Abstract
Background
Rhinovirus (RV) is one of the most common etiologic agents of acute respiratory infection (ARI), which is a leading cause of morbidity and mortality in young children. The clinical significance of RV co-detection with other respiratory viruses, including respiratory syncytial virus (RSV), remains unclear. We aimed to compare the clinical characteristics and outcomes of children with ARI-associated RV-only detection and those with RV co-detection—with an emphasis on RV/RSV co-detection.
Methods
We conducted a prospective viral surveillance study (11/2015–7/2016) in Nashville, Tennessee. Children < 18 years old who presented to the emergency department (ED) or were hospitalized with fever and/or respiratory symptoms of < 14 days duration were eligible if they resided in one of nine counties in Middle Tennessee. Demographics and clinical characteristics were collected by parental interviews and medical chart abstractions. Nasal and/or throat specimens were collected and tested for RV, RSV, metapneumovirus, adenovirus, parainfluenza 1–4, and influenza A–C using reverse transcription quantitative polymerase chain reaction assays. We compared the clinical characteristics and outcomes of children with RV-only detection and those with RV co-detection using Pearson’s χ2 test for categorical variables and the two-sample t-test with unequal variances for continuous variables.
Results
Of 1250 children, 904 (72.3%) were virus-positive. RV was the most common virus (n = 406; 44.9%), followed by RSV (n = 207; 19.3%). Of 406 children with RV, 289 (71.2%) had RV-only detection, and 117 (28.8%) had RV co-detection. The most common virus co-detected with RV was RSV (n = 43; 36.8%). Children with RV co-detection were less likely than those with RV-only detection to be diagnosed with asthma or reactive airway disease both in the ED and in-hospital. We did not identify differences in hospitalization, intensive care unit admission, supplemental oxygen use, or length of stay between children with RV-only detection and those with RV co-detection.
Conclusion
We found no evidence that RV co-detection was associated with poorer outcomes. However, the clinical significance of RV co-detection is heterogeneous and varies by virus pair and age group. Future studies of RV co-detection should incorporate analyses of RV/non-RV pairs and include age as a key covariate of RV contribution to clinical manifestations and infection outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Acute respiratory infection (ARI) is a leading cause of morbidity and mortality in young children and accounts for 20–40% of hospitalizations in this age group [1, 2]. The most common etiologic agents of ARI are viral pathogens, among which rhinovirus (RV) is a leading cause. Though usually associated with upper respiratory illness, RV is also associated with lower respiratory illnesses such as asthma exacerbations, bronchiolitis, and pneumonia [3].
Due to the increased availability and use of multipathogen molecular testing in clinical settings, RV is commonly detected alongside multiple respiratory viruses, including respiratory syncytial virus (RSV) [4,5,6]. The prevalence of viral co-detection in children with ARI generally ranges from 10 to 30% and is higher in those who are hospitalized, younger, and attend day care [7,8,9]. However, it remains unclear whether co-detections are associated with more severe illness [8]. Some studies have reported worse outcomes in children with viral co-detection [10], while others have reported no differences [7, 9, 11, 12]. In addition, the use of aggregated data assumes that the relationship between viral co-detection and disease severity is homogeneous across virus pairs. Therefore, analyses of aggregated data may mask the clinical significance of specific pairs [8, 13]. Therefore, we aimed to compare the clinical characteristics and outcomes of children with ARI-associated RV-only detection and those with RV co-detection—with an emphasis on RV/RSV co-detection.
Methods
Study design
We conducted a prospective viral surveillance study from November 15, 2015, to July 15, 2016, at Monroe Carell Jr. Children’s Hospital at Vanderbilt in Nashville, Tennessee. Children were enrolled 5 days per week (Monday, Wednesday, Thursday, Friday, and Sunday) from both the emergency department (ED) and inpatient service. Patients admitted to the ED were actively screened for symptoms of ARI.
Study setting and population
Children < 18 years old who presented with fever and/or respiratory symptoms of duration < 14 days were eligible if they resided in the study catchment area, which included the following nine counties in Middle Tennessee: Cheatham, Davidson, Dickson, Montgomery, Robertson, Rutherford, Sumner, Williamson, and Wilson. We selected the counties based on geographic proximity to Davidson County. We excluded children who were previously enrolled for the same episode of ARI in the past week, newborns who were never discharged, children with fever and neutropenia or a known nonrespiratory cause of symptoms, and children who were hospitalized for > 48 h.
Data collection
Research staff interviewed parents/guardians and collected data using a standardized case report form. They then performed medical chart abstractions to record additional information on clinical characteristics (e.g., final clinical diagnosis) and outcomes, including hospitalization, intensive care unit (ICU) admission, supplemental oxygen use, and length of stay. Any child readmitted more than a week after their initial enrollment with fever and/or respiratory symptoms of duration < 14 days was considered a new and unique case.
Sample collection and testing
After obtaining consent, research staff collected nose and/or throat swabs and combined them in a viral transport medium (BD) if both were collected. Specimens were stored at 2–8 °C, transported to the laboratory, and divided into multiple aliquots. Total nucleic acid extraction was performed using the Roche MagNA Pure LC automated extraction system. Using reverse transcription quantitative polymerase chain reaction (RT-qPCR) assays, all specimens were tested for rhinovirus (RV)/enterovirus, RSV, adenovirus (AdV), influenza (Flu) A, B, and C, metapneumovirus (MPV), parainfluenza virus (PIV)-1–4, and human RNase P (as an indicator of specimen quality). Cycle threshold (Ct) values served as a surrogate for viral load. Specimens were considered positive if the Ct value was less than 45 cycles. All laboratory results and clinical data were entered into a REDCap database [14]. We did not include the results of clinical viral testing in our study.
Statistical analysis
We determined descriptive statistics as absolute/relative frequency, mean/standard deviation (SD), or median/interquartile range (IQR) as appropriate. We used Pearson’s χ2 test and the two-sample t-test with unequal variances to compare categorical and continuous variables, respectively, between children with RV-only detection and those with RV co-detection. To account for children who were enrolled more than once and adjust for important covariates, we used generalized estimating equations with a logistic link and a working independence correlation structure to estimate adjusted odds ratios (aORs) and 95% confidence intervals (95% CIs) comparing the odds of hospitalization between children with RV-only detection and those with RV co-detection. We included in the model age, sex, race and Hispanic origin, tobacco smoke exposure, and history of asthma as covariates [15]. Finally, we performed a subgroup analysis of children < 2 years old with RV/RSV co-detection, RV-only detection, or RSV-only detection. Significance was determined to be achieved at a nominal level of α = 0.05 (two-tailed, where appropriate). All analyses were conducted using R (version 4.1.2).
Ethical considerations
The study protocol was approved by the Vanderbilt University Institutional Review Board, and written informed consent was obtained from parents/guardians.
Results
Study population
We screened 2300 children for eligibility and enrolled 1255 (54.6%); 1184 (97.3%) were enrolled once, and 33 (2.7%) more than once. Of children enrolled more than once, one was enrolled five times, another two were enrolled three times, and 30 were enrolled twice. Of those enrolled, we collected nose and/or throat swabs from 1251 children (99.7%) and subsequently excluded one child (0.1%) with an inconclusive test result for RV. The median age of the cohort was 2.2 years (IQR, 0.8–5.5 years). Of the 1,250 children we included in our analysis, 904 (72.3%) were virus-positive. A nasal swab alone was collected in one case (0.1%), a throat swab alone in another (0.1%), and both in the remaining 1,248 cases (99.8%). RV was the most common virus (n = 406; 44.9%), followed by RSV (n = 207; 19.3%), AdV (n = 152; 14.2%), Flu (n = 150; 14.0%), MPV (n = 106; 9.9%), and PIV (n = 51; 4.8%). Additional file 1: Table S1 presents comparisons of clinical characteristics and outcomes between children who were RV-positive and those who were RV-negative but positive for another respiratory virus.
RV co-detection
Of 406 children with RV, 289 (71.2%) had RV-only detection and 117 (28.8%) had RV co-detection (Fig. 1). Four children were enrolled twice (i.e., n = 402 unique children). The most common virus co-detected with RV was RSV (n = 43; 36.8%), followed by AdV (n = 40; 34.2%), MPV (n = 19; 16.2%), Flu (n = 17; 14.5%), and PIV (n = 10; 8.5%). In 105 cases (89.7%), one other virus was co-detected with RV, and in 12 cases (10.3%), two other viruses were co-detected with RV. The most frequently detected virus pair was RV/RSV (n = 36; 34.3% of all pairs) and the most frequently detected virus triplet was RV/RSV/AdV (n = 6; 50.0% of all triplets). The mean Ct value for RV was higher in children with RV co-detection than in children with RV-only detection (32.3 ± 4.5 vs. 28.2 ± 5.7; p < 0.001). Similarly, the mean Ct value for RV was higher in children with RV/RSV co-detection than in children with RV-only detection (32.0 ± 4.6 vs. 28.2 ± 5.7; p < 0.001). The mean Ct value for RSV was also higher in children with RV/RSV co-detection than in children with RSV-only detection (28.7 ± 5.8 vs. 26.4 ± 4.6; p = 0.029).
Clinical characteristics of children with RV-only detection and RV co-detection
The mean age at enrollment of the 406 children with RV was 3.8 years (SD, 4.1 years); 189 (46.6%) were < 2 years old, 100 (24.6%) were 2–4 years old, 79 (19.5%) were 5–9 years old, and 38 (9.4%) were 10–17 years old. Boys outnumbered girls 247 (60.8%) to 159 (39.2%) for a male-to-female ratio of 1.6. By race and Hispanic origin, 158 children (38.9%) were non-Hispanic black, 123 (30.3%) were non-Hispanic white, 97 (23.9%) were Hispanic, and 28 (6.9%) were non-Hispanic other.
The clinical characteristics of children with RV-only detection and those with RV co-detection are compared in Table 1. Children with RV co-detection were, on average, younger, had a longer mean duration of illness at presentation, were more likely to attend day care or preschool, were more likely to have received antibiotics for the illness before presentation, and were less likely to have a history of asthma than children with RV-only detection. Children with RV/RSV co-detection were older, had a longer duration of illness at presentation, were more likely to have received antibiotics for the illness before presentation, and were less likely to have a history of asthma than children with RV-only detection. Race and Hispanic origin was associated with RV/RSV co-detection (p = 0.042), with non-Hispanic white children being the most likely to have RV/RSV co-detection.
Clinical presentation of children with RV-only detection and RV co-detection
The most common presenting signs and symptoms were cough (n = 367; 90.4%), rhinorrhea (n = 354; 87.2%), and congestion (n = 352; 86.7%). Children with RV co-detection were more likely than children with RV-only detection to present with rhinorrhea, congestion, irritability, loud or noisy breathing, fever, diarrhea, and chills (Fig. 2). The subset of children with RV/RSV co-detection had a distinct clinical presentation; they were more likely than children with RV-only detection to present with cough, rhinorrhea, congestion, irritability, loud or noisy breathing, rapid or shallow breathing, fever, difficulty breathing, wheezing, nasal flaring, retractions, diarrhea, and apnea (Additional file 1: Fig. S1).
Diagnoses of children with RV-only detection and RV co-detection
Of all 406 children with RV, 283 (69.7%) were discharged from the ED and 123 (30.3%) were hospitalized. The diagnoses of the study population, stratified by RV detection status, are summarized in Fig. 3 and Additional file 1: Fig. S2. The most common diagnoses in children discharged from the ED were asthma (n = 51; 18.0%), otitis media (n = 28; 9.9%), and pharyngitis (n = 26; 9.2%). Children with RV co-detection who were discharged from the ED were less likely to be diagnosed with asthma or reactive airway disease (RAD) than children with RV-only detection (10.1% vs. 21.6%, respectively; p = 0.019) but more likely to be diagnosed with bronchiolitis (18.0% vs. 1.5%, respectively; p < 0.001). Though children with RV/RSV co-detection were also more likely to be diagnosed with bronchiolitis than children with RV-only detection (35.0% vs. 1.5%; p < 0.001), the likelihood of an asthma/RAD diagnosis was similar between the two groups (15.0% vs. 21.6%, respectively; p = 0.49).
The most common diagnoses in hospitalized children were asthma/RAD (n = 43; 35.0%), bronchiolitis (n = 23; 18.7%), and pneumonia (n = 17; 13.8%). Hospitalized children with RV-codetection were less likely to be diagnosed with asthma/RAD than children with RV-only detection (7.1% vs. 43.2%, respectively; p < 0.001) but more likely to be diagnosed with bronchiolitis (32.1% vs. 14.7%, respectively; p = 0.038) and pneumonia (32.1% vs. 8.4%, respectively; p = 0.001). Similarly, children with RV/RSV co-detection were less likely to be diagnosed with asthma/RAD than children with RV-only detection (0.0% vs. 43.2%, respectively; p < 0.001) but more likely to be diagnosed with bronchiolitis (56.2% vs. 14.7%, respectively; p < 0.001) and pneumonia (32.1% vs. 8.4%, respectively; p = 0.048).
Outcomes of children with RV-only detection and RV co-detection
The proportions of children who were hospitalized did not significantly differ between the RV-only detection (32.9%) and RV co-detection (23.9%) groups (p = 0.076; Table 1). Among children who were hospitalized, the proportions of children who were admitted to the ICU (9.5% and 14.3%, respectively; p = 0.47) or required supplemental oxygen (38.9% and 57.1%, respectively; p = 0.088) did not differ. In addition, the mean lengths of stay were not different between groups (2.0 ± 2.6 days and 2.9 ± 2.2 days, respectively; p = 0.097). Two children (both of whom had RV-only detection) were intubated, and none of the children received extracorporeal membrane oxygenation or died. Results from our logistic regression model for odds of hospitalization are shown in Table 2. We found that age at enrollment (aOR [95% CI], 0.86 [0.79–0.93]; p < 0.001), black, non-Hispanic origin (0.26 [0.14–0.45]; p < 0.001), Hispanic origin (0.34 [0.18–0.63]; p < 0.001), and history of asthma (3.37 [1.82–6.40]; p < 0.001) were associated with odds of hospitalization. Importantly, RV co-detection was not a significant predictor of hospitalization (0.59 [0.34–1.00], p = 0.054). Our subgroup analysis comparing children with RV-only detection and those with RV/RSV co-detection (Table 3) showed a similar pattern of results, with one exception; the odds of hospitalization were lower in boys than in girls (0.56 [0.34–0.92]; p = 0.023). RV/RSV co-detection was not a significant predictor of hospitalization (1.23 [0.56–2.67], p = 0.60).
Analysis of children < 2 years old with RV/RSV co-detection, RV-only detection, or RSV-only detection
The clinical characteristics and outcomes of children with RV/RSV co-detection and those with RSV-only detection were largely similar, while those of children with RV/RSV co-detection and those with RV-only detection were largely distinct (Additional file 1: Table S2). Notably, young children with RV/RSV co-detection were more likely than young children with RV-only detection to be admitted to the ICU (21.4% vs. 4.3%, respectively; p = 0.040) and require supplemental oxygen (64.3% vs. 27.7%, respectively; p = 0.012).
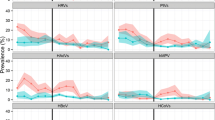
Seasonality
RV was the most common virus throughout the study months except in early winter (December) and midwinter (January), when RSV predominated (Fig. 4). Overall, RV detections peaked in early spring (March) and dropped to a nadir in midsummer (July). RV-only detections peaked in early spring (March), while RV co-detections peaked in late winter (February).
a Seasonality of rhinovirus (RV), respiratory syncytial virus (RSV), metapneumovirus (MPV), adenovirus (AdV), parainfluenza virus (PIV), and influenza (Flu) detected in 904 virus-positive children with acute respiratory infection in Middle Tennessee between November 15, 2015, and July 15, 2016. b Area plot of RV-only detections and RV co-detections in the same population and period
Discussion
In our prospective viral surveillance study of 1250 children with ARI enrolled from November 2015 to July 2016, we found that RV was the most frequently detected respiratory virus, while RV/RSV was the most frequent virus co-detection. We also found that children with RV co-detection were younger, on average, than children with RV-only detection, had a longer duration of illness at presentation, were similarly or more likely to present with all but one of the symptoms reported, were less likely to be diagnosed with asthma/RAD but more likely to be diagnosed with bronchiolitis if discharged from the ED, and were less likely to be diagnosed with asthma/RAD but more likely to be diagnosed with bronchiolitis or pneumonia if hospitalized. However, RV co-detection was not significantly associated with hospitalization in unadjusted or adjusted analyses, and among children who were hospitalized, the proportions of those who were admitted to the ICU or required supplemental oxygen were similar between groups, as were the lengths of stay. Finally, we performed a subgroup analysis of children with RV-only detection compared with those with RV/RSV co-detection and found that, although outcomes did not significantly differ between groups, the clinical presentation of children with RV/RSV co-detection was distinct from that of children with any RV co-detection.
The RV/RSV pair was the most frequent co-detection in our study, which is expected because RV and RSV are the most common causes of upper and lower respiratory infection, respectively, in children and the two most common respiratory viruses in viral surveillance studies [16, 17]. Given that RSV was positive in more than one-third of co-detected cases, the clinical characteristics of RSV-associated ARI may explain many of the differences between children with RV-only detection and those with RV co-detection. For example, RSV is the leading cause of hospitalization in children with ARI, which may explain our finding that children with RV co-detection were younger, on average, than those with RV-only detection [18]. In support, we showed that most children with RSV were < 2 years old, and in our subgroup analysis comparing children with RV-only detection and those with RV/RSV co-detection, the difference in the age at enrollment was more pronounced than in the main analysis.
The effect of viral co-infection on the severity of ARI remains unclear, and results from systematic reviews and meta-analyses are conflicting [7, 8, 19,20,21]. The heterogeneity of results may be explained by distinct virus-virus interactions that are obscured by analyses of aggregated data. DaPalma et al. identified 15 subtypes of virus-virus interactions that may ultimately attenuate or accentuate the severity of clinical disease [22]. In our subgroup analyses, we compared children with RV-only detection and those with RV/RSV co-detection and found that co-detection was not associated with hospitalization. In children who were hospitalized, we found no evidence that RV/RSV co-detection conferred worse outcomes. In support, Li et al. conducted a systematic review and meta-analysis comparing children < 5 years old with RSV-only detection and those with RSV co-detection and found no evidence that RV/RSV co-detection portended worse outcomes [23]. However, Comte et al. found that children ≤ 2 years old with RV/RSV co-detection were more likely than children with RV-only detection to have severe disease [24]. The discrepancy between our results and those of Comte et al. is likely a result of age differences; RV is associated with a considerable proportion of asthma exacerbations, and most asthma cases are diagnosed in children > 2 years old—a population that was not included in their study [24, 25]. Indeed, asthma/RAD was the most common diagnosis in our study, and most children with asthma/RAD were 2–17 years old. Our main analysis also showed no differences in outcome between children with RV-only and those with RV co-detection, but further studies of specific RV/non-RV pairs are needed to validate these results.
Based on the differential clinical characteristics of children with RV-only detection and those with RV/RSV co-detection as well as the results reported by Comte et al., we speculated that RSV was driving the clinical presentation of children with RV/RSV co-detection [24]. Compared to children with RV-only detection, those with RV/RSV co-detection were more likely to have multiple signs and symptoms associated with lower respiratory tract infections, and they were more likely to be diagnosed with bronchiolitis if discharged from the ED and more likely to be diagnosed with bronchiolitis or pneumonia if admitted. To test our hypothesis, we performed a comparison of the clinical characteristics and outcomes of children < 2 years old with RV/RSV co-detection and those with RV-only or RSV-only detection. We found that the clinical characteristics and outcomes of children < 2 years old with RV/RSV co-detection and those with RSV-only detection were alike, while children < 2 years old with RV-only detection were less likely than those with RV/RSV co-detection to have signs and symptoms of respiratory distress, less likely to be diagnosed with bronchiolitis if discharged from the ED or admitted, and less likely to be admitted to the ICU and require supplemental oxygen if hospitalized. Therefore, our results are consistent with the hypothesis that RV acts as a “bystander” in young children with RV/RSV co-detection [26]. Nevertheless, our study lacks long-term follow-up, precluding us from studying whether RV/RSV co-detection predisposes children to subsequent wheezing in later life, which must be addressed in a future study.
The strengths of our study include enrollment of children of all ages from both the ED and inpatient service, systematic collection of nose and/or throat swabs from each participant regardless of provider-ordered testing, and RT-qPCR testing for a wide spectrum of common viral etiologies of pediatric ARI. We also note some limitations. First, our PCR panel did not include all frequently encountered respiratory viruses, such as bocavirus and endemic coronaviruses. We nonetheless detected at least one virus in 72.3% of all children, which is equivalent to the proportion of children with ARI in a previous study who tested positive for at least one virus using a pathogen panel that included bocavirus and the endemic coronaviruses [27]. Second, the catchment area in our single-center study included nine counties in Middle Tennessee, and the dates of enrollment spanned less than a year; therefore, our results may not be generalizable to other regions in the United States. In addition, as with many other viruses, pathogenicity is affected by the specific strain or genotype of RV, which is subject to seasonal variation [28]. Therefore, that our study spans a single respiratory season is an important limitation, and future studies should span multiple seasons. Third, we interpreted any Ct value (up to 45, the number of assay cycles) to indicate pathogen presence. While very low viral loads can be difficult to resolve from nonspecific amplification, all PCR growth curves were inspected for features of authentic target amplification, followed by retesting of specimens yielding ambiguous results. Furthermore, of 1,072 detections, only 0.4% (n = 4) were defined as positive based on a Ct value exceeding 40. Finally, we performed a subgroup analysis of only the most common RV/non-RV pair, namely RV/RSV, because of sample size limitations. The clinical significance of other RV/non-RV pairs should be explored in further studies, as should the clinical significance of individual RV species and serotypes paired with RSV or other respiratory viruses. In addition, the clinical significance of these pairs should be explored in the context of specific clinical diagnoses, such as asthma exacerbation, bronchiolitis, and pneumonia.
In conclusion, aggregated analysis showed no evidence that RV co-detection was associated with poorer outcomes, consistent with previous reports. However, our subset analyses showed that the clinical significance of RV co-detection is heterogeneous and varies by virus pair and age group. Future studies of RV co-detection should incorporate analyses of RV/non-RV pairs and include age as a key covariate of RV contribution to clinical manifestations and infection outcomes.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request.
Abbreviations
- ARI:
-
Acute respiratory infection
- RV:
-
Rhinovirus
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- RT-qPCR:
-
Reverse transcription quantitative polymerase chain reaction
- RSV:
-
Respiratory syncytial virus
- AdV:
-
Adenovirus
- Flu:
-
Influenza
- MPV:
-
Metapneumovirus
- PIV:
-
Parainfluenza virus
- Ct:
-
Cycle threshold
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- RAD:
-
Reactive airway disease
References
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027–35. https://doi.org/10.1016/S0140-6736(16)31593-8.
Brini Khalifa I, Hannachi N, Guerrero A, Orth-Höller D, Bhiri S, Bougila J, Boughamoura L, Merchaoui SN, Sboui H, Mahdhaoui N, Schiela B, Laer DH, Boukadida J, Stoiber H. Demographic and seasonal characteristics of respiratory pathogens in neonates and infants aged 0 to 12 months in the Central-East region of Tunisia. J Med Virol. 2019;91(4):570–81. https://doi.org/10.1002/jmv.25347.
Jacobs SE, Lamson DM, St George K, Walsh TJ. Human rhinoviruses. Clin Microbiol Rev. 2013;26(1):135–62. https://doi.org/10.1128/CMR.00077-12.
Hendley JO, Gwaltney JM Jr. Viral titers in nasal lining fluid compared to viral titers in nasal washes during experimental rhinovirus infection. J Clin Virol. 2004;30(4):326–8. https://doi.org/10.1016/j.jcv.2004.02.011.
van de Pol AC, Wolfs TF, Jansen NJ, van Loon AM, Rossen JW. Diagnostic value of real-time polymerase chain reaction to detect viruses in young children admitted to the paediatric intensive care unit with lower respiratory tract infection. Crit Care. 2006;10(2):R61. https://doi.org/10.1186/cc4895.
Freymuth F, Vabret A, Galateau-Salle F, Ferey J, Eugene G, Petitjean J, Gennetay E, Brouard J, Jokik M, Duhamel JF, Guillois B. Detection of respiratory syncytial virus, parainfluenzavirus 3, adenovirus and rhinovirus sequences in respiratory tract of infants by polymerase chain reaction and hybridization. Clin Diagn Virol. 1997;8(1):31–40. https://doi.org/10.1016/s0928-0197(97)00060-3.
Scotta MC, Chakr VC, de Moura A, Becker RG, de Souza AP, Jones MH, Pinto LA, Sarria EE, Pitrez PM, Stein RT, Mattiello R. Respiratory viral coinfection and disease severity in children: a systematic review and meta-analysis. J Clin Virol. 2016;80:45–56. https://doi.org/10.1016/j.jcv.2016.04.019.
Goka EA, Vallely PJ, Mutton KJ, Klapper PE. Single and multiple respiratory virus infections and severity of respiratory disease: a systematic review. Paediatr Respir Rev. 2014;15(4):363–70. https://doi.org/10.1016/j.prrv.2013.11.001.
Wishaupt JO, van der Ploeg T, de Groot R, Versteegh FG, Hartwig NG. Single- and multiple viral respiratory infections in children: disease and management cannot be related to a specific pathogen. BMC Infect Dis. 2017;17(1):62. https://doi.org/10.1186/s12879-016-2118-6.
Debiaggi M, Canducci F, Ceresola ER, Clementi M. The role of infections and coinfections with newly identified and emerging respiratory viruses in children. Virol J. 2012;9:247. https://doi.org/10.1186/1743-422X-9-247.
Bekhof J, Bakker J, Reimink R, Wessels M, Langenhorst V, Brand PL, Ruijs GJ. Co-infections in children hospitalized for bronchiolitis: role of roomsharing. J Clin Med Res. 2013;5(6):426–31. https://doi.org/10.4021/jocmr1556w.
Asner SA, Rose W, Petrich A, Richardson S, Tran DJ. Is virus coinfection a predictor of severity in children with viral respiratory infections? Clin Microbiol Infect. 2015;21(3):26416.e1-6. https://doi.org/10.1016/j.cmi.2014.08.024.
Lim FJ, Wake ZV, Levy A, Tempone S, Moore HC, Richmond PC, de Klerk N, Conway NT, Keil AD, Effler PV, Smith DW, Blyth CC, WAIVE group. Viral etiology and the impact of Codetection in Young Children presenting with Influenza-Like Illness. J Pediatr Infect Dis Soc. 2017;6(3):260–6. https://doi.org/10.1093/jpids/piw042.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Diggle P, Heagerty P, Liang KY, Zeger S. Analysis of Longitudinal Data. In: Oxford Statistical Science Series. 2nd ed. Oxford: Oxford University Press; 2013.
Mahony JB, Petrich A, Smieja M. Molecular diagnosis of respiratory virus infections. Crit Rev Clin Lab Sci. 2011;48(5–6):217–49. https://doi.org/10.3109/10408363.2011.640976.
Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, O’Brien KL, Roca A, Wright PF, Bruce N, Chandran A, Theodoratou E, Sutanto A, Sedyaningsih ER, Ngama M, Munywoki PK, Kartasasmita C, Simões EA, Rudan I, Weber MW, Campbell H. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545–55. https://doi.org/10.1016/S0140-6736(10)60206-1.
Calvo C, García-García ML, Blanco C, Pozo F, Flecha IC, Pérez-Breña P. Role of rhinovirus in hospitalized infants with respiratory tract infections in Spain. Pediatr Infect Dis J. 2007;26(10):904–8. https://doi.org/10.1097/INF.0b013e31812e52e6.
Martin ET, Kuypers J, Wald A, Englund JA. Multiple versus single virus respiratory infections: viral load and clinical disease severity in hospitalized children. Influenza Other Respir Viruses. 2012;6(1):71–7. https://doi.org/10.1111/j.1750-2659.2011.00265.x.
Lim FJ, de Klerk N, Blyth CC, Fathima P, Moore HC. Systematic review and meta-analysis of respiratory viral coinfections in children. Respirology. 2016;21(4):648–55. https://doi.org/10.1111/resp.12741.
Asner SA, Science ME, Tran D, Smieja M, Merglen A, Mertz D. Clinical disease severity of respiratory viral co-infection versus single viral infection: a systematic review and meta-analysis. PLoS ONE. 2014;9(6):e99392. https://doi.org/10.1371/journal.pone.0099392.
DaPalma T, Doonan BP, Trager NM, Kasman LM. A systematic approach to virus-virus interactions. Virus Res. 2010;149(1):1–9. https://doi.org/10.1016/j.virusres.2010.01.002.
Li Y, Pillai P, Miyake F, Nair H. The role of viral co-infections in the severity of acute respiratory infections among children infected with respiratory syncytial virus (RSV): a systematic review and meta-analysis. J Glob Health. 2020;10(1):010426. https://doi.org/10.7189/jogh.10.010426.
Comte A, Bour JB, Darniot M, Pitoiset C, Aho-Glélé LS, Manoha C. Epidemiological characteristics and clinical outcomes of human rhinovirus infections in a hospitalized population. Severity is independently linked to RSV coinfection and comorbidities. J Clin Virol. 2020;125:104290. https://doi.org/10.1016/j.jcv.2020.104290.
Radhakrishnan DK, Dell SD, Guttmann A, Shariff SZ, Liu K, To T. Trends in the age of diagnosis of childhood asthma. J Allergy Clin Immunol. 2014;134(5):1057-1062e5. https://doi.org/10.1016/j.jaci.2014.05.012.
Gerna G, Piralla A, Rovida F, Rognoni V, Marchi A, Locatelli F, Meloni F. Correlation of rhinovirus load in the respiratory tract and clinical symptoms in hospitalized immunocompetent and immunocompromised patients. J Med Virol. 2009;81(8):1498–507. https://doi.org/10.1002/jmv.21548.
Rhedin S, Lindstrand A, Rotzén-Östlund M, Tolfvenstam T, Ohrmalm L, Rinder MR, Zweygberg-Wirgart B, Ortqvist A, Henriques-Normark B, Broliden K, Naucler P. Clinical utility of PCR for common viruses in acute respiratory illness. Pediatrics. 2014;133(3):e538-545. https://doi.org/10.1542/peds.2013-3042.
Moore ML, Stokes KL, Hartert TV. The impact of viral genotype on pathogenesis and disease severity: respiratory syncytial virus and human rhinoviruses. Curr Opin Immunol. 2013;25(6):761–8. https://doi.org/10.1016/j.coi.2013.09.016.
Acknowledgements
None.
Funding
This work was supported by the Centers for Disease Control and Prevention Emerging Infections Program Cooperative Agreement (1U50CK000491) and Clinical and Translational Science Awards Program (UL1TR000445). Danielle A. Rankin is supported by the National Institutes of Health (TL1TR002244).
Author information
Authors and Affiliations
Contributions
Conceptualization: TMM, MLL, WS, NBH; formal analysis: JZA, MP, DAR, VP, ZH, HR, AJS; investigation: JT, VP, LSS; methodology: MLL, WS, NBH; writing – original draft: JZA; writing – review and editing: MP, JT, DAR, VP, ZH, AY, RT, JC, WS, AJS, NBH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Vanderbilt University Institutional Review Board, and written informed consent was obtained from parents/guardians. The study was conducted according to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Natasha Halasa, MD, MPH, receives grant support from Sanofi Pasteur, Quidel, and speaker compensation from an education grant supported by Genentech. Sanofi Pasteur also donated vaccines and influenza antibody testing for an influenza vaccine trial. The remaining authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary analyses of the clinical characteristics and outcomes of children with single or co-detected rhinovirus-associated acute respiratory infection in Middle Tennessee.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amarin, J.Z., Potter, M., Thota, J. et al. Clinical characteristics and outcomes of children with single or co-detected rhinovirus-associated acute respiratory infection in Middle Tennessee. BMC Infect Dis 23, 136 (2023). https://doi.org/10.1186/s12879-023-08084-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08084-4