimated that over 55 million older adults worldwide have cognitive impairment [1]. Over 360,000 Chinese older adults are diagnosed with cognitive impairment every year, with a projected total of 48.68 million by 2060 [2]. Cognitive impairment diminishes the healthy lifespan of older adults, escalates the economic burden of the disease, and also strains community-based and societal long-term care systems [3]. The Health China 2030 plan issued in 2016 regarded controlling the prevalence of cognitive impairment diseases as one of the core indicators of health promotion behavior for older adults [4]. It clearly stated that strategies should be established from the three dimensions of individuals and families, government, and society.
Hearing impairment, a significant contributor to cognitive decline, has been consistently substantiated by studies. People with hearing impairment are 1.9 times more likely to develop cognitive impairment than those without hearing impairment [5]. Even mild levels of hearing impairment have been demonstrated to increase the long-term risk of cognitive impairment in individuals with initially intact cognitive functions [6]. Hearing impairment also leads to a substantial increase in the likelihood of dementia among older adults [6,7,8]. In a previous study, hearing loss was identified as potentially the most modifiable risk factor for dementia, with the highest Population Attributable Fraction (22.2%) [8]. Simultaneously, studies have shown that cognitive impairment often coincides with declining hearing function, which can worsen the effects of hearing loss by affecting sound perception and understanding [9]. Furthermore, cognitive impairment can cause central auditory processing disorders, even with intact peripheral hearing, creating a "vicious cycle" between hearing and cognitive impairments [10]. These findings underscore the need for heightened attention to the cognitive well-being among older adults with hearing impairments.
Socio-economic factors are significantly associated with the health and cognitive function of older adults, including age [11, 12], level of education [13], economic status [14], and living environment [15, 16]. Marital status is recognized as a crucial socio-economic factors that affects the health outcomes of older adults, given its profound influence on multiple facets of their lives [17]. Widowhood, as a distinct marital status, has garnered significant scholarly interest due to its health implications. Upon the loss of a spouse, older adults face numerous challenges, including disruptions in daily routines, changes in social networks, and increased feelings of loneliness. These factors constitute substantial determinants that affect the health status or cognitive function of older adults [18, 19]. Data from the Sixth Chinese National Population Census in 2010 showed that there were 47.7 million widowed older adults in China, accounting for 26.9% of the total population over the age of 60 years. As a result, the number of widowed older adults is expected to grow rapidly in China, reaching 118.4 million by 2050 [20]. As a life event stressor, widowhood is linked to poorer physical and mental health outcomes among older adults, encompassing heightened susceptibility to disability, mortality [21], compromised immune function [22], weight loss [23], sleep disturbance [24], and depression [25]. Several studies indicated that widowhood is correlated with cognitive impairment and heightened dementia risk in older adults. Håkansson et al. [26] and Feng et al. [27] both pointed out that widowhood can increase the risk of cognitive impairment. A meta-analysis also showed that people who were widowed had a higher risk of developing cognitive impairment than married people [28]. Older adults with hearing impairments were also a vulnerable cohort prone to cognitive impairment. However, research investigating the effect of widowhood on the cognitive function of this group is notably lacking.
The effect of widowhood on cognitive impairment among older adults may be moderated by individual social support and participation. Social support is a resource that can help individuals effectively relieve and cope with stress, reflecting the social network of people, including communication with others, receiving support from family and society [29]. Social support can be divided into formal social support (FSS) and informal social support (ISS). FSS refers to the social security policies and medical welfare systems administered by governmental authorities or services provided by the community [30]; ISS refers to economic support, daily care, and emotional support provided by family members, friends, or neighbors [31]. Social participation comprises physical participation, intelligent involvement, and other organized activities. Physical participation involves activities promoting physical health and social interaction; intellectual involvement includes activities that stimulate cognitive functions; other organized activities refer to structured group events or community gatherings that encourage social interaction and community bonding. In the context of traditional Chinese culture, older adults in China tend to engage in intellectual activities such as playing mahjong (a Chinese game played with small pieces of wood with symbols on them) and card, as well as physical activities like Tai Chi Chuan (a kind of traditional Chinese shadow boxing) and square dancing. Social support and participation play pivotal roles as a stress-moderating factor, as the social activities and support formed within one’s social networks can enhance older adults' resilience to stress. Research has indicated that social support can moderate the relationship between widowhood and depressive symptoms [32]. Studies by Holm et al. and Sullivan and Infurna both underscored that the availability of social support could improve coping mechanisms after widowhood, thereby mitigating the negative health impact of widowhood [33, 34]. Prior research has also elucidated that increased social participation after widowhood strengthens the resilience of widowed older adults [35]. By participating in social activities to build a new social network, the widowed older adults can fill the loneliness generated by widowhood and gain more psychological companionship and social acceptance, thus reducing their own health risks [36]. Previous studies have demonstrated that social support can moderate the relationship between widowhood and cognitive function [37]. Additionally, social participation is also associated with levels of cognitive function at the time of spousal loss and can mitigate its negative effects on cognitive function [38]. Therefore, to examine the relationship between widowhood and cognitive function among older adults, it is essential to account for the moderating effect of social support and participation.
The increasing concern regarding cognitive impairment among older adults in the backdrop of China's aging population has garnered significant attention. The cognitive susceptibility of older adults with hearing impairment underscores the necessity for a heightened focus on the cognitive well-being of this group. While several studies indicate a correlation between widowhood and cognitive impairment, further investigation is needed to elucidate the effect of widowhood on cognitive function and the moderating effects of social support and participation on widowhood-related cognitive impairment among older adults with hearing impairments. Using data obtained from a nationally representative survey on older adults' health in China, we initially conducted a descriptive statistical analysis to meticulously examine sample characteristics and discern differences in cognitive function among older adults with and without hearing impairments across different marital statuses. Subsequently, multiple linear regression analysis was employed to investigate the association between widowhood and the cognitive function of older adults, both with and without hearing impairments. Afterwards, we utilized multivariate logistic regression to further probe the effect of widowhood on the likelihood of experiencing different levels of cognitive impairment among older adults with hearing impairments. Finally, we examined the moderating effect of social support and social participation on cognitive impairment associated with widowhood among this vulnerable demographic.
Methods
Data source
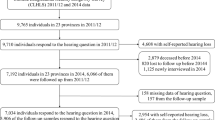
The data utilized in this study were obtained from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) [39], covering the years 2011, 2014, and 2018. This nationally representative survey is conducted by the Chinese Center for Disease Control and Prevention. In this survey, half of the total number of counties and cities in the 22 provinces in China were randomly selected as survey sites, covering 85% of the country's population. Unequal proportional random sampling and multistage methods were used to investigate older adults aged ≥ 65 years. The original dataset for the sample comprises a total of 32,831 observations. Specifically, the sample sizes for 2011, 2014, and 2018 are 9,765, 7,192, and 15,874, respectively. As the central focus of this study concerns the cognitive functional disparities between widowhood and being married, a total of 23,981 individuals aged 65 years or older were included in the study, after excluding those who were divorced, single, or had missing data. The specific composition of the sample was as follows: 9,263 participants in 2011, 6,490 in 2014, and 8,228 in 2018. Within the selected total sample, a cumulative count of 10,292 older adults with hearing impairments was identified and the numbers of older adults with hearing impairment were 4,391, 2,717, and 3,184 in 2011, 2014, and 2018, respectively. The data in the CLHLS covered detailed information including basic demographics, health status, mental health, cognitive function, chronic diseases, family structure, lifestyle, economic status, social support, and social participation. Statistical analysis was performed using STATA software (v. 14.0; STATA Corp., College Station, TX, USA).
Variable selection
Cognition function
Cognitive function was defined by the Mini-Mental State Examination (MMSE), which is composed of 24 questions and a total score of 30 points, with higher scores indicating better cognitive function. It includes questions that evaluate general ability, reaction capability, attention, and calculating ability, recall and language ability, and self-coordination ability. According to CLHLS and the MMSE international standard [40], the level of cognitive function among older adults can be classified into four categories: 24–30 points indicate the absence of cognitive impairment, 18–23 points indicate mild cognitive impairment, 10–17 points suggest moderate cognitive impairment, and 0–9 points indicate severe cognitive impairment.
Widowhood
Given the primary emphasis of this study on examining the relationship between widowhood and cognitive function among older adults, samples pertaining to divorced and single older adults were excluded during the initial data preprocessing phase, resulting in the inclusion of only individuals with spouses and those who were widowed. Therefore, in the present study, the variable of widowhood was confined to a dichotomous classification: 0 for individuals having spouses and 1 for those who are widowed.
Social support and social participation
Social support is classified into two aspects in terms of the contents of the CLHLS questionnaire: informal support (the number of children, co-residence, children’s financial supports, and kinship connection and formal support (community service, social pension insurance, and social medical insurance). The number of children was assessed by inquiring, "How many children have you given birth to?" and was categorized as no child, one child, and more than one child. Co-residence status was categorized as 0 = 'with household', 1 = 'alone', and 2 = 'in institution', based on the response to the question, "Who are you living with now?". The availability of financial support from one’s children was evaluated through the question, "Do you receive financial support from your children?" and was dichotomized into 0 = 'no' and 1 = 'yes'. Kinship connection was quantified by the selections related to kinship among the three options to answer the question, "With whom do you typically engage in frequent conversations or share thoughts in your daily life." The participants were asked to select from options including son, daughter, daughter-in-law, son-in-law, grandchildren and their spouses, other relatives, friends, neighbors, social workers, housekeepers, and nobody. Community service was evaluated by quantifying the availability and inclusivity of these services in the community, including personal daily care services, home visits, psychological consulting, daily shopping, social and recreational services, human rights consulting services, health education, and others.
Social participation consists of physical participation, intelligent involvement, and other organized activities. Physical participation included activities such as Tai Chi Chuan and square dancing, while intelligent involvement comprised activities such as playing cards or mahjong. Organized activities refer to planned and structured events or gatherings that bring people together for a common purpose, often within a community or society. These organized activities include community events, charity fundraisers, workshops, seminars, cultural celebrations, sports competitions, and other planned gatherings that aim to engage and involve participants in a collaborative and purposeful manner. In this study, social participation was categorized into two groups: 0 = 'no' and 1 = 'yes', based on the original questionnaire's question, 'Do you now perform the following activities regularly? (Please choose one from frequency)'. Responses indicating 'never' were classified as 'no', while all other responses were classified as 'yes'. It is worth noting that, owing to the lack of inquiries regarding social participation in the survey questionnaires for the years 2011 and 2014, this study exclusively utilizes the dataset in 2018 to investigate the moderating effect of social participation.
Other control variables
Other control variables in this study primarily encompass basic demographic variables, health status variables, and lifestyle variables. Basic demographic variables include age, residence area, education, and income. Education was classified into four distinct levels: no education, primary school, middle school, and high school and above. Income level was categorized based on annual household earnings as ≤ 30,000, 30,001–50000, 50,001–100000, and > 100,000 Yuan. Health status variables refer to self-rated health status, chronic disease, sleep quality, depression, and activities of Daily Living (ADL). Self-rated health status and sleep quality were both divided into three categories, namely, good, moderate, and bad. Chronic disease was classified into the following categories: no chronic disease, one chronic disease, and multiple chronic diseases. Depression was dichotomized into 0 = 'no' and 1 = 'yes'. ADL was assessed using the Katz scale, which includes evaluation criteria such as bathing, dressing, indoor activities, toileting, independent eating, and bowel and bladder control [41]. According to the original questionnaire, individuals were organized into three groups based on their level of self-care: those with complete self-care (score of 1), those with partial self-care (score of 2), and those with a total inability to perform self-care tasks (score of 3). In line with the reports of previous studies [42], individuals with a score of 1 on all six items in this study were classified as the no disability group. Those with scores greater than 1 on 1–4 evaluation items were classified as the semi-disability group, while those with scores greater than 1 on 5–6 evaluation items were classified as the disability group. Lifestyle variables included smoking, drinking, and daily exercise.
Statistical analysis
Mann–Whitney U test was used to investigate differences in MMSE scores across marital statuses among older adults. A chi-square test was employed to examine the differences in cognitive function between widowed and spousal older adults with hearing impairments. In order to investigate the association between widowhood and cognitive function across diverse demographic groups, we initially conducted multiple linear regressions among older adults with and without hearing impairments, respectively, as delineated in the following formula:
In formula (1), \({Y}_{i}\) represents the MMSE score of older adults, and \({X}_{k}\) denotes widowhood and other control variables. Control variables include basic demographic information, health status, and lifestyle. The basic demographic information included age, residence area, education, and income, while health status comprised self-rated health status, chronic disease, sleep quality, depression, and ADL. Lifestyle encompasses smoking, drinking, and daily exercise. \({Year}_{t}\) is time-varying variable.
Furthermore, we investigated the effect of widowhood on the probability of experiencing different levels of cognitive impairment among older adults with hearing impairments (mild cognitive impairment, moderate cognitive impairment and severe cognitive impairment). Specifically, the dependent variable was defined as "0" (no cognitive impairment), "1" (mild cognitive impairment), "2" (moderate cognitive impairment), and "3" (severe cognitive impairment). As the dependent variable is a multi-classification virtual variable, we employed multiple logistic regression to conduct the analysis. The formula was as follows:
In formula (2), i represents the i-th older adults with hearing impairment; n is the classification of cognitive function, that is, 0, 1, 2, and 3, and \({p}_{n}\) is the hypothesis that the probability of category n cognitive impairment under the action of \({X}_{k}\). In addition, we explored the moderating effect of social support and social participation on cognitive impairment associated with widowhood among older adults with hearing impairment. The specific models are as follows:
In formula (3), \({X}_{k}\) represents widowhood, social support/participation, and other control variables. Social support included ISS and FSS, where ISS comprised the number of children, co-residence, children’s financial support, and kinship connection, and FSS encompassed community service, social pension insurance, and social medical insurance. \({\beta }_{k}\) denote the main effects of widowhood and social support/participation. \({X}_{m}\) is the intersection of widowhood and social support/participation. \({\beta }_{m}\) denotes the moderating effect of social support/participation.
Results
Descriptive statistics
As shown in Supplementary Table 1the total number of effective samples was 23,981; this included 13,689 older adults without hearing impairment and 10,292 with hearing impairment. 72.97% of the total sample consisted of older adults aged 75 years and above. The proportions of male and female participants were 44.74% and 55.26%, respectively. Furthermore, approximately 50.10% of older adults in this study resided in rural settings. Educational attainment was notably low, with approximately 50% of older adults having no formal education. Furthermore, the majority (58.93%) of the participants had an annual income below or equal to 30,000 Yuan. Approximately 49.59% of older adults assessed their health status as being in good condition. Additionally, 27.53% and 35.94% of older adults were afflicted with one or multiple chronic conditions, respectively, while 23.76% had depression. The proportions of semi-disabled and disabled older adults were 8.04% and 7.01%, respectively. In addition, 16.52% of older adults engaged in smoking, 15.39% reported alcohol consumption, and 31.40% maintained daily exercise.
Supplementary Table 2 presents the levels of social support and participation among older adults in this study. Regarding informal social support, most older adults had two or more children (92.69%) and predominantly resided with their household members (80.51%). Furthermore, 80.18% of the participants received financial support from their children, while the average level of selected kinship connection is 1.50. Regarding formal social support, the average number of available community services was approximately 1.62, and approximately 86.32% of older adults had social medical insurance, whereas only 14.00% had social pension insurance. Regarding social participation, 3.03% and 4.84% of older adults engaged in physical activities, such as Tai Chi Chuan and square dancing, respectively. The proportion of participants that engaged in intelligent activities was slightly higher, with 17.17% of older adults engaging in activities, such as playing cards or Mahjong. Additionally, 14.63% of the sample participated in organized activities. Furthermore, as shown in Supplementary Table 2 the proportion of social participation among older adults with hearing impairments was dramatically lower compared to those without hearing impairments.
Cognitive function across different marital statuses among older adults
As shown in Table 1, a notable disparity emerges between the mean MMSE scores for older adults with hearing impairment and those without (2011: 19.227 vs. 25.933, 2014: 19.526 vs. 25.994, 2018: 19.679 vs. 26.549); the cognitive function of older participants with hearing impairment was worse than that of those without hearing impairment. Furthermore, the mean MMSE scores of widowed older adults, both with and without hearing impairment, were significantly lower than those of their counterparts who had spouses, indicating poorer cognitive function among the widowed older population. We further examined the distribution of hearing-impaired older adults across various cognitive function statuses, as shown in Table 2. The proportion of older adults without cognitive impairment was significantly higher among hearing-impaired older adults with spouses compared to those who were widowed across all surveyed years (2011: 58.10% vs. 29.31%; 2014: 59.88% vs. 31.08%; and 2018: 63.13% vs. 28.79%). Additionally, the prevalence of moderate cognitive impairment (2011: 25.41% vs. 13.01%; 2014: 24.50% vs. 13.53%; and 2018: 27.19% vs. 13.83%) and severe cognitive impairment (2011: 27.72% vs. 9.66%; 2014: 26.35% vs. 10.06%; and 2018: 25.86% vs. 6.54%) was significantly higher among hearing-impaired older adults who were widowed compared to those who had spouses. This indicated a poorer cognitive function condition among widowed older adults with hearing impairment compared to their counterparts with spouses.
Multivariate regression results
Leveraging formula (1), we initially conducted a multiple linear regression to examine the association between widowhood and the cognitive function of older adults, both with and without hearing impairments, as shown in Table 3. Widowhood exhibits a significant negative correlation with MMSE scores among older adults, both those without (Coef. = -0.680) and those with hearing impairments (Coef. = -0.898). This indicated that widowhood was significantly associated with a decline in cognitive function in older adults. The absolute value of the coefficient for widowhood was estimated to be greater among older adults with hearing impairment compared to those without, indicating a stronger association between widowhood and declining cognitive function in this demographic. Other socioeconomic factors, including age, gender, education level, income, self-rated health, chronic diseases, depression, activities of daily living (ADL), drinking, and exercise, were found to be significantly associated with MMSE scores.
We further estimated the association between widowhood and various levels of cognitive function among older adults with hearing impairments using formula (2). As shown in Table 4, a statistically significant correlation was observed between widowhood and an increased likelihood of experiencing mild, moderate, and severe cognitive impairment (RRR = 1.155, 1.326, and 1.538). This underscores the fact that widowed older adults with hearing impairments exhibit a significantly heightened risk of cognitive impairment compared to their counterparts who have spouses. Moreover, the Relative Risk Ratio (RRR) of widowhood for severe cognitive impairment was estimated to be the highest (RRR = 1.538), while for moderate cognitive impairment, it was the second highest (RRR = 1.326). This suggests that widowhood may be more inclined to significantly increase the risk of severe and moderate cognitive impairment among older adults with hearing impairments. Regarding other control variables, advancing age was found to substantially heighten the likelihood of mild (RRR = 1.665, 2.827, and 3.650), moderate (RRR = 2.727, 6.471, and 12.955), and severe cognitive impairment (RRR = 1.959, 6.289, and 14.229). Compared to men, women are significantly more likely to suffer from mild, moderate, and severe cognitive impairment (RRR = 1.357, 1.794, and 1.550). Older adults with hearing impairments residing in rural areas are significantly more likely to experience mild, moderate, and severe cognitive impairment (RRR = 1.161, 1.287, and 1.376) compared to their urban counterparts. Higher education level was significantly associated with a lower likelihood of mild (RRR = 0.647, 0.366, and 0.507), moderate (RRR = 0.476, 0.330, and 0.447), and severe cognitive impairment (RRR = 0.461, 0.248, and 0.427). Older adults with hearing impairments who self-rated their health as moderate or poor were more likely to experience mild cognitive impairment (RRR = 1.253 and 1.539) and moderate cognitive impairment (RRR = 1.252 and 2.105) than those who self-rated their health as good. Semi-disability and disability significantly increased the likelihood of mild (RRR = 1.985 and 2.466), moderate (RRR = 3.390 and 7.425), and severe cognitive impairment (RRR = 6.419 and 36.441). Regarding lifestyle variables, smoking only significantly increased the likelihood of moderate cognitive impairment (RRR = 1.248), while daily exercise significantly reduced the likelihood of moderate cognitive impairment (RRR = 0.608) and severe cognitive impairment (RRR = 0.389).
Moderating effect of social support and participation on widowhood-related cognitive impairment among hearing-impaired older adults
Utilizing formula (3), we estimated the moderating effect of social support and participation on cognitive impairment associated with widowhood among older adults with hearing impairment, as illustrated in Table 5. The interaction terms represent this moderation effect. Regarding informal social support, compared to hearing-impaired older adults without children, those with one child had a significantly lower likelihood of mild (RRR = 0.771) and moderate cognitive impairment after widowhood (RRR = 0.933), while those with more than one child had a significantly reduced risk of mild (RRR = 0.618) and severe cognitive impairment associated with widowhood (RRR = 0.911). Notably, having children more effectively mitigates the risk of widowhood-related mild cognitive impairment in older adults with hearing impairment. Living alone after widowhood significantly increased the likelihood of mild cognitive impairment (RRR = 1.943) and moderate cognitive impairment (RRR = 1.301) compared to living with family. Moreover, residing in a care institution elevated the probability of moderate cognitive impairment (RRR = 2.337) and severe cognitive impairment (RRR = 1.257) among older adults with hearing impairment following widowhood. Therefore, both living alone and residing in a care institution demonstrated adverse moderating effects on widowhood-related cognitive impairment. Regarding the interaction term of kinship connection, a diminished likelihood of widowhood-related cognitive impairment was noted among hearing-impaired older adults (RRR = 0.709, 0.902, and 0.832), with mild cognitive impairment exhibiting the most notable reduction (RRR = 0.709). In terms of formal social support, community service and social medical insurance significantly reduced the likelihood of widowhood-related severe cognitive impairment (RRR = 0.752, 0.759), while social pension insurance alleviated the risk of mild, moderate, and severe cognitive impairment related to widowhood (RRR = 0.912, 0.859, and 0.829).
Table 6 reports the moderating effect of social participation on widowhood-related cognitive impairment among older adults with hearing impairments. In terms of physical participation, Tai Chi Chuan and square dancing significantly reduced the risk of severe cognitive impairment related to widowhood compared to those who did not engage in these activities (RRR = 0.332 and 0.331). Regarding intelligent involvement, playing cards or Mahjong significantly diminished the likelihood of moderate and severe cognitive impairment after widowhood (RRR = 0.772, 0.355), indicating that these intellectually stimulating activities mitigate widowhood-related cognitive impairment. Meanwhile, the moderating effect on severe cognitive impairment is more pronounced (RRR = 0.355). Additionally, participation in organized activities was found to significantly decrease the likelihood of severe cognitive impairment following widowhood (RRR = 0.400), exhibiting a favorable moderating effect on severe cognitive impairment related to widowhood among older adults with hearing impairment.
Discussion
As a significant life stressor, widowhood may have a profound effect on the cognitive function of older adults with hearing impairments. However, there remains a dearth of research concerning the association between widowhood and cognitive impairment within this demographic. Furthermore, it is imperative to elucidate how social support and participation can mitigate the cognitive decline associated with widowhood. In this study, we employed nationally representative survey data to explore the effect of widowhood on the cognitive function of older adults with hearing impairment. Additionally, we investigated the moderating effects of social support and participation on widowhood-related cognitive impairment.
Our findings indicate that the cognitive function of older adults with hearing impairment was worse than that of older adults without hearing impairment. This aligns with existing literature suggesting that hearing-impaired older adults represent a vulnerable cohort susceptible to cognitive impairment [8]. This may be attributed to factors, such as cognitive load and auditory deprivation among hearing-impairedindividuals [43, 44]. In addition, the cognitive function of widowed older adults, both with and without hearing impairment, is significantly lower than that of their counterparts who have spouses. Particularly notable is the higher prevalence of moderate and severe cognitive impairment among widowed older adults with hearing impairments. Therefore, it is imperative to prioritize monitoring the cognitive function of widowed older adults, particularly those with hearing impairment, and providing support to assist this vulnerable population in maintaining cognitive health.
The findings of our multiple linear regression analysis indicated that widowhood was negatively associated with the cognitive function of older adults, which is consistent with the results of prior studies [26, 28]. Furthermore, we found a stronger association between widowhood and declining cognitive function among older adults with hearing impairments. Widowhood increases social isolation, and hearing impairment intensifies this effect due to communication challenges. Severe social isolation may lead to substantial cognitive decline due to a lack of stimulation and increased loneliness [45]. Additionally, the older adults with hearing impairment demonstrates higher cognitive load and mental fatigue [46]. When encountering the stress and emotional toll of widowhood, this increased cognitive load may lead to faster cognitive decline. It is worth noting that, according to the findings from the multivariate logistic regression, widowhood may be more likely to significantly increase the likelihood of severe and moderate cognitive impairment among older adults with hearing impairments. Given that older adults with hearing impairments constitute a population particularly vulnerable to cognitive impairment, the stress from widowhood may dramatically exacerbate their condition, increasing the risk of experiencing relative severe cognitive impairments. Therefore, implementing strategies, such as early screening and assessment, specialized cognitive rehabilitation programs, and comprehensive care (including counseling, mental health services, health education, etc.) is crucial to effectively addressing this heightened risk among this vulnerable population following widowhood.
With regard to other control variables, our findings showed that advancing age, being female, or residence in rural settings were significantly associated with an increased likelihood of mild, moderate, and severe cognitive impairment among hearing-impaired older adults, which is consistent with the findings of previous studies [12, 13, 47]. Aging leads to neurological changes such as reduced brain volume and altered neurotransmitter systems, contributing to cognitive decline. Meanwhile, the limited availability of resources in rural China may impede access to adequate healthcare, exacerbating the challenges of this demographic. Furthermore, higher educational levels were correlated with a lower likelihood of cognitive impairment across varying severity levels, which is consistent with the findings of a previous study [13]. Higher educational attainment is often associated with better socioeconomic status, which improves access to healthcare, nutrition, and other factors that affect cognitive health [48], resulting in better cognitive status. Regarding health status and health behavior factors, poor self-rated health, semi-disability, or disability among older adults with hearing impairments are significantly associated with an increased risk of cognitive impairment. However, similar to existing research [49], daily exercise demonstrated a statistically significant reduction in the likelihood of moderate and severe cognitive impairments. Therefore, it is advisable to conduct regular health assessments, promote daily exercise programs tailored to older adults with hearing impairments, and create supportive environments to reduce the risk of cognitive impairments in this vulnerable population.
Our findings revealed the moderating effects of social support on widowhood-related cognitive impairments among hearing-impaired older adults in China. Specifically, informal social support from family and relatives can significantly reduce the risk of widowhood-related cognitive impairment. In our study, having one or more children and having a high level of kinship connections reduced the likelihood of widowhood-related cognitive impairment in older adults with hearing impairment, particularly the risk of mild cognitive impairment. Conversely, living alone or in a care institution exacerbates this risk. Therefore, emotional and practical assistance from family and relatives are crucial for the cognitive health of widowed older adults [50]. In Chinese traditional culture, family and relatives form the most important social network for older adults [51]. Older adults with hearing impairment, as a vulnerable group for cognitive decline, require enhanced informal social support from their networks to help mitigate cognitive impairment related to widowhood, particularly mild cognitive impairment. Strategies should prioritize encouraging regular interaction and support from children and relatives, promoting family involvement, fostering kinship connections, and ensuring accessible housing options to minimize isolation for widowed older adults with hearing impairment, thereby addressing their emotional and practical needs. In terms of formal social support, community services significantly reduce the risk of severe cognitive impairment related to widowhood among hearing-impaired older adults, which contrasts with the findings of previous related research [52]. The possible explanation is that community services offer social interaction, cognitive stimulation, and emotional assistance [53], mitigating the negative effects of widowhood on cognitive health. Furthermore, social pension insurance and social medical insurance have been found to alleviate the likelihood of widowhood-related cognitive impairment among hearing-impaired older adults. This could be attributed to the fact that these insurance schemes may enhance self-coping abilities and resilience in dealing with the challenges of stressful events [30]. Consequently, they have a mitigating effect on widowhood-related cognitive decline.
Social participation has also been shown to moderate cognitive impairments related to widowhood among older adults with hearing impairments. Physical activities such as Tai Chi Chuan, square dancing, and organized activities significantly reduce the risk of severe cognitive impairment associated with widowhood. Likewise, intellectually stimulating activities, such as playing cards or Mahjong, also mitigate widowhood-related cognitive decline, with a particularly stronger effect on severe impairment. Previous studies have indicated that physical activity can improve blood flow to the brain, enhance neuroplasticity, and reduce the risk of cognitive impairment [54]; intellectually stimulating activities can also challenge the brain and help preserve cognitive function, particularly in tasks related to memory, attention, and problem-solving [55]; organized activities foster belonging and resilience to stressors, such as widowhood, through collaboration and interaction, potentially mitigating the risk of cognitive impairment [56]. In light of this, engaging in social participation may offer cognitive and emotional benefits to older adults with hearing impairments, especially when they experience widowhood. Therefore, promoting and facilitating such engagement could be an effective strategy to reduce the risk of severe cognitive impairment associated with widowhood.
Our study has several limitations that warrant acknowledgment. First, although we employed regression analysis on pooled cross-sectional data from 2011, 2014, and 2018 to examine the relationship between widowhood and cognitive impairment, causal inferences cannot be strictly drawn from these analyses. Second, while there were differences in widowhood status over the long and short term, this study could not determine the impact of the duration of widowhood on cognitive impairment among older adults. Thirdly, the data on hearing impairment, being sourced from self-reports, may introduce certain biases. Future research should consider employing more objective evaluation methods to improve the reliability of the data and the validity of the finding. Finally, cognitive function among older adults is likely to have been influenced by additional factors that were not included in the data obtained from CLHLS, which is another limitation of this study.
Conclusion
Our findings indicated that widowhood is negatively associated with cognitive function in older adults. A stronger association was observed between widowhood and declining cognitive function in older adults with hearing impairments. Specifically, widowhood may be more likely to significantly increase the likelihood of severe and moderate cognitive impairment among older adults with hearing impairments. Therefore, early screening, specialized cognitive rehabilitation, and comprehensive care are crucial to address the heightened risk in this vulnerable population following widowhood. Both social support and participation played a significant role in mitigating the risk of cognitive impairment associated with widowhood among older adults with hearing impairments. Thus, strategies should prioritize improving social support and promoting active participation in social activities to mitigate this risk in this vulnerable population following widowhood. Additionally, factors such as age, gender, type of residence, and education level were found to be significantly associated with cognitive function. Therefore, practitioners should consider these factors when developing interventions to maintain and promote cognitive function in older adults with hearing impairments.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PAF:
-
Population attributable proportion
- CLHLS:
-
Chinese longitudinal healthy longevity survey
- FSS:
-
Formal social support
- ISS:
-
Informal social support
- MMSE:
-
Mini-mental state examination
- ADL:
-
Activities of daily living
- RRR:
-
Relative risk ratio
References
Alzheimer’s Disease International. World Alzheimer Report 2021: Journey Through the Diagnosis of Dementia. 2021.
Prince M, Ali G-C, Guerchet M, Prina AM, Albanese E, Wu Y-T. Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimers Res Ther. 2016;8:23.
Jia L, Quan M, Fu Y, Zhao T, Li Y, Wei C, et al. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. 2020;19:81–92.
State Council of the People’s Republic of China. 2016. Health China 2030 Planning Outline. https://www.gov.cn/gongbao/content/2016/content_5133024.htm. Accessed 11 May 2024.
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. Lancet. 2017;390:2673–734.
Lin FR, Ferrucci L, Metter EJ, An Y, Zonderman AB, Resnick SM. Hearing loss and cognition in the Baltimore longitudinal study of aging. Neuropsychology. 2011;25:763–70.
Lin FR. Hearing loss and cognition among older adults in the United States. J Gerontol A Biol Sci Med Sci. 2011;66A:1131–6.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–46.
Hardy CJD, Marshall CR, Golden HL, Clark CN, Mummery CJ, Griffiths TD, et al. Hearing and dementia. J Neurol. 2016;263:2339–54.
Johnson JCS, Marshall CR, Weil RS, Bamiou DE, Hardy CJD, Warren JD. Hearing and dementia: from ears to brain. Brain. 2021;144:391–401.
Klich-Rączka A, Piotrowicz K, Mossakowska M, Skalska A, Wizner B, Broczek K, et al. The assessment of cognitive impairment suspected of dementia in Polish elderly people: results of the population-based PolSenior Study. Exp Gerontol. 2014;57:233–42.
Ward A, Arrighi HM, Michels S, Cedarbaum JM. Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement. 2012;8:14–21.
Tervo S, Kivipelto M, Hänninen T, Vanhanen M, Hallikainen M, Mannermaa A, et al. Incidence and risk factors for mild cognitive impairment: a population-based three-year follow-up study of cognitively healthy elderly subjects. Dem Geriatr Cogn Disord. 2004;17:196–203.
Simsek H, Doganay S, Budak R, Ucku R. Relationship of socioeconomic status with health behaviors and self-perceived health in the elderly: a community-based study. Turkey Geriatr Gerontol Int. 2014;14:960–8.
Liu Y, Dijst M, Faber J, Geertman S, Cui C. Healthy urban living: residential environment and health of older adults in Shanghai. Health Place. 2017;47:80–9.
Fangfang H, Xiao H, Shuai Z, Qiong W, Jingya Z, Guodong S, et al. Living environment, built environment and cognitive function among older Chinese adults: results from a cross-sectional study. J Prev Alzheimers Dis. 2022;9:126–35.
Han K, Milosevic M, Fyles A, Pintilie M, Viswanathan AN. Trends in the utilization of brachytherapy in cervical cancer in the United States. Int J Radiat Oncol Biol Phys. 2013;87:111–9.
Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000;355:1315–9.
Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English longitudinal study of ageing. Psychosom Med. 2013;75:161–70.
Eggleston KN, Meng D, Xu G, He L, Zhang M, Lin D. What determines the preference for future living arrangements of middle-aged and older people in urban China? PLoS ONE. 2017;12:e0180764.
Rendall MS, Weden MM, Favreault MM, Waldron H. The protective effect of marriage for survival: a review and update. Demography. 2011;48:481–506.
Phillips AC, Carroll D, Burns VE, Ring C, Macleod J, Drayson M. Bereavement and marriage are associated with antibody response to influenza vaccination in the elderly. Brain Behav Immun. 2006;20:279–89.
Stahl ST, Schulz R. Changes in routine health behaviors following late-life bereavement: a systematic review. J Behav Med. 2014;37:736–55.
van de Straat V, Bracke P. How well does Europe sleep? A cross-national study of sleep problems in European older adults. Int J Public Health. 2015;60:643–50.
Blanner Kristiansen C, Kjær JN, Hjorth P, Andersen K, Prina AM. Prevalence of common mental disorders in widowhood: a systematic review and meta-analysis. J Affect Disord. 2019;245:1016–23.
Håkansson K, Rovio S, Helkala E-L, Vilska A-R, Winblad B, Soininen H, et al. Association between mid-life marital status and cognitive function in later life: population based cohort study. BMJ. 2009;339:b2462.
Feng L, Ng X-T, Yap P, Li J, Lee T-S, Håkansson K, et al. Marital status and cognitive impairment among community-dwelling Chinese older adults: the role of gender and social engagement. Dem Geriatr Cogn Disord Extra. 2014;4:375–84.
Sommerlad A, Ruegger J, Singh-Manoux A, Lewis G, Livingston G. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Neurosurg Psychiatry. 2018;89:231–8.
Barrera M. Distinctions between social support concepts, measures, and models. Am J Community Psychol. 1986;14:413–45.
Tao YC, Shen Y. The influence of social support on the physical and mental health of the rural elderly. Popul Econ. 2014;3:3–14 (In Chinese).
Lu S, Wu Y, Mao Z, Liang X. Association of formal and informal social support with health-related quality of life among Chinese rural elders. Int J Environ Res Public Health. 2020;17:1351.
Monserud MA, Markides KS. Changes in depressive symptoms during widowhood among older Mexican Americans: the role of financial strain, social support, and church attendance. Aging Ment Health. 2017;21:586–94.
Holm AL, Berland AK, Severinsson E. Factors that influence the health of older widows and widowers—a systematic review of quantitative research. Nurs Open. 2019;6:591–611.
Sullivan C, Infurna FJ. The multidimensional nature of social support and engagement in contributing to adjustment following spousal loss. Aging Ment Health. 2020;24:857–69.
Lim-Soh JW, Carr DS. Social participation in widowhood: evidence from a 12-year panel. J Gerontol B Psychol Sci Soc Sci. 2022;77:972–82.
Pang J, Xu S, Wu Y. Effect of widowhood on the risk of disability among the elderly in China. Front Psychiatry. 2023;14:1169952.
Lee Y, Jiang Y. Examining sociocultural factors in widowhood and cognitive function among older Chinese immigrants: findings from the PINE study. Aging Ment Health. 2023;27:2144–52.
Hülür G, Elayoubi J, Nelson ME, Haley WE. Change in episodic memory with spousal loss: the role of social relationships. J Gerontol B Psychol Sci Soc Sci. 2022;77:683–94.
The Chinese Longitudinal Healthy Longevity Survey (CLHLS)-Longitudinal Data (1998–2018). http://opendata.pku.edu.cn/dataset.xhtml?persistentId=10.18170/DVN/WBO7LK. Accessed 30 Oct 2023.
Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.
Hou C, Ping Z, Yang K, Chen S, Liu X, Li H, et al. Trends of activities of daily living disability situation and association with chronic conditions among elderly aged 80 years and over in China. J Nutr Health Aging. 2018;22:439–45.
Uchida Y, Nishita Y, Kato T, Iwata K, Sugiura S, Suzuki H, et al. Smaller hippocampal volume and degraded peripheral hearing among Japanese community dwellers. Front Aging Neurosci. 2018;10:319.
Martini A, Castiglione A, Bovo R, Vallesi A, Gabelli C. Aging, cognitive load, dementia and hearing loss. Audiol Neurootol. 2014;19:2–5.
Monserud MA, Wong R. Depressive symptoms among older Mexicans: the role of widowhood, gender, and social integration. Res Aging. 2015;37:856–86.
Slade K, Plack CJ, Nuttall HE. The effects of age-related hearing loss on the brain and cognitive function. Trends Neurosci. 2020;43:810–21.
Zhang Q, Wu Y, Han T, Liu E. Changes in cognitive function and risk factors for cognitive impairment of the elderly in China: 2005–2014. Int J Environ Res Public Health. 2019;16:2847.
Banerjee S. Determinants of rural-urban differential in healthcare utilization among the elderly population in India. BMC Public Health. 2021;21:939.
Kirk-Sanchez NJ, McGough EL. Physical exercise and cognitive performance in the elderly: current perspectives. Clin Interv Aging. 2014;9:51–62.
Wu HX, Jia YZ. Self-related health of the widowed elderly in rural and urban areas: findings from the perspective of social support. Popul Dev. 2017;23:66–73.
Gao W, Chen J. The Chinese law of human relationship and its operating mode. Trib Soc Sci. 2008;7:67–71 (In Chinese).
Jiang C, Song H, Shi J. The impact of widowhood on mental health of older adults. Geriatr Nurs. 2023;50:38–43.
Zhu HL, Zeng XQ. Social activities and the cognitive ability of rural middle-aged and old people-evidence from CHARLS 2011–2015. Labor. 2019;9:25–39 (in Chinese).
Bettio L, Thacker JS, Hutton C, Christie BR. Modulation of synaptic plasticity by exercise. Int Rev Neurobiol. 2019;147:295–322.
Hultsch DF, Hertzog C, Small BJ, Dixon RA. Use it or lose it: engaged lifestyle as a buffer of cognitive decline in aging? Psychol Aging. 1999;14:245–63.
Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3:343–53.
Acknowledgements
Authors thank all the participants as well as all the interviewers for helping collect data. We also thank all the reviewers for their insightful and constructive comments.
Funding
This study was conducted without any external funding support.
Author information
Authors and Affiliations
Contributions
X.W. led the analysis of the data and wrote the draft of the manuscript; S.L. participated in data analysis and writing; Z.Z. contributed to writing; Z.C and Z.W. contributed equally to the study design, interpretation of the data and helped in the writing of the final draft of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Academic Research Ethics Committee of Nanjing Medical University; reference number: 2022460. All procedures were in accordance with the ethical standards of the Helsinki Declaration. Participants provided informed consent prior to data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Li, S., Zhang, Z. et al. Association between widowhood and cognitive function among Chinese older adults with hearing impairment: the moderating effect of social support and participation. BMC Geriatr 24, 764 (2024). https://doi.org/10.1186/s12877-024-05358-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05358-7