Abstract
Background
Post-stroke depression (PSD) is closely associated with poor stroke prognosis. However, there are some challenges in identifying and assessing PSD. This study aimed to identify scales for PSD diagnosis, assessment, and follow-up that are straightforward, accurate, efficient, and reproducible.
Methods
A systematic literature search was conducted in 7 electronic databases from January 1985 to December 2023.
Results
Thirty-two studies were included, the Patient Health Questionnaire-9 (PHQ-9) and Hamilton Depression Scale (HDRS) had higher diagnostic accuracy for PSD. The sensitivity, specificity, and diagnostic odds ratio of PHQ-9 or diagnosing any depression were 0.82, 0.87, and 29 respectively. And for HDRS, used for diagnosing major depression, the scores were 0.92, 0.89, and 94. Furthermore, these two scales also had higher diagnostic accuracy in assessing depressive symptoms during both the acute and chronic phases of stroke. In patients with post-stroke aphasia and cognitive impairment, highly diagnostic scales have not been identified for assessing depressive symptoms yet.
Conclusions
The PHQ-9 and HDRS scales are recommended to assess PSD. HDRS, which demonstrates high diagnostic performance, can replace structured interviews based on diagnostic criteria.
Similar content being viewed by others
Introduction
Stroke is a significant cardiovascular disease, with its incidence rate and associated disease risks being of global concern [1].With the increasing incidence of stroke worldwide, the number of people suffering from post-stroke depression (PSD) has increased significantly [2]. PSD is one of the most common complications after the stroke. The main manifestations are depressive mood and loss of interest, often accompanied by somatic symptoms such as weight loss, insomnia, and fatigue [3, 4]. PSD seriously hinders the recovery of neurological function in stroke patients, leading to prolonged hospital stays loss of social interaction and independent living skills, and even increased stroke recurrence and mortality [5, 6]. Therefore, early diagnosis and treatment of PSD are crucial for prognosis. Currently, the diagnosis of PSD is still based on structured interviews [7]. Since the pathogenesis of PSD is not entirely clear [8], the dual effects of stroke-induced brain damage and mental stress complicate its diagnosis. Presently, PSD is classified as a mental disorder rather than neurological disorder. For example, in the Diagnostic and Statistical Manual of Mental Disorders—5th Edition (DSM-V), PSD is categorized under depressive disorder due to other physical diseases [7]; In the 10th edition of the International Classification of Mental Disorders (ICD-10), it is classified as an organic mental disorder [9]; Similarly, in the Chinese Classification and Diagnostic Standard of Mental Disorders (CCMD-3), it is regarded as a mental disorder caused by cerebrovascular diseases [10]. The diverse diagnostic criteria across to different classification systems further complicate the diagnosis of PSD. Additionally, most of the scales used to assess PSD usually refer to the scales of Major Depressive Disorder (MDD) [4, 11].
There are mainly three types of depression scales. Firstly, self-rating scales, such as Patient Health Questionnaire-9 (PHQ-9), Beck Depression Inventory (BDI), and Self-rating Depression Scale (SDS). Secondly, clinician-rated scales, including Hamilton Depression Rating Scale (HDRS) and Montgomery Asberg Depression Rating Scale (MADRS). Thirdly, depression assessment scales for specific populations are Geriatric Depression Screening Scale (GDS) and Stroke Aphasic Depression Questionnaire (SADQ-10). Due to the lack of uniform standards, clinical studies may apply different scales to assess the same PSD populations or use a single scale to assess PSD populations with different characteristics. The validity of these scales varies widely, leading to differences in the epidemiology, diagnosis, and assessment of PSD. Although some research teams have developed PSD-specific scales, such as Post-Stroke Depression Symptom Inventory (PSDS) [12] and Post-Stroke Depression Prediction Scale (DePreS) [13], their validity is still under clinical evaluation and they are not widely used.
Therefore, it is urgent to identify scales that can simplify the diagnostic process of PSD and facilitate the prognosis evaluation. This meta-analysis aimed to select the accurate, simple and reproducible assessment scales for PSD.
Methods
Literature search
Through computer retrieval, seven English electronic databases (PubMed, EMBASE, Medline, Web of Science, Clinical trial.gov, CINAHL, and Cochrane library) were searched for published literature on PSD and scale assessment from January 1985 to December 2023.The search scope included title and abstract, and the language was limited to English. According to the Medical Subject Headings (MeSH), the searched keywords include:
-
1)
Post-stroke depression: ‘post-stroke depression’ or ‘post stroke depression’ or ‘PSD’ or ‘depression after stroke’ or ‘emotional disturbances after stroke’ or ‘emotionalism after stroke’ or ‘vascular depression’ or ‘post stroke depressive disorder’ or ‘depressive disorder after stroke’.
-
2)
Assessment: ‘assessment scale’ or ‘validity’ or ‘measure’ or ‘measures’ or ‘evaluation’.
The retrieval formula was (#1 and #2) not (‘Meta-Analysis’ or ‘Review’ or ‘Systematic Review’).
Inclusion and exclusion criteria
Inclusion criteria were as follows:
-
(1)
The studies were original studies, including case-control and cohort studies with a clearly defined period of development or publication.
-
(2)
The study content involved the use of depression scales to evaluate PSD
-
(3)
Participants met the diagnostic criteria for stroke
-
(4)
The evaluation of PSD adhered to the relevant classification and diagnostic criteria (DSM, ICD, CCMD)
-
(5)
The study needed to provide the number of patients with stroke and PSD.
Exclusion criteria were:
-
(1)
Animal studies related to PSD
-
(2)
Lack of clear criteria for the diagnosis of stroke
-
(3)
Failure to use the diagnostic criteria for PSD based on structured interviews or assessments
-
(4)
Researchers did not adopt scientific data collection methods
-
(5)
Inappropriate use of statistical methods in research or errors in data analysis
-
(6)
Reviews, systematic reviews, dissertations, conference papers, and repeated publications
-
(7)
The literature was not in English.
Study selection
We included, but not limit to, the following types of scales: ‘The Patient Health Questionnaire-2 (PHQ-2)’, ‘The Patient Health Questionnaire-9 (PHQ-9)’, ‘Center for Epidemiological Studies-Depression(CES-D)’, ‘Montgomery Asberg Depression Rating Scale(MADRS)’, ‘Beck Depression Inventory(BDI)’, ‘Hamilton Depression Rating Scale(HDRS or HAMD)’, ‘Hospital Anxiety and Depression Scale(HADS)”, ‘Self-Rating Depression Scale(SDS)’, ‘The Geriatric Depression Scale(GDS)’, ‘Post stroke depression scale(PSDS)’, ‘ Post Stroke Depression Rating Scale(PSDRS)’, ‘Visual Analog Mood Scale(VAMS)’, and ‘Stroke Aphasic Depression Questionnaire Hospital Version( SADQ-H)’.
Data extraction
Firstly, the selected studies in the database were entered into the EndNote X9.3.2 software (Thomson Scientific, America). After screening for duplicate studies, the titles and abstracts of the remaining studies were screened again. Secondly, included studies were identified after reading the full text of each study according to the inclusion and exclusion criteria. The extracted data mainly included: author, publication time, number of cases, assessment scales and cut-offs, PSD diagnostic criteria, type of stroke, onset time of stroke when evaluating depressive symptoms, and type of depression.
Quality evaluation
Two reviewers independently assessed the quality and risk of bias of all included studies using The Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) [14], Any disagreements between the reviewers were be discussed with the superior expert until a consensus was reached.
Data analysis
The RevMan 5.4 statistical software provided by Cochrane collaboration was used for quality assessment of the data and statistical description. We used Stata15.1 software for meta-analysis and heterogeneity test. In cases where the heterogeneity between studies was P > 0.1 and I2 < 50%, we employed a fixed-effect model for comprehensive analysis. Conversely, if the heterogeneity between studies was P ≤ 0.1 and I2 ≥ 50%, the random-effect model was used. We utilized the bivariate mixed-effects model to assess the diagnostic efficacy of the scale, focusing on key evaluation indicators [15] sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio. Samples of the scales included in the evaluation must meet the criteria of the bivariate mixed-effects model analysis, with a minimum sample size of 3 (n ≥ 3).
Subgroup analysis can be divided into three subgroups: (1) Depression type, which was divided into any depression group and major depression group. Major depression was defined according to the diagnosis of MDD in DSM-V [7]: Patients were required to have five or more of nine depressive symptoms lasting more than two weeks after the stroke event, and at least one of them was 1) mood depression or 2) loss of interest or pleasure. The definition of any depression was broader, according to the depressive disorder definition in DSM-III [16], encompassing adjustment disorder with depressive mood, disorder, and dysthymia. (2) Stroke staging, which was divided into acute phase after stroke (≤ 2 months) and chronic phase after stroke (> 2 months). (3) Specific populations, it includes patients with certain characteristics, such as a comorbid history of pre-stroke depression, stroke with aphasia, cognitive dysfunction, and other features.
Results
This study followed the PRISMA guidelines on reporting [17]. The screening flowchart was shown in Fig. 1.Thirty-two studies [12, 13, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47] involving 3865 people aged between 18 and 92 were included. The relevant information from the studies was presented in Table 1. The ROBINS-I was used to evaluate the quality of the included literature. The evaluation results were presented in Fig. 2 and Fig. 3.
Meta-analysis of scale selection
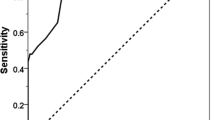
Sensitivity and specificity of the scales were assessed when the number of articles involved in each scale was two or more (n ≥ 2). The study assessed ten scales (PHQ-9, HDRS, MADRS, BDI, GDS, HADS-D, PHQ-2, CES-D, HADS, and PSDS) involving 28 articles. These ten scales had different sensitivities and specificities, and the same scale had different sensitivities and specificities in different studies (Fig. 4).
Forest plot of sensitivity and specificity for each scale. PHQ-9: Patient Health Questionnaire-9. HDRS: Hamilton Depression Scale. MADRS: Montgomery Asberg Depression Rating Scale. BDI: Beck Depression Inventory. GDS: Geriatric Depression Screening Scale. HADS-D: Hospital Anxiety and Depression Scale-Depression. PHQ-2: The Patient Health Questionnaire-2. CES-D: Center for Epidemiological Studies-Depression. HADS: Hospital Anxiety and Depression Scale. PSDS: Post-Stroke Depression Symptom Inventory
Subgroup analysis
Depression type
Any depression
Five scales were used to assess PSD when depression was classified as any depression in the study. Overall, PHQ-9 had high diagnostic efficacy when both sensitivity and specificity were considered, with a sensitivity of 0.82 (95%CI: 0.72–0.89), specificity 0.87 (95%CI: 0.68–0.95), and diagnostic odds ratio 29 (95%CI: 10.0–84.0); If only higher sensitivity was required, HDRS and MADRS were more advantageous. However, when only higher specificity was considered, PHQ-9 and HADS-D were more advantageous (Table 2).
Major depression
When classifying depression as major depression, six scales were used to assess PSD. Overall, when the sensitivity and specificity were considered together, HDRS had a high diagnostic power, with a sensitivity of 0.92 (95%CI: 0.82–0.97), specificity of 0.89 (95%CI: 0.84–0.92), and diagnostic odds ratio of 94 (95%CI: 32–281); Likewise, if only the sensitivity was considered, BDI, HDRS, MADRS had the advantage; but for higher specificity, PHQ-9 and PHQ-2 had the advantage (Table 3).
Staging of stroke
Acute phase after stroke
A total of three scales were used to assess PSD in the acute phase of stroke. PHQ-9 had high diagnostic performance when both sensitivity and specificity were considered, with a sensitivity of 0.85 (95%CI: 0.78–0.91), specificity of 0.90 (95%CI: 0.82–0.95), diagnostic odds ratio of 55 (95%CI: 30–102); If only higher sensitivity was considered, MADRS was more favorable, and if only higher specificity was considered, PHQ-9 was more favorable (Table 4).
Chronic phase after stroke
There were eight scales to assess PSD in the chronic phase of stroke. Overall, when high sensitivity and specificity were considered together, HDRS had high diagnostic power, with a sensitivity of 0.94 (95%CI: 0.87–0.98), specificity of 0.85 (95%CI: 0.76–0.91), diagnostic odds ratio of 96 (95%CI: 27–346); If only higher sensitivity was considered, HDRS and BDI had the advantage, on the contrary, if only higher specificity was considered, PHQ-2 and CES-D had the advantage (Table 5).
Specific populations
For analysis the specific populations for PSD, 9 out of 32 studies compared the baseline data characteristics of depressed and nondepressed patients after stroke. According to the previous and included data in this study, a total of seven specific populations were analyzed, with clinical features including cognitive impairment, severe aphasia, pre-onset antidepressant medication, first stroke, severity of neurological deficit, educational level, and previous psychiatric history (Table 6). However, due to the different inclusion and exclusion criteria and priorities among the original studies, the included data were insufficient, and effective statistical analysis could not be performed.
Prevalence of PSD
The results showed that the prevalence of PSD was approximately 17.0% to 29.0%, and the prevalence of PSD in the acute and chronic phases of stroke was 0.23 (95%CI 0.16–0.32) and 0.25 (95%CI 0.19–0.31), respectively. The prevalence of PSD for any depression and major depression was 0.29 (95%CI 0.23–0.34) and 0.17 (95%CI 0.13–0.22), respectively (Table 7 and Fig. 5).
Discussion
Thirty-two studies were analyzed to determine the best assessment scale for PSD. The results showed that each of these scales (PHQ-9, HDRS, MADRS, BDI, PHQ-2, CES-D, and HADS-D) had different degrees of advantage in diagnosing PSD based on depression type and stroke staging. When evaluating PSD, PHQ-9 exhibits higher diagnostic efficacy for any depression and acute phase after stroke compared to other scales. Conversely, HDRS performs better for major depression and chronic phase after stroke. Due to limitations in the data included in the literature, no effective scale has been found yet to accurately assess PSD patients with combined aphasia and cognitive impairments.
Currently, many studies utilize depression assessment scales for diagnosing PSD. However, controversy remains, as some studies suggest that these scales are not suitable for diagnosing PSD but rather for assessing the severity of depressive symptoms, treatment efficacy, or prognosis [48, 49]. Whether a scale can substitute for structured interviews in diagnosing PSD depends on its diagnostic accuracy. Our analysis revealed that PHQ-9 and HDRS performed excellently in identifying depressive symptoms and severity. The PHQ-9 is a self-rating scale consisting of 9 items with high sensitivity and specificity [50, 51]. It has been widely used in screening of PSD, because of its simplicity, less time-consuming, and low requirements for patient cooperation. HDRS, introduced in 1960, comprises seven categories, including items for somatic symptoms [52]. It is well known that in the chronic phase of stroke, many patients experience atypical depressive symptoms, such as gastrointestinal symptoms, weight loss, general pain, fatigue, and other physical discomforts [53]. HDRS can be used to assess these patients more accurately. Additionally, studies have shown that HDRS is not only uesd to evaluate the severity of PSD, but also to assess the efficacy of antidepressant treatment [54, 55].
Burton conducted a review of the scales used for screening post-stroke mood disorders in 2015 [56]. They focus on mood disorders after stoke, which include various emotions, such as major depression, any degree of depression, or anxiety. Meader also conducted a related meta-analysis in 2014, which included 24 studies involving 2907 patients [57], the results showed that many scales could screen the PSD, such as CESD, HDRS, and PHQ-9. However, these scales should not be used alone but should be combined with detailed clinical assessments. In comparison to Burton’s and Meader's studies, our study included thirty-two studies, and we provided a clearer description of the stage of stroke and the type of depression for PSD. Additionally, we discussed the selection of scales for PSD in special populations and analyzed the prevalence of PSD.
For the staging of stroke, there is still no unified conclusion at present, and the duration of stroke will affect the symptoms of PSD [58, 59]. Some studies recommend assessing PSD at 2 or 8 weeks after stroke, and Toso 's study found that PSD most occurred within 3 months after stroke [60]. In our study, stroke was staged into the acute phase (within 2 months of stroke onset) and chronic phase (2 months after stroke onset). According to the severity of depression, Robinson classified PSD into mild PSD (mild depression) and severe PSD (severe depression). Mild PSD corresponds to dysthymia in DSM-III, while severe PSD meets the diagnostic criteria for MDD [61]. Therefore, in this study, PSD was divided into two groups: any depression and major depression, and it should be emphasized that any depression included major depression and mild depression.
This study aimed to analyze which scale was more effective in identifying and assessing depressive symptoms in the specific population with PSD. However, due to the different inclusion and exclusion criteria and priorities among the original studies, the included data were insufficient, and effective statistical analysis could not be performed. Stroke patients often experience complications such as aphasia and cognitive dysfunction, which can exacerbate PSD. A related study found that post-stroke aphasia patients are more likely to suffer from depression than non-aphasia patients [62]. According to a systematic review by Mariska, there was insufficient evidence supporting the use of a specific scale to evaluate the depressive symptoms in aphasia patients, and the evidence level of existing studies was relatively low [63]. In addition, relevant studies have shown that post-stroke cognitive impairment (PSCI) was closely related to the occurrence of PSD [64, 65]. Impairment oognitive function can affect the evaluation of depressive symptoms to varying degrees. At present, cognitive function scales based on the assessment of Alzheimer's disease are often used in clinical work to assess PSCI, such as Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment Scale (MoCA), and Cambridge Geriatric Cognitive Scale (CAMCOG). However, the organic damage of cerebral parenchyma in stroke patients, along with complications such as aphasia, visual impairment, dyslexia, and limb dysfunction, can impose limitations in the evaluation of PSCI using the aforementioned scales [66, 67]. Hence, further research is warranted to determine the most suitable scales for assessing depressive symptoms in patients with post-stroke aphasia and cognitive impairment.
The results of the study revealed that the prevalence of PSD, determined through standard structured interviews, ranged from 17.0% to 29.0%. Previous studies by Ayerbe and Hackett indicated that approximately one-third of stroke patients experienced varying degrees of depression within five years after the stroke event [68,69,70]. It is important to note that the assessment of prevalence was primarily conducted using depression scales. Many factors affect the prevalence of the PSD, such as the population, time, and place of assessment. Nowadays, there is a divergence of opinions regarding whether the timing of PSD assessment influences the prevalence of depression. Some studies showed that the prevalence of depression in the acute phase after stroke was higher than in the chronic phase, and the prevalence gradually decreases over time [71,72,73], However, another study found no difference in the prevalence of PSD in the early, middle, and late stages of stroke [74]. Therefore, more high-quality prospective studies will be needed in the future to clarify this issue.
Limitations
There are also some limitations in this study [1]. This study was a secondary analysis, and the included studies exhibited significant heterogeneity due to variations in diagnostic thresholds for each scale. Additionally, the optimal diagnostic cut-off of each scale was not analyzed, so it needs to clarify in future studies [2]. Data limitations and mismatches between the original studies hindered subgroup analyses of scale selection, thereby preventing adequate analyses for different types and severity of stroke, aphasia population, the elderly population, individuals with a history of depression, and other populations. In the future, developing more comprehensive research protocols for PSD is crucial.
Conclusion
In conclusion, there are various scales to evaluate PSD. To improve diagnostic effectiveness, a variety of scales can be used for dynamic, multi-directional evaluation and follow-up. The PHQ-9 and HDRS are recommended for the evaluation PSD due to their high diagnostic efficiency. Structured interviews based on diagnostic criteria can determine whether stroke patients have depressive symptoms, and depression scales can further determine the severity of symptoms. It is recommended to replace the structured interviews based on diagnostic criteria with rating scales, such as HDRS, with high diagnostic efficacy. Currently, there is still a lack of depression scales for evaluating patients with post-stroke aphasia and cognitive dysfunction.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- ADRS:
-
Aphasic Depression Rating Scale
- BDI:
-
Beck Depression Inventory
- CAMCOG:
-
Cambridge Geriatric Cognitive Scale
- CCMD-3:
-
Chinese Classification and Diagnostic Standard of Mental Disorders
- CES-D:
-
Center for Epidemiological Studies-Depression
- CGI-S:
-
Clinical Global Impression-Scale
- DePreS:
-
Post-Stroke Depression Prediction Scale
- DSM-V:
-
Diagnostic and Statistical Manual of Mental Disorders
- GDS:
-
Geriatric Depression Screening Scale
- HADS:
-
Hospital Anxiety and Depression Scale
- HADS-D:
-
Hospital Anxiety and Depression Scale—Depression
- HDRS:
-
Hamilton Depression Scale
- ICD-10:
-
International Classification of Mental Disorders
- MADRS:
-
Montgomery Asberg Depression Rating Scale
- MDD:
-
Major Depressive Disorder
- MeSH:
-
Medical Subject Headings
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment Scale
- PHQ-2:
-
The Patient Health Questionnaire-2
- PHQ-9:
-
Patient Health Questionnaire-9
- PSCI:
-
Post-Stroke Cognitive Impairment
- PSD:
-
Post-stroke depression
- PSDRS:
-
Post Stroke Depression Rating Scale
- PSDS:
-
Post-Stroke Depression Symptom Inventory
- SADQ-10:
-
Stroke Aphasic Depression Questionnaire
- SDS:
-
Self-rating Depression Scale
- SODS:
-
Signs of Depression Scale
- VAMS:
-
Visual Analog Mood Scale
- VASES:
-
Visual Analogue self-esteem Scale
References
GBD 2021 diseases and injuries collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global burden of disease study 2021. Lancet. 2024;403(10440):2133–61.
Feigin PVL. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–80.
Lanctôt KL, Lindsay MP, Smith EE, Sahlas DJ, Foley N, Gubitz G, et al. Canadian stroke best practice recommendations: mood, cognition and fatigue following stroke, 6th edition update 2019. Int J Stroke. 2020;15(6):668–88.
Towfighi A, Ovbiagele B, El Husseini N, Hackett ML, Jorge RE, Kissela BM, et al. Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(2):e30–43.
Pohjasvaara T, Leskelä M, Vataja R, Kalska H, Ylikoski R, Hietanen M, et al. Post-stroke depression, executive dysfunction and functional outcome. Eur J Neurol. 2002;9(3):269–75.
Villa RF, Ferrari F, Moretti A. Post-stroke depression: mechanisms and pharmacological treatment. Pharmacol Ther. 2018;184:131–44.
Battle DE. Diagnostic and Statistical Manual of mental disorders (DSM). Codas. 2013;25(2):191–2.
Guo J, Wang J, Sun W, Liu X. The advances of post-stroke depression: 2021 update. J Neurol. 2022;269(3):1236–49.
World Health Organization. ICD-10 : international statistical classification of diseases and related health problems : tenth revision, 2nd ed. World Health Organization; 2004. https://iris.who.int/handle/10665/42980.
Chen YF. Chinese classification and diagnostic criteria of mental disorders, third version. Psych branch Chin Med Assoc. 2001;1:18–19.
Wang SS, Zhou XY, Zhu CY. Chinese expert consensus on clinical practice of post-stroke depression. Chin J Stroke. 2016;11(8):685–93.
Yue Y, Liu R, Lu J, Wang X, Zhang S, Wu A, et al. Reliability and validity of a new post-stroke depression scale in Chinese population. J Affect Disord. 2015;174:317–23.
Hirt J, van Meijeren LCJ, Saal S, Hafsteinsdóttir TB, Hofmeijer J, Kraft A, et al. Predictive accuracy of the post-stroke depression prediction scale: a prospective binational observational study ✰. J Affect Disord. 2020;265:39–44.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61.
Zhang TS. Applied methodology for evidence-based medicine. Changsha: Central South University Press; 2014. p. 417–8.
Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gener Psychiatry. 1992;49(8):624–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Mikami K, Sudo T, Orihashi Y, Kimoto K, Mizuma A, Uesugi T, et al. Effective tools to predict depression in acute and subacute phase of ischemic stroke. J Neuropsychiatry Clin Neurosci. 2021;33(1):43–8.
Dajpratham P, Pukrittayakamee P, Atsariyasing W, Wannarit K, Boonhong J, Pongpirul K. The validity and reliability of the PHQ-9 in screening for post-stroke depression. BMC Psychiatry. 2020;20(1):291.
Wang EY, Meyer C, Graham GD, Whooley MA. Evaluating screening tests for depression in post-stroke older adults. J Geriatr Psychiatry Neurol. 2018;31(3):129–35.
Prisnie JC, Fiest KM, Coutts SB, Patten SB, Atta CA, Blaikie L, et al. Validating screening tools for depression in stroke and transient ischemic attack patients. Int J Psychiatry Med. 2016;51(3):262–77.
Lewin-Richter A, Volz M, Jöbges M, Werheid K. Predictivity of early depressive symptoms for post-stroke depression. J Nutr Health Aging. 2015;19(7):754–8.
Imarhiagbe FA, Owolabi A. Post-stroke depression in a sub-Saharan Africans: validation of the japanese stroke scale for depression. Sahel Med J. 2015;18(3):121.
Lees R, Stott DJ, Quinn TJ, Broomfield NM. Feasibility and diagnostic accuracy of early mood screening to diagnose persisting clinical depression/anxiety disorder after stroke. Cerebrovasc Dis. 2014;37(5):323–9.
Kang HJ, Stewart R, Kim JM, Jang JE, Kim SY, Bae KY, et al. Comparative validity of depression assessment scales for screening poststroke depression. J Affect Disord. 2013;147(1–3):186–91.
Turner A, Hambridge J, White J, Carter G, Clover K, Nelson L, et al. Depression screening in stroke: a comparison of alternative measures with the structured diagnostic interview for the diagnostic and statistical manual of mental disorders, fourth edition (major depressive episode) as criterion standard. Stroke. 2012;43(4):1000–5.
de Man-van Ginkel JM, Hafsteinsdóttir T, Lindeman E, Burger H, Grobbee D, Schuurmans M. An efficient way to detect poststroke depression by subsequent administration of a 9-item and a 2-item Patient Health Questionnaire. Stroke. 2012;43(3):854–6.
Sagen U, Vik TG, Moum T, Mørland T, Finset A, Dammen T. Screening for anxiety and depression after stroke: comparison of the hospital anxiety and depression scale and the Montgomery and Asberg depression rating scale. J Psychosom Res. 2009;67(4):325–32.
Roger PR, Johnson-Greene D. Comparison of assessment measures for post-stroke depression. Clin Neuropsychol. 2009;23(5):780–93.
Berg A, Lönnqvist J, Palomäki H, Kaste M. Assessment of depression after stroke a comparison of different screening instruments. Stroke. 2009;40(2):523–9.
Quaranta D, Marra C, Gainotti G. Mood disorders after stroke: diagnostic validation of the poststroke depression rating scale. Cerebrovasc Dis. 2008;26(3):237–43.
Lee AC, Tang SW, Yu GK, Cheung RT. The smiley as a simple screening tool for depression after stroke: a preliminary study. Int J Nurs Stud. 2008;45(7):1081–9.
Healey AK, Kneebone II, Carroll M, Anderson SJ. A preliminary investigation of the reliability and validity of the Brief Assessment Schedule Depression Cards and the Beck Depression Inventory-Fast Screen to screen for depression in older stroke survivors. Int J Geriatr Psychiatry. 2008;23(5):531–6.
Lightbody CE, Baldwin R, Connolly M, Gibbon B, Jawaid N, Leathley M, et al. Can nurses help identify patients with depression following stroke? A pilot study using two methods of detection. J Adv Nurs. 2007;57(5):505–12.
Laska AC, Mårtensson B, Kahan T, von Arbin M, Murray V. Recognition of depression in aphasic stroke patients. Cerebrovasc Dis. 2007;24(1):74–9.
Williams LS, Brizendine EJ, Plue L, Bakas T, Tu W, Hendrie H, et al. Performance of the PHQ-9 as a screening tool for depression after stroke. Stroke. 2005;36(3):635–8.
Tang WK, Ungvari GS, Chiu HFK, Sze KH. Detecting depression in Chinese stroke patients: a pilot study comparing four screening instruments. Int J Psychiatry Med. 2004;34(2):155–63.
Tang WK, Ungvari GS, Chiu HF, Sze KH, Yu AC, Leung TL. Screening post-stroke depression in Chinese older adults using the hospital anxiety and depression scale. Aging Ment Health. 2004;8(5):397–9.
Tang WK, Chan SS, Chiu HF, Wong KS, Kwok TC, Mok V, et al. Can the Geriatric Depression Scale detect poststroke depression in Chinese elderly? J Affect Disord. 2004;81(2):153–6.
Lincoln NB, Nicholl CR, Flannaghan T, Leonard M, Van der Gucht E. The validity of questionnaire measures for assessing depression after stroke. Clin Rehabil. 2003;17(8):840–6.
Naarding P, Leentjens AF, van Kooten F, Verhey FR. Disease-specific properties of the rating scale for depression in patients with stroke, Alzheimer’s dementia, and Parkinson’s disease. J Neuropsychiatry Clin Neurosci. 2002;14(3):329–34.
Aben I, Verhey F, Lousberg R, Lodder J, Honig A. Validity of the beck depression inventory, hospital anxiety and depression scale, SCL-90, and hamilton depression rating scale as screening instruments for depression in stroke patients. Psychosomatics. 2002;43(5):386–93.
O’Rourke S, MacHale S, Signorini D, Dennis M. Detecting psychiatric morbidity after stroke: comparison of the GHQ and the HAD Scale. Stroke. 1998;29(5):980–5.
Agrell B, Dehlin O. Comparison of six depression rating scales in geriatric stroke patients. Stroke. 1989;20(9):1190–4.
Parikh RM, Eden DT, Price TR, Robinson RG. The sensitivity and specificity of the Center for Epidemiologic Studies Depression Scale in screening for post-stroke depression. Int J Psychiatry Med. 1988;18(2):169–81.
Shinar D, Gross CR, Price TR, Banko M, Bolduc PL, Robinson RG. Screening for depression in stroke patients: the reliability and validity of the Center for Epidemiologic Studies Depression Scale. Stroke. 1986;17(2):241–5.
Yue Y, Liu R, Chen J, Cao Y, Wu Y, Zhang S, et al. The reliability and validity of Post Stroke Depression Scale in different type of Post Stroke Depression patients. J Stroke Cerebrovasc Dis. 2022;31(2):106222.
Yue YY, Yuan YG. Evaluation and diagnosis of post-stroke depression. Pract Geriatr. 2015;29(2):5.
Yuan YG, Jiang HT. Preface-pay attention to the standardized diagnosis and treatment of post-stroke depression. Pract Geriatr. 2015;29(2):91–2.
Trotter TL, Denny DL, Evanson TA. Reliability and validity of the patient health questionnaire-9 as a screening tool for poststroke depression. J Neurosci Nurs. 2019;51(3):147–52.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Leng HX, Ding WJ, Zhang WR, Wang HX. Progress in assessment of post-stoke depression. Chin J Stroke. 2020;15(7):795–800.
van de Weg FB, Kuik DJ, Lankhorst GJ. Post-stroke depression and functional outcome: a cohort study investigating the influence of depression on functional recovery from stroke. Clin Rehabil. 1999;13(3):268–72.
Hung CYF, Wu XY, Chung VCH, Tang ECH, Wu JCY, Lau AYL. Overview of systematic reviews with meta-analyses on acupuncture in post-stroke cognitive impairment and depression management. Integr Med Res. 2019;8(3):145–59.
Chen YK, Qu JF, Xiao WM, Li WY, Li W, Fang XW, et al. Intracranial atherosclerosis and poststroke depression in Chinese patients with ischemic stroke. J Stroke Cerebrovasc Dis. 2016;25(4):998–1004.
Burton LJ, Tyson S. Screening for mood disorders after stroke: a systematic review of psychometric properties and clinical utility. Psychol Med. 2015;45(1):29–49.
Meader N, Moe-Byrne T, Llewellyn A, Mitchell AJ. Screening for poststroke major depression: a meta-analysis of diagnostic validity studies. J Neurol Neurosurg Psychiatry. 2014;85(2):198–206.
Bernhardt J, Hayward KS, Kwakkel G, Ward NS, Wolf SL, Borschmann K, et al. Agreed definitions and a shared vision for new standards in stroke recovery research: the stroke recovery and rehabilitation roundtable taskforce. Int J Stroke. 2017;12(5):444–50.
Guerra ZF, Lucchetti G. Divergence among researchers regarding the stratification of time after stroke is still a concern. Int J Stroke. 2018;13(4):NP9.
Toso V, Gandolfo C, Paolucci S, Provinciali L, Torta R, Grassivaro N. Post-stroke depression: research methodology of a large multicentre observational study (DESTRO). Neurol Sci. 2004;25(3):138–44.
Robinson RG, Starr LB, Kubos KL, Price TR. A two-year longitudinal study of post-stroke mood disorders: findings during the initial evaluation. Stroke. 1983;14(5):736–41.
Shehata GA, El Mistikawi T, Risha ASK, Hassan HS. The effect of aphasia upon personality traits, depression and anxiety among stroke patients. J Affect Disord. 2015;172:312–4.
van Dijk MJ, de Man-van Ginkel JM, Hafsteinsdóttir TB, Schuurmans MJ. Identifying depression post-stroke in patients with aphasia: a systematic review of the reliability, validity and feasibility of available instruments. Clin Rehabil. 2016;30(8):795–810.
Kauhanen M, Korpelainen JT, Hiltunen P, Brusin E, Mononen H, Määttä R, et al. Poststroke depression correlates with cognitive impairment and neurological deficits. Stroke. 1999;30(9):1875–80.
Williams OA, Demeyere N. Association of depression and anxiety with cognitive impairment 6 months after stroke. Neurology. 2021;96(15):e1966–74.
Nys GMS, van Zandvoort MJE, de Kort PLM, Jansen BPW, Kappelle LJ, de Haan EHF. Restrictions of the Mini-Mental State Examination in acute stroke. Arch Clin Neuropsychol. 2005;20(5):623–9.
Demeyere N, Riddoch MJ, Slavkova ED, Jones K, Reckless I, Mathieson P, et al. Domain-specific versus generalized cognitive screening in acute stroke. J Neurol. 2016;263(2):306–15.
Ayerbe L, Ayis S, Wolfe CD, Rudd AG. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry. 2013;202(1):14–21.
Kowalska K, Pasinska P, Klimiec-Moskal E, Pera J, Slowik A, Klimkowicz-Mrowiec A, et al. C-reactive protein and post-stroke depressive symptoms. Sci Rep. 2020;10(1):1431.
Hackett ML, Pickles K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke. 2014;9(8):1017–25.
Robinson RG. Poststroke depression: prevalence, diagnosis, treatment, and disease progression. Biol Psychiatry. 2003;54(3):376–87.
Yuan HW, Wang CX, Zhang N, Bai Y, Shi YZ, Zhou Y, et al. Poststroke depression and risk of recurrent stroke at 1 year in a Chinese cohort study. PLoS One. 2012;7(10):e46906.
Zhang N, Wang CX, Wang AX, Bai Y, Zhou Y, Wang YL, et al. Time course of depression and one-year prognosis of patients with stroke in mainland China. CNS Neurosci Ther. 2012;18(6):475–81.
Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(6):1330–40.
Acknowledgements
Thanks to Ms. Zhang Fan from Chongqing Medical University for consulting help on the application of statistical methods in the study.
Funding
This article was funded by the Chongqing Health Commission (Grant No. 2020MSXM038) and Special support project for clinical research of young and middle-aged doctors in the south of the Five Ridges neurology (Grant No. Z20210305).
Author information
Authors and Affiliations
Contributions
Jun Mu and Fang Liu designed the study, Fang Liu and Lei Gong collected the data and material, Huan Zhao and Ying-li Li checked the data, Fang Liu analyzed the data and wrote the first draft of the manuscript, Zhiwen Yan gave the advice for analysis the data. And all authors contributed to comment on previous versions of the manuscript, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, F., Gong, L., Zhao, H. et al. Validity of evaluation scales for post-stroke depression: a systematic review and meta-analysis. BMC Neurol 24, 286 (2024). https://doi.org/10.1186/s12883-024-03744-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03744-7