Abstract
Background
Measles remains a major public health burden worldwide. Parents often hesitate to vaccinate children with chronic diseases. We investigated the association between the percentage of vaccination and chronic diseases and explore hospital infections’ role in the 2017–2019 measles outbreak across northern Vietnam provinces.
Methods
A total of 2,064 children aged 0–15 years old admitted for measles to the National Children’s Hospital during the outbreak were included in the study. Demographic information, clinical characteristics, vaccination statuses and laboratory examination were extracted from electronic medical records, vaccination records, or interviews with parents when other sources were unavailable.
Results
The incidence rate that provincial hospitals sent to the National Children’s Hospital was proportional to the population density of their provinces of residence. Early nosocomial transmission of measles was observed before community-acquired cases emerged in many provinces. Among patients aged over 18 months, those with chronic diseases had a proportion of vaccination of 9.4%, lower than patients without chronic diseases at 32.4%. Unvaccinated patients had a higher proportion of hospital-acquired infections with aOR = 2.42 (1.65–3.65), p < 0.001 relative to vaccinated patients. The proportion of hospital-acquired infections was higher among children with chronic diseases compared to those without, with aOR = 3.81 (2.90–5.02), p < 0.001.
Conclusion
Measles spread in healthcare settings prior to community cases that occurred in several provinces. We recommend enhancing hospital infection control by increasing staff training and improving early detection and isolation during non-outbreak periods. Measles patients with chronic diseases exhibited lower proportions of vaccination and faced a higher risk of hospital-acquired infections. It is crucial to establish comprehensive vaccination guidelines and enhance parental awareness regarding the significance and safety of measles vaccination to protect these vulnerable individuals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Measles is a highly contagious acute viral infection that can lead to severe morbidity and mortality in children [1]. Despite the availability of effective vaccines, measles continues to be a significant cause of illness and mortality globally, resulting in approximately 100,000 deaths annually [1]. In 2011, the Global Measles and Rubella Strategic Plan was established by the World Health Organization aimed to achieve measles elimination in five out of six World Health Organization regions by the end of 2020. However, no region has been able to achieve or maintain elimination as outlined in the plan [2].
Eliminating measles remains a crucial goal for every country worldwide [3], which requires a combination of multiple measures simultaneously including epidemic control, effective surveillance, and immunization [4]. Measles vaccination has been estimated to have prevented approximately 31.7 million deaths worldwide between 2000 and 2020 [2]. The World Health Organization advises a vaccination coverage of 90–95% is crucial in attaining herd immunity. Despite many efforts in the vaccination programs, measles outbreaks continue to occur at intervals of 2 to 5 years in endemic areas [5]. Countries that previously declared the elimination of measles still experience intermittent outbreaks. For example, although reporting a national vaccination coverage of 94.7%, the United States experienced a resurgence of measles outbreak with a total of 1,282 cases across 31 states and 94 counties in 2019 [1, 6]. Between 2017 and 2019, measles cases hit historic peaks in many European countries, including France, Georgia, Greece, Italy, Romania, Serbia and Ukraine [7]. Pockets of under-immunized communities within populations are often what pose a large risk for outbreaks. Specifically, despite vaccine coverage of approximately 90–95% in the United States, there still could be pockets of very low vaccine coverage. In 2022, both the United States Centers for Disease Control and Prevention and World Health Organization have declared measles to be an “imminent threat” worldwide. This alarming status is attributed to declining vaccination rates and weakened surveillance during the COVID-19 pandemic [8].
Vietnam is a lower middle-income country which implements the WHO’s Expanded Program on Immunization. The country added measles-containing vaccines to its routine vaccination schedule in 1982 [9], with the recommendation being to administer a first dose at 9 months of age and a second dose at 18 months of age [10]. Studies have shown that measles vaccine coverage rates in Vietnam are significantly influenced by social factors. These factors include doubts about vaccine safety, lack of trust in public vaccination centers, and concerns about side effects, all contribute to lower participation in child immunization programs among specific groups [11]. Children from ethnic minority groups, lower-educated mothers, and from the poorest households were less likely to receive the measles vaccine. However, a notable proportion of highly educated, wealthy mothers also chose not to vaccinate their children against measles [11]. Major outbreaks continue to occur every 4–5 years, such as outbreaks in 2009, 2013–2014 and 2017–2019. The 2014 outbreak in northern Vietnam recorded 9,577 confirmed cases of measles, with an incidence rate of 116.4 per 1,000,000 population during the outbreak [12]. Many hospitalized children with measles were under 12 months old and not fully vaccinated. Among older children admitted with measles, a large proportion had no vaccination history [13]. Moreover, during extensive community outbreaks, tertiary care hospitals become overwhelmed with a large influx of patients. The overcrowding and compromised infection control measures within the hospital setting pose a clear and significant risk of in-hospital transmission [14]. Nosocomial infections can further exacerbate the scale of epidemics and may lead to an increase in both morbidity and mortality rates.
The period from 2017 to 2019 witnessed a significant rise in measles cases in Vietnam. The National Children’s Hospital in Ha Noi is the largest pediatric tertiary referral hospital that received patients from all northern provinces, particularly moderate to severe cases and individuals with congenital or comorbid conditions referred from provincial hospitals. Given the substantial number of cases during the outbreak, the National Children’s Hospital faced multiple challenges in terms of providing clinical services while maintaining infection control prevention activities. In this study, we conducted an analysis of the epidemiological and clinical characteristics of all measles patients admitted to the National Children’s Hospital during the 2017–2019 outbreak. Our objectives were to explore the spatial and temporal transmission pattern, the association between lack of vaccination and the presence of chronic diseases, as well as to assess the potential role of hospital-acquired infections in measles outbreak spread among northern provinces in Vietnam.
Methods
Data collection
We conducted a retrospective study at the National Children’s Hospital in Ha Noi, Vietnam. All patients diagnosed with measles admitted to the Infectious Disease Department and Intensive Care Unit during the 2017–2019 outbreak were included in the study. Demographic information (age, sex, and commune of residence), clinical characteristics (date of onset, date of hospitalization, pneumonia condition, chronic diseases), interventions (oxygen therapy, high-flow oxygen, mechanical ventilation, dialysis, extracorporeal membrane oxygenation support), laboratory examination (IgM, PCR) were extracted from electronic medical records. Data regarding vaccination status were collected from the child’s vaccination record on paper form or electronic medical record (for approximately 90% of cases), or interviewing parents if the other sources are not available. The study health record form is included as Supplementary 1.
During the outbreak, a variety of infection control measures were implemented at the National Children’s Hospital. All staff members and visiting students were required to be vaccinated against measles. A separate unit was established at the Center of Clinical Medicine for Tropical Diseases in Children to treat measles patients, and an isolated room was set up for measles patients in the intensive care unit. In each chronic disease department (cardiovascular, neurology), separate rooms were designated to isolate suspected cases or treat confirmed measles cases. For patients with severe chronic diseases, separate treatment rooms were arranged in the respective chronic disease departments. Family visits were prohibited, and separate care items and staff were designated. Special requirements for personal protective equipment such as N95 masks and protective clothing were enforced in line with international recommendations for measles. Throughout the epidemic, no cases of measles were detected among the hospital staff.
Definitions
Measles cases were defined as in-patients under 16 years old who exhibited fever, rash, and were confirmed to have measles through positive results from either IgM or PCR tests. The date of onset was determined as the first day the patient presented with rash symptoms.
The patient’s vaccination status was categorized as “unvaccinated” if they have not received any vaccine doses, or as “vaccinated” if they had received at least one dose.
Patients were classified as hospital-acquired infections if they met one of the following conditions:
-
Patients treated at the hospital and experiencing symptom onset at least 22 days after admission;
-
Patients who stayed in the hospital for a minimum of 14 days and developed symptoms within 7 days after discharge;
-
Patients admitted to the hospital between 8 and 21 days before symptom onset;
-
Patients who were hospitalized and experienced symptom onset within 21 days after discharge.
Severe patients were defined as individuals diagnosed with measles who were presented with pneumonia or bronchitis and required supplemental oxygen therapy. The severity of the condition was categorized into two levels:
-
Severity level 1: Patients who required either oxygen therapy or continuous positive airway pressure to manage their respiratory distress.
-
Severity level 2: Patients exhibited a more critical condition and received advanced interventions such as high-flow oxygen, mechanical ventilation, dialysis, or extracorporeal membrane oxygenation support.
Chronic diseases were defined as any chronic diseases identified from the electronic medical record of patients. Chronic diseases were classified into:
-
Chronic infection: chronic hepatitis B infection, hepatitis C infection, HIV infection, congenital syphilis.
-
Cancer: acute lymphoblastic leukemia, neuroblastoma, nephroblastoma, Burkitt lymphoma, osteosarcoma and other cancer diseases.
-
Metabolic disorders: beta-ketothiolase deficiency, citrin deficiency, glycogen storage disease, glutaric acidemia type II, isovaleric acidemia, cow milk protein allergy, and other metabolic disorders.
-
Cardiovascular system: transposition of great arteries, patent ductus arteriosus, aortic coarctation, ventricular septal defect, tetralogy of Fallot, total anomalous pulmonary venous return and other congenital heart diseases.
-
Gastrointestinal system: Crohn’s disease, biliary atresia, Hirschsprung’s disease, autoimmune hepatitis, cirrhosis, anorectal malformation, megacolon and other congenital gastrointestinal diseases.
-
Neurological system: cerebral palsy, mental retardation, epilepsy, ventriculomegaly, craniosynostosis, hydrocephalus and other chronic diseases of the neurological system.
-
Autoimmune and immunodeficiency: systemic lupus erythematosus, aplastic anemia, common variable immunodeficiency, Wiskott-Aldrich syndrome and other autoimmune and immunodeficiency diseases.
-
Kidney and urology system: congenital nephrotic syndrome, kidney failure, polycystic kidney disease, Bartter syndrome, and other congenital kidney diseases.
-
Other chronic diseases: such as thalassemia, eczema, undescended testicle, craniosynostosis, Erb’s palsy….
Ethics statement
The study was approved by the Institutional Review Board of the Vietnam National Children’s Hospital, which waived the requirement for consent to participate because the analysis was retrospective (Approval reference number: 473/BVNTW-HDDD, IRB identifier:
IRB-VN01037/IRB00011976/FWA00028418).
Statistical analysis
Categorical data are described using frequency and percentage. The relationships between hospital-acquired infection, vaccination status and presence of chronic diseases were assessed using Chi-square test. We fitted a cubic polynomial to demonstrate how vaccination percentages vary across different age groups. We computed Pearson correlation coefficient to examine the correlation between the incidence rate and population density across all provinces. Multivariable logistic regression was performed on vaccination status, the presence of chronic diseases and age to estimate adjusted odds ratios (OR). All statistical analyses were performed using R Statistical Software (v4.3.2; R Core Team 2021).
Results
Measles outbreak in children
From July 2017 to December 2019, a total of 2,064 children admitted to the hospital were confirmed with measles. Demographic and clinical characteristics of patients were described in Table 1. The first case was a 2-year-old child who was community-acquired infected. The age distribution of children was stable during the outbreak, with approximately half of the children under the age of 9 months (Fig. 1A). The temporal distribution of cases reached a peak in May 2019 for all age groups, except the age group of over 2-years-old which reached its peak sooner, in around March 2019 (Fig. 1B).
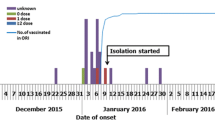
Vaccination status of measles children. (A) The percentage of vaccination among all patients in the National Children’s Hospital as a function of time of onset. (B) Mean vaccination proportion of decile age groups (dots) with 95% CI plotted together with a cubic logistic regression. (C) The percentage of vaccination as a function of time in different age groups. (D) Vaccination proportion of different age groups categorised by chronic disease status
During the outbreak, the percentage of patients with severity levels 1 and 2 were 33.4% and 7.7%, respectively. An increasing trend in the percentage of severe patients was observed since December 2017, then remained relatively constant until the end of 2019 (Fig. 2A). The peaks of the temporal distribution of the cases in most provinces were in May 2019, regardless of the source of infection. The peak of patients infected in the community and provincial hospital in Nghe An was reached earlier than the rest, around November 2018 (Fig. 2C). Indeed, measles cases from Nghe An were the highest in November 2018 and decreased in subsequent months (Fig. 4B, C). Early nosocomial transmission of measles was observed before community-acquired cases emerged in provinces including Hung Yen, Ha Nam, Nam Dinh, and Hai Phong. Among measles patients admitted to the National Children’s Hospital. The percentage of hospital-acquired infection was higher among unvaccinated patients than vaccinated patients with aOR = 2.42 (1.65–3.65), p < 0.001. The proportion of hospital-acquired infection among measles patients who have chronic diseases was higher than patients without chronic diseases with aOR = 3.81 (2.90–5.02), p < 0.001 (Table 2).
Vaccination status and measles infections among children with chronic diseases
During the first few months of the outbreak, all measles patients were unvaccinated. Beginning from October 2017, some vaccinated children got infected. The percentage of patients who were vaccinated was < 30% of the hospitalized cases during the outbreak period (Fig. 3A). The percentage of vaccinated children among the measles patients increases with age until 22 months where it reaches a plateau of about 27% (Fig. 3B). All patients under 6 months were unvaccinated, while a fraction of patients at 6–9-month-old (1.8%), 9-18-month-old (10.1%) and over 18-month-old (27.7%) were vaccinated (Fig. 3C). Lower proportion of vaccination (5.6%) were found in patients with chronic diseases as compared to those without chronic diseases (10.8%). Among patients aged 9 to 18 months, only 8.1% of patients with chronic diseases received vaccination, whereas 10.4% of patients without chronic diseases were vaccinated. Similarly, among patients over 18 months old, the proportion of vaccination was 9.4% for those with chronic diseases, much lower than the proportion of vaccination of 32.3% observed in patients without chronic diseases (Fig. 3D).
Incidence rate and population density
The incidence rates of measles patients from provinces across the north sending to the National Children’s Hospital in each year were shown in Fig. 4A. The incidence rate of provincial hospitals sent to the National Children’s Hospital were proportional to the population density of corresponding provinces with a correlation coefficient of 0.76 (p < 0.001) (Fig. 4B). Beginning from August 2017, there were 2 clusters (Ha Noi and Nghe An) spreading the disease to nearby provinces. When the epidemic curve flattened at the end of 2017, almost no cases were sent from provinces other than Ha Noi and Nghe An (Fig. 4C). At the end of 2018, almost all provinces in northern Vietnam sent measles patients to the National Children’s Hospital (Fig. 4C). In the second half of 2019, fewer children from nearby provinces were admitted to the hospital, and the outbreak subsided by September 2019, with only sporadic cases primarily originating from Ha Noi and Nghe An (Fig. 4C).
Disscussion
Despite achieving high measles vaccination coverage of over 95% for children who received the first dose consistently since 2004, Vietnam continues to experience endemic measles outbreaks. The country has encountered several significant outbreaks, including those in 2006, 2009, 2014, and the most recent one spanning from 2017 to 2019. The National Children’s Hospital is the largest pediatric tertiary referral hospital responsible for treating almost all moderate to severe cases in northern Vietnam. This study analyzes all measles cases admitted to National Children’s Hospital throughout the duration of the most recent national-scale measles outbreak.
During the outbreak, approximately half of the children hospitalized for measles at the National Children’s Hospital were under 9 months old, and this percentage remained consistent throughout the outbreak. This pattern aligns with studies that reported measles outbreaks in Southern China from 2009 to 2016 [15] and the United States in 2018–2019 [16]. The reason behind this trend may be attributed to the immunization system’s design, which considers these infants too young to receive routine immunization. In Vietnam, the recommended schedule for measles vaccination involves administering a first dose at 9 months old and a second dose at 18 months old. Maternal immunity against measles diminishes rapidly, with levels generally falling below the protective threshold by 3 months of age [17], and infants aged 0 to 8 months have been identified as a high transmissibility group in previous studies [15]. However, lowering the minimum age for the first measles vaccination to 6 months remains a topic of controversy. Studies have shown that receiving measles vaccination before 9 months of age may result in lower antibody titers and reduced vaccine effectiveness [18]. In addition, among children aged over 2 years, who generally receive two doses of the measles vaccine, there was an earlier peak in measles cases compared to all other age groups. Given the higher vaccination coverage in this older age cohort, the proportion of susceptible individuals is lower than in other groups, potentially leading to an earlier end to the outbreak compared to younger children. First-dose measles-containing vaccine coverage globally has remained at 84–85% for over a decade [19], which reflected in our study’s early low vaccination rates. In Hanoi, parents often choose to wait until 12 months for the measles-rubella vaccine at private vaccination centers, rather than the 9-month monovalent measles vaccine in the Expanded Program on Immunization, contributing to a larger vaccination gap [20]. Amidst the 2018 outbreak, the Ministry of Health of Vietnam launched a measles-rubella vaccination campaign for 4.2 million children aged 1 to 5 years in high-risk areas across 57 cities and provinces [21], which likely contributed to the observed increase in vaccination rates.
In contrast to the 2014 outbreak which only lasted for 1 year, the 2017–2019 outbreak lasted for 3 years and had caused hospital overloading which led to a mortality rate of 10% among hospitalized patients, while the typical mortality rate of measles hospitalizations is reported as 2–3% [22, 23]. We found that once the national pediatric hospital started to receive a lot of patients from Ha Noi and Nghe An, which means the outbreaks have occurred in these two provinces, it quickly spread to neighboring areas. The outbreak also came to an end when cases sent from these two provinces decreased. Ha Noi and Nghe An are the two provinces with the highest population sizes in northern Vietnam. Provinces with higher population densities tend to have higher incidence rates of cases sent to the National Children’s Hospital. Densely populated provinces may have higher transmission rates of infectious diseases, leading to higher incidence rates. The healthcare systems in these provinces typically serve larger patient numbers and are more prone to overload, necessitating the transfer of cases to the National Children’s Hospital. During outbreaks, policymakers should consider population density when designing and implementing public health policies to ensure that higher-risk regions are prioritized and adequately supported. Being the capital, Ha Noi is also characterized by a very high volume of human mobility [24]. A research using data of the 2017–2019 outbreak in southern Vietnam also suggested that human mobility is one of the most important factors contributing to inter-provincial transmission [25]. In March 2019, the outbreak seemed to have reached its peak and have spread to almost all provinces in the north, as the national pediatric hospital received patients from 22 out of 29 provinces of northern Vietnam. A hypothesis has been stated that measles outbreak could be triggered by large volume of inter-provincial travel and person-to-person transmission during the Lunar New Year [25, 26], which usually happens in January or February in Vietnam. Concerns about rapid expansion after holidays has also been raised in the previous measles outbreak in Vietnam in 2009 and 2014 [12]. In 2014, nationwide measles vaccination campaigns for children were triggered that led to the control of the outbreak [12]. Similar vaccination campaigns were organized in 2019 when the outbreak was at its peak. Given that increased human mobility during holidays can potentially contribute to a surge in measles cases, future control strategies, like vaccination campaigns, would be more effective if planned before holidays. These strategies should focus on assessing population-level susceptibility rather than waiting until an outbreak has already occurred.
Research in Vietnam has found that children from ethnic minority groups, lower-educated mothers, and the poorest households are less likely to receive the measles vaccine due to limited access to healthcare, lack of awareness, and financial constraints [11]. Conversely, in economically developed areas like Ha Noi, highly educated and wealthy mothers avoid vaccinating their children due to concerns about vaccine safety and side effects [11]. This variation in vaccination coverage is strongly linked to measles incidence [25], particularly affecting children with chronic diseases whose parents are often more cautious about vaccination. Additionally, socio-economic disparities impact the risk of hospital-acquired infections, as underprivileged populations have less access to quality healthcare and face delays in treatment, increasing their vulnerability.
Our research findings indicate that some provinces experienced infection starting from a suspected or confirmed case from the National Children’s Hospital or within provincial hospitals before the emergence of community-acquired hospitalizations. The transmission of measles within healthcare facilities can amplify the propagation of outbreaks that originate from community-acquired cases and subsequent hospitalizations, potentially resulting in longer outbreak periods during 2017 to 2019 compared to previous occurrences. And vice versa: the outbreak lasting for such a long period of time may also exacerbate nosocomial infection since resource constraints, such as lack of space and inadequate ventilation, make isolating measles patients very challenging, thus contributing to the spread within healthcare settings [14]. Controlling nosocomial infections remains challenging. Healthcare facilities are usually full of in-patients with compromised immune systems and lower vaccination rates due to chronic and congenital illnesses. Measles patients sometimes present with initial respiratory symptoms or fever alone without the classic accompanying symptoms of cough, coryza, and rash. In our study, only 40.9% of patients were diagnosed with measles upon admission, making early diagnosis and tracking difficult before admission. Many prevention measures are known such as performing serological test for all patients with atypical clinical manifestation, strengthening infection control measures in healthcare facilities, and early isolation of suspected cases [27]. However, integrating these measures in the context of low and middle-income countries like Vietnam presents significant challenges. From our experience at the National Children’s Hospital, we have managed to maintain a nosocomial infection rate of 5%, but complete eradication of these cases remains unattainable as long as measles persists within the community and necessitates hospitalization for treatment.
Children with underlying chronic diseases or comorbid conditions face a dilemma regarding vaccination. Concerns regarding potential side effects and the fragility of their health often lead parents to hesitate in vaccinating their children. However, the consequence of remaining unvaccinated is an elevated risk of contracting and progressing to severe diseases [28]. Our study found that children with chronic diseases have a higher risk of nosocomial infection. Children with chronic diseases are reported to exhibit reduced immune responses and more rapid waning antibody titers [29]. They usually visit the hospital more often, and spend more time in the hospital, which also explains the higher risk of contracting hospital-acquired infections. In Vietnam, vaccination centers frequently decline to administer vaccines to these children due to concerns related to post-vaccination complications, parents complains and a lack of detailed guidelines for vaccination for these subjects. Until now, the National Children’s Hospital is the only facility in northern Vietnam capable of vaccinating children with chronic diseases. Our findings highlight the need for enhanced protection and specialized guidelines for this vulnerable population to prevent future outbreaks. Future studies should investigate the attitudes of parents of children with chronic diseases towards measles vaccination, conducting long-term follow-up on patients with chronic diseases who contracted measles to understand the lasting impacts on their health and quality of life, and evaluate the vaccine effectiveness in this group to help inform better decisions about the benefits and risks for these vulnerable children.
Limitation
A major limitation of our study is that our data only comes from one hospital. In absence of community-wide data, we were unable to make an inference about the probability of infection, and it is very difficult to see the trend of overall measles outbreak during the study period. In addition, the reported severity proportion in our study is expected to be greater than that in smaller hospitals, primarily because the National Children’s Hospital serves as the region’s last-resort facility for pediatric care, receiving a higher number of moderate to severe cases. Risk factors for severe morbidity such as nutrition, lactation status, laboratory tests or vitamin A dose were not available to be analyzed in this study. Our study categorizes children as “unvaccinated” if they received no vaccine doses, or “vaccinated” if they received at least one dose, but our data lacks detailed information on the number of doses. This limitation may affect findings, as vaccine effectiveness can be lower among partially vaccinated children. Additionally, the source of data regarding the type of vaccination report was unavailable. While approximately 90% of vaccination status information was collected from vaccination records or electronic medical records, we were unable to investigate the association between the reliability of vaccination report sources and measles cases among vaccinated children.
Conclusion
In conclusion, our study highlights the early transmission of measles within healthcare settings before community-acquired cases emerged in many provinces in the 2017–2019 outbreak. Beyond existing non-pharmaceutical interventions in hospital settings, we propose strengthening these efforts during non-outbreak periods through regular staff training on infection control, improving early detection and isolation of suspected cases, and conducting periodic audits of infection control practices. Measles cases with chronic diseases appeared to have lower proportion of vaccination, with the most pronounced disparity observed among children aged 18 months and older. Comprehensive vaccination guidelines and increased parental awareness regarding the importance and safety of vaccination are vital for protecting high-risk individuals in the future.
Data availability
Data available on request from the corresponding author due to institutional privacy restrictions.
References
Paules CI, Marston HD, Fauci AS. Measles in 2019 — going backward. N Engl J Med. 2019;380:2185–7.
Dixon MG, Ferrari M, Antoni S, Li X, Portnoy A, Lambert B, et al. Progress toward Regional Measles Elimination — Worldwide, 2000–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1563–9.
Moss WJ, Griffin DE. Global measles elimination. Nat Rev Microbiol. 2006;4:900–8.
Evolution of Measles Elimination Strategies in the United States. J Infect Dis. 2004;189 Supplement1:S17–22.
Berche P. History of measles. La Presse Médicale. 2022;51:104149.
Gardner L, Dong E, Khan K, Sarkar S. Persistence of US measles risk due to vaccine hesitancy and outbreaks abroad. Lancet Infect Dis. 2020;20:1114–5.
Leong WY. Measles cases hit record high in Europe in 2018. J Travel Med. 2018;25:tay080.
Iacobucci G. Measles is now an imminent threat globally, WHO and CDC warn. BMJ. 2022;379:o2844.
Sniadack DH, Mendoza-Aldana J, Thanh Huyen DT, Thanh Van TT, Van Cuong N, Olive JM, et al. Epidemiology of a Measles Epidemic in Vietnam 2008–2010. J Infect Dis. 2011;204 suppl1:S476–82.
Cuong HQ, Nguyen HX, Van Hau P, Ha NLK, Lan PT, Mounts A, et al. Gap in measles vaccination coverage among children aged 9 months to 10 years in Ho Chi Minh City, Viet Nam, 2014. Western Pac Surveill Response J. 2019;10:39–45.
Kien VD, Van Minh H, Giang KB, Mai VQ, Tuan NT, Quam MB. Trends in childhood measles vaccination highlight socioeconomic inequalities in Vietnam. Int J Public Health. 2017;62:41–9.
Do LP, Van TTT, Nguyen DTM, Van Khang P, Pham QT, Tran MT, et al. Epidemiological and molecular characteristics of a measles outbreak in northern Vietnam, 2013–2014. J Clin Virol. 2021;139:104840.
Choisy M, Trinh ST, Nguyen TND, Nguyen TH, Mai QL, Pham QT, et al. Sero-prevalence surveillance to Predict Vaccine-Preventable Disease outbreaks; a lesson from the 2014 Measles Epidemic in Northern Vietnam. Open Forum Infect Dis. 2019;6:ofz030.
Shakoor S, Mir F, Zaidi AKM, Zafar A. Hospital preparedness in community measles outbreaks—challenges and recommendations for low-resource settings. Emerg Health Threats J. 2015;8. https://doi.org/10.3402/ehtj.v8.24173.
Chong KC, Hu P, Lau S, Jia KM, Liang W, Wang MH, et al. Monitoring the age-specificity of measles transmissions during 2009–2016 in Southern China. PLoS ONE. 2018;13:e0205339.
Yang W. Transmission dynamics of and insights from the 2018–2019 measles outbreak in New York City: a modeling study. Sci Adv. 2020;6:eaaz4037.
Wang Q, Wang W, Winter AK, Zhan Z, Ajelli M, Trentini F, et al. Long-term measles antibody profiles following different vaccine schedules in China, a longitudinal study. Nat Commun. 2023;14:1746.
Lochlainn LMN, Gier B, van der de, Maas N, Strebel PM, Goodman T, van Binnendijk RS, et al. Immunogenicity, effectiveness, and safety of measles vaccination in infants younger than 9 months: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19:1235–45.
Worldwide measles deaths climb 50%. from 2016 to 2019 claiming over 207 500 lives in 2019. https://www.who.int/news/item/12-11-2020-worldwide-measles-deaths-climb-50-from-2016-to-2019-claiming-over-207-500-lives-in-2019. Accessed 14 Aug 2024.
Dang TTH, Carnahan E, Nguyen L, Mvundura M, Dao S, Duong TH, et al. Outcomes and costs of the transition from a paper-based immunization system to a Digital Immunization System in Vietnam: mixed methods study. J Med Internet Res. 2024;26:e45070.
Ministry of Health of Vietnam. Decree no. 137/QD-BYT regarding the planning for preventionand control of infectious diseases in 2020. 2024. https://thuvienphapluat.vn/van-ban/The-thao-Y-te/Quyet-dinh-137-QD-BYT-2020-Ke-hoach-Phong-chong-dich-benh-truyen-nhiem-433228.aspx. Accessed 14 Aug 2024.
Chovatiya R, Silverberg JI. Inpatient morbidity and mortality of measles in the United States. PLoS ONE. 2020;15:e0231329.
Hassan MY, Mohamud RYH, Kassim MM, Hussein AI, Adam MK, Akbulut UE, et al. Clinical characteristics and outcomes of patients hospitalized with measles during an outbreak in Somalia. IJID Reg. 2023;8:31–5.
Luo W, Zhou Y, Liu Z, Kang W, He S, Zhu R, et al. Cross-regional analysis of the association between human mobility and COVID-19 infection in Southeast Asia during the transitional period of living with COVID-19. Health Place. 2023;81:103000.
Nguyen THT, Nguyen TV, Luong QC, Ho TV, Faes C, Hens N. Understanding the transmission dynamics of a large-scale measles outbreak in Southern Vietnam. Int J Infect Dis. 2022;122:1009–17.
Yang W, Wen L, Li S-L, Chen K, Zhang W-Y, Shaman J. Geospatial characteristics of measles transmission in China during 2005 – 2014. PLoS Comput Biol. 2017;13:e1005474.
Pampaka D, López-Perea N, Fernández-García A, Huertas-Zarco I, Castellanos-Martínez M, Villatoro-Bongiorno K, et al. An interregional measles outbreak in Spain with nosocomial transmission, November 2017 to July 2018. Eurosurveillance. 2023;28:2200634.
Ciofi degli Atti M, Filia A, Bella A, Sisto A, Barbieri MA, Reale A, et al. Measles cases in children requiring Hospital Access in an academic Pediatric Hospital in Italy, 2008–2013. Pediatr Infect Dis J. 2017;36:844–8.
Papaevangelou V. Measles vaccination of special risk groups. Hum Vaccines Immunotherapeutics. 2021;17:5384–7.
Acknowledgements
Not applicable.
Funding
The study was supported by the Hospital’s Internal Research fund. TO is supported by the Nuffield Department of Medicine Tropical Network Fund and OUCRU Studentship. MC is supported by the Wellcome Trust through the core grant of OUCRU.
Author information
Authors and Affiliations
Contributions
Conceptualization: NTP, TMD, DHH, PHP, TCV and TO; funding acquisition: NTP, TMD, and MC; methodology: NTP, TMD, QTP, TO and MC; data analysis: NTP, TO, and MC; investigation: NTP, TMD, DHH, TMD, TCV and PHP; resources: TMD; data curation: NTP, TO, and MC; supervision: NTP, TMD, and MC; project administration: NTP; validation: NTP, TO, TMD, MC and PHP; visualization: NTP, and TO; writing—original draft preparation, NTP, and TO; writing— review and editing, NTP, TMD, TO, MC, QTP and DHH.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the Vietnam National Children’s Hospital, which waived the requirement for consent to participate because the analysis was retrospective (Approval reference number: 473/BVNTW-HDDD, IRB identifier: IRB-VN01037/IRB00011976/FWA00028418).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tran, D.M., Ong, T., Cao, T.V. et al. Hospital-acquired infections and unvaccinated children due to chronic diseases: an investigation of the 2017–2019 measles outbreak in the northern region of Vietnam. BMC Infect Dis 24, 948 (2024). https://doi.org/10.1186/s12879-024-09816-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09816-w