Abstract
Objective
To assess the prevalence of anxiety and depression and their associated risk factors throughout the pregnancy and postpartum process using a new screening for the early detection of mental health problems.
Design
A prospective cross-sectional descriptive multicentred study. Participants were consecutively enrolled at ≥ 12 weeks’ gestation and followed at three different time points: at 12–14 weeks of pregnancy, at 29–30 weeks of pregnancy, and 4–6 weeks postpartum. All women completed a mental screening at week 12–14 of pregnancy consisting of two questions from the Generalised Anxiety Disorder Scale (GAD-2) and the two Whooley questions. If this screening was positive, the woman completed the Edinburgh Postnatal Depression Scale (EPDS).
Setting
Seven primary care centres coordinated by a Gynaecology and Obstetrics Department in the city of Terrassa (Barcelona) in northern Spain.
Participants
Pregnant women (N = 335, age 18–45 years), in their first trimester of pregnancy, and receiving prenatal care in the public health system between July 2018 and July 2020.
Findings
The most relevant factors associated with positive screening for antenatal depression or anxiety during pregnancy, that appear after the first trimester of pregnancy, are systematically repeated throughout the pregnancy, and are maintained in the postpartum period were: a history of previous depression, previous anxiety, abuse, and marital problems. In weeks 12–14 early risk factors for positive depression and anxiety screening and positive EPDS were: age, smoking, educational level, employment status, previous psychological/psychiatric history and treatment, suicide in the family environment, voluntary termination of pregnancy and current planned pregnancy, living with a partner and partner’s income. In weeks 29–30 risk factors were: being a skilled worker, a history of previous depression or anxiety, and marital problems. In weeks 4–6 postpartum, risk factors were: age, a history of previous depression or anxiety or psychological/psychiatric treatment, type of treatment, having been mistreated, and marital problems.
Conclusions
Early screening for anxiety and depression in pregnancy may enable the creation of more effective healthcare pathways, by acting long before mental health problems in pregnant women worsen or by preventing their onset. Assessment of anxiety and depression symptoms before and after childbirth and emotional support needs to be incorporated into routine practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Motherhood is a normal life process characterized not only by physiological and biological changes in the mother’s body, but also by a psychological adjustment to the new reality of pregnancy, childbirth, and the future baby [1]. Non-psychotic perinatal mental disorders (PMDs) refer to common mental health conditions (i.e., anxiety, depression) that occur during pregnancy or in the first year after birth. Most of these PMDs have a non-negligible prevalence worldwide. Different countries have characterized the prevalence of anxiety and depression in their pregnant and postpartum populations. In western countries the prevalence of antenatal and postnatal anxiety and depression varies: e.g., Canada, 16% and 17%, 4% and 5%, respectively [2]; Italy, 21% and 25%, 22% and 13%, respectively [3]; Spain, 4% and 15% in the postpartum period [4]. Even in certain subpopulations (low and lower-middle-income countries), the average prevalence of PMDs (mainly anxiety and depression) is about 16% prenatally and 20% postnatally [5], and between 10% and 13%, respectively, in high-income countries [6, 7]. A 2015 meta-analysis showed a high variation in the percentage of mothers with perinatal anxiety, from 3 to 39% [8]. Against this background, estimates of anxiety and depression vary considerably by the population studied, and even the evidence is inconclusive as to whether the prevalence among pregnant women differs from that of non-pregnant populations [9].
Furthermore, the negative relationship that anxiety and depression during pregnancy can have for both mother and baby, due to the increase in the hormone cortisol has been demonstrated [10, 11]. In addition, anxiety processes in pregnant and postpartum mothers lead to increased smoking and alcohol consumption [12,13,14], which in turn will have a clear impact on the foetus and on breastfeeding infants [15]. Anxiety during pregnancy has also been associated with a higher number of follow-up visits [16], a higher likelihood of caesarean section and requesting an elective caesarean Sect. [17]. Similarly, those who expressed distress during childbearing were more likely to experience disaffection towards their babies and postpartum depression (PPD) [2, 18]. These factors are of relevance as they negatively influence pregnancy, childbirth, and the postpartum period, and affect women’s coping, with high health, economic and social costs across cultures [19]. Some studies link maternal anxiety to adverse neurodevelopmental outcomes in the baby, including cognitive, language, emotional, and behavioural problems [11, 20]. Prenatal anxiety has also been associated with low weight for gestational age, pre-term birth, endocrine and inflammatory changes in infants, and even foetal physiological changes (heart rate abnormalities), among other effects [20,21,22,23].
However, despite the health and social impact of PMDs [24], even with a worrying associated childhood morbidity [25], there is little research on PMDs, with prevalence not always concordant and conclusive, and relatively little funding for research and specialized services and public health interventions to improve detection and management of such PMDs in pregnant women.
It is clear from the above studies that there is no common systematization in determining the existence of PMDs and associated factors, partly due to the use of different instruments to measure some of the mental conditions. In this sense, the significant heterogeneity in the methodology of the studies may explain the discrepancies between them. There are even studies that try to assess which instruments seem to be the most accurate for assessing some of the PMDs in women, based on their co-morbidity [2, 25] during pregnancy or postpartum [26].
The introduction of preventive perinatal mental health screening is a quality standard in pregnancy and postpartum management [27], as assessment, detection, management, and treatment of mental health problems that women may experience during pregnancy and postpartum are essential to ensure optimum health outcomes for both mother and baby, as well as for the rest of the family. In Catalonia, the Protocol for Pregnancy Control, in its latest revision of 2018, introduces for the first time, and in a systematic way, a universal screening in perinatal mental health [1]. This preventive intervention improves the detection of potential mental health problems that may occur in women during pregnancy and puerperium. To correctly detect and assess these problems in pregnant women, this new protocol recommends a good anamnesis, as well as the initial identification of symptoms of depression and/or anxiety through the Whooley Questions [28], the Generalised Anxiety Disorder Scale (GAD-2) [29,30,31], and the Edinburgh Postpartum Depression Scale (EPDS) [32], and using a timetable based on different pregnancy and postpartum periods.
The aim of this study is to determine the pre- and post-natal evolution of anxiety and depression symptoms and associated factors at 12–14 weeks and at 30 weeks of gestation, and during the puerperium (at 4–6 weeks postpartum), in a large population of women attending our services by using a standardised protocol resulting from the consensus of a large group of professionals and scientific societies in the obstetric field [1]. This protocol introduces a new screening for the early detection, by midwives, of mental health problems that may affect pregnant women, who are particularly vulnerable at this time of life. This will help to confirm the usefulness of this pre- and post-natal screening performed by a midwife, as a first step. We believe that our research to accurately determine the prevalence, understand the course, and identify risk factors and outcomes related to anxiety and depression in pregnant women can have a real impact on effective treatments for anxiety and mood disorders in pregnancy.
Materials and methods
This is a prospective descriptive multicentre study (7 primary care centres involved) co-ordinated by the Gynaecology and Obstetrics Department in Mutua Terrassa (Barcelona, Spain) between July 2018 and July 2020 and including 335 cognitively normal pregnant women (mean age [range] 32.0 [18.0–45.0] years) who regularly come to the Sexual and Reproductive Health Care (ASSIR) unit of Mutua Terrassa to control their pregnancy. Participants were consecutively included at ≥ 12 weeks gestation.
The inclusion criteria involved: (1) women aged ≥ 18 years; (2) women controlled at the ASSIR unit of Mutua Terrassa; and (3) verbal and written comprehension of instructions and the assessment. The exclusion criteria involved: (1) any condition preventing demographic or mental health assessment, and (2) women with a diagnosed psychiatric pathology who were being monitored by the mental health team.
Following a standardised protocol created by obstetric experts [1], all participants underwent an initial demographic and medical interview and a mental health screening by midwifery visits to detect possible anxiety and depression-related symptomatology (see below) at three different time points: at week 12–14 of pregnancy (Visit 1), at week 29–30 of pregnancy (Visit 2) and at week 4–6 of postpartum (Visit 3) (see Fig. 1). Mental health screening was conducted at 12–14 weeks of gestation, at 29–30 weeks of gestation, and during the postpartum visit, as described in the Pregnancy Monitoring Protocol in Catalonia (Spain), which is agreed upon by the group of experts from the Department of Health and the scientific societies of Catalonia [1].
Screening for anxiety and depression symptoms in pregnant women and during the early postpartum period by the Protocol for Pregnancy Control [1]
The study was approved by the Clinical Research Ethics Committee (CEIC) of Mutua Terrassa (Spain) (# approval: B1803) and was conducted in accordance with the principles of the Declaration of Helsinki (World Medical Association Declaration of Helsinki, 1997) and its later amendments (revised in 2013). Informed written consent was obtained from all the participants. Informed consent to participate was obtained for illiterate participants from their legal guardians.
Sociodemographic and clinical screening for mental health disorders
At the 12-14-week gestational visit, the women were enrolled in the study, completed the sociodemographic and medical history questionnaire, and underwent mental health screening consisting of the two GAD-2 questions and the two Whooley questions. If one of the four questions was positive, the EPDS was performed. In the 30th week of pregnancy, the mental health screening was performed again, and in the 4th-6th week postpartum the EPDS was performed (see Fig. 1).
Sociodemographic characteristics, current obstetric history, current mental health history, and family history information were collected at 12–14 weeks of pregnancy.
Following the guidelines of the National Institute of Clinical Excellence (NICE) [27] and the Pregnancy Control Protocol in Catalonia [1], we performed a perinatal mental screening using different questions and instruments to identify symptoms of depression and/or anxiety at 12–14 weeks of pregnancy. Specifically, the Whooley questionnaire for depression and two anxiety-related questions from the GAD-2 were used first. Based on the results of these two instruments, the EPDS was passed (Fig. 1). The specific tests for the clinical screening can be found in the Supplementary Material.
Statistical analyses
Descriptive statistics were calculated for each sociodemographic, clinical, and obstetric variable, using median and range for quantitative variables, and absolute (n) and relative (%) frequencies for categorical variables. The McNemar test was used to compare the results of the initial screening (Whooley and GAD-2) between visits. Complementary exploratory analyses were performed at each visit to assess potential risk factors associated with a positive screening and EPDS result. Independent t-test was used for comparisons between groups in continuous variables and Mann Whitney U test was used when the variables did not display a normal distribution and the chi-square test or, when appropriate, Fisher’s exact test was used in the case of qualitative variables. All analyses were conducted using IBM SPSS Statistics for Windows, version 26.0 (Armonk, NY: IBM Corp. Released 2019). As this was a preliminary study, α was set at a p-value < 0.05, without correction for multiple comparisons.
Results
Sociodemographic, clinical, and obstetric variables
A final sample of 335 pregnant women was initially included. Figure 2 shows losses across the study’s midwifery visits. Between visit 1 (weeks 12 and 14 of pregnancy) and visit 3 (weeks 4 and 6 postpartum) there was a sample loss of 14.2% (N = 48), of which 16.7% were miscarriages (in weeks 29–30 of pregnancy).
The majority of the sample either live with a partner or live with a partner and children (89.9%). 35% have a university education, while 19.8% have minimal or no education. 44.3% are skilled workers. Most report the couple’s income (92.8%). In relation to obstetric and clinical variables, the majority had planned the pregnancy (75.8%), 53.1% being first-time mothers. 8.1% had traumatic experiences related to a previous birth. 34.4% show current high/very high gestational risk level (Table 1). 6.6% (N = 22) of the sample suffered from maltreatment prior to the study, 2.4% (N = 8) from sexual abuse and 5.1% (N = 17) cited relationship problems with their partner.
A total of 14.6% (N = 49) of the women reported psychiatric disorders diagnosed in 1st-degree relatives, 9% (N = 30) showed severe mental illness in family members, and 2.1% (N = 7) reported cases of suicide in the family environment. 3% (N = 10) reported postpartum depression in mothers and/or sisters.
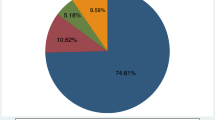
Figure 3 shows the psychiatric history of the sample. 18.5% (N = 62) of the women reported having received previous psychological/psychiatric treatment (7.5% [N = 25] psychopharmaceuticals, 5.4% [N = 18] psychological treatment, and 5.4% [N = 18] both types of approach), while 2.1% (N = 7) required hospitalisation for mental health problems (Table 1).
Clinical screening for detecting anxiety and depression
At week 12–14 of pregnancy, 53.4% of the sample (N = 179) showed positive screening for symptoms of anxiety and depression (at least one positive response to the Whooley or the GAD-2 questions). Figure 4a) illustrates the evolution of cases showing anxious and/or depressive symptomatology as a function of the established screening. Figure 4b) shows specifically the percentages of women in the initial sample (N = 335) who scored ≥ 13 on the EPDS at the three midwife follow-up visits. Overall, there is a reduction in the percentage of cases scoring ≥ 13 on the EPDS across visits, which is most evident at the week 29–30 visit. A decrease of 2.3 is observed from week 12–14 antepartum to week 4–6 postpartum. A final sample of 80 out of 335 women (23.9%) were referred for psychiatric evaluation (in orange). See also Supplementary Fig. 1.
(a) Pie charts showing the evolution of cases with anxious and/or depressive symptomatology based on established screening. The percentages for each pie chart are calculated since the previous N from which they start (relative percentages). The EPDS scores threshold to consider pathology is established at 13 points and or to ask positively to question 10 (thoughts of harming oneself). In orange, women who over the course of the months of screening required a referral for diagnosis and assessment of psychological or psychiatric pathology. (b) Absolute percentages versus the original sample N = 335
There were significant differences in the positive screening for anxiety and depression (including Whooley and GASD-2) between visit 1 and visit 2 (p < 0.001) with the proportion of positive cases at week 29–30 versus week 12–14 increased to 16.4%. The proportion of positive cases at weeks 12–14 that resulted in a negative screening at weeks 29–30 was 37.2%.
Risk factors for positive screening (Whooley and GAD-2 questions)
Weeks 12–14 of pregnancy (visit 1)
Eleven sociodemographic, clinical, and obstetric variables were risk factors for positive screening at weeks 12–14.
Sociodemographic variables
Age is lower in patients screened positive (mean [SD] of 30.4 [6.1] years versus 32.1 [5.7] years, p = 0.009). Smoking habit (smoking, but not the number of cigarettes), with women smokers having the highest percentages of positive screenings (15.1% [10.4%-20.9] versus 7.7% [4.3-12.7%], p = 0.035), education level, with illiterate women showing higher percentages of positive screenings (% [CI95%] 25.3% [19.3-32.0%] versus 13.5% [8.8-19.5%], p = 0.025), employment status, with women in skilled jobs having more negative screenings at week 12–14 than women in semi-skilled or unskilled jobs or unemployed (52.6% [44.7%-60.4] versus 37.1% [30.2-44.3%], p = 0.010).
A higher percentage of women living in a couple score < 13 on the scale (97.2% [93.6-99.1%] vs. 79.4% [63.8-90.3%], p < 0.001), and a higher percentage of women reporting a couple’s income score < 13 (93.8% [89.0-96.9%] vs. 82.4% [67.2-92.3%], p = 0.042).
Clinical variables
Women with a history of previous depression have higher percentages of positive screenings (15.6% [10.9-21.5%] versus 3.8% [1.6-7.7%], p < 0.001), history of previous anxiety, with women with a history of anxiety having a higher percentages of positive screenings (27.9% [21.8-34.8%] versus 10.3% [6.2-15.74%], p < 0.001), previous psychological/psychiatric history, with women receiving previous treatment having higher percentages of positive screenings (25.7% [19.7-32.4%] versus 10.3% [6.2-15.7%], p < 0.001), type of treatment (psychological and/or pharmacological), with women who have received some treatment, especially pharmacological, having more cases of positive screening (cases with pharmacological treatment, 10.1% [6.3-15.1%] versus 4.5% [2.0-8.6%], p = 0.005), mistreated, with mistreated women having higher percentages of positive screenings (11.2% [7.2-16.4%] versus 1.3% [0.3-4.0%], p < 0.001), and marital problems, with women who are in a bad relationship having higher percentages of positive screenings (7.8% [4.6-12.4%] versus negative 1.9% [0.5-5.0%], p = 0.014). A higher percentage of women reporting cases of suicide in the family environment score ≥ 13 (0.7% [0.1-3.2%] vs. 8.8% [2.5-21.7%], p = 0.022), more women with previous depression history score ≥ 13 (10.3% [6.2-16.1%] vs. 38.2% [23.4-55.0%], p < 0.001), more women with previous anxiety history score ≥ 13 (58.8% [42.1-74.1%] vs. 20.7% [14.7-27.8%], p < 0.001), more non-mistreated women score < 13 (92.4% [87.3-95.9%] vs. 73.5% [57.2-86.0%], p = 0.004), and marital problems, with more women without a bad relationship scoring < 13 on the scale (95.9% [91.7-98.3%] vs. 76.5% [60.5-88.2%], p < 0.001).
Obstetric variables
Only one variable emerged as an obstetric risk factor: voluntary termination of pregnancy, with women who voluntarily terminate pregnancy having more positive screenings than women who do not (17.9% [12.8-24.0%] versus 9.0% [5.2-14.2%], p = 0.010). A higher percentage of women with a current planned pregnancy score < 13 on the scale (75.9% [68.4-82.3%] vs. 55.9% [39.3-71.5%], p = 0.019).
Weeks 29–30 of pregnancy (visit 2)
Ten sociodemographic, clinical, and obstetric variables were risk factors for positive screening responses at weeks 29–30.
Sociodemographic variables
Educational level, with illiterate women having higher percentages of positive screenings (27.5% [19.8-36.4%] versus 15.6% [11.1-21.1%], p = 0.019). Type of job position affects EPDS score, i.e., a higher percentage of skilled workers score < 13 (40.4% [30.7-50.8%] vs. 20.0% [7.2-40.8%], p = 0.019).
Clinical variables
Women with a history of depression show higher percentages of positive screenings (17.3% [11.1-25.1%] versus 7.0% [4.1-11.2%], p = 0.005), history of anxiety, with women with a history of previous anxiety showing higher percentages of positive screenings (35.5% [27.0%-44.7] versus 12.6% [8.5-17.7%], p < 0.001), prior psychological/psychiatric treatment, with women who received prior treatment having higher percentages of positive screenings (35.5% [27.0-44.7%] versus 10.1% [6.4-14.8%], p < 0.001), type of treatment (psychological and/or pharmacological), with women who have received some treatment having more cases of positive screening (cases with psychological treatment: 14.5% [8.9-22.0%] versus 1.0% [0.2-3.2%], p = 0 < 0.001), mistreated, with mistreated women having higher percentages of positive screenings (11.8% [6.8-18.8%] versus 3.0% [1.3-6.1%], p = 0.002), sexual abuse, with sexually abused women having higher percentages of positive screenings (5.5% [2.3-10.9%] versus 0.5% [0.1-2.3%], p = 0.009), and marital problems, with women who are in a bad relationship having higher percentages of positive screenings (10.0% [5.4-16.6%] versus 2.0% [0.7-4.7%], p = 0.003). More women without previous depression history score < 13 on the scale (89.0% [81.4-94.2%] vs. 55.0% [33.8-74.9%], p < 0.001), more women with previous anxiety history score ≥ 13 (55.0% [33.8-74.9%] vs. 30.8% [22.0-40.7%], p = 0.04), and marital problems, with more women without a bad relationship scoring < 13 (94.5% [88.4-97.9%] vs. 70.0% [48.3-86.4%], p = 0.004).
Obstetric variables
Two obstetric variables emerged as risk factors associated with screening responses at 29–30 weeks: previous spontaneous/deferred miscarriages, with women with previous spontaneous/deferred miscarriages having more positive screenings than women without (33.6% [25.3-42.8%] versus 16.6% [11.9-22.2%], p < 0.001), the level of current gestational risk, with a trend to show more positive screening for those women at higher risk (37.3% [28.7-46.5%] versus 21.1% [15.9-27.2%], Fisher exact test, p = 0.003). There were no associated obstetric risk factors at visit 2.
Week 4–6 postpartum (visit 3)
Eight sociodemographic, clinical and obstetric variables are risk factors for scoring ≥ 13 on the EPDS at week 4–6 postpartum.
Sociodemographic variables
Age is higher in patients scoring ≥ 13 on the EPDS (35.0 [18.0–45.0] years vs. 32.0 [18.0–44.0] years, p = 0.035),
Clinical variables
More women without previous depression history score < 13 (91.2% [87.2-94.2%] vs. 69.2% [50.2-84.2%], p < 0.001), more women without previous anxiety history score < 13 (81.9% [76.9-86.2%] vs. 50.0% [31.6-68.4%], p < 0.001), women without a previous psychological/psychiatric treatment score < 13 (83.5% [78.6-87.6%] vs. 50.0% [31.6-68.4%], p < 0.001), type of treatment (psychological and/or pharmacological), with women who have received both treatments scoring ≥ 13 (19.2 [7.7%-37.1] vs. women receiving only one type of treatment 4.2% [3.1-8.6%], p < 0.001), more non-mistreated women score < 13 (95.0% [91.8-97.2%] vs. 76.9% [58.5-89.7%], p = 0.004), and marital problems, with more women without a bad relationship scoring < 13 on the scale (97.3% [94.8-98.8%] vs. 73.1% [54.3-87.1%], p < 0.001).
Obstetric variables
A higher percentage of women with a current planned pregnancy score < 13 (78.8% [73.6-83.5%] vs. 61.5% [42.4-78.2%], p = 0.045).
See Supplementary Fig. 2 for a mapping of all risk factors.
Discussion
There is little evidence that screening to identify and treat depression during pregnancy improves outcomes. This may be due to variations in access to resources and appropriate treatment once a diagnosis of depression and/or anxiety has been established. However, screening for depression during pregnancy may provide some self-awareness of the risk of depression and anxiety. This study assesses for the first time the prevalence of anxiety and depression and their associated risk factors throughout the pregnancy and postpartum process in a large population of women attending the public health system, using a new screening tool for early detection of mental health problems.
Clinical screening for detecting anxiety and depression
Around the first trimester of pregnancy, just over half of the sample (53%) showed positive initial screening for symptoms of anxiety and depression. Assessing the EPDS score ≥ 13 at this time, we found that 10% of the entire sample required referral to the psychological/psychiatric service during the study, with a reduction in the percentage of women scoring ≥ 13 on the EPDS during the period of the visits, this reduction being most evident at the 29–30-week visit. We note that the first part of the screening alone showed that half of the women were potentially at risk, while the EPDS assessment gives more accurate values (around 19%). A total of 80 women out of 335 (23.9%) were ultimately referred for psychiatric assessment throughout the study. Although anxiety and depression vary considerably depending on the population assessed [8, 9], this is certainly a high percentage, higher than previously reported in other studies [2, 3, 5,6,7]. One possible reason is that most of the previous literature does not pay attention to mental health screening in early pregnancy, starting to assess women’s mental health problems in their second trimester of pregnancy [3, 5] or as already as postpartum [2, 5, 7].
Risk factors for positive anxiety and depression screening through Whooley and GAD-2 questions
There is a clear influence of a prior history of anxiety and depression on the initial positive screening, already in the first trimester of pregnancy and extending into the third trimester. Not only do the diagnoses of anxiety and depression tend to co-occur [33,34,35], but their risk factors appear to be similar. A history of anxiety or depression, or of previous psychiatric conditions, has been reported as a risk factor for anxiety and depressive symptoms not only in pregnant women [36] but also in other populations [37, 38]. So pregnant women with previous mental health conditions appear as a special target to be followed from the beginning of pregnancy.
We found smoking and the age to be risk factors for positive screening for anxiety and depression already in the first trimester. Increasing evidence suggests that smoking influences mental health negatively [39] and that there is a co-occurrence between depression/anxiety and smoking [40,41,42]. Although nicotine creates an instant feeling of relaxation, this feeling is momentary and soon gives way to withdrawal symptoms, increasing anxiety and tension. Nicotine stimulates the release of the chemical dopamine in the brain [43], which is initially involved in triggering positive feelings, but causes altered moods [44]. Reducing smoking rates in pregnancy is a priority [45]. Current evidence suggests that smoking is directly related to the onset of depressive and anxious symptoms early in pregnancy, so early action in this area appears to be of great benefit for mothers-to-be.
Adolescent mothers are known to experience health-related problems [46]. Younger age hinders economic and emotional stability for coping with financial, family, and social adversities. Younger mothers are more likely to be impoverished and to reside in socially and economically deprived families [47]. This can lead to anxiety and depression, especially during the postpartum period [48]. A very curious paradox appears in our data and that is that age appears as a differential risk factor pre- and postpartum, in an opposite way. We found that while in the early weeks of pregnancy, younger mothers are more likely to suffer anxiety and depression, in the postpartum period it is older mothers who show a greater tendency to depression. In the study of Agnafors et al. [48], only 3.5% of the sample are ≤ 20 years old, so the comparison with older mothers is quite unbalanced. Likewise, that study presents mothers with a mean age of 28 years (maximum range not shown). The mothers in that study are, on average, younger than the mothers included in our study, and their ages range from 18 to 45 years. Possibly the young mothers in that study had a specific casuistry that made them show more postpartum depression. In this sense, the characteristics of the mothers, their possibilities, coping skills, family and social support, and marital problems, among other factors, may come into play, as we shall discuss later.
Consistent with our postpartum findings, a previous study of pregnant women with a similar age range to those in our study (20–44 years) reported that older women had a higher risk of postpartum depression [49]. Possible reasons for this result could be multifactorial: the perception that older women find it more difficult to adapt to motherhood (because they have already had their lives structured for years, so there are difficulties in reconciling motherhood with work and personal life), and the lack of support from society due to prejudices in social norms around maternal age.
In this regard, we found that illiterate women had higher percentages of positive tests related to anxiety and depression. School dropout has been reported to be an even more influential factor in postpartum depressive symptoms than maternal age [47]. This factor appears to be influential throughout pregnancy from the beginning, so special attention should be paid to young and uneducated mothers in the first weeks of pregnancy.
Relationship problems (abuse and marital problems) seem to influence the likelihood of anxiety and depression in early pregnancy. The connection between any type of domestic violence and anxiety and depression is clear [50], affecting the mental health of pregnant women [51, 52]. It is essential to understand these aspects in the first weeks of pregnancy, to try to establish interventions aimed at minimizing these factors.
Difficulty in deciding whether to terminate a pregnancy voluntarily is an obvious cause of a mother’s anxiety and depression in early pregnancy, and it results in a risk of miscarriage in the third trimester. In both cases, it is a factor underlying the loss of the baby, but in early pregnancy, it is a personal decision, which increases the effect of regrets, etc., whereas in the third trimester, it is no longer voluntary, and the baby is lost for reasons other than personal decisions. Although depression has been found to occur up to eight times more frequently after childbirth than after miscarriage, it is also present in those cases [53]. Women who had a miscarriage scored higher on the anxiety and depression scale 10 days after miscarriage than the general population [53]. Although miscarriage is difficult to prevent in some cases, personal decisions about the termination of pregnancy can be worked on by professionals to reduce the impact of these decisions and offer support after the termination.
Risk factors for positive results on the EDPS
The positive EDPS result shows a similar trend to that found in the initial Whooley and the GAD-2 screening, i.e., psychiatric history and a history of anxiety and depression are the risk factors that recur at each stage of pregnancy as predisposing to symptoms of anxiety and depression in the pregnant mother, and in the postpartum period, together with abuse and marital problems. The economic situation and the emotional stability of the couple are also important. Compared to married mothers, single mothers report being more likely to have experienced an episode of depression [54].
Current planned pregnancy is associated with lower rates of anxiety and depression in early pregnancy, consistent with a previous study [55]. Pregnancy intention is a complex concept involving different psychological aspects (e.g., psychological adjustment to the presence of a future baby, willingness to change one’s current life with the presence of another family member). This psychological preparation is essential to minimize the impact of stress and depression processes. We found that family suicide may increase the risk of psychiatric problems in pregnant women. Strategies learned in the family environment for coping and for solving problems seem to be important in reducing psychiatric problems.
It may therefore no longer be a question of screening for possible depressive states, but of providing general coping strategies for the postpartum period in the early stages of pregnancy as a vital element, and not simply focusing on childcare responsibilities alone [56].
Limitations of the study
This study is not without limitations. First, although the sample is very large, its representativeness should be mentioned. Adolescent women are not represented in the current sample. Existing studies suggest that pregnant adolescents are at greater risk of suffering from depressive symptoms than pregnant and postpartum adult women [57,58,59]. Our percentages should therefore be contextualized considering the age of the sample, because the percentages may have been higher if adolescent mothers, with possible different risk factors for psychiatric symptoms, had been included. Also, women who are followed up in the private healthcare system are not part of the recruited sample. Significant differences have been reported in obstetric intervention rates between those with private and public health coverage [60,61,62]. It is well-known that private sector healthcare facilities are associated with a substantial increase in caesarean deliveries worldwide [63,64,65], even among low-risk obstetric births [61, 66], and this increase may also be related to anxiety and depression. Anxiety felt by women before caesarean section may cause psychological problems: most women are afraid of facing this procedure that may pose unnecessary risks for them, which is very significantly related to the level of stress or anxiety of patients [67]; also, prolonged anxiety and depression have been observed after this medical intervention [68]. However, this study aimed to evaluate a standardised protocol recommended by the public health system to assess how this new screening can assist in the early detection of psychological symptoms, thereby reducing the economic and clinical-staffing burden of monitoring established psychiatric disorders at later stages. Secondly, considering that religious beliefs appears as a powerful coping strategy to help deal with stressful situations [69], and that religion has been related to different coping strategies for pregnancy-related processes that dismisse psychological and psychiatric symptoms [70, 71], our study has not assessed whether this factor is influencing our results. Future studies should take this factor into account. Thirdly, the study did not include variables related to the time of delivery (e.g., type of delivery, complications, etc.), and perhaps these variables could affect the EPDS postpartum scores.
One of the strengths of this study is that, although there were sample losses, given the long period over which these women were being followed, the sample reduction was not high.
Conclusion
Although the existence of different antenatal, perinatal, and postnatal depression and anxiety risk factors in this cohort is of concern, screening in the first trimester of pregnancy may improve the mental health status of pregnant women, as well as reduce the subsequent burden in the mental health system. Care for young mothers in the early weeks and for older mothers during the postpartum period seems to be crucial.
The schedule of visits and follow-ups for pregnant women is likely to differ in the public health system from what is usually done in private practices, and a quick screening seems to be very useful to detect women potentially targeted for referral for diagnosis and assessment of psychological/psychiatric pathology in early stages, to catch them in time and prevent the disorder from becoming chronic, which would involve more expense and more effort from medical staff.
The fact that this protocol allows early psychological and psychiatric screening of pregnant women through the midwife is very valuable, as it reduces the burden of the medical staff who carry out the psychological assessments.
Data availability
The datasets and materials utilized in this study are available upon reasonable request from the corresponding author. Access to these resources is subject to ethical and legal constraints, and data-sharing will be in compliance with institutional and regulatory guidelines. Researchers interested in obtaining the data and materials should contact the corresponding author to initiate the request process. Please provide a detailed rationale for the request, and we will strive to facilitate access following applicable policies.
For proprietary or confidential information that cannot be shared, summaries or excerpts that maintain the integrity of the research outcomes may be provided upon request.
The study was conducted under ethical approvals and data protection regulations, and any data-sharing will be carried out while upholding participant confidentiality and data privacy.
References
Generalitat de Catalunya D, de Salut. 2018. Protocol de seguiment de l’embaràs a Catalunya. https://www.bio-centre.ad/Uploads/Noticies/protocol-seguiment-embaras-2018_def.pdf.
Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH. Perinatal anxiety disorder prevalence and incidence. J Affect Disord. 2016;200:148–55. https://doi.org/10.1016/j.jad.2015.12.082.
Giardinelli L, Innocenti A, Benni L, Stefanini MC, Lino G, Lunardi C, Svelto V, Afshar S, Bovani R, Castellini G, Faravelli C. Depression and anxiety in perinatal period: prevalence and risk factors in an Italian sample. Arch Womens Ment Health. 2012;15:21–30. https://doi.org/10.1007/s00737-011-0249-8.
Navarro P, García-Esteve L, Ascaso C, Aguado J, Gelabert E, Martín-Santos R. Non-psychotic psychiatric disorders after childbirth: prevalence and comorbidity in a community sample. J Affect Disord. 2008;109:171–6. https://doi.org/10.1016/j.jad.2007.10.008.
Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139–49. https://doi.org/10.2471/BLT.11.091850. G.
Hendrick V, Altshuler L, Cohen L, Stowe Z. Evaluation of mental health and depression during pregnancy: position paper. Psychopharmacol Bull. 1998;34:297–9.
O’Hara M, Swain A. Rates and risk of Postpartum Depression-a Meta-analysis. Int Rev Psychiatry. 2009;8:37–54. https://doi.org/10.3109/09540269609037816.
Leach LS, Poyser C, Fairweather-Schmidt K. Maternal perinatal anxiety: a review of prevalence and correlates. Clin Psychol. 2017;21:4–19. https://doi.org/10.1111/cp.12058.
Goodman JH, Chenausky KL, Freeman MP. Anxiety disorders during pregnancy: a systematic review. J Clin Psychiatry. 2014;75:e1153–1184. https://doi.org/10.4088/JCP.14r09035.
Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35. https://doi.org/10.1016/j.bpobgyn.2013.08.017.
Van den Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioral development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005;29:237–58. https://doi.org/10.1016/j.neubiorev.2004.10.007.
Goodwin R, Keyes K, Simuro N. Mental disorders and Nicotine Dependence among pregnant women in the United States. Obstet Gynecol. 2007;109:875–83. https://doi.org/10.1097/01.AOG.0000255979.62280.e6.
Meshberg-Cohen S, Svikis D. Panic disorder, trait anxiety, and alcohol use in pregnant and nonpregnant women. Compr Psychiatr. 2007;48:504–10. https://doi.org/10.1016/j.comppsych.2007.06.004.
Ventura SJ, Hamilton BE, Mathews TJ, Chandra A. Trends and variations in smoking during pregnancy and low birth weight: evidence from the birth certificate, 1990–2000. Pediatrics. 2003;111:1176–80.
Parackal S, Ferguson E, Harraway J. Alcohol and tobacco consumption among 6-24-months post-partum New Zealand women. Matern Child Nutr. 2007. https://doi.org/10.1111/J.1740-8709.2007.00064.X.
Andersson L, Sundström-Poromaa I, Wulff M, Aström M, Bixo M. Implications of antenatal depression and anxiety for obstetric outcome. Obstet Gynecol. 2004;104:467–76. https://doi.org/10.1097/01.AOG.0000135277.04565.e9.
Waldenström U, Hildingsson I, Ryding EL. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. 2006;113:638–46. https://doi.org/10.1111/j.1471-0528.2006.00950.x.
Farré-Sender B, Torres A, Gelabert E, Andrés S, Roca A, Lasheras G, Valdés M, Garcia-Esteve L. Mother-infant bonding in the postpartum period: assessment of the impact of pre-delivery factors in a clinical sample. Arch Womens Ment Health. 2018;21:287–97. https://doi.org/10.1007/s00737-017-0785-y.
Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO collaborative study on psychological problems in General Health Care. JAMA. 1994;272:1741–8. https://doi.org/10.1001/jama.272.22.1741.
Talge NM, Neal C, Glover V, Stress E. Translational Research and Prevention Science Network: fetal and neonatal experience on child and Adolescent Mental Health, 2007. Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry 48, 245–61. https://doi.org/10.1111/j.1469-7610.2006.01714.x.
Coussons-Read ME. Effects of prenatal stress on pregnancy and human development: mechanisms and pathways. Obstet Med. 2013;6:52–7. https://doi.org/10.1177/1753495X12473751.
Kinsella MT, Monk C. Impact of maternal stress, Depression & anxiety on fetal Neurobehavioral Development. Clin Obstet Gynecol. 2009;52:425–40. https://doi.org/10.1097/GRF.0b013e3181b52df1.
Ruiz RJ, Avant KC. Effects of maternal prenatal stress on infant outcomes: a synthesis of the literature. ANS Adv Nurs Sci. 2005;28:345–55. https://doi.org/10.1097/00012272-200510000-00006.
Berger A, Bachmann N, Signorell A, Erdin R, Oelhafen S, Reich O, Cignacco E. Perinatal mental disorders in Switzerland: prevalence estimates and use of mental-health services. Swiss Med Wkly. 2017;147:w14417. https://doi.org/10.4414/smw.2017.14417.
Bauer A, Knapp M, Parsonage M. Lifetime costs of perinatal anxiety and depression. J Affect Disord. 2016;192:83–90. https://doi.org/10.1016/j.jad.2015.12.005.
Simpson W, Glazer M, Michalski N, Steiner M, Frey BN. Comparative efficacy of the generalized anxiety disorder 7-Item Scale and the Edinburgh Postnatal Depression Scale as screening tools for generalized anxiety disorder in pregnancy and the Postpartum Period. Can J Psychiatry. 2014;59:434–40.
National Institute for Health and Care Excellence (NICE). Antenatal and postnatal mental health: clinical management and service guidance. 2020. https://www.nice.org.uk/guidance/cg192.
Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–45. https://doi.org/10.1046/j.1525-1497.1997.00076.x.
Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004.
Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using generalized anxiety Disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12(e8224). https://doi.org/10.7759/cureus.8224.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. https://doi.org/10.1001/archinte.166.10.1092.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–6. https://doi.org/10.1192/bjp.150.6.782.
Choi KW, Kim Y-K, Jeon HJ. Comorbid anxiety and depression: clinical and conceptual consideration and Transdiagnostic Treatment. Adv Exp Med Biol. 2020;1191:219–35. https://doi.org/10.1007/978-981-32-9705-0_14.
Garber J, Weersing VR. Comorbidity of anxiety and depression in Youth: implications for treatment and Prevention. Clin Psychol (New York). 2010;17:293–306. https://doi.org/10.1111/j.1468-2850.2010.01221.x.
Pollack MH. Comorbid anxiety and depression. J Clin Psychiatry. 2005;66(Suppl 8):22–9.
Ahmed A, Bowen A, Feng CX, Muhajarine N. Trajectories of maternal depressive and anxiety symptoms from pregnancy to five years postpartum and their prenatal predictors. BMC Pregnancy Childbirth. 2019;19:26. https://doi.org/10.1186/s12884-019-2177-y.
Stafford L, Judd F, Gibson P, Komiti A, Mann GB, Quinn M. Anxiety and depression symptoms in the 2 years following diagnosis of breast or gynaecologic cancer: prevalence, course and determinants of outcome. Support Care Cancer. 2015;23:2215–24. https://doi.org/10.1007/s00520-014-2571-y.
Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, Li W, Xiao S. 2020. Prevalence and influencing factors of anxiety and depression symptoms in the First-Line Medical Staff fighting against COVID-19 in Gansu. Frontiers in Psychiatry 11.
Bruijnzeel AW. Tobacco Addiction and the dysregulation of brain stress systems. Neurosci Biobehav Rev. 2012;36:1418–41. https://doi.org/10.1016/j.neubiorev.2012.02.015.
Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19:3–13. https://doi.org/10.1093/ntr/ntw140.
Mykletun A, Overland S, Aarø LE, Liabø H-M, Stewart R. Smoking in relation to anxiety and depression: evidence from a large population survey: the HUNT study. Eur Psychiatry. 2008;23:77–84. https://doi.org/10.1016/j.eurpsy.2007.10.005.
Skov-Ettrup LS, Nordestgaard BG, Petersen CB, Tolstrup JS. Does high Tobacco Consumption cause psychological distress? A mendelian randomization study. Nicotine Tob Res. 2017;19:32–8. https://doi.org/10.1093/ntr/ntw186.
Di Chiara G. Role of dopamine in the behavioural actions of nicotine related to addiction. Eur J Pharmacol. 2000;393:295–314. https://doi.org/10.1016/s0014-2999(00)00122-9.
Picciotto MR, Brunzell DH, Caldarone BJ. Effect of nicotine and nicotinic receptors on anxiety and depression. NeuroReport. 2002;13:1097–106. https://doi.org/10.1097/00001756-200207020-00006.
Diamanti A, Papadakis S, Schoretsaniti S, Rovina N, Vivilaki V, Gratziou C, Katsaounou PA. Smoking cessation in pregnancy: an update for maternity care practitioners. Tob Induc Dis. 2019;17:57. https://doi.org/10.18332/tid/109906.
Lesser J, Escoto-Lloyd S. Health-related problems in a vulnerable population: pregnant teens and adolescent mothers. Nurs Clin North Am. 1999;34:289–99.
Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the Mental Health needs of pregnant and parenting adolescents. Pediatrics. 2014;133:114–22. https://doi.org/10.1542/peds.2013-0927.
Agnafors S, Bladh M, Svedin CG, Sydsjö G. Mental health in young mothers, single mothers and their children. BMC Psychiatry. 2019;19:112. https://doi.org/10.1186/s12888-019-2082-y.
Muraca GM, Joseph KS. The association between maternal age and depression. J Obstet Gynaecol Can. 2014;36:803–10. https://doi.org/10.1016/S1701-2163(15)30482-5.
Malik M, Munir N, Ghani MU, Ahmad N. Domestic violence and its relationship with depression, anxiety and quality of life: a hidden dilemma of Pakistani women. Pak J Med Sci. 2021;37:191–4. https://doi.org/10.12669/pjms.37.1.2893.
Gharacheh M, Azadi S, Mohammadi N, Montazeri S, Khalajinia Z. Domestic violence during pregnancy and women’s Health-Related Quality of Life. Glob J Health Sci. 2015;8:27–34. https://doi.org/10.5539/gjhs.v8n2p27.
Tavoli Z, Tavoli A, Amirpour R, Hosseini R, Montazeri A. Quality of life in women who were exposed to domestic violence during pregnancy. BMC Pregnancy Childbirth. 2016;16:19. https://doi.org/10.1186/s12884-016-0810-6.
Ambriz-López R, Guerrero-González G, Rodríguez-Valero CG, Treviño-Montemayor OR, Guzmán-López A, Saldívar-Rodríguez D. Evaluation of symptoms of anxiety and depression in patients with a miscarriage. Med Universitaria. 2017;19:7–12. https://doi.org/10.1016/j.rmu.2017.02.005.
Cairney J, Boyle M, Offord DR, Racine Y. Stress, social support and depression in single and married mothers. Soc Psychiatry Psychiatr Epidemiol. 2003;38:442–9. https://doi.org/10.1007/s00127-003-0661-0.
Barton K, Redshaw M, Quigley MA, Carson C. Unplanned pregnancy and subsequent psychological distress in partnered women: a cross-sectional study of the role of relationship quality and wider social support. BMC Pregnancy Childbirth. 2017;17:44. https://doi.org/10.1186/s12884-017-1223-x.
Corrigan CP, Kwasky AN, Groh CJ. Social Support, Postpartum Depression, and Professional Assistance: a survey of mothers in the Midwestern United States. J Perinat Educ. 2015;24:48–60. https://doi.org/10.1891/1058-1243.24.1.48.
Kamalak Z, Köşüş N, Köşüş A, Hizli D, Akçal B, Kafali H, Canbal M, Isaoğlu Ü. Adolescent pregnancy and depression: is there an association? Clin Exp Obstet Gynecol. 2016;43:427–30.
Reid V, Meadows-Oliver M. Postpartum depression in adolescent mothers: an integrative review of the literature. J Pediatr Health Care. 2007;21:289–98. https://doi.org/10.1016/j.pedhc.2006.05.010.
Siegel RS, Brandon AR. Adolescents, pregnancy, and mental health. J Pediatr Adolesc Gynecol. 2014;27:138–50. https://doi.org/10.1016/j.jpag.2013.09.008.
Craven S, Byrne F, Mahony R, Walsh JM. Do you pay to go private? A single centre comparison of induction of labour and caesarean section rates in private versus public patients. BMC Pregnancy Childbirth. 2020;20:746. https://doi.org/10.1186/s12884-020-03443-4.
Dahlen HG, Tracy S, Tracy M, Bisits A, Brown C, Thornton C. Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000–2008): a linked data population-based cohort study. BMJ Open. 2014;4:e004551. https://doi.org/10.1136/bmjopen-2013-004551.
Hoxha I, Syrogiannouli L, Braha M, Goodman DC, da Costa BR, Jüni P. Caesarean sections and private insurance: systematic review and meta-analysis. BMJ Open. 2017;7:e016600. https://doi.org/10.1136/bmjopen-2017-016600.
Belizán JM, Althabe F, Cafferata ML. Health consequences of the increasing caesarean section rates. Epidemiology. 2007;18:485–6. https://doi.org/10.1097/EDE.0b013e318068646a.
Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The increasing Trend in caesarean section rates: Global, Regional and National estimates: 1990–2014. PLoS ONE. 2016;11:e0148343. https://doi.org/10.1371/journal.pone.0148343.
Bhatia M, Banerjee K, Dixit P, Dwivedi LK. Assessment of Variation in Cesarean Delivery Rates between Public and Private Health Facilities in India from 2005 to 2016. JAMA Netw Open. 2020;3:e2015022. https://doi.org/10.1001/jamanetworkopen.2020.15022.
Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, Moller A-B, Say L, Hosseinpoor AR, Yi M, Neto D, de Temmerman LR, M. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392:1341–8. https://doi.org/10.1016/S0140-6736(18)31928-7.
Hepp P, Hagenbeck C, Burghardt B, Jaeger B, Wolf OT, Fehm T, Schaal NK, Group MAGIC. Measuring the course of anxiety in women giving birth by caesarean section: a prospective study. BMC Pregnancy Childbirth. 2016;16:113. https://doi.org/10.1186/s12884-016-0906-z.
Janssen AB, Savory KA, Garay SM, Sumption L, Watkins W, Garcia-Martin I, Savory NA, Ridgway A, Isles AR, Penketh R, Jones IR, John RM. Persistence of anxiety symptoms after elective caesarean delivery. BJPsych Open. 2018;4:354–60. https://doi.org/10.1192/bjo.2018.48.
Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. 2005;61:461–80. https://doi.org/10.1002/jclp.20049.
Hamilton JG, Lobel M. Types, patterns, and predictors of coping with stress during pregnancy: examination of the revised prenatal coping inventory in a diverse sample. J Psychosom Obstet Gynecol. 2008;29:97–104. https://doi.org/10.1080/01674820701690624.
Peñacoba-Puente C, Carmona-Monge FJ, Marín-Morales D, Naber K. Coping strategies of Spanish pregnant women and their impact on anxiety and depression. Res Nurs Health. 2013;36:54–64. https://doi.org/10.1002/nur.21513.
Acknowledgements
We express our gratitude to all the women who participated in this study. We extend our appreciation to the healthcare services that facilitated the recruitment of the current sample, including CAP Rambla, CAP Sud, CAP Rubí, CAP Can Mates, CAP Olesa, CAP Oest, and CAP Can Tries, located in Catalonia, Spain. We also wish to acknowledge the dedicated efforts of the midwives responsible for the recruitment of the participants in this study.
Funding
Marta Jiménez-Barragan received a PERIS grant (2018–2020) from the Departament de Salut, Generalitat de Catalunya (Grant No. PERIS SLT006/17/249).
This study had been funded partially by the Official College of Nurses of Barcelona (www.coib.cat) as part of the Nurse Research Projects Grants (PR-642/2023).
This study received the Mustela Scholarship for midwifery research projects awarded by the Mustela Foundation (FAME 2023).
Author information
Authors and Affiliations
Contributions
M.JB: Conceptualization, Methodology, Software, Investigation, Writing and Original Draft Preparation.G.FP: Methodology, Writing - Original Draft Preparation.JJ.CG: Software, Formal Analysis.O.MR: Investigation, Resources, Writing - Original Draft Preparation.E.CN: Visualization, Investigation.M.TG: Investigation, Resources.O.ER: Investigation, Resources.A.CR: Software, Validation.L.CC: Methodology, Investigation.X.UB: Supervision.A.DG: Writing - Reviewing and Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Clinical Research Ethics Committee (CEIC) of the Mutua Terrassa (Spain) (# approval: B1803) and was conducted in accordance with the principles of the Declaration of Helsinki (World Medical Association Declaration of Helsinki, 1997) and its later amendments (revised in 2013). Informed written consent was obtained from all the participants.
Consent for publication
I, Marta Jimenez-Barragan, hereby extend my consent for the publication of my manuscript titled “Prevalence of Anxiety and Depression and Their Associated Risk Factors Throughout Pregnancy and Postpartum: A Prospective Cross-Sectional Descriptive Multicentred Study” in the BMC Nursing journal. I assume the role of corresponding author and hold ownership of the intellectual property rights affiliated with this manuscript. Consent to publish has been obtained from all study participants. In offering this consent, I acknowledge and authorize BMC Nursing to exercise the non-exclusive privilege to publish, reproduce, distribute, and publicly display the manuscript as mentioned above in all formats and media. Additionally, I grant BMC Nursing the right to employ my name, affiliation, and any biographical information furnished in connection with the publication. I validate the originality of the manuscript, affirming that it has not been previously published elsewhere and is not presently under consideration for publication in any other journal. I have diligently acknowledged the contributions of other individuals by duly citing their work, and I have secured all necessary permissions for any copyrighted material integrated within the manuscript. I want to clarify that the manuscript does not contain any identifying information or images of patients. Understanding that BMC Nursing will diligently strive to ensure the precision and integrity of the published work, I assume full responsibility for the content of the manuscript, as well as any pertinent data, figures, or supplementary materials. I recognize that the peer review process and editorial decisions fall within the jurisdiction of BMC Nursing, and I pledge my cooperation with any revisions or recommendations put forth by the editorial team. I commit to promptly addressing any queries or revision requests initiated by the editorial team, and I will provide essential clarifications or additional information as necessitated. I am cognizant that the publication of the manuscript is subject to the terms and conditions outlined by BMC Nursing, and I hereby express my agreement to adhere to these stipulations. By appending my signature to this consent for publication, I affirm that I have comprehensively read and understood the statements. Furthermore, I assert my authority to provide this consent on behalf of all co-authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jimènez-Barragan, M., Falguera-Puig, G., Curto-Garcia, J.J. et al. Prevalence of anxiety and depression and their associated risk factors throughout pregnancy and postpartum: a prospective cross-sectional descriptive multicentred study. BMC Pregnancy Childbirth 24, 500 (2024). https://doi.org/10.1186/s12884-024-06695-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06695-6