Abstract
Background
In 2012, the World Health Organization recommended screening and investigation of contacts of index tuberculosis patients as a strategy to accelerate detection of tuberculosis (TB) cases. Nine years after the adoption of this recommendation, coverage of TB contact investigations in Uganda remains low. The objective of this study was to examine health care providers’ perceptions of factors influencing coverage of TB contact investigations in three selected rural health facilities in Mbarara district, southwestern Uganda.
Methods
This study identified provider opinions on the barriers and facilitators to implementation of TB contact investigation using the Consolidated Framework for Implementation Research. Using an exploratory qualitative study design, semi-structured interviews with 19 health workers involved in the TB program at district, health facility and community levels were conducted from April 2020 and July 2020. Analysis was conducted inductively using reflexive thematic analysis in six iterative steps: familiarizing with the data, creating initial codes, searching for themes, reviewing themes, developing theme definitions, and writing the report.
Results
Nineteen health care workers participated in this study which translates to a 100% response rate. These included two district TB and leprosy supervisors, five nurses, five clinical officers, six village health team members and one laboratory technician. The three themes that emerged from the analysis were intervention-related, health system and contextual factors. Health system-related barriers included inadequate or delayed government funding for the TB program, shortage of human resources, insufficient personal protective equipment, and a stock-out of supplies such as Xpert MTB cartridges. Contextual barriers included steep terrain, poverty or low income, and the stigma associated with TB and COVID-19. Facilitators comprised increased knowledge and understanding of the intervention, performance review and on-the-job training of health workers.
Conclusions
This study found that most of the factors affecting TB contact investigations in this rural community were related to health system constraints such as inadequate or delayed funding and human resource shortages. This can be addressed by strengthening the foundational elements of the health system - health financing and human resources - to establish a comprehensive TB control program that will enable the efficient identification of missing TB patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An estimated 10 million people suffer from active tuberculosis (TB) every year [1]. The disease continues to be the leading infectious cause of death globally, causing about 1.5 million deaths—95% of which occurred in low- and middle-income countries [2, 3]. Although the African region has 9% of the world population, the region contributed 25% of all new TB cases in 2019, becoming the continent with the second-highest TB cases after South-East Asia. In Africa TB is mainly driven by the HIV pandemic, with about 50% of TB cases co-infected with HIV, and is the top cause of death among patients with HIV, causing more than 30% of all AIDS-related deaths [4, 5].
In 2012, the WHO recommended the screening and evaluation of contacts of persons with infectious TB as an intervention for increasing TB case detection [6]. The intervention also provides an opportunity to diagnose latent TB and to scale-up TB preventive therapy among the eligible contacts, such as, children below five years, HIV positive patients, and other high-risk groups [7, 8]. Five years later, in 2017, the Uganda Ministry of Health (MoH) adopted these WHO recommendations as high-level policy, and integrated them into the Manual for Management and Control of TB and Leprosy in Uganda [9]. Furthermore, in 2019, detailed operational guidelines were developed by the Uganda National Tuberculosis and Leprosy Program (NTLP) to guide and standardize TB contact investigation processes at health facility and community levels [8].
Despite the WHO policy guidance, coverage of TB contact investigation in many TB high burden countries such as Uganda, Kenya, Lao Republic, Pakistan and Yemen is still low [10]. A meta-analysis conducted in 2015 by Block et al., showed low TB contact investigation coverage in five countries (2.8% in the Lao Republic, 4.8% in Kenya, 14.9% in Pakistan and 15.1% in Uganda) and high coverage in one country (91.7% in the Democratic Republic of Congo) [10]. Armstrong et al. (2017), in a prospective multi-center observational study conducted in Kampala, Uganda, reported significant drop-out rates across the steps in the contact investigation cascade [11]. Among the 338 clients eligible for TB contact investigation, only 61% were scheduled for home visits, and only 50% of them were visited [11]. Furthermore, among the 131 people who were screened for TB and required definitive evaluation, only 20% were evaluated [11].
In rural Uganda, the coverage of TB contact investigation is much lower (15.1%) than that in urban areas such as Kampala (20%), and yet many of the missing TB cases are in such hard to reach and underserved rural areas [10, 11]. This low coverage increases undiagnosed and untreated TB patients, thus perpetuating the TB pandemic. Furthermore, without TB contact investigation, many TB patients might infect other people in the household and the community, or die from TB related complications [12]. The low contact investigation coverage contributes to a high numbers of missed diagnoses in Uganda (400,000 in 2014), and high TB transmission rates, which hamper progress towards achievement of the third United Nations Sustainable Development Goal of ending the TB epidemic by 2030 [13].
Implementation research helps to connect research and practice by speeding-up the development and provision of public health interventions [14]. Given that urban settings have been the primary focus of the majority of implementation research studies in Africa and that the burden of TB differs between urban and rural areas [7, 15, 16], this study used implementation research tools to investigate the barriers to and enablers of TB contact investigation coverage in rural southwestern Uganda [3]. Although 82% of the Ugandan population lives in rural areas, there is inadequate information about TB contact investigation coverage, and its barriers and facilitators in rural settings [17]. The purpose of this study was to investigate the barriers and facilitators of investigation coverage among contacts of TB patients in rural Uganda.
The Consolidated Framework for Implementation Research (CFIR) by Damschroder et al. was used to explore barriers and facilitators of implementation in this study [18]. The framework consists of 39 constructs and five domains: characteristics of the intervention, inner setting, outer setting, individuals involved and implementation process [18]. The framework has been widely used across the globe to identify the barriers and facilitators of implementation outcomes in various healthcare settings, for example, evaluation of the online frailty tool in primary health care in Canada, integration of hypertension-HIV management in three Ugandan HIV clinics, examining the task shifting strategy for hypertension control at 32 hospitals and community health centers in Ghana and evaluating the implementation context of a quality improvement program for increasing vaccination coverage in Nigeria [19,20,21,22].
Methods
Study setting
This study was conducted in the rural district of Mbarara, located in the southwestern region of Uganda, about 270 km southwest of the capital city, Kampala. According to the 2014 population and housing census, the district had a population of 472,629 (Land area 1785.6 km2), of which 59% resided in rural areas [23]. In total the district had 87 health facilities including 48 government owned, 26 private clinics and 13 nonprofit health facilities [24]. There were no data on TB contact investigation available at district level. Health Centres (HC) in Uganda are ranked II, III or IV based on the administrative zone served by the health facility with level II serving a parish, level III serving a sub-county and level IV serving a county [25]. A HC IV is expected to serve a population of at least 100,000 people. The services offered included general outpatient clinic (including TB and HIV care), immunization, antenatal care, maternity services, inpatient, laboratory, emergency surgery and blood transfusion [25].
The Ugandan health system operates on a referral basis, with the lowest level of health care provided by community health workers called Village Health Teams (VHTs) and the highest level of care offered at highly specialized hospitals called National Referral Hospitals. Levels of health care increase with complexity in terms of the packages of services offered, staffing levels, and the size of the population served. Three health facilities where the study was conducted were purposively selected due to their rural location, level of care (IV), and significant volume of patients compared to lower levels (II and III).
Coordination of TB services in the district was done by the District TB and Leprosy Supervisor (DTLS), who is responsible for 26 TB diagnostic and treatment centers. Regional coordination of TB activities is done by the Zonal TB and Leprosy Supervisor (ZTLS), while national level coordination and policy formulation is done by the National TB and Leprosy Program (NTLP) [15].
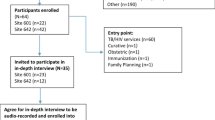
Study design and study population
A qualitative, exploratory study design was conducted to identify barriers and facilitators to implementing TB contact investigations between April and July 2020. Semi-structured interviews were conducted with all 19 health workers who were purposively selected based on their direct participation in the implementation of TB interventions since they were likely to have the most knowledge and experience with TB contact investigations. These included TB focal persons at the health facilities, clinical officers, nurses, laboratory staff, VHTs, and District TB and Leprosy Supervisors. Health workers who were not in the health facility during the data collection period were excluded from the study. The Consolidated criteria for reporting qualitative studies (COREQ) were applied to comply with the reporting standards (Table S2) [26].
Data collection
Semi-structured interview guides were developed and included background information about study participants and questions developed according to the five domains of the CFIR. The VHT interview guides were translated into the regional dialect and put through a pilot test to ensure that the questions were understood and to gauge how long the interviews would take. Two health facilities that provided comparable research sites in terms of staffing levels and services were used for the pilot testing.
Physical interviews for the study participants were conducted by the lead researcher (PT) in either English or Runyankore and each interview was tape recorded while a trained research assistant took field notes. Data collection for each category of study participants was continued until saturation was reached [27]. Since data collection took place during the first wave of the COVID-19 pandemic, precautions were taken to prevent COVID-19 cross-infection on both the researcher and the participants. Interviews were conducted at the selected health facilities in well-ventilated spaces, with both the interviewer and the participant wearing N-95 respirators, and surgical masks, respectively. Each interview lasted between 30 and 45 min and no repeat interviews were conducted.
Data management and analysis
Data were transcribed verbatim by the research team and the lead researcher listened to each audio recording while reading through the transcripts to correct errors in transcription and familiarize himself with the data. Transcripts were not given back to the participants for review or comments because evidence suggests that interviewee transcript review does not add value to the quality and rigor of qualitative research [28]. PT and JN reviewed the transcripts and made initial notes of interesting features or potential codes and themes in the data. The transcripts were then uploaded into MAXQDA 2020, and analyzed using reflexive thematic analysis in six iterative and recursive steps as described by Braun and Clarke [29]. The six steps included (1) familiarization with the data, (2) coding, (3) searching for themes, (4) reviewing the themes, (5) naming and defining the themes, and (6) writing the report [29]. The first step of the analysis was to look at the participants’ own words and expressions, without preconceived notions or classifications. The researchers then examined the language used by each participant in relation to the five domains of the CFIR. To ensure the reliability and credibility of the research analysis, both researchers PT and JN developed the themes by reading the transcripts independently to establish inter-coder agreement [30]. After the initial coding, the two-member team met to discuss the independently developed codes and themes and to reach an agreement on the themes. The transcribed texts and quotes were then grouped into themes, and the lead researcher used a reflexive approach to identify similarities or differences among CFIR domains and constructs. This iterative and recursive process provided space for reflexivity and ensured the credibility of the research findings. Themes were then defined and further refined to reflect the challenges and enablers of contact investigation coverage.
The research team and reflexivity
The field research team consisted of the principal investigator (PT), a male master’s student at the University of the Witwatersrand, and a female research assistant (GA), who is trained in population studies and monitoring and evaluation, and she was not employed at the time of this study. The principal investigator is a medical doctor who has training and experience in TB care and is familiar with WHO TB guidelines for contact investigations. He was not affiliated with the District Health Department or the Ministry of Health NTLP and is therefore unlikely to have influenced participant responses. Prior to the study, the principal investigator received training in qualitative research methods at the University of the Witwatersrand, so he was aware of how a researcher’s background, location, and assumptions can influence a qualitative study. The research team did not know the participants beforehand, and they were not directly involved in patient care in a way that would have influenced their responses.
Ethical considerations
This study was cleared by the Human Research Ethics Committees (Medical) at the University of the Witwatersrand (M200101), and Mbarara University of Science and Technology (MUREC 1/7). The Uganda National Council for Science and Technology granted permission to conduct the study in Uganda (HS569ES). Administrative approval was obtained from the District Health Officer, and the health facility managers of the respective study sites. Information about the study was shared with the participants before the interviews and written informed consent for participation and audio recording was obtained from each participant. To preserve participant privacy, interviews were conducted in a private space within the outpatient units, with only the researchers and the participants present.
Results
Characteristics of study participants
Nineteen participants took part in semi-structured interviews with a response rate of 100% and 21.1% (n = 4) of them were male (Table 1). The sample comprised five clinical officers (26.3%), five nurses (26.3%), six VHT members (31.6%), one laboratory technician (5.2%), and two DTLs (10.5%). Eight of the participants (42.1%) had over three years’ experience in offering TB care. Clinical officers were paramedics with a diploma in clinical medicine, as opposed to nurses who had a bachelor’s degree in nursing, a diploma, or a nursing certificate. VHTs were lay health workers based in the community to aid with TB interventions in the local population. Laboratory technicians had a diploma in laboratory sciences, whereas DTLSs had one in nursing or clinical medicine.
Barriers and facilitators of TB contact investigation coverage
A reflective thematic analysis of the data gave rise to three themes: health system, contextual and intervention-related factors. The barriers and facilitators identified under each of the three themes (Table S3). Based on the WHO’s health system building blocks, the factors affecting the health system emerged under six sub-themes: human resources, commodities, service delivery, leadership and coordination, funding, and health information systems. Contextual factors were further categorized into geographic, social, and cultural, economic, and policy-related factors. Issues affecting TB contact investigations linked to the intervention itself were covered by the final theme (intervention-associated factors).
Barriers and facilitators
Domain 1: characteristics of the intervention
The intervention related factors reported by the participants fell under three constructs, that is: evidence-base, intervention complexity and implementation cost.
Evidence-base
Out of the 19 healthcare workers involved in this research, 16 were aware of the intervention and its effectiveness in detecting, treating, and stopping the spread of tuberculosis in the community. Some of them had even engaged in relevant programs at the district, health facility, and community levels to improve uptake, such as support supervision, enlisting household contacts, home visits, health education, screening, and sputum sample collection. The DTLSs reported that training and regular orientation on several aspects of TB management, including TB contact investigation, provided easy access to knowledge and information. The district provided training on TB contact investigation to health workers in different platforms, including quarterly performance review meetings. As a result, they had the necessary information, abilities, or confidence to carry out contact investigation tasks.
“Even in meetings, we talk about contact tracing and investigation. Because for us we do meetings quarterly, all those meetings we…include a training in contact tracing and investigation”(Respondent 1—Nurse).
Intervention complexity
Three VHTs reported that TB contact investigations had multiple processes and therefore required a team to go for community visits, which interfered with other ongoing interventions at the health facility, such as TB screening at outpatient clinics, linking positive patients to treatment, providing community-based DOTs for patients on treatment, and following up with clients who defaulted on treatment. They also assisted with other medical services, such as immunizations, prenatal care, and providing ART refills to stable HIV patients. Therefore, during contact investigations, VHTs were mostly involved in community activities, leaving some of the basic facility-based interventions unattended.
“…it interferes with other programs… Now I am here working at the health facility, collecting sputum, screening and… I have many patients attending immunization, antenatal, ART (HIV clinic), and I am the one who works on them too. And after that, I want to go and do contact tracing… Sometimes I ignore some of the facility activities so that I spare some time to go and do contact tracing in the community”(Respondent 4—VHT).
Cost of the intervention
During TB contact investigations, it may be required to phone many patients or contacts. It is frequently necessary to call people who have appointments but do not show up at the health facility. Healthcare workers find it challenging to make these calls due to the high airtime requirements of this intervention and the associated cost.
“…some of these contacts need to be contacted on the phone several times because someone tells you he is coming tomorrow; and he doesn’t come. And the person keeps giving appointments without coming. And we do not have all that airtime…”(Respondent 5—Clinical Officer).
Domain 2: outer setting
Funding from external entities: inadequate funding
Multiple funding related challenges were reported at national, district and health facility levels. Funding for TB contact investigation was provided, through the Primary Health Care grants released from the Ministry of Health to public health facilities. Additional funds for contact investigation came from USAID through the Regional Health Integration to Enhance Services in Southwestern Uganda; a program for scaling up access to comprehensive HIV, TB and reproductive health services in the region.
Health workers believed that TB was not considered a priority by the Ministry of Health, which led to underfunding of the NTLP, and eventually underfunded TB work at district, health facility and community levels. TB interventions were not integrated into the annual budgeting processes like other interventions. For example, Malaria and sanitation interventions received funds, while TB remained unfunded, since 2014. The DTLS reported that the sanitation program was prioritized and funded better than the TB program, because of the advocacy by the sanitation program.
“…I think if the government says, ‘let us fight this disease’, they need to put in (funds). Let them consider TB across the board. Let them budget for it like the way they budget for other conditions. Malaria is budgeted for, sanitation…receives money every quarter. But it is like six years (since 2014) when there was money for TB…and it was for only one quarter”(Respondent 1—Nurse).
The DTLSs reported insufficient funds for TB support supervision at the district level, which limited the amount of time the district TB supervisor spends in each health facility for supervision visits. Eventually, the quality of the supervision was compromised because teams did not have sufficient resources to train, mentor and supervise health facility teams.
“Because of the funds being little, we are forced, like in a day, to move to about four facilities. Remember, in TB, there are six indicators that you need to focus on and get to understand what the problem is. So, you find we do not have sufficient time to spend in the facility and support it.”(Respondent 2—Clinical Officer).
Health facility level funding challenges included delayed reimbursement of funds, and inadequate funds for home visits. In some cases, health facilities rely on NGOs for extra funds to conduct contact investigations, because of insufficient funds from the Primary Health Care (PHC) fund.
“…but when you do not have that NGO, things are challenging because you know that PHC money cannot be enough. You find that the PHC money is for only two patients, yet you have like six of them (to follow-up). So, when you do not have that money from NGOs, you cannot do it smoothly.”(Respondent 2—Clinical Officer).
Some participants reported that they used their own money to trace index TB contacts; however, this money takes a long time to be refunded. Some participants even had a pay gap of about five months, which lowered their morale to continue with community visits.
“Most of the cases, we use our own money… you want to do your job, but transport facilitation (is missing)! Even…when they decide to refund it (money), it takes so long…for example, since January we have never got that transport (money). We did contact tracing in January, February, March, April and May; we gave them reports, and they see that we are working, but we do not see our transport (refund)”(Respondent 16—VHT).
Critical incidents: COVID-19 pandemic related factors
This study was conducted during the first wave of the COVID-19 pandemic a lockdown policy was implemented by the government. This was characterized by suspension of public and private transportation, some health workers, TB patients and their contacts were unable to access health facilities. These restrictions affected the mobility of the health workers and patients to the health facility, and undermined TB contact investigation efforts. Besides lockdown measures, the COVID-19 pandemic was also associated with stigma among patients and health workers. Some TB contacts were afraid to report cough, in fear of being suspected of having COVID-19 and having to be quarantined for 14 days as per the MOH recommendations at the time. COVID-19 heightened the stigma associated with TB, because the two conditions have similar symptoms. Health workers could not tell who had COVID-19 or TB and, therefore, avoided anyone presenting with cough, because they feared it might be COVID-19. Some laboratory personnel declined to examine sputum samples because they were concerned that the samples might contain COVID-19 and increase their risk of getting the virus.
“Now with corona (COVID-19), we would come here and not find any patient or health worker because they did not have transport means during the lockdown. Most of our people stayed at home. Even if you had your own motorcycle, they would not allow you to ride it…”(Respondent 13—Clinical officer).
Partnerships and connections: collaboration with NGOs and community-based organizations
Health workers and VHTs reported that the district and health facilities are networked with NGOs and community-based organizations which support the implementation of TB contact investigation and other health interventions. The primary implementing partner was Regional Health Integration to Enhance Services in Southwestern (RHITES-SW) Uganda, which supports the district with transportation and materials, while doing household visits.
Along with funding TB contact investigation, district-based NGOs also sponsored radio airtime to increase awareness and create demand for TB services.
“…RHITES-SW provides us with materials to use, like carrier bags. They provide us with transport to do contact tracing and the information. They normally update us on each and everything that is current in contact tracing and investigation”(Respondent 5—Clinical officer).
“Other stakeholders are working hand in hand with the government and our implementing partners. I see them working as a team to sponsor airtime on radios to create awareness and give some financial assistance.”(Respondent 12, Clinical Officer).
Policies and laws: availability of updated operational guidelines
The district established favorable communication networks at district and health facility levels, facilitating efficient communication of guidelines, reference materials, and patients’ results. For example, the district had a WhatsApp group, specifically for the district TB team, to share information and monitor district activities.
“…we have a WhatsApp group of all the in charges and TB focal persons, where we discuss TB management and…share guidelines, so whoever needs guideline in TB management, he just goes there”(Respondent 1—Nurse).
Domain 3: inner setting
Available resources
The barriers that emerged under available resources included, lack of personal protective equipment (PPE), stock-outs of Xpert MTB cartridges and shortage of human resources. Commodities that frequently went out of stock included toolkits for TB contact investigations and Xpert MTB cartridges for conducting Xpert MTB and RIF tests. At times health facilities spend about two months without cartridges, and health workers were notified by the laboratory team not to send sputum samples for analysis, which weighs down contact investigation efforts. Additionally, VHTs reported the lack of essential tools for community visits, especially during extreme weather. Health facilities also frequently ran short of PPE for home-based contact screening, such as masks and gloves, which discouraged them from doing community contact tracing out of fear of acquiring TB.
“…sometimes, there are no GeneXpert (Xpert MTB) cartridges; you find that we are not doing GeneXpert (tests) because cartridges are finished…, at times we take like a month or two without cartridges and…that is not good…, the lab people tell us, ‘do not send samples this month, we do not have (cartridges)’, which means we are missing people (patients).”(Respondent 12—Clinical Officer).
“At times you go to a difficult place…in a rainy season…, you climb a hill while it is raining on you. You do not have an umbrella; you do not have boots or a bag to carry the stuff (materials)…”(Respondent 4—VHT).
Human resource shortage was also reported as barrier. Sometimes, only one health worker was available to go for community visits, yet there are multiple tasks to do, including health education, screening, and sample collection. Therefore, this scarcity of human resources affects the quality of implementation since some of the tasks are left incomplete.
“…sometimes there is a lack of manpower because…the health workers are not enough at the facility, so you find that only one person is going for contact tracing, and the work there is huge, and that person cannot do all the work alone. So, most of the things are not done. They do part of the work and leave out some”(Respondent 15—Nurse).
Two facilitators were discussed under the construct of available resources: presence of a landline telephones to aid communication and a motorcycle to support transportation during community visits. The telephones were loaded with airtime for scheduling household visits and communicating Xpert MTB/RIF results from the hub laboratory while the motorcycle helped to reduce the cost of transportation since community visits only required fuel for the motorcycle.
“We have a health facility motorcycle, which does not force us to put in a lot of money… We just consider the distance we are covering and then put in fuel and move, which is easier than getting a boda-boda (motorcycle taxi).”(Respondent 16—VHT).
Structural characteristics: rugged terrain and poor road network, paper-based reporting systems, and hub and spoke laboratory system
All six VHTs reported that some patients came from hard-to-reach areas, characterized by rugged terrain, where vehicles or motorcycles cannot reach. This makes it hard for health workers to visit such communities for contact investigations. Additionally, some places have poor roads that are impassable during the rainy season, thus affecting service delivery. In such circumstances, health workers use boda-bodas (motorcycle taxis) to a certain point, and then walk the remaining distance. Sometimes the terrain is hilly and exhausting, which discourages teams from doing community visits. Large health facility catchment areas also made it more difficult for field teams to deliver contact investigation services to distant households. As a result, contacts of index TB cases from remote places were instead asked to come to the health facility for further evaluation, however, some of them did not come.
“…for those people who come from hard-to-reach areas, going to those homes is quite challenging. Sometimes we reach a point of walking on foot because we cannot reach there using a car or a motorcycle. So, we must climb a steep hill to look for those patients”(Respondent 4—VHT).
“This is a big sub-county; people come from distant areas, even neighboring districts. And of course, as a health worker, you cannot reach every homestead. So, some (contacts) are called to come to the health facility. But because of the long distances, some fail to come.”(Respondent 4—VHT).
Another barrier was the use of the paper-based reporting system. One of the TB focal persons reported that TB contact investigation reports were submitted manually using a paper-based system which affects timeliness of reporting. Submission of reports had to wait for an opportunity when someone was going to the district headquarters, which causes a delay and eventually affects re-imbursement of the payments for activities.
“Sometimes, since we are sending the reports to Mbarara, they reach late because of transport issues. It becomes hard for someone to send the report since you cannot get any transport, so you get someone going to Mbarara, give them the reports, and tell that person where they should be delivering the reports. So, it also takes a bit of time”(Respondent 8—Nurse).
The laboratory system in the district used a “hub and spoke” system, where laboratory samples are collected in peripheral laboratories and transported by motorcycle riders to the central laboratory for analysis. However, participants reported that this system was dysfunctional because of the long results turn-around time, compromised early TB diagnosis and treatment and affected TB contact investigation coverage. In some cases, health workers spent up to two months, waiting for Xpert MTB results.
“And we have a challenge with hub riders… Sometimes, the hub riders take sputum samples to Mbarara, and if they do not go back to pick the results, you will never see them. And you end up spending around two months without results”(Respondent 12—Clinical Officer).
Domain 4: individuals involved
Under characteristics of the individuals involved, participants reported the presence of internal implementation leads called TB focal persons at health facility and DTLS at district level. These were responsible for coordinating the provision of TB services and technical leadership and supervision of the TB program and different levels of care. Additionally, health workers received adequate training on various aspects of TB management including TB contact investigation. Such training sessions supported them with the adequate knowledge and skills to confidently conduct contact investigation activities.
Domain 5: implementation process
The three constructs that emerged under implementation process were planning, engaging and reflection and evaluation.
Planning
The DTLSs reported that leaders at the Ministry of Health had transferred the planning, coordination, and funding of TB interventions, including TB contact investigation. Instead, this role was left to implementing partners, usually local and international Non-Governmental Organizations (NGOs), which negatively impacted the TB program at district level. Also, participants reported that implementing partners tend to have different priorities. For example, these organizations mainly focus on HIV interventions, and less on TB. Therefore, it is challenging to divert them from their preferences and focus them on district priorities, since their priorities are often guided by donor funding.
“Also, The Ministry of Health has deliberately left this work (TB contact investigation) …to implementing partners, and it has killed everything. And in that line, I think we can eradicate TB, but if the government is putting in (effort), not leaving this disease for the implementing partners.”(Respondent 1—Nurse).
“They tell you their priority is HIV, and you cannot shift them. They have their …operational guidelines that you cannot change.”(Respondent 1, Nurse).
Reflection and evaluation
data use to inform program decisions by the district health team was identified as a facilitator. The district held quarterly performance and reflection meetings with the participation of the district’s NGOs, community-based organizations, district health management team, and healthcare providers from the various health centers. In these meetings, attendees discussed their performance, challenges across the different technical areas, and strategies for bridging the gaps.
Engaging
the involvement of all stakeholders within the district, including health facility teams, district teams, NGOs, and community-based organizations involved in the TB program, in regular engagements to review implementation progress, performance, and plan improvement strategies was reported as a facilitator. Non-Governmental Organizations are actively involved in discussions regarding potential funding opportunities for specific activities.
“…we normally have the district stakeholders meeting, where they (external stakeholders) normally come here, and we discuss performance in different areas - MCH (maternal and child health) and HIV; TB is also given a platform. We tell them about our challenges.”(Respondent 1—Nurse).
Others
The stigma associated with TB was reported as a common challenge by all participants in this study. For this reason, index TB patients preferred not to be visited at home by a health worker, out of fear of being stigmatized if neighbors and other community members found out that they had TB. Some index TB patients even tried to avoid being visited by giving health workers incorrect phone numbers and physical addresses. Patients with TB and HIV co-infection have an increased fear of disclosing their status because of the misconception that every TB patient has HIV. Additionally, poverty among index TB patients was also found to be a challenge because contacts of TB patients lacked funds to transport them to the health facility for assessment, diagnosis, and treatment. As a result, it was necessary for health professionals to collect sputum samples from the community and bring them to the health facility for analysis. This, however, was not always feasible, leaving some of the contacts of TB patients unevaluated.
“…some patients give us wrong telephone contacts, we call the number, it is not on, or a different person picks it. So, we fail to trace that person. Some fear health workers going to their homes. Mostly when the index TB patient is also HIV positive, they do not want people in their villages to see any health care worker coming to their home because they may identify them”(Respondent 11—VHT).
Discussion
This study explored the factors influencing TB contact investigation coverage in three rural, primary health facilities in Southwestern Uganda. The study is unique in its rural focus unlike previous studies in Uganda and Kenya, which were conducted in cities [7, 15, 31]. The barriers and facilitators identified in this study were diverse and covered all the five domains of the CFIR. Although some studies have used other implementation research tools to identify the barriers and facilitators to implementing TB contact investigation, this study used the CFIR to explore the factors influencing TB contact investigation coverage in Africa.
The key challenges that emerged from this study included health system challenges, such as the lack of funding for TB contact investigation, insufficient PPE and inadequate Xpert MTB equipment for diagnostic testing. The rugged terrain and poor road networks in rural communities also made it difficult for health workers to access patients in the community, and vice versa. Poverty, TB- and COVID19-related stigma were also perceived as barriers. On the other hand, the facilitators to TB contact investigation included an increased awareness of TB contact investigation, adequate knowledge of the Ugandan MoH guidelines, confidence in delivering the intervention and on-the-job training of health workers. In addition, the availability of a telephone and transport to schedule and make household visits were reported as facilitators. The support of key district stakeholders involved in TB contact investigations and quarterly performance review meetings also emerged as facilitators.
Barriers
The health system barriers that emerged from this research were inadequate or irregular funding, human resource shortages, lack of PPE supplies (face masks, gloves, raincoats, and gumboots), out of stock of Xpert MTB cartridges and lack of airtime for communication. In addition, inadequate or inconsistent funding limited the frequency of the DTLS visits to health facilities for supervision and caused a delay in payment of travel and allowances to field teams, causing TB contact investigation operations to be hampered. This finding is in contrast with another study conducted in urban Kenya, which found that the TB program received sustainable funding for infrastructure and health workforce for contact investigation [32]. Furthermore, this Kenyan study used the WHO health systems framework. It focused on the stakeholder perspectives of the barriers and facilitators to optimizing TB contact investigation in Nairobi, the capital of Kenya. This funding disparity between rural and urban areas could be due to a higher TB prevalence in most urban settings thus attracting the attention of policy makers to allocate more resources there [33].
Consistent with this study, three studies conducted in Botswana, Ethiopia and Uganda reported human resource shortages as a considerable hindrance to TB contact investigation coverage [3, 15, 16]. In urban Uganda, health workers had other competing duties in the TB clinics, thus, they did not have sufficient time for community-level activities, including household contact tracing [15]. In this study, sometimes only one health worker was available for community visits, and they could not complete multiple tasks, such as health education, screening, sample collection, HIV testing and documentation in the registers. The staff shortage is partly attributed to a small number of staff trained in TB, and assigning them responsibilities in other units outside the TB unit [3].
Another challenge identified in this study was a lack of PPE materials such as masks, gloves, raincoats and gumboots for health workers to protect themselves against TB and other infectious diseases (such as COVID-19). Health staff were hesitant to conduct household contact investigations without wearing masks and gloves, to avoid contracting TB and COVID-19. Similarly, protective gear, such as raincoats and gumboots, to be used in harsh weather conditions, were not provided to health workers. There is limited literature on the influence of PPE materials on TB contact investigation coverage and this calls for more research in this area. These findings indicate that the supply chain management system for essential infection control materials is weak. These findings emphasize the need to strengthen mechanisms to guarantee sufficient PPE supplies and sustain the supply chain for these products.
The context within which an intervention is implemented, is recognized as a significant determinant of implementation success [18]. Contextual factors refer to issues about a person or their environment that can positively or negatively affect the delivery of an intervention [18]. Socio-economic, policy-related, and geographical barriers emerged as contextual barriers in this research. The socio-economic factors included poverty, lack of phones where patients can be contacted to confirm the appointment of household visits, stigma, and fear of reporting cough in fear of being labelled as having COVID-19.
In Botswana, Kenya, Ethiopia, and Uganda, the stigma associated with Tuberculosis has been reported as a barrier to TB contact investigation. [3, 7, 15, 16]. Although these studies did not specifically focus on TB contact investigation coverage, stigma hindered household visits, because index TB patients avoided home visits by health workers, out of fear of their status being disclosed to the community and discrimination from them, which could eventually affect demand and coverage of the intervention. An important observation in our study was that stigma was aggravated by the misconception that every TB patient has HIV, and the emergence of the COVID-19 pandemic. Tuberculosis and COVID-19 have common respiratory symptoms (cough, fever, and breathing difficulties), making it difficult to distinguish the two. This causes diagnostic confusion, and the health workers may also avoid such patients, in fear of contracting COVID-19 [34]. Furthermore, because of the new COVID-19 stigma, patients with a chronic cough might fear coming to the health facilities for diagnosis, thus complicating the two pandemics [34].
The COVID-19 lockdown policy implemented in 2020 by the Government of Uganda posed significant challenges to TB contact investigation efforts. Both health staff and patients could not access health facilities, due to stringent lockdown measures, including travel restrictions and public and private transportation prohibitions. Additionally, health providers could not conduct home visits to screen the contacts. Similar findings were found in another study on the impact of COVID-19 on TB programs in Western Pacific nations [35]. Other COVID-19 related problems encountered in the Western Pacific study included a change in priorities towards the COVID-19 response, as demonstrated by the relocation of TB program staff to the COVID-19 response, and a reduced willingness of patients and contacts to visit health facilities [35]. Therefore, innovative strategies are required to streamline TB contact investigation in the context of the COVID-19 pandemic.
As reported by Cattamanchi et al., geographical challenges contribute to the failure of TB patients and contacts to present at health facilities for TB care [36]. In their study, health workers reported that the physical remoteness of patients’ homes from the health facility and the rugged terrain encountered during travel, was a challenge [36]. Likewise, in this study, health workers reported that some index TB patients and contacts came from distant and challenging areas, with steep hills and poor road networks, preventing access to health facilities. This challenge was aggravated by poverty, because patients and contacts from the periphery of the county could not travel to health facilities because of high transport costs.
Facilitators
All health workers interviewed in this study reported awareness of the intervention. They had even engaged in relevant programs to improve its uptake, including enlisting household contacts, home visits, screening, and sputum sample collection. In addition, the clarification of the various steps demonstrated health workers’ adherence to the organizational protocols for TB contact investigations. The increased awareness and fidelity to the guidelines may be attributed to the development and dissemination of local contact investigation guidelines through training and the use of electronic media, such as WhatsApp. Conversely, a similar study conducted in rural Ethiopia found that awareness and adherence to the guidelines were poor because of a lack of refresher training. [3].
The health system facilitators that emerged from this study include good provider knowledge and access to information, performance review meetings at the district level, and engagement of district stakeholders to obtain their support. In contrast to other studies in Uganda, Ethiopia, and the USA, provider knowledge and confidence (self-efficacy) worked as a facilitator in this study because staff involved in TB contact investigation had received on-the-job training on various aspects of TB management, including contact investigation, diagnosis, and management [3, 15, 37]. In this study, health workers reported that they had the knowledge, skills, and confidence to conduct TB contact investigations successfully. These results are partly attributed to the quarterly district performance review meetings, in which an orientation on TB contact investigation was done and guidelines were shared with health workers.
Reflection and evaluation in TB contact investigation performance were demonstrated by Karamagi et al., in a Quality Improvement study to improve case finding in Northern Uganda [38]. A review meeting was held to discuss progress on active case finding and develop scale-up plans for the intervention [38]. Similarly, this study found that quarterly district review meetings were held, to discuss district and health facility performance, challenges, and improvement strategies in various program components, including TB contact investigation. These reflection meetings involved district-based stakeholders such as NGOs, health workers, TB focal persons, and health facility managers, and this promoted ownership of the interventions, and helped in resource mobilization. These meetings were also used to review quarterly TB performance, and develop action plans to improve multiple TB indicators, including TB contact investigation.
Strengths and limitations of the study
This study had the following strengths. First, we included various health provider categories at different levels of the district healthcare system, including community, health facility and district levels, to obtain different perspectives from the participants. Second, this study used implementation science methods such as the CFIR to investigate the rural perceptions of the challenges and enablers of TB contact investigation coverage. The CFIR provided a framework for developing the semi-structured interview guides and interpretation of study findings and this promotes transferability of these results to other settings.
Some weaknesses were also observed. First, index TB patients and their contacts were not interviewed; therefore, some information on the challenges and enablers of contact investigation coverage from the patients’ and caregivers’ perspective may have been missed. Second, data collection was conducted during the COVID-19 lockdown, and some health workers were inaccessible, especially laboratory personnel involved in pandemic control activities at the time. Consequently, the laboratory may have challenges that were not identified in this study. Third, the COVID-19 pandemic may have aggravated some challenges, which were not so pronounced before the pandemic. Finally, the generalizability of our results to other geographical locations may be limited, because this study was conducted in one district in Uganda, which gives it a smaller scope. However, we included three health facilities in different counties, which may improve transferability to other settings.
Conclusion
This study explored health providers perceptions of the barriers and facilitators of TB contact investigation in rural Mbarara district, Southwestern Uganda. This study found that most of the challenges limiting TB contact investigations in rural communities are related to health system; for-example inadequate or delayed funding and human resource shortages. The Ministry of Health in Uganda therefore must strengthen the health system building blocks, particularly health financing and human resources to establish a robust TB control program that will enable the efficient identification of missing TB patients. It also demonstrated the unique challenges affecting the rural settings regarding tuberculosis contact investigation including lack of personal protective equipment, stock-out of Xpert MTB cartridges, shortage of airtime for communication, TB-related stigma, and inconsistent funding for TB contact investigation. Further research is needed to determine the effectiveness of potential implementation strategies for eliminating these barriers in rural communities. Also, having identified the disruptive nature of the COVID-19 pandemic to the achievement of optimal TB contact investigation coverage, there is a need to develop measures for integrating both COVID-19 and TB contact investigation interventions.
Data availability
The dataset used in the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Global Tuberculosis Report 2023. 2023. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023
World Health Organization. Global Tuberculosis Report. 2019. https://www.who.int/tb/global-report-2019
Tesfaye L, Lemu YK, Tareke KG, Chaka M, Feyissa GT. Exploration of barriers and facilitators to household contact tracing of index tuberculosis cases in Anlemo District, Hadiya Zone, Southern Ethiopia: qualitative study. PLoS ONE. 2020;15(5):e0233358.
Zumla A, Petersen E, Nyirenda T, Chakaya J. Tackling the tuberculosis epidemic in sub-saharan Africa–unique opportunities arising from the second European developing countries clinical trials Partnership (EDCTP) programme 2015–2024. Int J Infect Dis. 2015;32:46–9.
United Nations Program on HIV and, Tuberculosis AIDS. and HIV. 2020. https://www.unaids.org/sites/default/files/media_asset/tb-and-hiv_en.pdf
World Health Organization. Recommendations for investigating contacts of persons with infectious tuberculosis in low- and middle-income countries. 2012. https://www.who.int/tb/publications/2012/contact_investigation2012/en/
Marangu DM. Optimizing tuberculosis contact investigation and linkage to care in Nairobi. Kenya: TB KWISHA. University of Nairobi; 2018.
Uganda Ministry of Health. Tuberculosis contact investigation in Uganda, operational guide 2019. In. Kampala, Uganda: Ministry of Health; 2019.
Uganda Ministry of Health. Manual for management and control of tuberculosis and leprosy in Uganda. 2017. https://health.go.ug/sites/default/files/NTLP%20Manual%203rd%20edition_17th%20Aug_final.pdf
Blok L, Sahu S, Creswell J, Alba S, Stevens R, Bakker MI. Comparative meta-analysis of tuberculosis contact investigation interventions in eleven high burden countries. PLoS ONE. 2015;10(3):e0119822.
Armstrong-Hough M, Turimumahoro P, Meyer AJ, Ochom E, Babirye D, Ayakaka I, Mark D, Ggita J, Cattamanchi A, Dowdy D, et al. Drop-out from the tuberculosis contact investigation cascade in a routine public health setting in urban Uganda: a prospective, multi-center study. PLoS ONE. 2017;12(11):e0187145.
Centres for Disease Control and Prevention. Finding the missing cases: The role of enhanced diagnostics and case-finding in reaching all people with TB (fact sheet). 2020. https://www.cdc.gov/globalhivtb/who-we-are/resources/keyareafactsheets/finding-the-missing-4-million.pdf
United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. https://www.unfpa.org/resources/transforming-our-world-2030-agenda-sustainable-development
Theobald S, Brandes N, Gyampong M, El-Saharty M, Proctor E, Diaz T, Wanji S, Elloker S, Raven J, Elsey H, et al. Implementation research: new imperatives and opportunities in global health. Lancet. 2018;392(10160):2214–28.
Ayakaka I, Ackerman S, Ggita JM, Kajubi P, Dowdy D, Haberer JE, Fair E, Hopewell P, Handley MA, Cattamanchi A, et al. Identifying barriers to and facilitators of tuberculosis contact investigation in Kampala, Uganda: a behavioral approach. Implement Sci. 2017;12(1):33.
Tlale L, Frasso R, Kgosiesele O, Selemogo M, Mothei Q, Habte D, Steenhoff A. Factors influencing health care workers’ implementation of tuberculosis contact tracing in Kweneng, Botswana. Pan Afr Med J. 2016;24:229.
Uganda Ministry of Health. The Uganda National Tuberculosis Prevalence Survey, 2014–2015 Survey Report. 2016. https://health.go.ug/sites/default/files/Uganda%20National%20TB%20Prevalence%20Survey%202014-2015_final%2023rd%20Aug17.pdf
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
Adamu AA, Uthman AO, Gadanya MA, Wiysonge CS. Using the consolidated framework for implementation research (CFIR) to assess the implementation context of a quality improvement program to reduce missed opportunities for vaccination in Kano, Nigeria: a mixed methods study. Hum Vaccin Immunother. 2019;16(2):465–75.
Gyamfi J, Allegrante JP, Iwelunmor J, Williams O, Plange-Rhule J, Blackstone S, Ntim M, Apusiga K, Peprah E, Ogedegbe G. Application of the Consolidated Framework for Implementation Research to examine nurses’ perception of the task shifting strategy for hypertension control trial in Ghana. BMC Health Serv Res. 2020;20(1):65.
Warner G, Lawson B, Sampalli T, Burge F, Gibson R, Wood S. Applying the consolidated framework for implementation research to identify barriers affecting implementation of an online frailty tool into primary health care: a qualitative study. BMC Health Serv Res. 2018;18(1):395.
Muddu M, Tusubira AK, Nakirya B, Nalwoga R, Semitala FC, Akiteng AR, Schwartz JI, Ssinabulya I. Exploring barriers and facilitators to integrated hypertension-HIV management in Ugandan HIV clinics using the Consolidated Framework for Implementation Research (CFIR). Implement Sci Commun. 2020;1:45.
Uganda Bureau of Statistics. Mbarara District Local Government statistical abstract 2016/17. 2017. https://www.mbarara.go.ug/sites/default/files/downloads/Statistical%20Abstract%202017%20Final.pdf
Uganda Ministry of Health. National Health Facility Master List; a complete list of all health facilities in Uganda. 2018.
Turyamureba M, Bruno LY, Oryema JB. Health Care Delivery System in Uganda: a review. Tanzan J Health Res 2023, 24(2).
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Rowlands J. Interviewee Transcript Review as a Tool to Improve Data Quality and participant confidence in Sensitive Research. Int J Qual Methods. 2021;20:16094069211066170.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
O’Connor C, Joffe H. Intercoder Reliability in Qualitative Research: debates and practical guidelines. Int J Qual Methods. 2020;19:1–13.
Davis JL, Turimumahoro P, Meyer AJ, Ayakaka I, Ochom E, Ggita J, Mark D, Babirye D, Okello DA, Mugabe F et al. Home-based Tuberculosis contact investigation in Uganda: a household randomised trial. ERJ Open Res 2019, 5(3).
Marangu D, Mwaniki H, Nduku S, Maleche-Obimbo E, Jaoko W, Babigumira J, John-Stewart G, Rao D. Stakeholder perspectives for optimization of tuberculosis contact investigation in a high-burden setting. PLoS ONE. 2017;12(9):e0183749.
Mutembo S, Mutanga JN, Musokotwane K, Kanene C, Dobbin K, Yao X, Li C, Marconi VC, Whalen CC. Urban-rural disparities in treatment outcomes among recurrent TB cases in Southern Province, Zambia. BMC Infect Dis. 2019;19(1087):1–8.
Togun T, Kampmann B, Stoker NG, Lipman M. Anticipating the impact of the COVID-19 pandemic on TB patients and TB control programmes. Ann Clin Microbiol Antimicrob. 2020;19(1):21.
Chiang CY, Islam T, Xu C. The impact of COVID-19 and the restoration of tuberculosis services in the Western Pacific Region. Eur Respir J. 2020;56:2003054.
Cattamanchi A, Miller CR, Tapley A, Haguma P, Ochom E, Ackerman S, Davis JL, Katamba A, Handley MA. Health worker perspectives on barriers to delivery of routine tuberculosis diagnostic evaluation services in Uganda: a qualitative study to guide clinic-based interventions. BMC Health Serv Res. 2015;15:10.
Wilce M, Shrestha-Kuwahara R, Taylor Z, Qualls N, Marks S. Tuberculosis Contact Investigation policies, practices, and challenges in 11 U.S. communites. J Public Health Manag Pract. 2017;8(6):69–78.
Karamagi E, Sensalire S, Muhire M, Kisamba H, Byabagambi J, Rahimzai M, Mugabe F, George U, Calnan J, Seyoum D, et al. Improving TB case notification in northern Uganda: evidence of a quality improvement-guided active case finding intervention. BMC Health Serv Res. 2018;18(1):954.
Acknowledgements
I acknowledge the contribution of Grace Ayebazibwe (GA), who supported me during the data collection and analysis by taking field notes, transcription, and translation of audio recordings.
Funding
This research work was supported by TDR, the Special Program for Research and Training in Tropical Diseases, which is hosted at the World Health Organization, and co-sponsored by UNICEF, UNDP, the World Bank and WHO. TDR grant number: B40299, first author ORCID ID: 0000-0001-9722-1202. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funder.
Author information
Authors and Affiliations
Contributions
PT, NN and PM participated in the conceptualization and design of the study, developing interview guides, writing the initial version of the manuscript, and reviewing subsequent versions, with substantial input from NMT. With assistance from NN and PM, PT and JN conducted the data analysis. Each author contributed to the writing of the manuscript, and they all reviewed and gave their approval for publishing of the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was cleared by the Human Research Ethics Committees at the University of the Witwatersrand Medical (M200101), and the Research Ethics Committee at Mbarara University of Science and Technology (MUREC 1/7). Permission to conduct the study was obtained from the Uganda National Council of Science and Technology (HS569ES). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tukamuhebwa, P.M., Munyewende, P., Tumwesigye, N.M. et al. Health worker perspectives on barriers and facilitators of tuberculosis investigation coverage among index case contacts in rural Southwestern Uganda: a qualitative study. BMC Infect Dis 24, 867 (2024). https://doi.org/10.1186/s12879-024-09798-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09798-9