Abstract
Background
Post-stroke delirium is a common problem in the care of stroke patients, and is associated with longer hospitalization, high short-term mortality, and an increased need for long-term care. Although post-stroke delirium occurs in approximately 10 ~ 30% of patients, little is known about the risk factors for post-stroke delirium in patients who experience acute stroke.
Methods
A total of 576 consecutive patients who experienced ischemic stroke (mean age, 65.2 years; range, 23–93 years) were screened for delirium over a 2-year period in an acute stroke care unit of a tertiary referral hospital. We screened for delirium using the Confusion Assessment Method. Once delirium was suspected, we evaluated the symptoms using the Korean Version of the Delirium Rating Scale-Revised-98. Neurological deficits were assessed using the National Institutes of Health Stroke Scale at admission and discharge, and functional ability was assessed using the Barthel Index and modified Rankin Scale at discharge and 3 months after discharge.
Results
Thirty-eight (6.7%) patients with stroke developed delirium during admission to the acute stroke care unit. Patients with delirium were significantly older (70.6 vs. 64.9 years of age, P = .001) and smoked cigarettes more frequently (40% vs. 24%, P = .033) than patients without delirium. In terms of clinical features, the delirium group experienced a significantly higher rate of major hemispheric stroke (55% vs. 26%, P < .001), exhibited poorer functional performance at discharge and 3 months after discharge, and stayed in hospital significantly longer. Independent risk factors for delirium were older age, history of cigarette smoking, and major hemispheric stroke.
Conclusion
Abrupt cessation of cigarette smoking may be a risk factor for post-stroke delirium in ischemic stroke patients. The development of delirium after stroke is associated with worse outcome and longer hospitalization.
Similar content being viewed by others
Background
Delirium is an acute confusional state characterized by decreased attention, an altered level of consciousness, and decreased cognitive function including impairment of memory and thought processes [1]. Substantial numbers of delirium cases are caused by systemic inflammation due to an infection or surgery in patients with predisposing risk factors, such as an old age, head trauma, stroke, or underlying dementia [2]. Delirium occurs in 10 ~ 48% of patients during admission and results in poorer functional outcome(s), lower quality of life, and longer hospitalization [3, 4]. Although the exact pathophysiology of delirium is not well understood, decreased acetylcholine and increased dopamine levels are believed to be important factors in this process [5].
Ischemic stroke is caused by an occlusion of the cerebral arteries, which may lead to neurological deficit. Presently, admission to a dedicated stroke care unit is the standard treatment for acute stroke care, and is associated with a long-term benefit in neurological and functional outcomes [6]. However, admission to such an unfamiliar environment for stroke patients and an abrupt cessation of cigarette and alcohol use could induce delirium [7]. Few studies, however, have investigated these variables as risk factors for post-stroke delirium.
The present study evaluated retrospective data from ischemic stroke patients in an acute stroke care unit over a 2-year period to identify the risk factors for post-stroke delirium.
Methods
Subjects and delirium screening
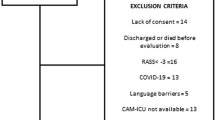
We screened a total of 589 consecutive ischemic stroke patients who were admitted to an acute stroke unit over a 2-year period. Of these patients, 13 were transferred out of the unit within 48 h and, thus, were excluded from further study, yielding a total of 576 patients who were enrolled in the present retrospective study. All patients were evaluated using brain computed tomography (CT) and magnetic resonance imaging (MRI); 28 patients showed negative results after brain magnetic resonance diffusion-weighted imaging.
Delirium was screened daily during admission using the Confusion Assessment Method (CAM) [8]. The diagnosis of delirium was based on the following four features: (i) acute onset and a fluctuating course; (ii) inattention; (iii) disorganized thinking; (iv) an altered level of consciousness. Once delirium was suspected, we evaluated the symptoms using the Korean Version of the Delirium Rating Scale-Revised-98 (K-DRS-R-98), which quantifies multiple parameters, such as the sleep-wake cycle, perception, hallucinations, delusions, mood, language, thought process, psychomotor behavior, orientation, attention, imprinting, short-term memory, and visuospatial orientation [9]. All items were scored on a 4-point scale, resulting in a total score range of 0 to 39.
Definition of variables
We divided all stroke patients into 5 groups based on the modified Oxfordshire Community Stroke Project criteria, which included major hemispheric, minor hemispheric (subcortical), lacunar, brainstem/cerebellar, and non-classified syndromes [10]. We recorded right, left, and bilateral hemispheric involvement. Cigarette smoking was defined as current smoking of any number of cigarettes. Daily alcohol use was defined as consuming more than 3 standard drinks per day. Infection during admission to the stroke unit was defined as a body temperature >38.5 °C [11]. Metabolic derangement was defined as follows: sodium <130 or >150 mmol/L; glucose <2.8 or >14 mmol/L; an estimated glomerular filtration rate <30 mL/min; calcium <2 or >2.75 mmol/L; and oxygen saturation <90% [11]. Neurological deficits were assessed using the National Institutes of Health Stroke Scale (NIHSS) at admission and discharge, and functional ability was assessed using the Barthel Index (BI) and modified Rankin Scale (mRS) at discharge and 3 months after discharge. Follow-up data at 3 months after discharge were available for 414 patients.
Statistics
The Student’s t-test and chi-square test were used to compare differences between patients with and without delirium. Logistic regression analysis was performed with delirium occurrence as the dependent variable to analyze independent risk factors and calculate odds ratios (OR). All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 576 ischemic stroke patients were investigated. The characteristics of these patients are summarized in Table 1. Among them, 368 patients (63.9%) were male and 25% (n = 144) were cigarette smokers. The average NIHSS at admission was 5.5 (range 0–29). The comparison between patients with and without post-stroke delirium is shown in Table 2. Thirty-eight of 576 patients (6.7%) developed delirium during admission to the acute stroke care unit. Compared with patients without delirium, patients with delirium were significantly older (70.6 vs. 64.9 years of age, P = .001) and smoked cigarettes more frequently (40% vs. 24%, P = .033). In terms of clinical features, the delirium group had a significantly higher rate of major hemispheric stroke (55% vs. 26%, P < .001), and showed a worse modified Rankin score at discharge (2.5 vs. 1.7, P = 0.01) and at 3 months after discharge (2.3 vs. 1.4, P = .018) (Fig. 1). The length of hospitalization was longer in patients with delirium (13.3 days vs. 10.7 days, P = .049). The univariate and multivariate logistic regression analyses are shown in Table 3. In the multivariate analysis of risk factors for delirium, independent risk factors for delirium were older age (OR = 1.05), cigarette smoking (OR = 2.8), and major hemispheric stroke (OR = 4.8) after adjustment for age, sex and alcohol use.
Discussion
To our knowledge, the present study was the first to identify cigarette smoking as a risk factor for post-stroke delirium. Our 2-year retrospective study suggests that older age, history of cigarette smoking, and major hemispheric stroke are independent risk factors for post-stroke delirium, which is associated with a poorer functional outcome and longer hospitalization.
Cigarette smoking was an independent risk factor for post-stroke delirium after adjustment for age, sex, and alcohol use. Although the exact mechanism of the contribution of cigarette smoking to delirium has yet to be elucidated, abrupt cessation of smoking and withdrawal of nicotinic stimulation has been postulated [7]. A recent systematic review suggested that current research evidence is insufficient to determine whether cigarette smoking is a risk factor for delirium [12]. However, there have been no systematic reviews to investigate post-stroke delirium cases with a relatively higher incidence of smoking. In contrast to cigarette smoking, alcohol consumption was not associated with delirium. This finding was consistent with previous studies that also reported no relationship [13, 14]. In clinical practice, alcohol withdrawal syndromes are usually considered in the management of patients with stroke, but cigarette withdrawal is not. Further studies are needed to ascertain the relationship between cigarette smoking, its proper management, such as the nicotine patch, and post-stroke delirium.
The incidence of post-stroke delirium in the present study was 6.7%, which was lower than that reported in previous studies [4]. This lower incidence is possibly due to the younger age of the stroke cohort in the present study. The mean age of the patients in the present study was 65.2 years, which is more than 7 years younger than that reported in recently published studies [11, 13]. The lower incidence of delirium in this young study cohort corresponds well with a study that had a mean age of 57.3, and reported a delirium incidence of 13%, which was significantly lower than other studies that were conducted at that time [14]. Younger age also affected the lower incidence of dementia in this population, as we could not find a significant association between preexisting dementia and post-stroke delirium. Another explanation for the lower incidence of delirium is our inclusion of patients who experienced only ischemic stroke. Previous studies report that post-stroke delirium is more frequent in hemorrhagic stroke than ischemic stroke [14, 15].
Our results suggest that major hemispheric stroke was another independent risk factor for post-stroke delirium. This finding is also consistent with previous studies [13, 16, 17]. However, other clinical factors, such as a high initial NIHSS and right hemispheric stroke, were not identified in the present study. These variables were associated with delirium in some studies [13, 14], but not in other studies [15, 18]. In previous studies, cortical involvement and subsequent decreased cortical function, such as neglect syndrome or aphasia, were important in the pathogenesis of post-stroke delirium [14, 16, 19, 20]. Our study cohort had a higher proportion of patients who experienced lacunar stroke and, in this particular population, the high NIHSS was not the result of cortical dysfunction, but motor-sensory dysfunction, which was not associated with delirium.
Patients with delirium exhibited poorer functional outcome at discharge and experienced longer hospitalization. In addition, the long-term outcome at 3 months after discharge was worse in the delirium group. These findings are consistent with the results of many previous studies [4]. Compared with our study, a recent review and meta-analysis evaluating the outcomes of acute stroke patients with delirium reported higher inpatient mortality (OR = 4.7) and a hospital stay that was 9 days longer [4]. We did not report high inpatient mortality because the overall mortality rate was very low (0.7%) due to the number of patients with a low stroke severity. Longitudinal follow-up of these patients regarding their long-term mortality and morbidity that includes their post-stroke dementia status is needed to elucidate the long-term effect of delirium in young patients who experience low severity stroke.
The present study had limitations stemming from its retrospective design. First, pre-stroke cognition was not measured using a structured questionnaire. Instead, we included the patient history of dementia diagnosis for analysis. Second, anticholinergic medication(s) was not recorded, and the use of this medication could be associated with delirium [17]. Furthermore, a prospective studies involving a structured questionnaire to assess pre-stroke cognition and medication use, and treatment trials involving cholinesterase inhibitors [21, 22] are warranted.
Conclusions
A history of cigarette smoking before stroke may be a risk factor for post-stroke delirium, most likely due to abrupt cessation of smoking, especially in young patients who experience a low severity stroke. The development of delirium after stroke was associated with a worse outcome and longer hospitalization.
Abbreviations
- BI:
-
Barthel index
- CAM:
-
Confusion assessment method
- CT:
-
Computed tomography
- K-DRS-R-98:
-
Korean version of the delirium rating scale-revised-98
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified rankin scale
- NIHSS:
-
National institutes of health stroke scale
References
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22.
van Gool WA, van de Beek D, Eikelenboom P. Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet. 2010;375(9716):773–5.
Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097–101.
Shi Q, Presutti R, Selchen D, Saposnik G. Delirium in acute stroke: a systematic review and meta-analysis. Stroke. 2012;43(3):645–9.
Maldonado JR. Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry. 2013;21(12):1190–222.
Trialists’Collaboration SU. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013;9:CD000197.
Lucidarme O, Seguin A, Daubin C, Ramakers M, Terzi N, Beck P, Charbonneau P, du Cheyron D. Nicotine withdrawal and agitation in ventilated critically ill patients. Crit Care. 2010;14(2):R58.
Inouye SK, Van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method: a new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8.
Lee Y, Ryu J, Lee J, Kim H-J, Shin IH, Kim J-L, Trzepacz PT. Korean version of the delirium rating scale-revised-98: reliability and validity. Psychiatry Invest. 2011;8(1):30–8.
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire community stroke project--1981-86. 2. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1990;53(1):16–22.
Miu DK, Yeung JC. Incidence of post-stroke delirium and 1-year outcome. Geriatr Gerontol Int. 2013;13(1):123–9.
Hsieh SJ, Shum M, Lee AN, Hasselmark F, Gong MN. Cigarette smoking as a risk factor for delirium in hospitalized and intensive care unit patients. A systematic review. Ann Am Thorac Soc. 2013;10(5):496–503.
Oldenbeuving AW, de Kort PL, Jansen BP, Algra A, Kappelle LJ, Roks G. Delirium in the acute phase after stroke: incidence, risk factors, and outcome. Neurology. 2011;76(11):993–9.
Caeiro L, Ferro JM, Albuquerque R, Figueira ML. Delirium in the first days of acute stroke. J Neurol. 2004;251(2):171–8.
Gustafson Y, Olsson T, Eriksson S, Asplund K, Bucht G. Acute confusional states (delirium) in stroke patients. Cerebrovasc Dis. 1991;1(5):257–64.
Sheng AZ, Shen Q, Cordato D, Zhang YY, Chan Y, Kam D. Delirium within three days of stroke in a cohort of elderly patients. J Am Geriatr Soc. 2006;54(8):1192–8.
Carin-Levy G, Mead GE, Nicol K, Rush R, van Wijck F. Delirium in acute stroke: screening tools, incidence rates and predictors: a systematic review. J Neurol. 2012;259(8):1590–9.
Shih H, Huang W, Liu C, Tsai T, Lu C, Lu M, Chen P, Tseng C, Jou S, Tsai C. Confusion or delirium in patients with posterior cerebral arterial infarction. Acta Neurol Taiwanica. 2007;16(3):136.
Dahl M, Rønning O, Thommessen B. Delirium in acute stroke–prevalence and risk factors. Acta Neurol Scand. 2010;122(s190):39–43.
McManus J, Pathansali R, Hassan H, Ouldred E, Cooper D, Stewart R, Macdonald A, Jackson S. The course of delirium in acute stroke. Age Ageing. 2009;38(4):385–9.
Klimiec E, Dziedzic T, Kowalska K, Szyper A, Pera J, Potoczek P, Slowik A, Klimkowicz-Mrowiec A. PRospective Observational POLIsh Study on post-stroke delirium (PROPOLIS): methodology of hospital-based cohort study on delirium prevalence, predictors and diagnostic tools. BMC Neurol. 2015;15:94.
Oldenbeuving AW, de Kort PL, Jansen BP, Kappelle LJ, Roks G. A pilot study of rivastigmine in the treatment of delirium after stroke: a safe alternative. BMC Neurol. 2008;8:34.
Acknowledgments
Not applicable.
Funding
This work was supported by grants from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare (HI14C1967) to Tae Sung Lim.
Availability of data and materials
The de-identified data sets analyzed during the current study are available from the corresponding author upon reasonable request.
Authors’ contributions
TSL performed the study, acquired data, conducted statistical analyses and drafted the manuscript. JSL, JHY, SYM, ISJ, and KH helped provide data, interpreted the data, and checked the final version of the manuscript. JMH conceptualized the study design, analyzed and interpreted the data, wrote and revised the manuscript. All authors read and approved the final manuscript.
Competing interests
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Ajou University Hospital, according to the Declaration of Helsinki and its amendments.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lim, T.S., Lee, J.S., Yoon, J.H. et al. Cigarette smoking is an independent risk factor for post-stroke delirium. BMC Neurol 17, 56 (2017). https://doi.org/10.1186/s12883-017-0840-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-017-0840-3