Abstract
Objective
This systematic review examined studies that assessed the relationship between mortality risk and multidimensional frailty. The pooled risk of mortality was estimated via a meta-analysis.
Design
A systematic review and meta-analysis.
Methods
A systematic search for potentially eligible literature was conducted on January 2, 2023, using five electronic databases: Web of Science, CINAHL, PubMed, the Cochrane Library and Embase. This review included cohort or longitudinal studies examining the association between multidimensional frailty/prefrailty and mortality in older adults. The quality of the included studies was evaluated via the Quality in Prognosis Studies (QUIPS) tool. Two independent researchers identified eligible studies and extracted the data. The data analyses were performed via STATA, version 15.0.
Results
A total of 24 studies with 34,664 participants were included. The 24 studies were published between 2012 and 2022, with most studies being performed in Italy (n = 16). The sample sizes of the included studies ranged from 71 to 12,020. Most included studies were conducted in hospital settings. The QUIPS bias assessment results showed that the most frequent source of potential bias was study confounding. The meta-analysis results showed that multidimensional frailty was a significant predictor of mortality (HR = 5.48, 95% CI = 3.91–7.67, p < 0.001). In addition, multidimensional prefrailty was also a significant predictor of mortality (HR = 2.56, 95% CI = 2.17–3.02, p < 0.001). The results of the meta-analysis using the ORs revealed that multidimensional frailty was a risk factor for mortality in older people (OR = 4.59, 95% CI = 2.47–8.55, p < 0.05).
Conclusions and implications
This systematic review of the relationship between multidimensional frailty and mortality found that multidimensional frailty/prefrailty is a predictor of mortality. More studies should be conducted in community dwelling populations and nursing homes.
Similar content being viewed by others
Introduction
Frailty is a condition distinguished by a noticeable decline in various forms of physiological functioning coupled with increased susceptibility to external stressors [1]. Numerous studies have identified frailty as a considerable health threat among older adults. Frailty is independently correlated with severe health outcomes such as disability, cognitive impairment and mortality [2,3,4,5]. Despite its significance, there remains an ongoing debate in the medical community regarding the assessment of frailty. As the research landscape evolved, a groundbreaking multidimensional model was introduced by Ferrucci and colleagues [6]. This innovative model considers frailty to be a disintegration of synergy across multiple dimensions, such as genetic components, biological processes, functional capabilities, cognitive aspects, psychological factors, and socioeconomic influences. This lack of harmony pushes individuals into an unstable state of equilibrium [6]. Within this paradigm, frailty is evaluated via a comprehensive geriatric assessment (CGA). The instrument that has emerged from this approach is the Multidimensional Prognostic Index (MPI), which was developed by Pilotto and his team in 2008 [7]. The MPI offers a holistic perspective and encompasses eight vital domains, including daily living activities, cognitive functions, and more. Scores on the MPI range from 0 to 1, with distinct categorizations indicating varying risk levels. Specifically, values below 0.33 indicate lower risk, values between 0.34 and 0.66 indicate moderate risk, and values exceeding 0.66 indicate high frailty risk [8,9,10].The MPI meticulously integrates a multitude of factors, spanning biological, psychological, and social domains, to provide a holistic evaluation of the patient.
The MPI is considered a predictive tool based on a CGA and is capable of extracting information from the standard CGA to categorize frailty into three subgroups, offering excellent prognostic value in identifying frailty [6]. A systematic review undertaken by Veronese et al. elucidated the prevalence of multidimensional frailty, as characterized by the MPI, across various settings. The findings revealed that within hospitals, communities, and nursing homes, the prevalence rates of frailty were 29.8%, 51.5%, and 13.3%, respectively [8]. These data underscore that multidimensional frailty is a widespread concern among older people. Originally, the MPI was developed with the primary goal of predicting mortality among senior patients admitted to hospitals [7]. However, its applicability has expanded over time. This predictive tool has been widely used in a range of clinical scenarios [10,11,12,13] and in older adults living in community [14] or institutional care environments [15]. This tool has demonstrated excellent calibration, reproducibility, and accuracy in predicting short- and long-term mortality in multiple cohorts of older patients [13, 15,16,17]. Cella et al. found that multidimensional frailty assessed by the MPI was significantly more accurate than physical frailty assessed by the Fried frailty phenotype (FP) in predicting mortality [14]. In addition, the MPI showed significantly greater discriminatory accuracy than the frailty index in predicting one-month mortality and one-year mortality, which demonstrated that the concept of multidimensional frailty might have greater predictive power for the mortality of older inpatients [18]. The efficacy of the MPI is further corroborated by its robust validity, feasibility, and reliability, making it an indispensable instrument not only for gauging prognosis risk but also for formulating individualized therapeutic strategies [19].
Current systematic reviews exploring the relationship between frailty and mortality have focused mainly on the frailty phenotype and frailty index, and the results have shown that these tools have a significant ability to predict mortality risk [2, 20]. Although many studies have indicated that older adults exhibiting signs of multidimensional frailty are at a significantly greater risk of mortality than their healthy peers are, some studies have shown that multidimensional prefrailty is not a significant predictor of mortality [13, 21]. There is a lack of systematic reviews that specifically focus on elucidating the relationship between multidimensional frailty/prefrailty and mortality. Therefore, the aim of this systematic review is to identify studies that examine the mortality risk associated with multidimensional frailty/prefrailty and to estimate the pooled risk of mortality by conducting a meta-analysis.
Methods
Design
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA 2020) guidelines [22] and was prospectively registered on the PROSPERO website (International Prospective Register of Systematic Reviews) with the number CRD42023443130.
Search methods
The Web of Science, CINAHL, PubMed, Cochrane Library and Embase electronic databases were systematically searched on 2 January 2023 to identify potentially eligible literature. In addition, the reference lists were manually searched to identify eligible studies. The search terms were developed with subject terms and free terms, including “multidimensional prognostic index”, “multidimensional frailty”, “aged”, “elder*”, “older*”, “geriatric*”, etc. Appendix 1 shows the details of the search strategy.
Study selection
Two independent researchers identified eligible studies on basis of the inclusion and exclusion criteria. The inclusion criteria were as follows: (1) The participants were over 60 years old. (2) Multidimensional frailty was diagnosed with the MPI. Multidimensional frailty is generally divided into three categories: robust (MPI value < 0.33, MPI-1 low risk), prefrailty (0.34 ≤ MPI value ≤ 0.66, MPI-2 moderate risk) and frailty (MPI value > 0.66, MPI-3 severe risk). (3) The study was designed as a prospective cohort study or longitudinal study. (4) Mortality risk data for frailty (MPI-3) or prefrailty (MPI-2) were reported as the hazard ratio (HR), odds ratio (OR), or relative risk (RR). (5) For multiple studies from the same cohort, the study with the largest sample size was selected. The exclusion criteria were as follows: (1) studies written in languages other than English; (2) the full paper was not available; (3) the study did not include sufficient data; and (4) conference abstracts, editorials, protocols, or comments. A third researcher resolved disagreements and made the final decision.
Data extraction
Two independent researchers extracted relevant data for the included studies via a standardized Excel spreadsheet. These data included the first author, year, country/region, sample size, percentage of females, mean age, setting, MPI categories, risk estimate HR/RR/OR (95% CI), adjusted variables and follow-up period.
Quality appraisal
Two independent reviewers assessed the methodological quality of the included studies using the Quality in Prognosis Studies (QUIPS) tool [23]. The QUIPS is divided into six domains: study participation, attrition, prognostic factor and outcome measurement, study confounding and statistical analysis and reporting. Each domain is classified as having a low, moderate, or high risk of bias. On the basis of a previous study [24], if a study has a low risk of bias in five or more of the QUIPS domains or a moderate risk in only two domains, it is categorized as possessing an overall low risk of bias. If these criteria are not met, the study is classified as having a high overall risk of bias.
Data Analysis
The data analyses were performed with STATA, version 15.0, and all analyses were considered statistically significant when the p value was < 0.05.
The pooled HRs, ORs or RRs of mortality along with the 95% confidence intervals (CIs) were analysed via a random effects or fixed effects model. The choice between the random effects or fixed effects model depended on the magnitude of heterogeneity. If the I2 statistic was ≥ 50%, a random effects model was used for meta-analysis; otherwise, a fixed effects model was used [25]. Egger’s test was performed to assess publication bias. To explore potential sources of heterogeneity, we performed sensitivity and subgroup analyses. The studies were divided into different subgroups to explore potential sources of heterogeneity. Subgroup analyses were conducted on the basis of the different settings (hospital, intermediate care facility/nursing home versus community dwelling), different follow-up durations (in-hospital mortality, less than 1 year, 1 year versus more than 1 year), different system diseases (all systems, nervous system, gastrointestinal system, respiratory system, cardiovascular system versus urinary system) and different models of multidimensional frailty (prefrailty and frailty, frailty versus prefrailty).
Results
Study selection
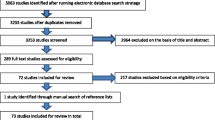
The process of study selection is shown in Fig. 1. A total of 1,053 records were identified, and 445 were duplicates. After the initial screening, 66 studies remained for full-text review. Among them, 24 studies were ultimately eligible for the systematic review [13,14,15,16,17, 21, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43].
Study characteristics
Table 1 presents the main characteristics of the included studies. The 24 studies were published between 2012 and 2022, with most studies being performed in Italy (n = 16). The sample sizes of the included studies ranged from 71 to 12,020, with a total sample size of 34,664. The proportion of females in the studies ranged from 42 to 70.4%. Nineteen studies were conducted in hospitals, three were conducted in the community, and two were conducted in nursing homes. Most studies (n = 21) reported the adjusted HRs and 95% CIs for mortality, with robust participants used as a reference. Three studies reported the adjusted OR for mortality, and one study reported the adjusted RR. Four studies reported in-hospital mortality, and the follow-up period of the other studies ranged from 1 month to 5 years.
Methodological quality
The 24 studies were evaluated for methodological quality. The details of the methodological quality assessment are shown in Appendix 2. The QUIPS bias assessment results revealed that 23 studies had a low risk of bias and one study had a high risk of bias. The most frequent source of potential bias was study confounding, followed by study participation. All of ten studies were classified as having a moderate risk in the study confounding domain because these studies were insufficient to adjust for important confounders in their multivariate models.
Meta-analysis findings
Meta-analysis of MPI-3 severe risk (multidimensional frailty)
Twenty-one studies reported the HRs of mortality for older people in the MPI-3 group. A random effects model was used (I2 = 96.5%), and the results revealed that multidimensional frailty was a significant predictor of mortality (HR = 5.48, 95% CI = 3.91–7.67, p < 0.001) (Fig. 2).
Meta-analysis of MPI-2 moderate risk (multidimensional prefrailty)
Nineteen studies reported the HRs of mortality for older people in the MPI-2 group. A random effects model was used (I2 = 85.5%), and the results revealed that multidimensional prefrailty was a significant predictor of mortality (HR = 2.56, 95% CI = 2.17–3.02, p < 0.001) (Fig. 3).
Meta-analysis of the studies reporting the ORs
Three studies reported the ORs of all-cause mortality. A random effects model was used (I2 = 73.9%), and the results revealed that multidimensional frailty was a risk factor for mortality in older people (OR = 4.59, 95% CI = 2.47–8.55, p < 0.05) (Fig. 4).
Sensitivity and subgroup analyses
Sensitivity analyses were performed to assess the impact of studies providing HRs of mortality for both multidimensional frailty and prefrailty. The objective of these analyses was to determine whether there were statistically significant differences between the combined effect value and the overall combined value. The results of these analyses did not reveal any significant disparities, indicating that the combined effect values adequately represented the overall findings.
Subgroup analyses of MPI-3 severe risk (multidimensional frailty)
When the risk of mortality across different settings was examined, the data showed variations. Specifically, the nursing homes group presented the lowest risk of mortality, with an HR of 3.38 (95% CI = 1.05–10.86, p < 0.05) (Appendix 3). Additionally, when considering different follow-up durations, the subgroup with a follow-up period of more than one year had the lowest mortality risk, with an HR of 4.32 (95% CI = 2.69–6.93, p < 0.001) (Appendix 4). When different systemic diseases were considered, the cardiovascular system subgroup had the lowest mortality risk (HR = 3.35, 95% CI = 2.55–4.40, p < 0.001) (Appendix 5).
Subgroup analyses of MPI-2 moderate risk (multidimensional prefrailty)
Furthermore, disparities in mortality risk were observed across different settings. Notably, the community group presented the highest risk (HR = 3.02, 95% CI = 2.22–4.12, p < 0.001) (Appendix 6). Moreover, when considering different follow-up durations, the subgroup with a follow-up period of more than one year had the lowest mortality risk (HR = 2.17, 95% CI = 1.80–2.60, p = 0.113) (Appendix 7). When different systemic diseases were considered, the cardiovascular system subgroup had the highest mortality risk (HR = 6.91, 95% CI = 2.36–20.22, p < 0.001) (Appendix 8).
Subgroup analyses of the studies reporting the ORs
Different models of multidimensional frailty were also assessed in the studies that reported the ORs. Interestingly, the multidimensional prefrailty group presented the lowest risk of mortality, with an OR of 2.66 (95% CI = 1.87–3.78, p = 0.537) (Appendix 9). These findings provide valuable insights into the relationships between different dimensions of frailty and mortality outcomes.
Publication bias
Publication bias analysis was performed via Egger’s test. The results of Egger’s test (p = 0.436) indicated that there was no significant publication bias for the studies reporting the HRs of mortality for older people in the MPI-3 group. With respect to the studies reporting the HRs of mortality for older people in the MPI-2 group, the results of Egger’s test (p = 0.526) revealed that there was also no significant publication bias. Owing to the limited number of studies that reported ORs for mortality, we did not assess publication bias for this subgroup.
Discussion
This systematic review included an exhaustive examination of 24 studies that reported the association between multidimensional frailty and the risk of mortality. The MPI has been widely used to predict mortality in various settings, such as hospitals, communities, and nursing homes. The subjects included patients with acute or chronic diseases (cardiovascular diseases [37], COVID-19 [26], cancer [32], dementia [36] and chronic kidney disease [42]), intensive care unit (ICU) patients [13], emergency room patients [28] and older individuals in the community or nursing homes [15, 39]. The included studies meticulously measured this association through metrics such as hazard ratios (HRs) or odds ratios (ORs). The meta-analysis indicated that, multidimensional frailty or prefrailty was a significant predictor of mortality. In addition, subgroup analyses based on different settings revealed that the community group presented the highest risk of mortality. When considering different follow-up durations, the subgroup with a follow-up period of more than one year had the lowest mortality risk. Moreover, different systemic diseases affected the risk of mortality.
A systematic review by Chang et al. explored the relationship between physical frailty assessed by the Fried frailty phenotype (FP) and mortality, and they reported that the pooled HRs of mortality for frail and prefrail older people were 2.00 and 1.335, respectively [20]. Another systematic review investigated the risk of mortality for frailty, defined by the frailty index (FI), and the results indicated a significant association between higher FI scores and a higher risk of mortality (pooled HR per 0.1 FI increase = 1.282) [2]. Our meta-analysis findings unequivocally revealed that older individuals with multidimensional frailty or prefrailty have a significantly greater risk of mortality than older adults without frailty (HR = 5.48 and HR = 2.56, respectively). These findings emphasize the importance of recognizing and addressing multidimensional frailty in the older population and underscore the importance of implementing interventions to mitigate the impact of multidimensional frailty and improve health outcomes in older adults.
Drawing from our current understanding, we can postulate several potential factors contributing to the connection between multidimensional frailty and a heightened risk of mortality. First, the Multidimensional Prognostic Index (MPI) is a tool derived from a comprehensive geriatric assessment and incorporates multiple relevant factors, such as physical function, cognitive function, and social function, as evaluation indicators, accounting for an individual’s health status and disease conditions [6]. By comprehensively assessing different factors, it is possible to provide a more accurate prediction of mortality risk for individuals [9, 11]. Second, the multidimensional frailty of older people is often associated with a decline in various physiological systems, including the cardiovascular [44], respiratory [45], musculoskeletal [46], and immune systems [47]. This decline in physiological function could increase the risk of mortality. Third, the assessment of multidimensional frailty accounts for comorbidity factors, which means that older adults with comorbidities are more likely to have an increased risk of developing multidimensional frailty. Comorbidities, such as cardiovascular disease, increase the risk of mortality [48]. Fourth, individuals with multidimensional frailty usually have lower resilience, which may result in individuals being more susceptible to adverse health events, leading to a higher risk of mortality [49]. Fifth, multidimensional frailty is also associated with a decline in cognitive function and physical function. These cognitive deficits may result in difficulties in effective self-management, adhering to treatment plans, and engaging in preventive behaviors, thereby increasing the risk of mortality [50]. A decline in physical function can result in limitations in mobility and balance, leading to an increased risk of falls and ultimately resulting in death [51]. Finally, social factors can also be contributing factors. Loneliness and social isolation are risk factors for frailty [52, 53], which might increase the risk of death in individuals with multidimensional frailty.
Further investigation through subgroup analyses revealed a noteworthy revelation—older adults with multidimensional frailty in the nursing homes group presented the lowest mortality risk. This might be because nursing homes often offer specialized treatments and close monitoring for older patients [15]. A scoping review by Sezgin et al. revealed that intermediate care had positive effects on reducing short- and long-term hospital re-admissions and improving ADL function [54], which might contribute to reducing the risk of mortality. Moreover, the lower mortality risk could also reflect selection bias, where individuals who enter these facilities may already be in a relatively better health status. The subjects from the hospital studies included older patients with acute or severe diseases [21, 27, 41], who may already be in the severe stages of disease or who are experiencing acute illness, thereby increasing their risk of mortality. However, it is essential to note that this observation is founded on a somewhat limited dataset, as only two studies have directly examined the nexus between multidimensional frailty and mortality within the context of older adults residing in nursing homes [15, 26]. Therefore, more research should be conducted in this field.
Additionally, we found that the risk of short-term mortality (in-hospital mortality or less than one year of follow-up) was greater among older adults with multidimensional frailty or multidimensional prefrailty than long-term mortality. A cohort study conducted by Hansen et al. revealed that 90-day mortality had higher hazard ratios (HR = 18.50) than did long-term mortality (HR = 7.10) [30]. Zanetti1 et al. investigated data from 529 medical patients and reported that the hazard ratio (HR = 4.152) for 60-day mortality was greater than that for 1-year mortality (HR = 2.986) [16]. Our findings were consistent with those of previous studies. These findings indicate that the MPI has high accuracy and predictive ability for forecasting short-term mortality [2, 9, 27]. This may be because long-term mortality is influenced by a variety of chronic and clinical factors [16], which means that the accurate prediction of long-term mortality needs to consider more potential variables and complex interactions. Moreover, some studies included in our review focused on acutely hospitalized patients. Owing to the urgent and serious nature of their medical conditions, hospitalized patients may have a greater risk of short-term mortality [16, 18, 41].
In general, this systematic review has several strengths. First, we provide a comprehensive synthesis of evidence on multidimensional frailty and mortality. We conducted a comprehensive and systematic search of electronic databases to minimize selection bias and provide a more complete overview of the available evidence. Additionally, we employed rigorous methods for study selection, data extraction, and quality assessment. Subgroup and sensitivity analyses were conducted to explore the sources of heterogeneity. These factors collectively enhance the rigor and reliability of our study, increasing confidence in the scientific validity and credibility of our findings.
However, several limitations of this study that should be acknowledged. First, there was significant heterogeneity in the studies, possibly due to the diverse environments in which the research was conducted. There was a lack of studies conducted in community and care facilities, which may have affected on the results. While numerous studies have been conducted in hospital environments, the patients in these studies exhibited a wide range of disease types. Owing to limitations in the number of studies available, we were unable to perform subgroup analyses on the basis of specific disease types. Second, in terms of the search strategy, our search terms did not utilize Emtree in the Embase search strategy, Medical Subject Headings (MeSH) in the Cochrane Library search strategy, or CINAHL Subject Headings in the CINAHL search strategy. Third, while most studies adjusted for confounding factors, each study had different confounding factors that were considered. These varying confounders may have had an impact on the results of the study. Finally, the follow-up durations of the studies were not consistent, with some studies having relatively short follow-up periods. This variation in follow-up time may have resulted in an underestimation of the outcomes of the study.
Hence, future studies should provide the HR or OR of mortality in community and care facilities, and respondents should be followed up for a longer period. Additionally, more research is needed to elucidate the mechanisms underlying the relationship between multidimensional frailty and mortality.
Conclusions
The systematic review of the relationship between multidimensional frailty and mortality revealed that multidimensional frailty/prefrailty is a predictor of mortality, which has prognostic value and can guide treatment decisions.
Relevance to clinical practice
The MPI is a reliable prognostic indicator for mortality in various populations and could be used to guide nursing decisions and identify individuals at risk of adverse outcomes. However, importantly, many of the studies included in this review were conducted in hospital settings and focused on specific patient populations. Further research is needed to evaluate the utility of the MPI in different environments and populations as well as to explore its potential applications in clinical practice.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Hoogendijk EO, et al. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–75.
Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193–200.
Vermeulen J, et al. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. 2011;11:33.
Ida S, et al. Relationship between frailty and mortality, hospitalization, and cardiovascular diseases in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2019;18(1):81.
Kojima G, et al. Frailty as a predictor of Alzheimer Disease, Vascular Dementia, and all Dementia among Community-Dwelling Older people: a systematic review and Meta-analysis. J Am Med Dir Assoc. 2016;17(10):881–8.
Pilotto A, et al. A multidimensional approach to frailty in older people. Ageing Res Rev. 2020;60:101047.
Pilotto A, et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res. 2008;11(1):151–61.
Veronese N, et al. Prevalence of multidimensional frailty and pre-frailty in older people in different settings: a systematic review and meta-analysis. Ageing Res Rev. 2021;72:101498.
Pilotto A, et al. The Multidimensional Prognostic Index predicts short- and long-term mortality in hospitalized geriatric patients with pneumonia. Journals Gerontol Ser A: Biol Sci Med Sci. 2009;64A(8):880–7.
Pilotto A, et al. The multidimensional prognostic index (MPI), based on a comprehensive geriatric assessment predicts short- and long-term mortality in hospitalized older patients with dementia. J Alzheimers Dis. 2009;18(1):191–9.
Sancarlo D, et al. The multidimensional prognostic index predicts short-and long-term mortality in hospitalized geriatric patients with type 2 diabetes (T2D). Eur Geriatr Med. 2010;1:S70–1.
Sancarlo D, et al. Validation of a modified-multidimensional prognostic index (m-MPI) including the mini nutritional assessment short-form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J Nutr Health Aging. 2011;15(3):169–73.
Pilotto A, et al. The multidimensional prognostic index (MPI) for the prognostic stratification of older inpatients with COVID-19: a multicenter prospective observational cohort study. Archives Gerontol Geriatr. 2021;95:NPAG–NPAG.
Cella A et al. Multidimensional frailty predicts mortality better than physical frailty in community-dwelling older people: a five-year longitudinal cohort study. Int J Environ Res Public Health, 2021. 18(23).
Veronese N et al. Multidimensional Prognostic Index and Mortality in Intermediate Care facilities: a retrospective study. J Clin Med, 2021. 10(12).
Zanetti M, et al. Predictors of short- and long-term mortality among acutely admitted older patients: role of inflammation and frailty. Aging Clin Experimental Res. 2022;34(2):409–18.
Overbeek FCMS et al. The Multidimensional Prognostic Index predicts mortality in older outpatients with cognitive decline. J Clin Med, 2022. 11(9).
Pilotto A, et al. Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS ONE. 2012;7(1):e29090.
Warnier RM, et al. Validity, Reliability and Feasibility of Tools to identify Frail older patients in Inpatient Hospital Care: a systematic review. J Nutr Health Aging. 2016;20(2):218–30.
Chang SF, Lin PL. Frail phenotype and mortality prediction: a systematic review and meta-analysis of prospective cohort studies. Int J Nurs Stud. 2015;52(8):1362–74.
Lenti MV, et al. Multidimensional Prognostic Index predicts clinical outcome and mortality in hospitalised older patients with Diverticular Disease. Gerontology. 2022;68(1):44–52.
Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583.
Hayden JA, et al. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
Tadayon Najafabadi B, et al. Obesity as an independent risk factor for COVID-19 severity and mortality. Cochrane Database Syst Rev. 2023;5(5):pCd015201.
Higgins JP, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Veronese N, et al. Mortality attributable to COVID-19 in nursing home residents: a retrospective study. Aging Clin Exp Res. 2021;33(6):1745–51.
Schäfer M, et al. Risk stratification of patients undergoing Percutaneous repair of mitral and tricuspid valves using a Multidimensional Geriatric Assessment. Volume 14. Circulation: Cardiovascular Quality & Outcomes; 2021. pp. e007624–007624. 8.
Rizza S, et al. IL-6 levels influence 3-month all-cause mortality in frail hospitalized older patients. Aging Disease. 2021;12(2):353–9.
Verholt, A.B., et al., Clinical presentation and outcomes of COVID-19 in older hospitalised patients assessed by the record-based multidimensional prognostic index, a cross-sectional study. Eur Geriatr Med, 2021. 12(6): p. 1147-1157.
Hansen TK, et al. Mortality and readmission risk can be predicted by the record-based Multidimensional Prognostic Index: a cohort study of medical inpatients older than 75 years. Eur Geriatr Med. 2021;12(2):253–61.
Goudzwaard JA et al. Multidimensional Prognostic Index and outcomes in older patients undergoing transcatheter aortic valve implantation: survival of the Fittest. J Clin Med, 2021. 10(16).
Liuu E, et al. Comprehensive geriatric assessment in older patients with cancer: an external validation of the multidimensional prognostic index in a French prospective cohort study. BMC Geriatr. 2020;20(1):295.
van Mourik MS, et al. Value of a comprehensive geriatric assessment for predicting one-year outcomes in patients undergoing transcatheter aortic valve implantation: results from the CGA-TAVI multicentre registry. J Geriatr Cardiol. 2019;16(6):468–77.
Pilotto A, et al. Using the Multidimensional Prognostic Index to predict clinical outcomes of hospitalized older persons: a prospective, Multicenter, International Study. J Gerontol A. 2019;74(10):p1643–1649.
Bryant K et al. Validation and adaptation of the multidimensional prognostic index in an older Australian cohort. J Clin Med, 2019. 8(11).
Pilotto A, et al. Association of Antidementia Drugs and Mortality in Community-Dwelling Frail older patients with dementia: the role of Mortality Risk Assessment. J Am Med Dir Assoc. 2018;19(2):162–8.
Bureau M-L, et al. Using a multidimensional prognostic index (MPI) based on comprehensive geriatric assessment (CGA) to predictmortality in elderly undergoing transcatheter aortic valve implantation. Int J Cardiol. 2017;236:381–6.
Volpato S, et al. Multidimensional Prognostic Index predicts mortality and length of Stay during hospitalization in the older patients: a Multicenter prospective study. Journals Gerontol Ser A: Biol Sci Med Sci. 2015;70(3):323–9.
Pilotto A, et al. Development and validation of a Multidimensional Prognostic Index for Mortality based on a standardized Multidimensional Assessment schedule (MPI-SVaMA) in Community-Dwelling older subjects. J Am Med Dir Assoc. 2013;14(4):287–92.
Giantin V, et al. Does the multidimensional prognostic index (MPI), based on a comprehensive geriatric assessment (CGA), predict mortality in cancer patients? Results of a prospective observational trial. J Geriatric Oncol. 2013;4(3):208–17.
Sancarlo D, et al. A Multidimensional Prognostic Index (MPI) based on a comprehensive geriatric assessment predicts short- and long-term all-cause mortality in older hospitalized patients with transient ischemic attack. J Neurol. 2012;259(4):670–8.
Pilotto A, et al. Addition of the multidimensional prognostic index to the estimated glomerular filtration rate improves prediction of long-term all-cause mortality in older patients with chronic kidney disease. Rejuven Res. 2012;15(1):82–8.
Pilotto A et al. Comparing the Prognostic Accuracy for all-cause mortality of Frailty instruments: a multicentre 1-Year Follow-Up in hospitalized older patients. PLoS ONE, 2012. 7(1).
Veronese N. Frailty as Cardiovascular Risk factor (and Vice Versa). Adv Exp Med Biol. 2020;1216:51–4.
Bone AE, et al. Sarcopenia and frailty in chronic respiratory disease. Chron Respir Dis. 2017;14(1):85–99.
McGuigan FE, Bartosch P, Åkesson KE. Musculoskeletal health and frailty. Best Pract Res Clin Rheumatol. 2017;31(2):145–59.
Wilson D, et al. Frailty and Sarcopenia: the potential role of an aged immune system. Ageing Res Rev. 2017;36:1–10.
Ko D, et al. Frailty and Cardiovascular Mortality: a narrative review. Curr Cardiol Rep. 2023;25(4):249–59.
Hamaker M, et al. Intrinsic capacity and resilience: taking frailty to the next level. J Geriatr Oncol. 2023;14(2):101421.
Lovett RM, et al. Cognitive impairment no dementia and associations with health literacy, self-management skills, and functional health status. Patient Educ Couns. 2020;103(9):1805–11.
Jehu DA, et al. Risk factors for recurrent falls in older adults: a systematic review with meta-analysis. Maturitas. 2021;144:23–8.
Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English Longitudinal Study of Ageing. Age Ageing. 2018;47(3):392–7.
Ge L, Yap CW, Heng BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. 2022;22(1):26.
Sezgin D, et al. The effectiveness of intermediate care including transitional care interventions on function, healthcare utilisation and costs: a scoping review. Eur Geriatr Med. 2020;11(6):961–74.
Funding
This work was supported by the Science and Technology Research Project of Education Department of Jilin Province (grant number: JJKH20200080KJ and grant number: JJKH20240105KJ) and the Health Science and Technology Capacity Enhancement Project of Jilin Province (grant number: 2023LC024).
Author information
Authors and Affiliations
Contributions
WL, BBM and YJL conceived and designed the study idea. TYL, BRQ and KY performed the search, quality assessment, and extraction of the data. ZC, RXQ and YMQ contributed to the analysis and interpretation of data. All authors contributed to the writing and editing of the manuscript and agreed to the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable (because this is a system review article).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, W., Qin, R., Qiu, Y. et al. Multidimensional frailty as a predictor of mortality among older adults: a systematic review and meta-analysis. BMC Geriatr 24, 793 (2024). https://doi.org/10.1186/s12877-024-05377-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05377-4