Abstract
Background
Nirmatrelvir/ritonavir (NM/r) is a safe and effective oral antiviral therapeutic used for treatment of mild-to-moderate COVID-19. Case reports described a clinical rebound syndrome whereby individuals experience a relapse of symptoms shortly after completing successful treatment. There is a lack of information on frequency of COVID-19 rebound after NM/r in routine clinical care, contributing factors, and clinical outcomes.
Methods
We reviewed electronic medical records to verify COVID-19 diagnosis, symptoms, and treatment with NM/r from January-June 2022. We defined COVID-19 clinical rebound as clear improvement in symptoms followed by recurrence or worsening of symptoms within 30 days of a five-day course of NM/r.
Results
We studied 268 adults with median age 57 (IQR 47, 68), 80% White race, 85% non-Hispanic ethnicity, 55% female, 80% vaccinated and boosted against SARS-CoV-2, and 68% with any co-morbidity. Sixteen (6.0%) of studied patients were determined to have COVID-19 clinical rebound. The median time from starting NM/r to rebound was 11 days (IQR 9, 13). Notable demographic and clinical factors with higher proportion (not statistically significant) among COVID-19 rebound patients were female sex (75% rebound vs. 54.5% no rebound), Black race (12.5% rebound vs. 4.9% no rebound), presence of at least one co-morbidity (81.3% rebound vs. 67.5% no rebound), and lack of prior SARS-CoV-2 infection (100% rebound vs. 92.9% no rebound). Only one patient (6.25%) was hospitalized after COVID-19 rebound.
Conclusions
COVID-19 clinical rebound after treatment with NM/r is mild with favorable outcomes and more common than previously reported from real-world clinical care studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Nirmatrelvir/ritonavir (NM/r) (Paxlovid) is an oral antiviral therapy that has been granted FDA approval for the treatment of mild-to-moderate COVID-19 with large cohort studies and randomized controlled trials demonstrating reductions in hospitalization or death [1,2,3] or subsequent complications [4] and lowering of SARS-CoV-2 viral load [5] among unvaccinated individuals with non-Omicron variants of SARS-CoV-2. After FDA Emergency Use Authorization (EUA) approval, NM/r was widely used in outpatient clinical practice and many providers observed symptomatic COVID-19 and SARS-CoV-2 antigen testing rebound several days after completing a five-day course of NM/r [6, 7]. Early case reports described individuals experiencing a relapse or recrudescence of COVID-19 symptoms or new symptoms after an initial clinical improvement on NM/r [8, 9]. One observational EMR-based study of outpatients with mild COVID-19 found the 30-day cumulative incidence of symptom rebound after NM/r treatment was only 0.8% [10]. In one carefully conducted cohort study with frequent symptom assessments, the 10-day cumulative incidence of COVID-19 symptom rebound (32%) was significantly greater in the treated group than the incidence (20%) among controls [11], while in other studies the 28-day cumulative incidence of COVID-19 symptom rebound was 19 to 26% regardless of anti-SARS-CoV-2 therapy [12, 13]. Thus, there remains uncertainty of the incidence of COVID-19 symptom rebound that is brought to medical attention and requires outpatient clinical assessment after NM/r treatment in the real-world.
There have been no clear clinical factors associated with COVID-19 symptom rebound and the current predominant, yet unproven, hypothesis is that COVID-19 rebound may occur due to a weaker or delayed immune response as NM/r suppresses SARS-CoV-2 early in infection; however, a thorough immunology study of patients with COVID-19 rebound observed robust antibody and T-cell immune responses regardless of NM/r treatment [14]. In terms of outcomes, COVID-19 rebound disease has been mild [7, 10, 15] and less than 1% have been hospitalized during rebound, but prior studies have not fully assessed healthcare system visits including telemedicine, emergency departments, urgent care centers, and ambulatory clinics [10, 16].
We performed this study from a large healthcare system in Chicago to provide additional real-world research on frequency and timing of COVID-19 clinical rebound, potential contributing factors, and outcomes among patients with varying levels of immunity due to vaccine or prior SARS-CoV-2 infection.
Methods
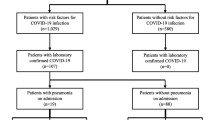
We conducted a clinical cohort study utilizing the Northwestern Medicine Enterprise Data Warehouse (NMEDW), an integrated repository of clinical data sources across the Northwestern Medicine (NM) system [17]. Inclusion criteria for our study was (1) patients who are above the age of 18, (2) have a confirmed positive COVID-19 diagnosis at a Northwestern Medicine location, (3) weigh > 40 kg, (4) had mild or moderate disease and (5) are at high risk for developing severe COVID-19 and being hospitalized. Mild COVID-19 disease was defined as having typical upper respiratory symptoms (rhinorrhea, cough, congestion, sore throat, etc.) without dyspnea, and moderate disease defined as having clinical or radiological evidence of lower respiratory tract disease and an oxygen saturation greater than or equal to 94% [18]. High risk has been elucidated in previous studies [19]; for this study it entailed having at least one of the following characteristics or comorbidities: chronic kidney disease, diabetes, hypertension, chronic obstructive pulmonary disease or chronic respiratory disease, age \(\:\ge\:\)65 years or age \(\:\ge\:\)55 years with cardiovascular disease, or BMI\(\:\ge\:\)30kg/m [2]. Patients who did not meet the above criteria were excluded from the study.
We identified adults (18 years or older) who had been prescribed NM/r by a NM provider between January 1, 2022 and May 31, 2022. We then reviewed electronic medical records (EMR) and included patients for whom we were able to verify COVID-19 diagnosis, determine symptoms, and confirm treatment with NM/r. We excluded individuals who did not have confirmed COVID-19 infection by testing (either antigen or PCR) or did not complete a full five-day course of NM/r. Finally, we evaluated for COVID-19 clinical rebound by reviewing provider and support staff EMR documentation of follow-up telehealth or in-person clinical encounters for a follow-up period of 30 days after starting NM/r. COVID-19 clinical rebound was defined as EMR documentation of provider-confirmed clinical improvement in COVID-19 symptoms followed by recurrence or worsening of prior COVID-19 symptoms or new symptoms consistent with COVID-19 after successful completion of NM/r and within 30 days of starting therapy.
Vaccine status was determined through NMEDW. Patients with at least one SARS-CoV-2 vaccine dose following a two-dose mRNA series (Pfizer or Moderna) or one-dose Janssen series were categorized as “boosted”, those with only a two-dose mRNA series or one-dose Janssen series were categorized as “fully vaccinated”, and all others were categorized as “not fully vaccinated”. Comorbidities were determined from ICD9/ICD10 diagnosis codes assigned at any time prior to starting NM//r. Obesity was determined by either coding or vitals indicating BMI > 30 within two years prior. Prior SARS-CoV-2 infection was determined by having any positive PCR tests at least 90 days prior to starting NM/r, with NMEDW capturing data as far back as March 2020. Health system encounter visits within 60 days of NM/r initiation were pulled from NMEDW, with chart review to verify whether the encounters listed COVID-19 as the primary diagnosis.
Descriptive statistics were utilized to describe patient characteristics, symptomology, and relapse clinical outcomes. This included proportions for categorical data and medians with interquartile ranges (IQRs) for continuous data. Bivariate comparative analyses between those with and without COVID-19 rebound were conducted using Fisher’s exact tests. Multivariable analyses were not performed due to the small number of COVID-19 rebound events. Analyses were performed in R (R version 4.2.1, https://www.r-project.org) and SAS (SAS Institute, Inc., Cary, NC) version 9.4.
Results
We included 268 adults who completed a five-day course of NM/r for outpatient treatment of mild COVID-19. The median age of patients was 57 years (IQR: 45, 69 years). We determined that 16 (6.0%) patients had COVID-19 clinical rebound within 30 days after completion of NM/r (Table 1). In the rebound group, 12 (75%) patients were female, compared to 134 (53.2%) in the no-rebound group (p = 0.12). Two (12.5%) patients identified as Black, compared to 11 (4.4%) in the no-rebound group (p = 0.18). None of the patients in the rebound group had previously tested positive for SARS-CoV-2 at NM, while 18 (7.1%) patients in the no-rebound group had prior positive testing (p = 0.61). Thirteen (81.3%) rebound patients had at least one comorbidity, compared to 168 (66.7%) in the no-rebound group (p = 0.29). All 16 (100%) of the COVID-19 rebound patients had been fully vaccinated and 12 (75%) had also received at least one booster vaccine dose, compared to 236 (93.6%) fully vaccinated and 203 (80.6%) vaccinated and boosted in the no-rebound group. None of the univariable statistical comparisons of demographic and clinical factors in Table 1 reached statistical significance (p-value < 0.05).
The median time from initiation of nirmatrelvir/ritonavir to COVID-19 clinical rebound was 11 days (IQR: 9,13). A graph of timing of COVID-19 clinical rebound can be found in Fig. 1.
The most common symptoms experienced during COVID-19 rebound were nasal congestion (68.8%) and cough (62.5%) (Table 2). COVID-19 rebound was brought to clinical attention and assessed via telemedicine (37.5%), immediate care (25%), and ambulatory (25%) visits (Table 2). Two COVID-19 rebound cases led to moderate-severe disease resulting in an emergency department visit with hospital admission, and a telemedicine assessment with subsequent immediate care center visit. A case-by-case description of demographics, clinical characteristics, and healthcare system visit for each of the 16 cases of COVID-19 rebound can be found in Table 3.
Discussion
We found that 6% of patients included in our study who completed a five-day course of NM/r developed COVID-19 clinical rebound leading to healthcare provider assessment within 30 days of treatment. Rebound symptoms were predominantly cough and nasal congestion occurring from 1 to 15 days following completion of NM/r. The timing of rebound was similar to prior case reports and cohort studies [20, 21]; however, our cumulative incidence was higher than 0.8% reported in one prior clinical care study [10] of outpatients with mild COVID-19. A rigorously conducted prospective study found a considerably higher cumulative incidence of symptom rebound after NM/r of 18.9%, and incidence in those not treated in this study was similar to our study at 7% 12. Several studies have observed frequency of symptom rebound similar between those who did and did not receive NM/r [2, 22]. One study of the placebo arm of ACTIV clinical trials found higher COVID-19 symptom rebound at 26%[13]. These results suggest symptom recrudescence or worsening is common in the natural course of resolving COVID-19 disease regardless of anti-viral treatment. These discrepancies are likely due to study methodology whereby carefully conducted cohort studies performed daily or every other day symptom and nasal swab virology assessments. Thus, they were more likely to pick up mild and/or transient symptom recurrence and overestimate the rate of COVID-19 rebound. Our study relied on both patient and provider reporting to the NM healthcare system and recording in medical records which may not have occurred for many patients with mild rebound illness or who sought care outside of our clinics. In summary, we estimate that COVID-19 symptom rebound frequency after NM/r lies between 6 and 19%, depending on patient characteristics, severity of symptoms, and ease of reporting or symptom assessment.
In terms of risk factors, like other studies, we did not find any significant associations between demographic or clinical characteristics and COVID-19 symptom rebound after NM/r. An interesting observation was an indication that patients with lower immunity to SARS-CoV-2 (less vaccine boosting, lack of prior infection, and co-morbidities) experienced higher frequency of COVID-19 symptom rebound after NM/r. This supports the current hypothesis that NM/r anti-viral activity and reduction of SARS-CoV-2 in tissues is enhanced by strong host immunity. Thus, COVID-19 viral and/or symptom rebound is more likely to occur among those who fail to adequately clear SARS-CoV-2 virus in the upper respiratory tract in a dynamic process. Anti-viral therapies, such as NM/r, inhibit viruses and reduce the potential for severe complications such as pneumonia; however, viral clearance takes time and virus replication after completion of NM/r could increase due to several potential mechanisms. This is supported by in a prior study with frequent early PCR and viral culture sampling that found significantly greater virologic rebound and prolonged shedding of replication-competent SARS-CoV-2 virus after NM/r treatment compared to no COVID-19 therapy [23]. Contrary to this hypothesis was a carefully conducted immunology study that found individuals treated with NM/r for COVID-19 had similar robust humoral and T-cell immune responses [14] regardless of whether they experienced rebound; however, it is unclear whether viral dynamics and clearance were different within upper respiratory tract tissues. In addition, while resistance gene mutations encoding in SARS-CoV-2 protease have been suggested as a cause of viral rebound, this has not yet been observed [14, 20].
Other potential risk factors we identified for clinical rebound after NM/r were female sex, Black race, having co-morbidities, and systemic symptoms. Similar to other studies [11], a non-significant, but higher proportion of patients with rebound had systemic symptoms of fever, shortness of breath, myalgia, and headache with their presenting COVID-19 illness, possibly indicating a more severe presentation. These findings are also likely to be the result of higher health awareness and health-seeking behaviors for certain demographic groups. Black race and certain comorbidities have been associated with more severe COVID-19 infection throughout the pandemic [24, 25]. It is unlikely that there is a biological basis to an association with Black race and a higher risk of rebound – rather, it is likely due to the higher prevalence of certain comorbidities among Black individuals [26]. This is potentially due to multiple factors, including socioeconomic status and access to and treatment within the healthcare system. Interestingly, this lack of access to the healthcare system would be expected to underestimate any potential association between Black race and rebound; this potential association should be investigated further in larger studies. As briefly mentioned above, comorbidities could contribute to rebound for several reasons -- a weaker immune response to SARS-CoV-2 infection and lower viral clearance/control, greater susceptibility to respiratory infection or multi-organ involvement, and greater engagement with the healthcare system.
As reported in many prior studies and case reports, we also found that rebound COVID-19 is generally mild, managed on an outpatient basis, and does not lead to poor health outcomes. Only one case of NM/r rebound in this study led to an ED visit and hospital admission, with the rest managed by ambulatory care or telemedicine. Thus, when weighing benefits and risks of NM/r treatment in light of the potential for rebound COVID-19, recent real-world research continues to show clear benefits of NM/r treatment in high-risk outpatient populations regardless of immunity from vaccine or natural infection [2].
Limitations
This study was subject to several limitations since it was observational, EMR-based, and relied on adequate documentation from providers and healthcare staff to meet our definition of COVID-19 rebound. Thus, there was the possibility of misclassification and underreporting of rebound symptoms and certain important risk factors such as SARS-CoV-2 vaccination or previous COVID-19. In addition, we were unable to assess patient adherence and had to assume that patients who started the regimen completed the entire 5-day course. However, our study of a diverse subset of patients in a large metropolitan healthcare system found that NM/r rebound is occurring, tends to be mild, and identified potential risk factors and rebound mechanisms to be further investigated.
Conclusion
COVID-19 clinical rebound after treatment with NM/r is more common than previously reported in the peer-reviewed published literature. Rebound is generally mild and has favorable outcomes. Potential risk factors for experiencing rebound are female sex, Black race, systemic symptoms with COVID-19 illness, the presence of comorbidities, and lower SARS-CoV-2 immunity due to under vaccination or lack of prior COVID-19, though none of these factors achieved statistical significance in our analysis. These factors should be investigated further in larger observational studies.
Data availability
A de-identified dataset may be made available upon reasonable request.
Abbreviations
- COVID:
-
19–coronavirus disease 2019
- EDW:
-
Enterprise data warehouse
- EMR:
-
Electronic medical record
- FDA:
-
Food and Drug Administration
- ICD:
-
International Classification of Diseases
- NM:
-
Northwestern Medicine
- NM/r:
-
Nirmatrelvir–ritonavir
- PCR:
-
Polymerase chain reaction
- SARS:
-
CoV–2–severe acute respiratory syndrome coronavirus 2
References
Mahase E. Covid-19: Pfizer’s paxlovid is 89% effective in patients at risk of serious illness, company reports. BMJ Nov. 2021;8:375:n2713. https://doi.org/10.1136/bmj.n2713.
Amani B, Amani B. Efficacy and safety of nirmatrelvir/ritonavir (paxlovid) for COVID-19: a rapid review and meta-analysis. J Med Virol Feb. 2023;95(2):e28441. https://doi.org/10.1002/jmv.28441.
Dryden-Peterson S, Kim A, Kim AY, et al. Nirmatrelvir plus Ritonavir for early COVID-19 in a large U.S. health system: a population-based cohort study. Ann Intern Med. Jan 2023;176(1):77–84. https://doi.org/10.7326/m22-2141.
Ganatra S, Dani SS, Ahmad J, et al. Oral nirmatrelvir and ritonavir in nonhospitalized vaccinated patients with coronavirus cisease 2019. Clinical infectious diseases: an Official publication of the Infectious Diseases Society of America. Feb 2023;18(4):563–72. https://doi.org/10.1093/cid/ciac673.
Hammond J, Leister-Tebbe H, Gardner A, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N Engl J Med. Apr 2022;14(15):1397–408. https://doi.org/10.1056/NEJMoa2118542.
Wong CKH, Lau KTK, Au ICH, et al. Viral burden rebound in hospitalised patients with COVID-19 receiving oral antivirals in Hong Kong: a population-wide retrospective cohort study. Lancet Infect Dis Feb. 2023;13. https://doi.org/10.1016/s1473-3099(22)00873-8.
Lai CC, Hsueh PR. Coronavirus disease 2019 rebounds following nirmatrelvir/ritonavir treatment. J Med Virol Feb. 2023;95(2):e28430. https://doi.org/10.1002/jmv.28430.
Coulson JM, Adams A, Gray LA, Evans A. COVID-19 rebound associated with nirmatrelvir/ritonavir pre-hospital therapy. J Infect Jun. 2022;17. https://doi.org/10.1016/j.jinf.2022.06.011.
CDC Health Alert Network. COVID-19 rebound after Paxlovid treatment. CDC. Updated May 24. Accessed July 1. 2022. https://emergency.cdc.gov/han/2022/han00467.asp
Ranganath N, O’Horo JC, Challener DW, et al. Rebound phenomenon after nirmatrelvir/ritonavir treatment of Coronavirus Disease 2019 (COVID-19) in high-risk persons. Clin Infect Diseases: Official Publication Infect Dis Soc Am Feb. 2023;8(3):e537–9. https://doi.org/10.1093/cid/ciac481.
Smith-Jeffcoat SE, Biddle JE, Talbot HK, et al. Symptoms, viral loads, and rebound among Coronavirus Disease 2019 (COVID-19) outpatients treated with nirmatrelvir/ritonavir compared with propensity score–matched untreated individuals. Clin Infect Dis. 2023. https://doi.org/10.1093/cid/ciad696.
Pandit JA, Radin JM, Chiang DC, et al. The Coronavirus Disease 2019 (COVID-19) rebound study: a prospective cohort study to evaluate viral and symptom rebound differences in participants treated with nirmatrelvir plus ritonavir versus untreated controls. Clin Infect Dis. 2023. https://doi.org/10.1093/cid/ciad102.
Deo R, Choudhary MC, Moser C, et al. Symptom and viral rebound in untreated SARS-CoV-2 infection. Ann Intern Med. Mar 2023;176(3):348–54. https://doi.org/10.7326/m22-2381.
Epling BP, Rocco JM, Boswell KL, et al. Clinical, virologic, and immunologic evaluation of symptomatic Coronavirus Disease 2019 rebound following nirmatrelvir/ritonavir treatment. Clin Infect Diseases: Official Publication Infect Dis Soc Am Feb. 2023;18(4):573–81. https://doi.org/10.1093/cid/ciac663.
Smith DJ, Lambrou A, Patel P. SARS-CoV-2 Rebound with and without use of COVID-19 oral antivirals. MMWR Morbidity Mortal Wkly Rep Dec. 2023;22(51):1357–64. https://doi.org/10.15585/mmwr.mm7251a1.
Malden D, Hong V, Lewin B. Hospitalization and emergency department encounters for COVID-19 after paxlovid treatment — California, December 2021–May 2022. MMWR Morbidity Mortal Wkly Rep 2022. 2022;71:830–3. https://doi.org/10.15585/mmwr.mm7125e2.
Starren JB, Winter AQ, Lloyd-Jones DM. Enabling a learning health system through a unified Enterprise Data Warehouse: the experience of the Northwestern University Clinical and Translational Sciences (NUCATS) Institute. Clin Transl Sci Aug. 2015;8(4):269–71. https://doi.org/10.1111/cts.12294.
Gandhi RT, Lynch JB, Del Rio C. Mild or moderate Covid-19. N Engl J Med Oct. 2020;29(18):1757–66. https://doi.org/10.1056/NEJMcp2009249.
Ko JY, Danielson ML, Town M, et al. Risk factors for Coronavirus Disease 2019 (COVID-19)-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and behavioral risk factor Surveillance System. Clin Infect Diseases: Official Publication Infect Dis Soc Am Jun. 2021;1(11):e695–703. https://doi.org/10.1093/cid/ciaa1419.
Charness ME, Gupta K, Stack G, et al. Rebound of SARS-CoV-2 infection after nirmatrelvir-ritonavir treatment. N Engl J Med Sep. 2022;15(11):1045–7. https://doi.org/10.1056/NEJMc2206449.
Han J, Bae S, Jung J, et al. Clinical characteristics of COVID-19 rebound after nirmatrelvir-ritonavir or molnupiravir therapy: a prospective cohort study. Med Sep. 2023;29(39):e35094. https://doi.org/10.1097/md.0000000000035094.
Anderson AS, Caubel P, Rusnak JM. Nirmatrelvir-Ritonavir and viral load rebound in Covid-19. N Engl J Med Sep. 2022;15(11):1047–9. https://doi.org/10.1056/NEJMc2205944.
Edelstein GE, Boucau J, Uddin R, et al. SARS-CoV-2 virologic rebound with nirmatrelvir-ritonavir therapy: an observational study. Ann Intern Med. Dec 2023;176(12):1577–85. https://doi.org/10.7326/m23-1756.
Hippisley-Cox J, Coupland CA, Mehta N, et al. Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: National prospective cohort study. Bmj Sep. 2021;17:374:n2244. https://doi.org/10.1136/bmj.n2244.
Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. Mar 2021;174(3):362–73. https://doi.org/10.7326/m20-6306.
Gupta R, Agrawal R, Bukhari Z et al. Higher comorbidities and early death in hospitalized African-American patients with Covid-19. BMC Infectious Diseases. 2021/01/18 2021;21(1):78. https://doi.org/10.1186/s12879-021-05782-9
Acknowledgements
Not applicable.
Funding
Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences (grant number UL1TR001422) which supports the Northwestern Medicine Enterprise Data Warehouse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Research reported in this publication was also supported by the Division of Infectious Diseases and its emerging and re-emerging pathogens program (EREPP) at the Northwestern University Feinberg School of Medicine.
Author information
Authors and Affiliations
Contributions
D.M.C., M.C., and C.J.A designed the study, wrote the research study procedures, defined variables/outcomes, and a priori statistical analysis plans. M.C. identified adults who received NM/r in the NM EDW system. D.M.C, F.M.E., and C.J.A conducted EMR chart review, determination of COVID-19 clinical rebound, and data collection. Statistical analyses were performed by M.C. with assistance from C.J.A. The initial draft of the manuscript was written by D.M.C., M.C. and C.J.A. Throughout the study, all authors participated in discussions about the study conduct, analyses, and interpretation of findings. All authors were also involved in the review and editing process of the final manuscript for submission. All authors declare that they have no conflicts of interest.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Northwestern University IRB (STU00212267) and a waiver of consent was granted. The study was conducted in accordance with the Declaration of Helsinki as revised in 2013.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Camp, D., Caputo, M., Echevarria, F.M. et al. Clinical rebound after treatment with nirmatrelvir/ritonavir in COVID-19. BMC Infect Dis 24, 963 (2024). https://doi.org/10.1186/s12879-024-09842-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09842-8