Abstract
Background
To conduct a systematic review looking into the possibility of US imaging to anticipate and identify future patellar or Achilles tendinopathy symptoms.
Methods
The studies that were taken into consideration for this review were prospective studies that employed baseline US imaging of the patellar OR Achilles tendons in asymptomatic patients and follow-up measures of pain and/or function. Two impartial reviewers evaluated the study’s quality using the Critical Appraisal Skills Programme instrument.
Results
Participants in the included studies in this review came from various sports. The systematic review revealed a link between baseline tendon abnormalities in the US and a higher chance of developing both patellar and Achilles tendinopathy as well as their future occurrence. Nine of the included studies examined the patellar tendon alone, eight the patellar and Achilles tendon together, and four the Achilles tendon exclusively. For both tendons, US administration is done in a largely consistent manner. The tendon abnormalities of tendon thickness, hypoechogenicity and vascularity at baseline were associated with an increased risk of both Achilles and patellar tendinopathy.
Conclusions
This systematic review shows that abnormal tendon structures seen by US in asymptomatic persons can predict the development of tendinopathy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Lower limb tendinopathy is distinguished by activity-related pain that prevents people from engaging in sports and recreational activities [1]. Both MRI and ultrasound can offer detailed morphological information about patients with Achilles and patellar tendons overuse problems. Despite these apparent benefits, structural abnormalities identified by imaging may not exactly match with symptoms [2]. In clinical practice, imaging has typically served as a diagnostic and monitoring tool. Due to its quick, easy, and practical application in sports and other disorders, the use of the US has expanded among musculoskeletal practitioners. Clinically, the US has been used to image the tendons to differentially diagnose, track the effectiveness of therapies, and eliminate the possibility of developing new symptoms in the future. The US has been used to assess painful tendons in athletes and identify structural anomalies such as tendon thickness with hypoechoic regions and increased vascularity [3]. Past prospective investigations have revealed that these structural irregularities raised the likelihood of tendinopathy symptoms developing in the future. Accordingly, it has been proposed that if these abnormalities are identified at baseline, high-risk asymptomatic athletes can be ruled out, and their training regimens and/or interventions can be changed to stop the development of further symptoms [4]. According to many cross-sectional studies assessing tendon structure, the phenomenon of future symptoms developing with structural abnormalities at baseline on imaging is still unclear, and it may be caused by a simple normal physiological response to the increased demands of sports and does not necessarily warrant future symptoms [5]. As a result, when medical experts discover structural abnormalities on imaging, they are unable to decide whether to change the training regimens of athletes or to take other preventative measures. Additionally, there is no standardized scanning process in place. Therefore, the purpose of this systematic review is to examine how ultrasound imaging might be used to anticipate future lower limb tendinopathy symptoms.
Search strategy and study selection
The study followed the strategy proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [6]. The institutional review board granted ethical approval (IRB-UOL-FAHS/829–1/2021) for data confidentiality. In January 2021, databases were used to build and conduct a thorough search strategy: Cumulative Index to Nursing and Allied Health Literature (CINHAL), MEDLINE, SPORTDiscs, AMED, EMBASE. The four categories of keywords were merged in search strategy: (1) US (2) tendinopathy (3) Achilles and patellar and (4) cohort/ prospective studies. The search strategies used MeSH terms and free terms combined with Boolean operators AND, OR, NOT. The summary of keywords for the search strategy is given in Table 1.
Inclusion criteria
The following were characteristics of prospective studies in which US imaging was utilized to predict patellar or Achilles tendon structure seen at baseline [7].
-
▸ To determine the likelihood of developing patellar or Achilles tendinopathy in the future, US readings associated with a clinical outcome measure (pain & functional impairment) are used.
-
▸ The follow-up period had to be at least 24 hours long.
-
▸ The analysis of the tendon structure could have been qualitative or quantitative.
-
▸ Studies must have been published within the last 20 years, in English.
-
▸ Participants in studies could be of any age.
-
▸ Participants with related comorbidities and those with insertional and mid-portion tendinopathy may be included in studies.
Exclusion criteria
Studies with the following characteristics excluded.
-
▸ Studies focusing solely on the evolution of tissue structural changes without accompanying clinical measurements (as indicated above).
-
▸ Studies that investigated the tendons other the patellar or Achilles tendon.
-
▸ examining the structure of animal tendons.
Assessment of methodological quality
The Critical Appraisal Skills Programme (CASP) checklist for cohort studies was utilized due to absence of an ideal methodological quality grading tool for prospective research of this kind [8]. There are 12 questions on this checklist; the first two are screening questions, and the following 10 probe the study’s findings, their reliability, and their application to the local population.
For the purposes of this review, questions 2, 7, 8, and 9 were combined because they address related topics. Consequently, seven guiding questions were used to evaluate the included studies. Consistency is crucial when analyzing research because the CASP has numerous factors to consider for each question. As a result, the authors developed and agreed upon a list of criteria for each issue to be taken into account when evaluating the quality of the included studies. Using the listed criteria, two authors independently rated the studies, with a third reviewer mediating any scoring discrepancies. No overall quality score was given to the included studies because the CASP checklist was initially intended to be used as a teaching tool in a workshop environment. Instead, based on these precise criteria, the advantages and disadvantages of each study were evaluated.
Data extraction
Two reviewers took data from the studies that were included, including information on patients’ demographics, population samples, measures of tendon structure, the number of tendons that developed symptoms among those who had baseline imaging that was normal or abnormal, and the definition of tendon abnormality given in each study. Any variation in tendon structure, such as hypoechogenicity, increased thickness, or increased vascularity as observed on power Doppler US, were all considered to be tendon abnormalities. Data were analyzed collectively due to similarities in the outcome measures utilized, the tendons involved, the participants, and the ability to predict future symptoms. The corresponding authors of the original study were contacted in cases where data weren’t accessible or where the methodology needed to be clarified. The results were not included in the systematic review and were instead presented descriptively if information on tendon structure measurements and the number of tendons among individuals with normal or abnormal imaging at baseline were not readily available.
Results
Studies identification
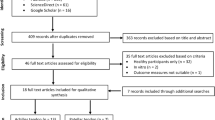
An electronic search yielded 2795 potentially pertinent studies in total. After data from 1274 studies overlapped, they were all excluded. After the screening of titles and abstracts of each study, 43 full-text studies were recognized as potentially relevant studies. Twenty-three further studies were excluded after screening the full text of short-listed studies. The procedure for studies identification is given in Fig. 1.
Features of the included studies
Table 2 provides a thorough illustration of the selected studies. Participants’ ages ranged from 15 to 66 years, with a similar mean age across all the included studies. Regarding participant characteristics, all but one of the 20 studies that were considered were conducted among athletes. Particularly five involved volleyball, [9, 36,37,38, 40] three had basketball, [14, 35, 39] three had soccer players, [11, 15, 16] one had elite fencers, [13] three had runners’ population, [12, 17, 18] one involved badminton, [19] and ballet dancers each, [20] and one had different sports playing populations [14]. Patients from the general population participated in one of the included studies [21]. There were exclusively male participants in seven out of the 20 studies, [11, 15,16,17,18, 38, 39] and the remaining 13 had participants of both genders. The follow-up time ranged widely, from 2 days to 4 years. An ultrasound was used in every study that was included to look into the tendon structure while only one study included used Ultrasound Tissue Characterization for tendon structure evaluation [36]. Nine studies explored tendon thickness, Hypoechogenicity, and vascularity, [9, 12, 13, 15, 21, 22, 37, 38, 40] six studies investigated tendon thickness and hypoechogenicity, [11, 14, 16, 18, 35, 39] two investigated Thickness, Hypoechogenicity, Intratendinous delamination, and Calcifications, [17, 23] two investigated hypoechogenicity, [20, 36] and one investigated vascularity only [19]. There were many different clinical outcome measures for pain and/or function, including subjective pain, functional capacity (such as VISA- scale), and performance-specific tests like the single-leg squat and plyometric exercises, as well as pain and tenderness on palpation.
Study quality & scoring
Table 3 displays the critical evaluation of included studies using the CASP checklist. Overall, most studies met the inclusion criteria. Each of the included studies employed a representative sample size and recruited people in accordance with predetermined suitable inclusion criteria. The control of confounding factors, such as the use of blinding and/or regulation of training load, was one of the key limitations of the studies that were included. There were differences in the methodological quality about the proper follow-up of the included participants. The above-mentioned wide heterogeneity in how pain and/or function were assessed is a last methodological point of concern. The completeness, interpretation, and generalizability of the results may have all been impacted because several studies did not fit the criteria. However, in general, each of the included research used adequate study designs, sound methodological quality, and had stated objectives.
Ultrasound protocol administration and results of the included studies are shown in Table 4. Mostly, studies included 1–2 positions to execute ultrasound scans of patellar and Achilles’ tendons: the supine positions and prone positions, respectively. Of the supine position, various knee flexion angles were used: 20degrees, [9, 18, 37] 30degrees, [13, 39] 90degrees, [16, 20] 100degrees, [36] 120degrees, [17] one study used patient in supine with knee extension, [40] while for Achilles the ankle flexion used: 90 degrees with feet hanging over the table [13, 15,16,17, 21, 22]. One study evaluated anterior knee tendons with supine and 15 degrees knee flexion, [19] five of the included studies did not describe a patient position for an ultrasound scan [13, 16, 20, 23, 36, 37]. Six out of all included studies used the proximal to distal approach for ultrasound scan. While the rest of the studies did not describe the approach used. Only two studies used unilateral ultrasound limb scans, [20, 36] while the rest had a bilateral scan of either patellar or Achilles’ tendons. Most of the studies that were reviewed looked on whether the US could forecast when patellar or Achilles tendinopathy will arise [7]. However, several authors claimed there is either no or little correlation between baseline structural abnormalities and subsequent tendinopathy. One of the studies revealed that there isn’t much of a change in tendon structure (echo types I–IV) during a sporting event, [36] and other studies concluded that ultrasound appearance of the tendon should not be solely responsible for the management of patellar tendinopathy [14]. Furthermore, a study that looked at tendons concluded that there is no connection between structural irregularity and potential tendinopathy [15].
Discussion
Main findings
The findings of this study showed a recurrent trend, which was consistent throughout the included studies, of an elevated risk of Achilles and patellar tendinopathy in the presence of baseline abnormalities of tendon thickness, Hypoechogenicity, and vascularity in the tendons.
The burden of tendinopathy
While patellar tendinopathy is prevalent, especially in activities involving jumping, Achilles tendinopathy can affect up to 30% of runners [24]. Despite the relatively high occurrence of lower limb tendinopathy, particularly in populations involved in sports, rehabilitation is still time-consuming and has a mixed history of success [25, 26]. This causes frustration from both the standpoint of the athlete and the health professionals. In addition, protracted and occasionally successful rehabilitation in amateur and professional sports places a greater financial strain on players and athletic organizations.
The role of ultrasound in predicting tendinopathy
Identification of “at risk” athletes is a top priority to try to prevent the detrimental effects of tendinopathy on sporting participation and quality of life, given the significant impact of Achilles and patellar tendinopathy [27]. The preferred imaging modalities for determining tendon dimensions are MRI and US technologies [28]. Particularly in the field of sports medicine and tendon disorders, US has grown in favor among musculoskeletal practitioners, and recent technological improvements have made US more accessible and cheaper [29, 30]. The findings of this systematic review showed a recurrent pattern suggesting that baseline structural abnormalities of tendon thickness, Hypoechogenicity and vascularity in the tendon are related to the emergence of future tendinopathy. As a result, it’s possible that structural abnormalities in populations who are asymptomatic are indicators of early, pre-symptomatic pathology that will eventually manifest as episodes of pain and/or diminished function [31]. These results’ robustness and consistency may have significant effects on the therapeutic treatment and avoidance of patellar and Achilles tendon disorders. Utilizing US to see tendon anomalies may help identify athletes who may be at risk and enable timely intervention through the use of preventative measures like modifying training loads [32] or adopting the proper tendon loading programs [11]. Future research is necessary because there is currently insufficient evidence to justify such techniques.
Given the generally poor link between structure and pain in tendinopathy, intervention may not be indicated in all instances of structurally aberrant tendons identified using US imaging. Studies have found tendon abnormalities in as many as 59% of asymptomatic populations, with the prevalence of these abnormalities rising with age and involvement in sports [10]. Tendon structural abnormalities have been observed in a significant proportion of asymptomatic individuals [10]. Numerous investigations have shown that structural changes in asymptomatic sports populations across the body, in addition to structural abnormalities in tendons, are common. Papavasiliou et al. [33] used MRI to examine structural changes in the hip in asymptomatic gymnasts, the results showed that up to 63% of the sample group had hip “impingement” symptoms. These findings are confirmed in a variety of body parts and among athletes, with structural abnormalities in the shoulder, knee, hip, and spine occurring in as many as 89% of asymptomatic athletes [34, 41,42,43].
Evidence also points to the possibility that unneeded imaging interventions may have a negative and damaging impact on patients’ perceptions and habits [44]. For instance, one study of low-risk LBP patients found that those who underwent imaging had worse overall outcomes in terms of pain and general health than those who got no imaging [45]. Unfortunately, there has not yet been any comparable studies on tendon problems, thus caution should be used when drawing direct analogies between LBP and tendon disorders. With the rising acceptance and potential benefits of techniques like UTC or elastography, it may be possible to see the tendon anatomy more clearly. The need to weigh the possible negative effects of having an athlete feel as though their body is vulnerable based on what may be typical physiological reactions to the loading demands arises with enhanced visualization. This may point to the critical importance of a clinician’s communication techniques when conveying imaging results to athletic populations. This illustrates how complicated tendinopathy is and how little we understand it [10].
Clinical implications
Although structural abnormalities are a strong indicator of future tendinopathy development, it can be challenging to interpret this association in a clinical setting due to the prevalence of abnormalities in asymptomatic people. Therefore, rather than serving as the primary predictor of tendinopathy, structural anomalies may instead need to be taken into account as one of numerous risk factors. There are numerous additional intrinsic and extrinsic risk factors for the onset of tendinopathy. Extrinsic risk factors have been identified for training frequency and volume, [46] larger impacts brought on by faster training, [47] a change in surface density, and shock absorption [48]. Modified foot function, [48] decreased ankle dorsiflexion, [49] sex, [35] diabetes, [50] obesity, [51] muscle weakness, [52] and hereditary factors [53] have all been proposed in relation to intrinsic risk variables. Unfortunately, because most studies on these issues have been cross-sectional, it has been difficult to establish a clear cause-and-effect relationship. Because of this, it is still unknown how these factors might interact to predict the development of tendinopathy, despite advances in our understanding of lower limb tendinopathy. One could argue that routine imaging might be expensive and time-consuming given the high prevalence of structural abnormalities in asymptomatic people. Any modality that enables the identification of athletes at higher risk of injury may, however, outweigh the cost or time-consuming aspect of routine imaging given the financial burden and the potentially career-threatening consequences of tendinopathy in sporty populations [54].
As the limitation of the biomedical structure-pain model become more apparent, there is a growing need to examine sports injuries and injury prevention from a biopsychosocial perspective, which takes into account factors like sociodemographic, psychological, lifestyle, and social factors in addition to local tissue damage [55]. Psychosocial problems that have been linked to injury development in athletic populations include sleep disturbances, [56] fatigue, [57] and anxiety [58]. However, in studies that predict injuries, there has been a reluctance to combine intrinsic psychosocial elements—such as training load, strength, or biomechanics—with other conventional biological risk factors, despite the significance of these factors in the development of injury. Prospective studies combining some of the psychological components mentioned above with traditional risk factors like tendon imaging may offer much-needed clarity and understanding in the complex field of tendinopathy, or possibly even sports injury prevention in general.
Limitations
Reliability is one of the most brought up objections to US imaging. Due to factors like inexperienced operators, non-standardized imaging techniques, and different transducer positions, [59] US is thought to have a larger chance of error or variance when measuring tendon diameters than MRI. A recent systematic review [60] showed that US displays good to exceptional levels of inter-rater and intra-rater reliability in evaluating tendon thickness and cross-sectional area, despite the fact that operator experience varied greatly among the included investigations.
The inconsistent wording used to describe what is considered a structurally “abnormal” tendon when examined via US is another potential weakness of this review. For instance, Comin et al. [23] employed hypoechoicity (mild, moderate, severe) or its absence to identify abnormalities. Greater than 1 mm of tendon thickening was deemed abnormal in three studies [11, 15, 16]. A tendon needed to be thicker than 3 mm in one study to be classified as abnormal, [22] whereas a tendon needed to be thicker than 6 mm in another study to be classified as abnormal [21]. Because of the wide variation in what constitutes an abnormal tendon among the studies that were included, it is possible to overestimate or underestimate the association between structure and potential future symptoms. Another limitation is to the study populations that were examined; the bulk of them focused on communities of athletes. When extrapolating results to non-athletic populations, care should be used because Achilles and patellar tendinopathy are common in non-athletic populations.
The absence of gold standard diagnostics for detecting tendinopathy is another possible limitation. Regarding the best clinical diagnostic test for tendinopathy, there is a lack of agreement in the research and clinical domains. It is challenging to determine the diagnostic value of US findings because of the broad variance in diagnostic tests utilized in the research in this evaluation and the lack of a commonly recognized gold standard test. Finally, several studies in this review investigated the Doppler US ability to predict tendon vascularity. When employing Doppler settings, temperature is a key confounding variable [61]. However, none of the included Doppler US studies showed that they were adjusting for this confounding factor. However, as only one study used vascularity as the sole indicator, it is doubtful that this concern had an impact on the results.
Future implications
This study implies that ultrasonography could be used to identify athletes and sportsmen who are more likely to have tendon pathology. In order to reduce the chance of discomfort, these “high-risk” sportsmen could be assessed for biomechanical and training risk factors and given recommendations for training plans or preventative exercise interventions, as well as for quicker rehabilitation should they start to experience symptoms. There is currently no evidence that preventative workouts based on these abnormalities are useful. The logical next step in study is to uncover biomechanical and training risk factors for the development of tendon pathologies in athletes.
Conclusion
According to the findings of this systematic review, tendon anomalies are a strong indicator of future Achilles or patellar tendinopathies. This could have significant therapeutic ramifications for the treatment and prevention of tendon diseases. The relationship between tendon anomalies and the emergence of subsequent symptoms, however, was only mild. Furthermore, imaging results should only be considered as one element of the clinical prediction of tendinopathy due to the high prevalence of tendon anomalies in asymptomatic tendons.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
References
Martin J, Perraton L, Gupta A, Garofolini A, Malliaras P. The use of physical function capacity measures in the management of lower limb tendinopathy: a scoping review of expert recommendations. Phys Ther Sport. 2022;59.
Barile A, Bruno F, Mariani S, Arrigoni F, Brunese L, Zappia M, et al. Follow-up of surgical and minimally invasive treatment of Achilles tendon pathology: a brief diagnostic imaging review. Musculoskelet Surg. 2017;101:51–61.
Arias-Buría JL, Fernández-de-Las-Peñas C, Rodríguez-Jiménez J, Plaza-Manzano G, Cleland JA, Gallego-Sendarrubias GM, et al. Ultrasound characterization of patellar tendon in non-elite sport players with painful patellar tendinopathy: absolute values or relative ratios? A pilot study. Diagnostics. 2020;10(11):882.
Cassel M, Risch L, Intziegianni K, Mueller J, Stoll J, Brecht P, et al. Incidence of Achilles and patellar tendinopathy in adolescent elite athletes. Int J Sports Med. 2018;39(9):726–32.
Fazekas ML, Sugimoto D, Cianci A, Minor JL, Corrado GD, d’Hemecourt PA. Ultrasound examination and patellar tendinopathy scores in asymptomatic college jumpers. Phys Sportsmed. 2018;46(4):477–84.
Gates NJ, March EG. A neuropsychologist’s guide to undertaking a systematic review for publication: making the most of PRISMA guidelines. Neuropsychol Rev. 2016;26:109–20.
McAuliffe S, McCreesh K, Culloty F, Purtill H, OSullivan K. Can ultrasound imaging predict the development of Achilles and patellar tendinopathy? A systematic review and meta-analysis. Br J Sports Med. 2016;50(24):1516–23.
Hyde M, Higgs P, Wiggins R, Blane D. A decade of research using the CASP scale: key findings and future directions. Taylor & Francis; 2015. p. 571–5.
Gisslén K, Gyulai C, Nordström P, Alfredson H. Normal clinical and ultrasound findings indicate a low risk to sustain jumper’s knee patellar tendinopathy: a longitudinal study on Swedish elite junior volleyball players. Br J Sports Med. 2007;41(4):253–8.
Docking SI, Ooi CC, Connell D. Tendinopathy: is imaging telling us the entire story? J Orthop Sports Phys Ther. 2015;45(11):842–52.
Fredberg U, Bolvig L, Andersen NT. Prophylactic training in asymptomatic soccer players with ultrasonographic abnormalities in Achilles and patellar tendons: the Danish super league study. Am J Sports Med. 2008;36(3):451–60.
Ooi C-C, Schneider ME, Malliaras P, Counsel P, Connell DA. Prevalence of morphological and mechanical stiffness alterations of mid Achilles tendons in asymptomatic marathon runners before and after a competition. Skelet Radiol. 2015;44:1119–27.
Giombini A, Dragoni S, Di Cesare A, Di Cesare M, Del Buono A, Maffulli N. Asymptomatic a chilles, patellar, and quadriceps tendinopathy: a longitudinal clinical and ultrasonographic study in elite fencers. Scand J Med Sci Sports. 2013;23(3):311–6.
Cook J, Khan K, Kiss Z, Coleman B, Griffiths L. Asymptomatic hypoechoic regions on patellar tendon ultrasound: a 4-year clinical and ultrasound followup of 46 tendons. Scand J Med Sci Sports. 2001;11(6):321–7.
Jhingan S, Perry M, O’Driscoll G, Lewin C, Teatino R, Malliaras P, et al. Thicker Achilles tendons are a risk factor to develop Achilles tendinopathy in elite professional soccer players. Muscles Ligaments Tendons J. 2011;1(2):51.
Fredberg U, Bolvig L. Significance of ultrasonographically detected asymptomatic tendinosis in the patellar and achilles tendons of elite soccer players: a longitudinal study. Am J Sports Med. 2002;30(4):488–91.
Cushman DM, Petrin Z, Eby S, Clements ND, Haight P, Snitily B, et al. Ultrasound evaluation of the patellar tendon and Achilles tendon and its association with future pain in distance runners. Phys Sportsmed. 2021;49(4):410–9.
Cushman DM, Petrin Z, Cummings K, Eby SF, English J, Teramoto M. Sonographic screening of distance runners for the development of future Achilles and Patellar tendon pain. Clin J Sport Med. 2022;32(5):493–500.
Boesen AP, Boesen MI, Torp-Pedersen S, Christensen R, Boesen L, Hölmich P, et al. Associations between abnormal ultrasound color Doppler measures and tendon pain symptoms in badminton players during a season: a prospective cohort study. Am J Sports Med. 2012;40(3):548–55.
Rudavsky A, Cook J, Docking S. Proximal patellar tendon pathology can develop during adolescence in young ballet dancers—a 2-year longitudinal study. Scand J Med Sci Sports. 2018;28(9):2035–41.
Khan K, Forster B, Robinson J, Cheong Y, Louis L, Maclean L, et al. Are ultrasound and magnetic resonance imaging of value in assessment of Achilles tendon disorders? A two year prospective study. Br J Sports Med. 2003;37(2):149–53.
Hirschmüller A, Frey V, Konstantinidis L, Baur H, Dickhuth H-H, Suedkamp NP, et al. Prognostic value of Achilles tendon Doppler sonography in asymptomatic runners. Med Sci Sports Exerc. 2012;44(2):199–205.
Comin J, Cook JL, Malliaras P, McCormack M, Calleja M, Clarke A, et al. The prevalence and clinical significance of sonographic tendon abnormalities in asymptomatic ballet dancers: a 24-month longitudinal study. Br J Sports Med. 2013;47(2):89–92.
Ackermann PW, Renström P. Tendinopathy in sport. Sports Health. 2012;4(3):193–201.
Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10(1):52–8.
Jonsson P, Alfredson H, Sunding K, Fahlström M, Cook J. New regimen for eccentric calf-muscle training in patients with chronic insertional Achilles tendinopathy: results of a pilot study. Br J Sports Med. 2008;42(9):746–9.
Kabore C, Salier Q, Geerts P, Kaux J-F. Management of systemic risk factors for chronic tendinopathy. Sci Sports. 2021;36(1):5–15.
Brushøj C, Henriksen B, Albrecht-Beste E, Hölmich P, Larsen K, Bachmann NM. Reproducibility of ultrasound and magnetic resonance imaging measurements of tendon size. Acta Radiol. 2006;47(9):954–9.
Albano D, Coppola A, Gitto S, Rapisarda S, Messina C, Sconfienza LM. Imaging of calcific tendinopathy around the shoulder: usual and unusual presentations and common pitfalls. Radiol Med. 2021;126:608–19.
Bjordal JM, Demmink JH, Ljunggren AE. Tendon thickness and depth from skin for supraspinatus, common wrist and finger extensors, patellar and Achilles tendons: ultrasonography study of healthy subjects. Physiotherapy. 2003;89(6):375–83.
Harris M, Schultz A, Drew MK, Rio E, Adams S, Edwards S. Thirty-seven jump-landing biomechanical variables are associated with asymptomatic patellar tendon abnormality and patellar tendinopathy: a systematic review. Phys Ther Sport. 2020;45:38–55.
Hulin BT, Gabbett TJ, Caputi P, Lawson DW, Sampson JA. Low chronic workload and the acute: chronic workload ratio are more predictive of injury than between-match recovery time: a two-season prospective cohort study in elite rugby league players. Br J Sports Med. 2016;50(16):1008–12.
Papavasiliou A, Siatras T, Bintoudi A, Milosis D, Lallas V, Sykaras E, et al. The gymnasts’ hip and groin: a magnetic resonance imaging study in asymptomatic elite athletes. Skelet Radiol. 2014;43:1071–7.
Reuter RM, Hiller WD, Ainge GR, Brown DW, Dierenfield L, Shellock FG, et al. Ironman triathletes: MRI assessment of the shoulder. Skelet Radiol. 2008;37:737–41.
Cook JL, Khan KM, Kiss ZS, Purdam CR, Griffiths L. Prospective imaging study of asymptomatic patellar tendinopathy in elite junior basketball players. J Ultrasound Med. 2000;19(7):473–9.
van Ark M, Docking S, van den Akker-Scheek I, Rudavsky A, Rio E, Zwerver J, et al. Does the adolescent patellar tendon respond to 5 days of cumulative load during a volleyball tournament? Scand J Med Sci Sports. 2016;26(2):189–96.
Visnes H, Tegnander A, Bahr R. Ultrasound characteristics of the patellar and quadriceps tendons among young elite athletes. Scand J Med Sci Sports. 2015;25(2):205–15.
Malliaras P, Purdam C, Maffulli N, Cook J. Temporal sequence of greyscale ultrasound changes and their relationship with neovascularity and pain in the patellar tendon. Br J Sports Med. 2010;44(13):944–7.
Benítez-Martínez JC, Martínez-Ramírez P, Valera-Garrido F, Casaña-Granell J, Medina-Mirapeix F. Comparison of pain measures between tendons of elite basketball players with different sonographic patterns. J Sport Rehabil. 2020;29(2):142–7.
Gisslén K, Alfredson H. Neovascularisation and pain in jumper’s knee: a prospective clinical and sonographic study in elite junior volleyball players. Br J Sports Med. 2005;39(7):423–8.
Soder RB, Mizerkowski MD, Petkowicz R, Baldisserotto M. MRI of the knee in asymptomatic adolescent swimmers: a controlled study. Br J Sports Med. 2012;46(4):268–72.
Silvis ML, Mosher TJ, Smetana BS, Chinchilli VM, Flemming DJ, Walker EA, et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med. 2011;39(4):715–21.
Walczak BE, McCulloch PC, Kang RW, Zelazny A, Tedeschi F, Cole BJ. Abnormal findings on knee magnetic resonance imaging in asymptomatic NBA players. J Knee Surg. 2008;21(1):27–33.
Deyo RA. Real help and red herrings in spinal imaging. Mass Medical Soc. 2013;368:1056–8.
Ash L, Modic M, Obuchowski N, Ross J, Brant-Zawadzki M, Grooff P. Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain. Am J Neuroradiol. 2008;29(6):1098–103.
Janssen I, Steele JR, Munro BJ, Brown N. Sex differences in neuromuscular recruitment are not related to patellar tendon load. Med Sci Sports Exerc. 2014;46(7):1410–6.
Hein T, Janssen P, Wagner-Fritz U, Haupt G, Grau S. Prospective analysis of intrinsic and extrinsic risk factors on the development of a chilles tendon pain in runners. Scand J Med Sci Sports. 2014;24(3):e201–ee12.
Crossley KM, Thancanamootoo K, Metcalf BR, Cook JL, Purdam CR, Warden SJ. Clinical features of patellar tendinopathy and their implications for rehabilitation. J Orthop Res. 2007;25(9):1164–75.
Malliaras P, Cook JL, Kent P. Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players. J Sci Med Sport. 2006;9(4):304–9.
Ranger TA, Wong AM, Cook JL, Gaida JE. Is there an association between tendinopathy and diabetes mellitus? A systematic review with meta-analysis. Br J Sports Med. 2016;50(16):982–9.
Gaida JE, Ashe MC, Bass SL, Cook JL. Is adiposity an under-recognized risk factor for tendinopathy? A systematic review. Arthritis Care Res: Off J Am Coll Rheumatol. 2009;61(6):840–9.
Mahieu NN, Witvrouw E, Stevens V, Van Tiggelen D, Roget P. Intrinsic risk factors for the development of achilles tendon overuse injury: a prospective study. Am J Sports Med. 2006;34(2):226–35.
September AV, Schwellnus MP, Collins M. Tendon and ligament injuries: the genetic component. Br J Sports Med. 2007;41(4):241–6.
Reinking MF, Austin TM, Hayes AM. A survey of exercise-related leg pain in community runners. Int J Sports Phys Ther. 2013;8(3):269.
Santi G, Pietrantoni L. Psychology of sport injury rehabilitation: a review of models and interventions. J Hum Sport Exerc. 2013;8(4):1029–44.
Milewski MD, Skaggs DL, Bishop GA, Pace JL, Ibrahim DA, Wren TA, et al. Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. J Pediatr Orthop. 2014;34(2):129–33.
Laux P, Krumm B, Diers M, Flor H. Recovery–stress balance and injury risk in professional football players: a prospective study. J Sports Sci. 2015;33(20):2140–8.
Alizadeh MH, Pashabadi A, Hosseini SM, Shahbazi M. Injury occurrence and psychological risk factors in junior football players. World J Sport Sci. 2012;6(4):401–5.
Gellhorn AC, Carlson MJ. Inter-rater, intra-rater, and inter-machine reliability of quantitative ultrasound measurements of the patellar tendon. Ultrasound Med Biol. 2013;39(5):791–6.
Mc Auliffe S, OSullivan K, Mc CK. A systematic review to investigate the reliability of ultrasound imaging in measuring tendon thickness. Br J Sports Med. 2014;48(7):635–6.
Petrofsky JS. Resting blood flow in the skin: does it exist, and what is the influence of temperature, aging, and diabetes? J Diabetes Sci Technol. 2012;6(3):674–85.
Acknowledgements
Not applicable.
Funding
No funding sources.
Author information
Authors and Affiliations
Contributions
FS contributed to the original idea and protocol, the conception of the work, conducting the study, revising the draft, and editing of the manuscript. AA contributed to the conception of the work and supervision of the manuscript. AS revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No human subject was involved so it is not applicable.
Consent for publication
“Not applicable”.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sharif, F., Ahmad, A. & Shabbir, A. Does the ultrasound imaging predict lower limb tendinopathy in athletes: a systematic review. BMC Med Imaging 23, 217 (2023). https://doi.org/10.1186/s12880-023-01181-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-023-01181-5