Abstract
Background
Current sequencing technologies have provided for a more comprehensive genome-wide assessment and have increased genotyping accuracy of rare variants. Scan statistic approaches have previously been adapted to genetic sequencing data. Unlike currently-employed association tests, scan-statistic-based approaches can both localize clusters of disease-related variants and, subsequently, examine the phenotype association within the resulting cluster. In this study, we present a novel Quantitative Phenotype Scan Statistic (QPSS) that extends an approach for dichotomous phenotypes to continuous outcomes in order to identify genomic regions where rare quantitative-phenotype-associated variants cluster.
Results
We demonstrate the performance and practicality of QPSS with extensive simulations and an application to a whole-genome sequencing (WGS) study of cerebrospinal fluid (CSF) biomarkers from the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Using QPSS, we identify regions of rare variant enrichment associated with levels of AD-related proteins, CSF Aβ1–42 and p-tau181P.
Conclusions
QPSS is implemented under the assumption that causal variants within a window have the same direction of effect. Typical self-contained tests employ a null hypothesis of no association between the target variant set and the phenotype. Therefore, an advantage of the proposed competitive test is that it is possible to refine a known region of interest to localize disease-associated clusters. The definition of clusters can be easily adapted based on variant function or annotation.
Similar content being viewed by others
Background
Rare variants have become a focus in the recent past. Although genome-wide association studies (GWAS) have been successful in interrogating genetic variants for association with disease, GWAS are performed under the “common disease – common variant” hypothesis positing that common traits are caused by the combination of common variants with a small to moderate effect [1, 2]. GWAS rely on genotyping an array of single nucleotide polymorphisms (SNPs) then imputing ungenotyped variants based on local linkage disequilibrium (LD) derived from reference population haplotypes. Imputation approaches have continually improved and are quite accurate for common variants [3, 4] but are not as reliable for rare variants [5]. Therefore, imputed rare variants are often removed from GWAS analysis. Although GWAS for common variants have revealed numerous susceptibility variants for common diseases, much of the genetic contribution to common diseases remains unexplained [6, 7]. A frequently hypothesized culprit of this missing heritability is the role of rare variants [7, 8].
Next-generation sequencing technologies have allowed for more comprehensive genome-wide approaches, enabling accurate genotyping of rare variants (often defined as a variant with minor allele frequency (MAF) < 1–5%). Consequently, whole-exome sequencing (WES) and whole-genome sequencing (WGS) are ideal approaches to identify novel genes and rare variants associated with complex traits.
Traditional single-variant-based association tests are underpowered to detect rare variant associations unless either or both of the sample size and the effect size are very large [9]. Instead of testing single variants individually, more powerful and computationally efficient approaches for aggregating the effects of rare variants have become the standard for association testing. Many such approaches for testing association between rare variants within a pre-specified region and a disease have been proposed. Burden and variance component tests are two of the most common classes of rare variant analysis methods. Burden tests collapse rare variant effects from a specified region (e.g., gene) using a weighted average of variant counts, whereas variance component tests like the sequence kernel association test (SKAT) use the variance of effect sizes to examine association [10, 11]. Burden tests are more powerful than the SKAT when most of the variants are causal and have the same direction of effect. On the other hand, SKAT is powerful when both risk and protective variants are mixed and when a small proportion of variants are causal [10]. The sheer number of published rare variant methods makes systematic evaluation of relative performance across a spectrum of realistic scenarios challenging [12].
A scan-statistic-based test was introduced into human genetics by Hoh et al. [13] and later adapted to find a window in which rare disease-associated risk variants cluster [1]. The underlying premise is that variants within a functional protein-coding domain may be located in close proximity and may play complementary roles in the genetic mechanisms of a disease. Unlike association tests or other cluster detection analyses, the scan-statistic-based test that we extend in this work can both detect the location of clusters and test for association [14]. Here, the null hypothesis is that rare variants within a certain genetic region/scan window are as likely to confer disease risk as are those outside the window. This approach is generally powerful when there are clusters of disease-related variants with the same direction of association within a selected region/window [14].
In this study, we propose the Quantitative Phenotype Scan Statistic (QPSS), expanding Ionita-Laza et al’s scan-statistic from dichotomized responses to continuous outcomes by way of a normal probability model ([15]; Supplementary Method 1). We then apply QPSS to WGS data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) with continuous outcomes to identify clusters harboring rare variants associated with Alzheimer’s disease-linked cerebrospinal fluid (CSF) biomarkers.
Implementation
QPSS: quantitative phenotype scan statistic
Assume a study comprising n subjects, each with a continuous outcome of interest yi (i = 1, …, n). Let mG denote the total number of rare variants in a genetic region of interest G, where “rare” is defined by a specified cutoff value (e.g., MAF < 5%). Variants are sorted by physical position in ascending order. We set a sub-window W containing mW variants (mW < mG) within the genetic region G (i. e., W ⊆ G). Let nG be the number of individuals who carry at least one rare variant within the genetic region G (nG ≤ N). Of the nG rare variants carriers, \( {n}_{W_{+}}\left(\le {n}_G\right) \) carry a rare variant in the window W. Similarly, \( {n}_{W_{-}}\Big(={n}_G-{n}_{W_{+}} \)) do not carry a rare variant within window W. We can then partition the maximum likelihood estimate of the trait variance \( {\sigma}_W^2 \) among the nG rare variant carriers as
where
Under the null hypothesis that variants within the sub-window W are equally as likely to correlate with the disease outcome that those outside the window (but still within the region of interest G), the outcome variance should be similar between the \( {n}_{W_{-}} \) and \( {n}_{W_{+}} \) subjects so that the pooled variance would equal the overall variance, that is,
where \( {\sigma}_0^2 \) is the variance under the null hypothesis and its maximum likelihood estimate is
Under the alternative hypothesis, we expect the outcome values of the \( {n}_{W_{+}} \) subjects carrying a rare variant within W to be more similar to each other than to the rare variant carrying subjects whose variants are all outside W, that is \( {\sigma}_W^2<{\sigma}_0^2 \). Using these definitions, we calculate the following log likelihood ratio test statistic
for the window W (see Supplementary Method 1 for full details).
In order to distinguish between risk and protective clusters, we can adjust the log likelihood ratio test statistic based on the estimated effect direction. For instance, Kulldorff et al. suggested the simple indicator function \( I\left({\hat{\mu}}_{W_{+}}>{\hat{\mu}}_{W_{-}}\right) \) for risk clusters with high values of the outcome, which effectively removes from consideration any window W where the trait mean among subjects in W+ is less that that for subjects in W−. Similarly, \( I\left({\hat{\mu}}_{W_{+}}<{\hat{\mu}}_{W_{-}}\right) \) can be used for protective clusters with low values of the outcome [15]. To evaluate both positive and negative associations of clusters with the phenotype simultaneously, we can employ the sign function \( \mathit{\operatorname{sgn}}\left({\hat{\mu}}_{W_{+}}-{\hat{\mu}}_{W_{-}}\right) \), that is, an indicator of +1 for \( {\hat{\mu}}_{W_{+}}>{\hat{\mu}}_{W_{-}} \) and −1 for \( {\hat{\mu}}_{W_{+}}<{\hat{\mu}}_{W_{-}} \). The window harboring rare variants associated with a phenotype can be identified as the window that maximizes the log likelihood ratio, i.e.,
The null distribution of the test statistic is unknown; thus, p-values are calculated by a permutation approach [16]. To minimize computation time, we applied a GPD approximation [17] (see Supplementary Method 2 for full details) for estimating p-value of permutation test in the application study.
Simulation study
Genotype data
We generated 10,000 haplotypes of a 1 Mb genomic region from a European population as implemented in the software Cosi2 (https://software.broadinstitute.org/mpg/cosi2/) [18]. We randomly extracted haplotype pairs to create genotypes for sample sizes (n) of 500 and 1000. We then removed common variants (MAF > 0.05) and singletons.
Phenotype data
We considered three cluster sizes: small (200 basepairs (bp)) and moderate (500 bp), both of which have consecutively located disease-associated rare variants; and large (2 kb) where 20% of rare variants are disease-related (thus, not consecutive). In each of the clusters, we randomly chose a start position and then generated quantitative phenotypes from the model
where βj = c|log10MAFj|, mC is the number of variants in the cluster, gij is the additively-coded genotype (gij = 0, 1, 2 according to the minor allele count) for the i th individual at the j th variant (j = 1, …, mC), and εi is the error for the i th individual generated from a standard normal (i.e., εi ∼ N(0, 1)). We set c = 0.2, c = 0.4 and c = 0.6 for the empirical power simulations, and c = 0 for the type I error simulations. For each scenario, we generated 1000 simulation replicates.
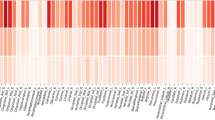
Specification of the overall genetic region G and the subwindows W are flexible. To find a window that maximizes the log likelihood ratio, we thus employed a sliding window approach considering several different window sizes. We used windows sizes of 5 k, 2 k, 1 k, and 500 bp, and then slid each of those windows by half its respective size (i.e., by 2.5 k, 1 k, 500, and 250 bp). These scenarios are depicted both graphically and via a table (Fig. 1 and Supplementary Table 1). To provide a better sense of the effect sizes examined, the means of the simulated phenotypes (Supplementary Figure 1) and the estimates of genetic heritability (Supplementary Figure 2) are shown for each scenario.
Results
Type I error simulation results
The empirical type I error rates were calculated as the proportion of p-values less than or equal to the corresponding Bonferroni-adjusted significance level (α∗ = α/ the number of examined sliding windows in the region G) for the window in which \( \ln {\hat{LR}}_W \) was maximized. As shown in Table 1, the type I error rates were acceptable in all scenarios.
Power simulation results
Power was calculated as the proportion of simulation replicates with an empirical p-value (corresponding to the window with maximum value of \( \ln {\hat{LR}}_W \)) reaching Bonferroni-adjusted significance. Supplementary Figures 3 to 20 show the means of \( \ln {\hat{LR}}_W \) (over the 1000 simulation replicates) in each of the windows. Supplementary Tables 2 and 3 show the number of the targeted sliding windows (those containing true disease-related variants) with achieved the maximum value of \( \ln {\hat{LR}}_W \). Figure 2 shows the empirical powers for the targeted sliding windows under the alternative hypothesis in each scenario when all disease-related variants had positive associations with the phenotype.
When the effect size and the cluster size were small (c = 0.2 and cluster size = 200 bp), the proposed QPSS had low power in all scanning windows. In other scenarios, power depends on the scanning window size relative to the cluster size. When the scanning window is too large compared to the cluster size, power can decrease considerably. On the other hand, when the scanning window size is smaller than the size of the variant-containing cluster, multiple sliding windows can overlap the outcome-related cluster; however, it was hard to identify the window most likely to harbor risk variants. Not surprisingly, the best scenario was when the scanning window is of similar length to the true cluster.
Application to Alzheimer’s Disease Neuroimaging Initiative (ADNI)
Data used in the preparation of this article were obtained from the ADNI database (adni.loni.usc.edu). The ADNI was launched in 2003 as a public-private partnership, led by Principal Investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of mild cognitive impairment (MCI) and early AD. We retrieved baseline data on CSF amyloid β 1–42 (Aβ1–42) and phosphorylated tau at the threonine 181 (p-tau181P) levels measured at the ADNI Biomarker Core laboratory at the University of Pennsylvania Medical Center [19, 20] and single nucleotide variants (SNVs) from WGS data sequenced on the Illumina HiSeq2000 using paired-end 100-bp reads. We used data from 538 subjects aged 65 years or older at the time when the baseline CSF sample was drawn.
The apolipoprotein E (APOE) gene, located on chromosome 19q13.32, is involved in Aβ1–42 deposition [21], and the microtubule-associated protein tau (MAPT) gene, located on chromosome 17q21.31, encodes tau protein. Thus, we first examined the associations of genes on chromosome 19 with CSF Aβ1–42 levels and of genes on chromosome 17 with CSF p-tau181P levels using common gene-based association tests including the burden test, SKAT, and SKAT-O. The start and end gene positions on hg19 assembly of each gene were obtained in the UCSC Genome Browser (https://genome.ucsc.edu/) [22]. Several genes close to APOE (19: 45,409,039 – 45,412,650) had significant associations (Bonferroni corrected for 1639 genes) with CSF Aβ1–42 levels: PVRL2 (19: 45,349,393 – 45,392,485; SKAT p = 1.87 × 10− 5); TOMM40 (19: 45,394,477 – 45,406,946; SKAT p = 2.81 × 10− 9 and SKAT-O p = 1.97 × 10− 8); APOC1 (19:45,417,921 – 45,422,606; SKAT p = 1.16 × 10− 8 and SKAT-O p = 3.47 × 10− 8) (Supplementary Figure 21). No genes that reached Bonferroni-adjusted significance in the gene-based association with CSF p-tau181P (Supplementary Figure 22).
Next, we evaluated whether QPSS detected clusters on chromosomes 19 and 17 associated with CSF Aβ1–42 and p-tau181P levels, respectively. We set the APOE and MAPT gene lengths ±10 Mbp as the large genetic region G, window sizes 5 k/2 k/1 k/500 bp and sliding length 2.5 k/1 k/500/250 bp. All analyses were restricted to rare variants (MAF < 0.05). The total numbers of windows evaluated were m = 133,687 in the APOE region and m = 126,623 in the MAPT region; therefore the Bonferroni-corrected significance levels were α = 0.05/133,687 ≈ 3.74 × 10−7 and α = 0.05/126,623 ≈ 3.95 × 10−7, respectively.
Figure 3 and Supplementary Figure 23 show the \( \ln {\hat{LR}}_W \) values and p-values for windows in the associations of rare variants in the APOE region ±10 Mbp with CSF Aβ1–42 levels. The positive \( \ln {\hat{LR}}_W \) values represent \( {\hat{\mu}}_{W_{+}}>{\hat{\mu}}_{W_{-}} \) for clusters associated with high values of the outcome and the negative one for \( {\hat{\mu}}_{W_{+}}<{\hat{\mu}}_{W_{-}} \) for clusters associated with low values of the outcome. Windows that maximized \( \ln {\hat{LR}}_W \) and resulted in a significant permutation-based p-values were 45,403,046 – 45,405,045 in TOMM40 for the scanning window size of 2 kbp (p = 4.50 × 10− 9), 45,404,046 – 45,405,045 in TOMM40 for the scanning window size of 1 kbp (p = 8.76 × 10− 9), and 45,412,796 – 45,413,295 in the intergenic region 150 bp away from APOE 3′ UTR (p = 5.14 × 10− 9). For the associations with CSF p-tau181P, significant windows were 36,636,821 – 36,638,820 for the scanning window size of 2 kbp (p = 1.94 × 10− 8) and 36,637,321 – 36,638,320 the scanning window size of 1 kbp (p = 9.13 × 10− 9), both of which were in ARHGAP23 (Fig. 4 and Supplementary Figure 24).
Plots of \( \ln {\hat{LR}}_W \) for the associations between rare variants around APOE (± 10 M bp) located on chromosome 19 and log-transformed CSF amyloid β 1–42 levels in ADNI. Positive \( \ln {\hat{LR}}_W \) represents test statistics for \( {\hat{\mu}}_{W_{+}}>{\hat{\mu}}_{W_{-}} \) and negatives for \( {\hat{\mu}}_{W_{+}}<{\hat{\mu}}_{W_{-}} \)
Plots of \( \ln {\hat{LR}}_W \) for the associations between rare variants around MAPT (± 10 M bp) located on chromosome 17 and log-transformed CSF phosphorylated tau levels in ADNI. Positive \( \ln {\hat{LR}}_W \) represents test statistics for \( {\hat{\mu}}_{W_{+}}>{\hat{\mu}}_{W_{-}} \) and negatives for \( {\hat{\mu}}_{W_{+}}<{\hat{\mu}}_{W_{-}} \)
Discussion
We showed the performance and practicality of QPSS with extensive simulations and in application to a WGS dataset with CSF biomarkers from ADNI. We identified regions enriched with rare variants in TOMM40 and the surrounding intergenic region that were associated with decreased CSF Aβ1–42 levels and a cluster in ARHGAP23 with rare variants associated with increased CSF p-tau181P levels. The window 45,403,046 – 45,405,045 in TOMM40 and the window 45,412,796 – 45,413,295 in the intergenic region contained 13 rare variants and two rare variants, respectively. These windows successfully captured three top loci associated with decreased CSF Aβ1–42 levels (Supplementary Tables 4 and 5 and Supplementary Figure 25). Unlike TOMM40, ARHGAP23 went undetected using commonly-used gene-based tests (i.e., burden test, SKAT, and SKAT-O). Using a 1 k bp window (and corresponding 500 bp slide), the window 36,637,321 – 36,638,320 in ARHGAP23 was the most likely to harbor a cluster of variants associated increased CSF p-tau181P levels, which was significant after Bonferroni correction (p = 9.13 × 10− 9 using generalized Pareto distribution (GPD) approximation). There were three rare variants in the implicated window in ARHGAP23; each minor allele associated with increased CSF p-tau181P levels (Supplementary Table 6). The association between ARHGAP23 and CSF p-tau181P levels is novel and warrants attempts at replication in future work. Notably, ARHGAP23 is located ~ 7 Mb from the MAPT gene suggesting that this is an independent signal.
Conclusions
QPSS is implemented under the assumption, similar to burden tests, that causal variants within a window have the same direction of effect. However, there is a difference in the nature of the tested hypotheses between these methods. The null hypothesis of the competitive tests, like our proposed method, is that associations between the phenotype and the set of variants within a specified window are the same as those outside the window. Typical self-contained tests employ a null hypothesis of no association between the target variant set and the phenotype. Therefore, an advantage of the proposed competitive test is that it is possible to refine a known region of interest to localize disease-associated clusters. Note that the definition of clusters can be easily adapted based on variant function or annotation. A limitation of these approaches is the possibility of population structure confounding as the proposed method does not take into account covariate adjustment. We aim to address this limitation in future work.
Availability and requirements
Project name: Quantitative Phenotype Scan Statistic (QPSS).
Project home page: https://github.com/kyka222/QPSS
Operating system(s): Platform independent.
Programming language: Python2.
Other requirements: PLINK 1.9, R 2.10 or higher, R package goft.
License: Free academic research use.
Any restrictions to use by non-academics: License required.
Availability of data and materials
Cerebrospinal fluid (CSF) biomarkers and whole genome sequences data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) were downloaded from the Image & Data Archive at the Laboratory of Neuro Imaging (https://ida.loni.usc.edu/login.jsp). We have received administrative approval for access to the ADNI database.
Abbreviations
- ADNI:
-
Alzheimer’s Disease Neuroimaging Initiative
- CSF:
-
Cerebrospinal fluid
- GPD:
-
Generalized Pareto distribution
- GWAS:
-
Genome-wide association studies
- LD:
-
Linkage disequilibrium
- MAF:
-
Minor allele frequency
- MCI:
-
Cognitive impairment
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- QPSS:
-
Quantitative phenotype scan statistic
- SKAT:
-
Sequence kernel association test
- SNPs:
-
Single nucleotide polymorphisms
- SNVs:
-
Single nucleotide variants
- WES:
-
Whole-exome sequencing
- WGS:
-
Whole-genome sequencing
References
Ionita-Laza I, Makarov V. ARRA autism sequencing Consortium, Buxbaum JD: scan-statistic approach identifies clusters of rare disease variants in LRP2, a gene linked and associated with autism spectrum disorders, in three datasets. Am J Hum Genet. 2012;90(6):1002–13.
Gibson G. Rare and common variants: twenty arguments. Nat Rev Genet. 2012;13(2):135–45.
Howie B, Fuchsberger C, Stephens M, Marchini J, Abecasis GR. Fast and accurate genotype imputation in genome-wide association studies through pre-phasing. Nat Genet. 2012;44(8):955–9.
van Leeuwen EM, Kanterakis A, Deelen P, Kattenberg MV, C, Slagboom PE, de Bakker PI, Wijmenga C, Swertz MA, Boomsma DI et al: Genome of the Netherlands population-specific genotype imputations using minimac or IMPUTE2. Nat Protoc 2015, 10(9):1285–1296.
1000 Genomes Project Consortium, Abecasis GR, Altshuler D, Auton A, Brooks LD, Durbin RM, Gibbs RA, Hurles ME, McVean GA: A map of human genome variation from population-scale sequencing. Nature 2010, 467(7319):1061–1073.
Maher B. Personal genomes: the case of the missing heritability. Nature. 2008;456(7218):18–21.
Eichler EE, Flint J, Gibson G, Kong A, Leal SM, Moore JH, Nadeau JH. Missing heritability and strategies for finding the underlying causes of complex disease. Nat Rev Genet. 2010;11(6):446–50.
Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, McCarthy MI, Ramos EM, Cardon LR, Chakravarti A, et al. Finding the missing heritability of complex diseases. Nature. 2009;461(7265):747–53.
Asimit J, Zeggini E. Rare variant association analysis methods for complex traits. Annu Rev Genet. 2010;44:293–308.
Lee S, Emond MJ, Bamshad MJ, Barnes KC, Rieder MJ, Nickerson DA, Team NGESP-ELP, Christiani DC, Wurfel MM, Lin X. Optimal unified approach for rare-variant association testing with application to small-sample case-control whole-exome sequencing studies. Am J Hum Genet. 2012;91(2):224–37.
Lee S, Wu MC, Lin X. Optimal tests for rare variant effects in sequencing association studies. Biostatistics. 2012;13(4):762–75.
Bomba L, Walter K, Soranzo N. The impact of rare and low-frequency genetic variants in common disease. Genome Biol. 2017;18(1):77.
Hoh J, Ott J. Scan statistics to scan markers for susceptibility genes. Proc Natl Acad Sci U S A. 2000;97(17):9615–7.
Ionita-Laza I, Makarov V, Consortium AAS, Buxbaum JD. Scan-statistic approach identifies clusters of rare disease variants in LRP2, a gene linked and associated with autism spectrum disorders, in three datasets. Am J Hum Genet. 2012;90(6):1002–13.
Kulldorff M, Huang L, Konty K. A scan statistic for continuous data based on the normal probability model. Int J Health Geogr. 2009;8:58.
Phipson B, Smyth GK. Permutation P-values should never be zero: calculating exact P-values when permutations are randomly drawn. Stat Appl Genet Mol Biol. 2010;9(1) Article39.
Knijnenburg TA, Wessels LF, Reinders MJ, Shmulevich I. Fewer permutations, more accurate P-values. Bioinformatics. 2009;25(12):i161–8.
Shlyakhter I, Sabeti PC, Schaffner SF. Cosi2: an efficient simulator of exact and approximate coalescent with selection. Bioinformatics. 2014;30(23):3427–9.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Figurski M, Coart E, Blennow K, Soares H, Simon AJ, Lewczuk P, Dean RA, et al. Qualification of the analytical and clinical performance of CSF biomarker analyses in ADNI. Acta Neuropathol. 2011;121(5):597–609.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Clark CM, Aisen PS, Petersen RC, Blennow K, Soares H, Simon A, Lewczuk P, et al. Cerebrospinal fluid biomarker signature in Alzheimer's disease neuroimaging initiative subjects. Ann Neurol. 2009;65(4):403–13.
Polvikoski T, Sulkava R, Haltia M, Kainulainen K, Vuorio A, Verkkoniemi A, Niinisto L, Halonen P, Kontula K. Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein. N Engl J Med. 1995;333(19):1242–7.
Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, Haussler D. The human genome browser at UCSC. Genome Res. 2002;12(6):996–1006.
Acknowledgements
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf. Data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Funding
This work was supported by the National Cell Repository for Alzheimer’s Disease (U24 AG21886), the National Institute on Aging (R56 AG057191, R01 AG054060, the UK-ADC P30 AG028383, and R01 AG057187) and the National Science Foundation (ACI-1626364). Funding bodies did not play any role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YK and DWF conceived the study. YK carried out the main programming work, performed the analysis, and drafted the manuscript. DWF interpreted the data and revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Supplementary Method 1
. Scan statistics for the normal probability model developed by Kulldorff et al. [1]. Supplementary Method 2. Computing empirical p-values based on permutation test and approximation by a generalized Pareto distribution described by Knijnenburg et al. [2]. Table S1. Simulation scenario for type I error and power evaluations. Table S2. Frequency of the number of targeted sliding windows that produced the maximum value of \( \ln {\hat{LR}}_W \) (n = 500). Table S3. Frequency of the number of targeted sliding windows that produced the maximum value of \( \ln {\hat{LR}}_W \) (n = 1000). Table S4. Single variant associations on the significant window of TOMM40 (45,403,046 – 45,405,045) with log-transformed cerebrospinal fluid amyloid β 1–42 levels in ADNI. Table S5. Single variant associations on the significant window of intergenic region (45,412,796 – 45,413,295) with log-transformed cerebrospinal fluid amyloid β 1–42 levels in ADNI. Table S6. Single variant associations on the significant window of ARHGAP23 (36,637,321 – 36,638,320) with log-transformed cerebrospinal fluid phosphorylated tau levels in ADNI. Figure S1. Mean of continuous phenotype y in each scenario. Figure S2. Estimate of heritability in each scenario. Figure S3. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 200 bp, and effect size c = 0.2. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S4. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 200 bp, and effect size c = 0.4. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S5. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 200 bp, and effect size c = 0.6. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S6. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 500 bp, and effect size c = 0.2. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S7. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 500 bp, and effect size c = 0.4. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S8. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 500 bp, and effect size c = 0.6. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S9. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 2 kbp (containing 20% disease-related variants), and effect size c = 0.2. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S10. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 2 kbp (containing 20% disease-related variants), and effect size c = 0.4. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S11. Mean of \( \ln {\hat{LR}}_W \) for n = 500, cluster size = 2 kbp (containing 20% disease-related variants), and effect size c = 0.6. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S12. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 200 bp, and effect size c = 0.2. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S13. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 200 bp, and effect size c = 0.4. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S14. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 200 bp, and effect size c = 0.6. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S15. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 500 bp, and effect size c = 0.2. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S16. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 500 bp, and effect size c = 0.4. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S17. Mean \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 500 bp, and effect size c = 0.6. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S18. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 2 kbp (containing 20% disease-related variants), and effect size c = 0.2. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S19. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 2 kbp (containing 20% disease-related variants), and effect size c = 0.4. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S20. Mean of \( \ln {\hat{LR}}_W \) for n = 1000, cluster size = 2 kbp (containing 20% disease-related variants), and effect size c = 0.6. Each point represents the center position of each of the windows, and the blue vertical line indicates the center of the cluster position. Figure S21. Gene-based associations between rare variants located on chromosome 19 and log-transformed CSF amyloid β 1–42 levels in ADNI using the burden test, SKAT, and SKAT-O. The red horizontal line indicates the significance level with Bonferroni correction (α = 0.05/the number of genes on chromosome 19). Figure S22. Gene-based associations between rare variants located on chromosome 17 and log-transformed CSF phosphorylated tau levels in ADNI using the burden test, SKAT, and SKAT-O. The red horizontal line indicates the significance level with Bonferroni correction (α = 0.05/the number of genes on chromosome 17). Figure S23. QPSS p-values computed by the permutation with generalized Pareto distribution approximation for the associations between rare variants around APOE (± 10 Mbp) located on chromosome 19 and log-transformed CSF amyloid β 1-42 in ADNI. Figure S24. QPSS p-values computed by the permutation with generalized Pareto distribution approximation for the associations between rare variants around MAPT (± 10 Mbp) located on chromosome 17 and log-transformed CSF phosphorylated tau levels in ADNI. Figure S25. Single variant associations between rare variants around APOE (± 10 Mbp) located on chromosome 19 and log-transformed CSF amyloid β 1- 42 in ADNI.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Katsumata, Y., Fardo, D.W. Quantitative phenotype scan statistic (QPSS) reveals rare variant associations with Alzheimer’s disease endophenotypes. BMC Med Genet 21, 106 (2020). https://doi.org/10.1186/s12881-020-01046-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12881-020-01046-6