Abstract
Background
Breast milk is the first, highly valuable, and solely natural food recommended for infants in their first six months of life, which is critical for children's overall growth and development. Evidence suggests that exclusive breastfeeding differs by geographic area in Ethiopia. However, little is known regarding the geographic distribution of exclusive breastfeeding practice. Hence, this study aimed to assess exclusive breastfeeding practice, its geographic variation and associated factors among Ethiopian mothers.
Method
The study used the 2019 Ethiopian mini demographic and health survey data. All living children born 0–23 months before the survey were included. Global Moran’s I statistics on Arc-GIS and Getis Ord Gi* statistics was used to visualize the spatial pattern and hotspot and cold spot areas, respectively. Kulldorff SaTScan was used to show purely significant spatial clusters. The associated factors were identified using a multilevel mixed-effects logistic regression model. Statistically significant factors were reported using the AOR with a 95% CI and a p-value of < 5%.
Result
The coverage of exclusive breastfeeding practice in Ethiopia was 56.05% (95% CI: 53.95%, 58.10%). The spatial pattern was non-random across the country’s regions. Somalia, Gambela, Benshangul Gumuz, Dire Dawa, and Harari regions had low clustering of exclusive breastfeeding practices, whereas Amhara, Eastern SNNPR, and Central and Northern Oromia regions had high clustering. Children born through caesarean delivery [AOR = 0.36; 95% CI: 0.21, 0.63], initiated breastfeeding within the first 1 h [AOR = 0.55; 95% CI: 0.34, 0.90], after 1–24 h of delivery [AOR = 0.36; 95% CI: 0.24, 0.54], after a day [AOR = 0.04; 95% CI: 0.02, 0.08], and women residing in the pastoralist region [AOR = 0.22; 95% CI: 0.12, 0.39] or city administrations [AOR = 0.49; 95% CI: 0.27, 0.89] had lower odds of exclusive breastfeeding practice.
Conclusion
Exclusive breastfeeding practice in Ethiopia remained low. The practice had a spatial variation across the country. Caesarean section delivery, late breastfeeding initiation, and region were statistically significant variables. Therefore, promoting timely initiation of breastfeeding and improving the utilization of maternal health services and designing special intervention strategy for women residing in city administrations and pastoralist regions of the country may increase the coverage of exclusive breastfeeding practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Exclusive breastfeeding is a practice in which infants receives only breast milk and no other food item in the form of solid, semi-solid or liquid including water except oral rehydration solution, drops/syrups of vitamins, minerals or medicines [1]. Breast milk is a natural food that contains all essential nutrients for the child survival, growth, and overall development. Thus, World Health Organization (WHO) recommends exclusive breastfeeding for the first six months of life. Breastfeeding the young children (above 6 months) should be continued up to two years and above along with complementary foods [2,3,4].
Improving child survival and healthy growth and development can be achieved through collective efforts made in the key area, infant and young child feeding. Optimal breastfeeding practice is the most effective, safe and top intervention which result in the reduction of morbidity and mortality of under five children [5, 6]. Exclusive breastfeeding has several health benefits for both the mother and newborn. It minimizes the risk of postpartum hemorrhage, ovarian and breast cancer, type 2 diabetes, conception in the first six months of delivery, and health costs incurred due to gastrointestinal infections caused by prelacteal feeding [7]. Evidence indicated that initiation of breastfeeding within the first one hour of birth and practicing exclusive breastfeeding in the first 6 months of birth alone is assumed to halt the death of neonates by 20% [8]. Moreover, studies have revealed that promoting exclusive breastfeeding practice can avert 55% of infant mortality in Latin America and the Caribbean due to diarrhea and severe respiratory infections [9].
Globally, the prevalence of exclusively breastfed infants in 2023 was 44% [5]. In Sub-Saharan Africa, the average coverage of exclusive breastfeeding was 50% between 2015 and 2019 [10]. Similarly, coverage varied from 22% in Nigeria to 70% in Malawi, according to data collected from 19 African nations between 2013 and 2019 [11]. Likewise, the pooled prevalence of exclusive breastfeeding practice among infants under six months in Ethiopia from 2015 to 2020 was 60.42% [12]. However, achieving the at least 70% target of exclusive breastfeeding in 94 low-or middle-income countries (LMICs) that had low exclusive breastfeeding rates is highly unlikely [13].
A number of studies conducted in the different parts of the country, east Africa and sub-Saharan Africa identified various factors that affect the practice of exclusive breastfeeding. Employment status, maternal age, educational level, marital status, institutional delivery, mode of delivery, infant age, ANC visit, timely initiation of breastfeeding, place of residence, and geographic region were factors associated with exclusive breastfeeding practice [10, 14,15,16,17,18,19,20,21,22].
The many efforts launched by the Ethiopian government to promote timely initiation and exclusive breastfeeding practice in the country failed to effectively overcome the gap. According to Ethiopian Demographic and Health Survey (EDHS) report, the progress observed in the prevalence of the exclusive breastfeeding practice almost in the last two decades was only 10%, it was 49% in 2005 and 59% in 2019 [23]. With this progression, it will be very difficult for the country to achieve the expected United Nations (UN) goal. The current prevalence is much below than the planned UN goal of 70% by 2030, indicating the need for further investigation. Moreover, few nationwide studies in Ethiopia have been undertaken on the relationship between individual and community-level factors and exclusive breastfeeding practice.
Evidence has shown that exclusive breastfeeding practices vary by geographical location in Ethiopia [18, 24]. Previous studies have revealed that maternal educational level, socio-cultural differences across geographic regions, household economic status, and access to and use of maternal and child health services all have a significant impact on exclusive breastfeeding [16, 18, 24,25,26,27]. These qualities are strongly influenced by one's place of residence or geographical region. And there is a lack of research, particularly on exclusive breastfeeding and its geographical variance. Spatial analysis is important because it allows you to find high and low burden areas in regard to the variable of interest in the country.
As a result, there is a need to investigate individual and community-level factors influencing exclusive breastfeeding practice. The study's findings will enable policymakers and planners to develop and implement effective area-specific interventions to enhance exclusive breastfeeding practice, which help to accomplish the sustainable development goal and reduce maternal and infant mortality in Ethiopia. Therefore, the purpose of this study was to investigate the regional distribution as well as individual and community-level factors associated with exclusive breastfeeding among Ethiopian children aged 0 to 23 months.
Methods
Study settings and data source
Ethiopia is a country located in the Northeastern part of Africa (horn of Africa). It is the second most populous country in Africa, next to Nigeria. The country consists of 9 regions and 2 city administrations at the time of the original survey. Demographic and Health Survey (DHS) is a nationally representative household survey usually conducted in every five-year time interval. For this analysis, we used the 2019 Ethiopian Mini Demographic and Health Survey (EMDHS) data.
Study design and sampling procedures
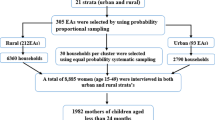
A community-based cross-sectional study design was conducted in Ethiopia between March 21, 2019 and June 28, 2019 among 9,012 eligible women identified for individual interviews. However, interviews were done with 8,885 women, giving a response rate of 99%. The EMDHS uses a multistage stratified cluster sampling design to collect data from study participants. Initially, country is first divided into geographic regions, which are then further divided into urban and rural sectors. The required number of enumeration areas (EA) within each region were picked at random using the sampling frame designed for the 2019 Ethiopian population and housing census. The frame includes information on the EA's location, type of dwelling (urban or rural), and the projected number of residential households. To make the sample comparable across regions, 25 EAs were picked from eight regions of the country, and 35 EAs were selected from each bigger region, namely Oromia, Amhara, and Southern Nations, Nationalities, and Peoples' Region (SNNPR). Accordingly, a total of 305 EAs (93 in urban and 212 in rural areas) were chosen for the 2019 EMDHS using a probability proportional to their size. Following that, a household listing procedure was carried out in each selected EA. Finally, 30 households per cluster were selected using equal probability systematic selection from the previously produced list. The DHS guide provides additional information on survey sampling strategies [23].
Source and study population
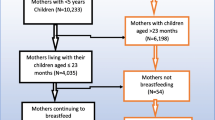
Eligible women for the 2019 EMDHS include all women aged 15 to 49 who were either permanent residents of the selected households or guests who slept in the household the night prior to the survey. However, our research used all live children born in the two years preceding the survey as the source population. The study population consisted of all youngest children (midx = 1) living with their mother in the selected EAs and born 0 to 23 months before the survey. The last-born child data was collected if the mother have two or more under 24 months old children. However, mothers who had twin birth for the most recent birth were asked for both children. In this study, missing data is managed as not currently breastfeeding in numerator and included in the denominator. Consequently, we included 2,052 under 24 months children data extracted from the 2019 EMDHS datasets (KR file) that satisfy the inclusion criteria.
Eligibility criteria
This analysis included, all mothers who gave birth in the last two years before the survey. In addition, we considered all women who live with their children and were breastfed but not given anything else in the 24 h preceding the interview (Fig. 1).
Measurement of variables
Dependent variable
The outcome variable of the study was exclusive breastfeeding practice among mothers with children under 24 months in Ethiopia. It was measured in two ways based on the age group of the children. For infants aged 0 to 5 months (< 6 months), mothers were asked if they breastfed and given nothing else except medications in the 24 h before the interview. Mothers of children aged 6 to 23 months were questioned if they breastfed and given nothing else while their children were under six months old [28, 29]. DHS used the information on exclusive breastfeeding collected from mothers’ verbal responses. Thus, the response variable was coded as “1” if the mother breastfed and provided nothing else in the day before the interview for children under 6 months, or if the mother responded as breastfed and given nothing else based on her dietary recall from birth for children aged 6 to 23 months and “0” otherwise.
Independent variables
The individual-level factors included in the analysis were maternal socio-demographic variables (such as maternal age, maternal education, marital status, religion, sex of household head, family size, and household wealth index); and infant related variables (like age of the child, sex of the child, birth order number, birth interval, number of living children, time of breastfeeding initiation, and duration of breastfeeding). And obstetric and health service related variables such as timing of 1st antenatal care (ANC), number of ANC visits, place of delivery, mode of delivery, delivery assistance, postnatal care (PNC), and age of respondent at 1st birth were also included.
Community-level factors like geographic regions, type of place of residence, community women education, community ANC utilization, and community poverty level were considered in this study (Table 1).
Data processing and analysis
We used STATA/SE version 14.0 to process and analyze the data. The study used descriptive statistics to report frequency and proportion of each independent variables. In the DHS survey, children are nested within households, which are then nested within clusters. As a result, children from the same clusters are more similar to each other in terms of the outcome variable as compared to those from different cluster. Individual observations in such data are not independent, which contradicts the assumption of independence of observations. Therefore, we used a multilevel mixed-effects logistic regression model to tackle the violation of independent observation and equal variance assumption of the traditional logistic regression that occurred due to the hierarchical structure of the DHS data. Hence, four models were fitted within the multilevel multivariable mixed-effects logistic regression analysis. The null model, without independent variables, was fitted first. This model was applied to test the null hypothesis that there is no cluster level difference in the outcome variable and to justify the use of multilevel analysis by obtaining the intra-class correlation coefficient (ICC). Secondly, a model with only individual-level factors was fitted. This model assumes that there is no difference in exclusive breastfeeding practice between clusters. Likewise, Model II (with only community-level factors) was constructed to assess community-level determinants using aggregate cluster variations in exclusive breastfeeding practice. Finally, mixed model, Model III, was fitted to test both the fixed and random effects of individual and community-level determinants on the exclusive breastfeeding practice. Variable with p-value < 0.25 were selected for the multilevel multivariable analysis. Finally, Adjusted Odds Ratio (AOR) with 95% confidence interval and p-value less than 5% was used to report statistically significant variables with the exclusive breastfeeding practice. We checked the goodness of fit of the model by Akaike information criterion (AIC), and Bayesian information criterion (BIC). AIC is computed as -2 (log-likelihood of the fitted model) + 2p, where p is the degree of freedom in the model. Similarly, BIC is calculated as -2 (log-likelihood of the fitted model) + ln (N)*p. The value of ICC of each model can be also calculated by using STATA software command (estat icc). The model with the lowest deviance (-2 log-likelihood) was selected as a best explanatory model. Also, multicollinearity amongst the covariates was examined using the Variance Inflation Factor (VIF).
Spatial analysis
The spatial analysis was carried out using ArcGIS 10.7 and SatScan 9.6. The weighted frequency of outcome variable with cluster number was cross tabulated using STATA software and exported to excel to get the case to total proportion. The excel file was then imported into Arc-GIS 10.7, and geographic coordinate data was joined with non-spatial data using each EA’s (Enumeration Area) unique identification code for spatial analysis. To produce the map of Ethiopia, the Ethiopian Poly-conic Projected Coordinate System was used. The units of spatial analysis were DHS clusters (Since geographic coordinates of EDHS were collected at cluster level).
Spatial autocorrelation analysis
To evaluate whether the pattern of outcome variable is clustered, dispersed, or random across the study areas, global spatial autocorrelation was assessed using the Global Moran’s-I statistics. Moran’s I is a spatial statistic used to measure spatial autocorrelation by taking the entire data set and produce a single output value which ranges from -1 to + 1. Moran’s I Values close to − 1 indicate the pattern is dispersed, whereas moron’s I close to + 1 indicates clustered and distributed randomly if the value is zero. A statistically significant Moran’s I (p < 0.05) lead to rejection of the null hypothesis (exclusive breastfeeding is randomly distributed) and indicates the presence of spatial autocorrelation and needs further local analysis. Anselin Local Moran’s I used to investigate at exclusive breastfeeding cluster locations at the local level, whether they were positively correlated (high-high and low-low) or negatively correlated (high-low and low–high). A positive value for ‘I’ indicated that a case had neighboring cases with similar values, part of a cluster. A negative value for ‘I’ indicated that a case was surrounded by cases with dissimilar values.
Host spot and cold spot analysis
Getis-Ord Gi* statistics was computed to measure how spatial autocorrelation varies over the study location by calculating Gi* statistic for each area. Z-score also computed to determine the statistical significance of clustering, and the p-value for the significance. The Getis-Ord Gi* statistic identified spatial clusters of high values (hotspots) and spatial clusters of low values (coldspots). Gi* serves as an indicator of local autocorrelation, i.e. it measures how spatial autocorrelation varies locally over an area and provide statistic for each data points. If z-score is higher, the intensity of the clustering is stronger and Z-score near zero indicates no apparent clustering. A positive z-score indicates clustering of high values and a negative z-score indicates clustering of low values.
Spatial interpolation
Spatial interpolation was done to estimate values for spatial locations with unknown value using known values. Among various deterministic and geo-statistical interpolation methods ordinary Kriging and empirical Bayesian are considered the best method since both incorporates the spatial autocorrelation and statistically optimizes the weight. For this study Ordinary Kriging spatial interpolation method was used to predict of exclusive breastfeeding in un-sampled areas in the country based on the value in sampled EAs.
Spatial scan statistical analysis
Spatial scan statistical analysis Bernoulli based model was employed to test for the presence of statistically significant spatial clusters of exclusive breastfeeding using SaTScan version 9.6. The spatial scan statistic uses a circular scanning window that moves across the study area. Women who give only breast milk for their child were taken as cases and those who give other food in addition to breast milk as controls to fit the Bernoulli model. The numbers of cases in each location had Bernoulli distribution and the model required data for cases, controls, population and geographic coordinates. For each potential cluster, a likelihood ratio test statistic and p-value was computed to determine whether the number of observed exclusive breastfeeding within the potential cluster was significantly higher than expected or not. The scanning window with maximum likelihood was the most likely performing cluster, and p-value was assigned to each cluster using Monte Carlo hypothesis testing by comparing the rank of the maximum likelihood from the real data with the maximum likelihood from the random datasets. The primary and secondary clusters were identified and assigned p-values and ranked based on their likelihood ratio test, on the basis of 999 Monte Carlo replications.
Ethical consideration
The MEASURE DHS team obtained ethical clearance from the Ethiopian Health Nutrition and Research Institute (EHNRI) Review Board and the National Research Ethics Review Committee (NRERC) at the Ministry of Science and Technology of Ethiopia. Thus, this study used secondary data from DHS data files. The authors formally requested the MEASURE DHS team to access the datasets by filling the online request form on their website (www.dhsprogram.com). Subsequently, the ICF international granted us permission to access the data and the letter of authorization. We kept all data confidential, and no effort was made to identify households or individuals. The authors also confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Result
Socio-demographic characteristics of mothers
This analysis considered 2,052 mothers who had under 24 month’s children in Ethiopia. Almost half of the mothers (51.95%) were in the age group of 25–34 and only 338(16.47%) mothers attended secondary and higher schools. Nearly one-fifth (19.05%) of the respondents were Protestant religion followers and majority of the women (94.98%) were currently in union. Almost two-third of the mothers (64.52%) were from family with number of household members less than or equal to 6 members. Sex of household head for one-fifth of the respondents (20.81%) were females. Less than one-half of the women (48.20%) were from household with low-income level and to the contrary, 754 (37.87%) women were from relatively rich household. One quarter of women included in the study (24.71%), reside in urban areas of the country while two-third of the total women (66.33%) were from agrarian regions (Table 2).
Obstetric characteristics of respondents
In this study, a quarter of the total respondents (25.00%) had no ANC visit. Out of the respondents who made ANC visit, four in ten (41.33%) initiated ANC check up in the first twelve weeks of the current pregnancy. Institutional delivery was 56.73% and out of these, 7.07% women gave birth through caesarean section. Women who received postnatal care service were 12.13% and 15 (6.02%) women went to non-health professional for PNC service. Four in ten women (38.35%) gave their first birth at the age of under 18 and nearly one quarter (23.49%) of the total respondents have at least one living children (Table 3).
Child profile
The sex ratio of the children included in the analysis was approximately one to one, with 49.61% male. One-third of the total children (28.60%) were in the range of 0–5 months during the survey period. Four hundred and sixty-one (22.47%) of the total children included in the analysis were first-born children. The preceding birth interval for the majority of the children (81.42%) was greater than or equal to 24 months (Table 4).
Exclusive breastfeeding practice coverage in Ethiopia
The coverage of exclusive breastfeeding practice in Ethiopia was 56.05% (95% CI: 53.95%, 58.10%) (Fig. 2). Nearly three-fourth women (74.03%) initiated breastfeeding immediately after birth while one in twenty women (5.02%) put their child to breast after a day and above (Fig. 3).
Factors affecting exclusive breastfeeding practice in Ethiopia
Multilevel multivariable analysis showed that mode of delivery, time of breastfeeding initiation, and geographic region were statistically significant variables with exclusive breastfeeding practice among mothers of 0–23 months old children. The odds of exclusive breastfeeding practice among women who gave birth through caesarean section were 64% [AOR = 0.36; 95% CI: 0.21, 0.63] lower than women who gave birth through spontaneous vaginal delivery. Women who initiated breastfeeding their children within the first 1 h of life, after 1–24 h of delivery, or after a day of birth were 45% [AOR = 0.55; 95% CI: 0.34, 0.90], 64% [AOR = 0.36; 95% CI: 0.24, 0.54], and 96% [AOR = 0.04; 95% CI: 0.02, 0.08] respectively less likely to practice exclusive breastfeeding as compared to women who initiated breastfeeding immediately after birth. In addition, women who live in the pastoralist region and women who live in the city administrations were 78% [AOR = 0.22; 95% CI: 0.12, 0.39] and 51% [AOR = 0.49; 95% CI: 0.27, 0.89] respectively less likely to practice exclusive breastfeeding as compared to women who live in the agrarian region of the country (Table 5).
Random effect analysis result
Table 6 depicts the random effect estimates obtained after fitting the four models (Null model, Model I, Model II, and Model III). The ICC of the Null model revealed the presence of EBF practice variance across the country's nine regions and two city administrations (ICC = 33.21%). This suggests that 33% of the variation in EBF practice among mothers of infants under the age of two was due to regional differences. Additionally, the highest PCV (46.01%) in the final model (Model III) indicates that the majority of differences in EBF practice among mothers seen in the null model were explained by both individual and community-level factors. Furthermore, the lowest deviance in the final model indicated that model III was the best fitted model (Table 6).
Spatial autocorrelation
Spatial distribution of exclusive breastfeeding found to be non-random with a global Moran’s I statistic value of (I = 0.13, P-value < 0.001) (Fig. 4). This means given the z-score of 10.19, there is less than 1% likelihood that this clustered pattern could be the result of random chance. Therefore, the null hypothesis was rejected, which was stated that exclusive breastfeeding practice distributed randomly. It shows that there is local clustering in the distribution of exclusive breastfeeding, which should be investigated further using local statistics.
The incremental autocorrelation was determined using the beginning distance (average at 0.220000) meter and increment by 0.217549 m. As shown in Fig. 5, at maximum peak (1.09-m) distance, statistically significant z-scores revealed that spatial factors encouraging clustering are most evident, and incremental spatial autocorrelation shows that ten distance bands were detected.
Hot spot and cold spot
The spatial distribution of exclusive breastfeeding was clustered in some parts of the country. Based on the Getis-Ord Gi* statistical analysis result significant hotspot of exclusive breastfeeding was found in some part of Amhara (Bahir Dar, South Gondar, Awi/Agew, West Gojam, part of North and South Wollo), a few places in SNNP (Sidama, Gedio and Wolayta) and Oromia (Arsi and West Harerge). Whereas, statistically significant cold spots of exclusive breastfeeding were found in Addis Abeba, Dire Dawa, Harari, a few parts of Gambela (Nuer and Agnuak), and Benshangul Gumuz (Assosa) regions of Ethiopia with 90%-99% confidence levels, as shown in the figure below, where the red colors indicate significant hotspots of exclusive breastfeeding and the blue colors indicate significant cold spots (Fig. 6).
Spatial interpolation
The spatial interpolation method allows estimating values for locations where no samples have been taken and to assess the uncertainty of these estimates. Geo-statistical ordinary kriging analysis predicted that the highest prevalence of exclusive breastfeeding (29.8%—37.8%) was detected in Eastern Tigray, Central Amhara, Eastern SNNP and Western part of Oromia. In contrast, area with relatively low prevalence (1.9%—9.9%) was detected in Addis Ababa, most part of Somali and Dire Dawa as shown in the figure below. The dark white color represents highest exclusive breastfeeding practice and dark green color predicted the lowest exclusive breastfeeding and dark yellow color indicates areas with moderate exclusive breastfeeding (Fig. 7).
Spatial SaTScan analysis
Purely spatial analysis was conducted using the Culldorff spatial SaTScan analysis to detect primary spatial clusters of exclusive breastfeeding. This purely spatial statistical analysis method creates a circular window that scans the entire study area. The radius of the circle varies continuously from zero to a specified maximum size. The maximum-size specified the percentage of the maximum total population at risk within the scanning window. As recommended by the researchers, the maximum cluster size was set at 50% of the population at risk. Thus, numerous overlapping windows of different sizes are generated, which together cover the entire study area. Each circular window is considered a possible candidate cluster. For each circle, the observed cases inside and outside the window were counted and compared to the number of expected cases, as calculated using Bernoulli model. On this basis, the likelihood ratio within each circle is then calculated. The circle with the maximum likelihood ratio and containing more cases than expected is identified as the most likely (primary) cluster. A significance level of P < 0.05 was used to test whether the cluster was significant or not.
Most likely (primary clusters) and secondary clusters of exclusive breastfeeding were identified. A total of 10 significant clusters were identified, of which, one of them was most likely (primary) cluster and 9 were secondary clusters. The primary clusters spatial window was found in Somali region which was located at (5.984681 N, 43.361253 E) of geographic location with 239.15 km radius, and Log-Likelihood ratio (LLR) of 111.86, which was detected as the most likely cluster with maximum Likelihood (Table 7). It referred that women within this spatial window had 0.35 times more likely to practice exclusive breastfeeding than the women outside that area of the spatial window (Fig. 8).
Discussion
This analysis was done to identify independent predictors of exclusive breastfeeding practice among mothers of children aged 0–23 months in Ethiopia using the recent EMDHS data. The prevalence of exclusive breastfeeding practice of infants under 24 months in Ethiopia was 56.05%. The current prevalence is lower than 88.0% in South and North Ethiopia [30], 76% in Southwest Ethiopia [14], 68% in Hargeisa, 59% in Tanzania [31], and 71% in Southern Ghana [32]. The disparity in coverage of exclusive breastfeeding practices could be attributable to a variety of factors. The practice of delivering fresh butter, plain water, milk other than breast milk, and sugar or glucose water to newborns right after birth may also lower the rate of exclusive breastfeeding in the country [16, 27]. Similarly, mothers' understanding of exclusive breastfeeding, access to and utilization of maternity and child health care, and the variation of study areas could all be contributing factors to the disparity. According to this study, barely four out of ten women (42.15%) had ANC services four or more times. Similarly, four in ten women gave birth at home while traditional birth attendants attended almost one-third of the total delivery. Surprisingly, nearly half of the total women included in the study had no education. All these factors could be the possible reasons for the discrepancy of the coverage rates [14, 15, 33, 34].
In this study, the probability of exclusive breastfeeding practice among women who gave birth through caesarean section was less likely as compared to those women who gave birth via spontaneous vaginal delivery. This finding is in line with studies conducted in Addis Ababa [35, 36], Bahir Dar [20], Bangladesh [37], and Hunan China [38]. Mothers who underwent caesarean delivery were unable to early initiate breastfeeding their newborn baby until they become stable following a long postoperative care. This might create an opportunity for the untimely introduction of formula or other milk, plain water, or non-milk liquids for the newborn. Furthermore, the observed difference between caesarean section and normal delivery in exclusive breastfeeding practice could be due to inadequate implementation of the ten steps of the baby-friendly hospital initiative, which are known to significantly increase breastfeeding rates [39]. The difficulty with inefficient implementation of the program can be attributed mostly to healthcare workers' knowledge, competence, and skills in supporting breastfeeding [40]. Similarly, it could occur as a result of a heavy workload and a deficiency of appropriate healthcare providers at health facilities [41]. Additionally, the absence or inefficient post-caesarean section breastfeeding counselling by healthcare personnel for mothers may have contributed to the disparity, as evidenced by other study conducted in Ethiopia [42]. According to study conducted in low-income country, health professionals or families should provide physical support and pain control measures to mothers who gave birth via caesarean section in order to promote mother-baby connection and mothers' confidence in breastfeeding their infant [43].
The current study found that women who started breastfeeding their baby early were more likely to practice exclusive breastfeeding than mothers who started breastfeeding their children later. The finding was consistent with studies done in Eastern Ethiopia [17], Cairo [44], and Indonesia [45]. Initiation of breastfeeding within the first hour of birth is considered as an integral part of the safe delivery procedure. It might be also linked with the effort of trained health professionals attending the delivery, who assist and encourage mothers to timely initiate breastfeeding.
Furthermore, the contextual region where the women reside also affected the practice of exclusive breastfeeding. In the present study, women who live in the pastoralist region and women who live in the city administrations were less likely to practice exclusive breastfeeding than women who live in the agrarian region of the country. Findings from studies done in Ethiopia [24, 25], Malawi [21] and Southern Ghana supported the current finding. This could be related with low health coverage of the pastoralist region, poor utilization of maternal health services, lack of awareness about the exclusive breastfeeding practice and cultural beliefs of women living in the pastoralist regions of the country. Women living in the pastoralist region provide holy water (taxalil) and digri (herbal infusion) for their infants by considering as it protects the newborn from evil eyes and enhance proper growth of the baby. Also, they believe that giving fresh cow or goat butter or milk immediately after birth by a known hero of the society for the newborn is used to transfer the character of the influential person to the newborn baby (“turufa /’onn’orr/ ferenga’etu”) [46,47,48]. Hence, these all practices could contribute reduction of the duration of exclusive breastfeeding practice. Contrarily, the possible reason for the low exclusive breastfeeding practice experienced among women who resided in the city administrations might be attributed with the work related factors, having relatively good income level, and interest to maintain their body shape.
The limitations of this study were disproportional nature of sampling, secondary nature of data, and hierarchical nature of the data. Because the outcome variable was measured using the maternal self-report, the study was vulnerable to recall and social desirability bias. In this study, exclusive breastfeeding is measured independently in two ways: 0–5 and 6–23 months, and then combined. However, there may be significant differences between this group of children, which could impact the overall measurements. Furthermore, because the data was secondary, the number of weeks at delivery, birth weight, mother's employment status, and other relevant variables were not included. As a result, while interpreting the study's findings, the limitations indicated earlier must be considered. In contrast, we strictly followed internationally accepted analysis criteria and used multilevel analysis, taking into account the data's clustering character, so the investigators are confident that the stated limitations will not have a significant impact on the validity of the study findings.
Conclusion
The study reported that more than half of the women practiced exclusive breastfeeding in Ethiopia. Birth through caesarean section, late initiation of breastfeeding, and geographic region were statistically significant variables with exclusive breastfeeding practice. To increase the coverage of exclusive breastfeeding among Ethiopian children aged 0 to 23 months, the Ministry of Health Ethiopia, in collaboration with its partners and all relevant agencies, should work to promote timely breastfeeding initiation and improve maternal health service utilization. Furthermore, they need to develop a special intervention strategy for women living in the country's city administrations and pastoralist regions in order to enhance the practice of exclusive breastfeeding.
Availability of data and materials
The survey dataset used in this analysis is the third-party data from the demographic and health survey website (www.dhsprogram.com) and permission to access the data is granted only for registered DHS data user.
Abbreviations
- DHS:
-
Ethiopian Demographic Health Survey
- EMDHS:
-
Ethiopian Mini Demographic Health Survey
- WHO:
-
World Health Organization
- UNICEF:
-
United Nation Children’s Fund
- SNNPR:
-
South Nations Nationalities and Peoples Region
- CI:
-
Confidence Interval
- ANC:
-
Antenatal Care
- PNC:
-
Postnatal Care
- AIC:
-
Akaike Information Criterion
- BIC:
-
Baye’s Information Criterion
- ICC:
-
Intra-class Correlation Coefficient
- PCV:
-
Proportional Change in Variance
- MOR:
-
Median Odds Ratio
References
WHO, UNICEF. Indicators for assessing infant and young child feeding practices. World Heal Organ United Nations Child Fund. 2021;WHA55 A55/:19. http://apps.who.int/iris/bitstream/handle/10665/44306/9789241599290_eng.pdf?sequence=1%0Ahttp://whqlibdoc.who.int/publications/2008/9789241596664_eng.pdf%5Cnhttp://www.unicef.org/programme/breastfeeding/innocenti.htm%5Cnhttp://innocenti15.net/declaration.
OMS UNICEF. The extension of the 2025 maternal, infant and young child nutrition targets to 2030. Discuss Pap. 2019;12. http://www.who.int/nutrition/healthygrowthproj/en/index1.html%0Ahttp://www.who.int/nutrition/healthygrowthproj/en/index1.html%0Ahttp://www.who.int/nutrition/healthygrowthproj/en/index1.html%0Ahttps://www.who.int/nutrition/global-target-2025/discussion-pap.
WHO. Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. WHO, editor. Geneva. 2009. https://apps.who.int/iris/handle/10665/44117.
WHO. Global Strategy for Infant and young child feeding. Fifthy-fourth world health assembly. Geneva: WHO Press; 2003. p. 8.
WHO. Infant and young child feeding. https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding.
Most THE, Intervention E, Reduce TO, Mortality C, Bihar IN. OPTIMAL Breastfeed. 2015;(June). https://www.aliveandthrive.org/sites/default/files/attachments/IndiaPolicyBrief_Breastfeeding_.pdf.
Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr Int J Paediatr. 2015;104:96–113.
Phukan D, Ranjan M, Dwivedi LK. Impact of timing of breastfeeding initiation on neonatal mortality in India. Int Breastfeed J. 2018;13(1):1–10.
Arifeen S, Black R, Antelman G, Baqui A, Caulfield L, Exclusive BS. Effect of breastfeeding on diarrheal mortality. Pediatrics. 2001;108(4):E67.
Wako WG, Wayessa Z, Fikrie A. Effects of maternal education on early initiation and exclusive breastfeeding practices in sub-saharan Africa: a secondary analysis of demographic and health surveys from 2015 to 2019. BMJ Open. 2022;12(3):e054302.
Apanga PA, Weber AM, Darrow LA, Riddle MS, Tung WC, Liu Y, et al. The interrelationship between water access, exclusive breastfeeding and diarrhea in children: a cross-sectional assessment across 19 African countries. J Glob Health. 2021;11:1–9.
Wake GE, Mittiku YM. Prevalence of exclusive breastfeeding practice and its association with maternal employment in Ethiopia: a systematic review and meta-analysis. Int Breastfeed J. 2021;16(1):1–14.
Amugsi D. Breastfeeding trends show most developing countries may miss global nutrition targets. Assoc Res Sci African Popul Heal Res Cent. 2021;3–6. https://theconversation.com/breastfeeding-trends-show-most-developing-countries-may-miss-global-nutrition-targets-166853.
Awoke S, Mulatu B. Determinants of exclusive breastfeeding practice among mothers in Sheka Zone, Southwest Ethiopia: a cross-sectional study. Public Heal Pract. 2021;2(March):100108. https://doi.org/10.1016/j.puhip.2021.100108.
Solomon T, Fufa G, Girma T. Exclusive breastfeeding practice and its associated factors among mothers with infants aged less than six months in Nono, Western Ethiopia : a cross-sectional study. J Women’s Heal Care. 2021;10(538):1–8.
Tewabe T, Mandesh A, Gualu T, Alem G, Mekuria G, Zeleke H. Exclusive breastfeeding practice and associated factors among mothers in Motta town, East Gojjam Zone, Amhara Regional State, Ethiopia, 2015 : a cross-sectional study. Int Breastfeed J. 2017;12(12):1–7.
Mulatu Dibisa T, Sintayehu Y. Exclusive breast feeding and its Associated factors among mothers of < 12 months old child in Harar Town, Eastern Ethiopia: a cross-sectional study. Pediatr Heal Med Ther. 2020;11:145–52.
Gebremedhin T, Geberu DM, Atnafu A. Less than one-fifth of the mothers practised exclusive breastfeeding in the emerging regions of Ethiopia: a multilevel analysis of the 2016 Ethiopian demographic and health survey. BMC Public Health. 2021;21:(1):1–13.
Desalew A, Sema A, Belay Y. Exclusive breastfeeding practice and its Associated factors among mothers with children aged 6–23 months in dire Dawa, Eastern Ethiopia: a community-based cross-sectional study. J Midwifery Reprod Heal. 2020;8(4):2419–28.
Seid AM, Yesuf ME, Koye DN. Prevalence of exclusive breastfeeding practices and associated factors among mothers in Bahir Dar City, Northwest Ethiopia: a community based cross-sectional study. Int Breastfeed J. 2013;8(1):1–8.
Nkoka O, Ntenda PAM, Kanje V, Milanzi EB, Arora A. Determinants of timely initiation of breast milk and exclusive breastfeeding in Malawi: a population-based cross-sectional study. Int Breastfeed J. 2019;14(37):1–9.
Ismail Mohamed A, Tegene Y, Jonah K. Prevalence of exclusive breastfeeding practice and its Associated factors among mothers with children aged 6–12 months in Hargeisa City, Somaliland. Sci J Public Heal. 2020;8(2):43.
Ethiopian Public Health Institute (EPHI) and ICF. 2019. Mini Demographic and Health Survey 2019: key Indicators. Rockville, Maryland, USA: EPHI and ICF; 2019. p. 35.
Tsegaw SA, Dawed YA, Tadesse E, Id A. Exploring the determinants of exclusive breastfeeding among infants under-six months in Ethiopia using multilevel analysis. PLoS One. 2021;16(1):1–17. https://doi.org/10.1371/journal.pone.0245034.
Alemayehu T, Haidar J, Habte D. Determinants of exclusive breastfeeding practices in Ethiopia. Ethiop JHealth Dev. 2009;23(1):12–8.
Jama A, Gebreyesus H, Wubayehu T, Gebregyorgis T, Teweldemedhin M, Berhe T, et al. Exclusive breastfeeding for the first six months of life and its associated factors among children age 6–24 months in Burao district, Somaliland. Int Breastfeed J. 2020;15(1):1–8.
Belachew AB, Kahsay AB, Abebe YG. Individual and community-level factors associated with introduction of prelacteal feeding in Ethiopia. Arch Public Heal. 2016;1–11. https://doi.org/10.1186/s13690-016-0117-0.
Gebru TT, Abady GG, Teklu FG, Tesfamichael YA, Bitow MT, Tekola KB, et al. Assessment of wasting and associated factors among under five children of Wukro town, Tigray regional, north Ethiopia: a cross sectional study. Pan Afr Med J. 2019;33:1–11.
Croft TN, Aileen MJ, Marshall CK, Allen, et al. Guide to DHS statistics. Maryland, USA ICF: Rockville; 2018. pp. 22–51.
Hagos D, Tadesse AW. Prevalence and factors associated with exclusive breastfeeding among rural mothers of infants less than six months of age in Southern nations, nationalities, peoples (SNNP) and Tigray regions, Ethiopia: a cross-sectional study. Int Breastfeed J. 2020;15(1):1–8.
Dede KS, Bras H. Exclusive breastfeeding patterns in Tanzania: do individual, household, or community factors matter? Int Breastfeed J. 2020;15(1).
Manyeh AK, Amu A, Akpakli DE, Williams JE, Gyapong M. Estimating the rate and determinants of exclusive breastfeeding practices among rural mothers in Southern Ghana. Int Breastfeed J. 2020;15(1):1V.
Hunegnaw MT, Gezie LD, Teferra AS. Exclusive breastfeeding and associated factors among mothers in Gozamin district, northwest Ethiopia : a community based cross-sectional study. Int Breastfeed Journa. 2017;12(30):1–8.
Atimati AO, Adam VY, Group F. Breastfeeding practices among mothers of children aged 1–24 months in Egor Local Government Area of Edo State, Nigeria Breastfeeding practices among mothers of children aged 1–24 months in Egor Local Government Area of Edo State, Nigeria. South African J Clin Nutr. 2020;0658:10–6. https://doi.org/10.1080/16070658.2018.1493071.
Shifraw T, Worku A, Berhane Y. Factors associated exclusive breastfeeding practices of urban women in Addis Ababa public health centers, Ethiopia: a cross sectional study. Int Breastfeed J. 2015;10(1):4–9. https://doi.org/10.1186/s13006-015-0047-4.
Elyas L, Mekasha A, Admasie A, Assefa E. Exclusive breastfeeding practice and Associated Factors among mothers attending private Pediatric and Child clinics, Addis Ababa, Ethiopia: a cross-sectional study. Int J Pediatr. 2017;2017:1–9.
Hasan M, Hassan N, Khan SI, Tareq A, Afroj MS. Prevalence, knowledge, attitudes and factors associated with exclusive breastfeeding among mothers in Dhaka, Bangladesh : a cross-sectional study. Popul Med 2021;(Who 2018):1–7.
Chen C, Yan Y, Gao X, Xiang S, He Q, Zeng G, Liu S, Sha TLL. Influences of cesarean delivery on breastfeeding practices and duration: a prospective cohort study. J Hum Lact. 34(3):526–34. https://pubmed.ncbi.nlm.nih.gov/29365288/.
OMS UNICEF. The baby-friendly hospital initiative for small, sick and preterm newborns. In: Report reflects the activities of the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF). 2020. p. 1–56. Available from: https://www.who.int/publications/i/item/9789240005648.
Blixt I, Rosenblad AK, Axelsson O, Funkquist EL. Breastfeeding training improved healthcare professional’s self-efficacy to provide evidence-based breastfeeding support: A pre-post intervention study. Midwifery. 2023;125(April):103794.https://doi.org/10.1016/j.midw.2023.103794
Fadl N, Haile Z. Association between mode of delivery and breastfeeding practices in Egypt: secondary analysis of Egypt demographic and health survey. East Mediterr Heal J. 2021;27(5):474–82.
Setegn T, Gerbaba M, Belachew T. Determinants of timely initiation of breastfeeding among mothers in Goba Woreda, South East Ethiopia: a cross sectional study. BMC Public Health. 2011;11(1):217 http://www.biomedcentral.com/1471-2458/11/217.
Kintu A, Abdulla S, Lubikire A, Nabukenya MT, Igaga E, Bulamba F, et al. Postoperative pain after cesarean section: assessment and management in a tertiary hospital in a low-income country. BMC Health Serv Res. 2019;19(1):1–6.
Tollah Mostafa Farag H, Essam El-Din Mohamed Ammar N, Yahia El-Awady M. Prevalence of breastfeeding and factors affect its practice in women attending primary Health Care Units in Cairo. Al-Azhar Med J. 2020;49(4):2033–40.
Karima UQ, Herbawani CK, Puspita ID, Pristya TYR, Choirunisa S. Determinants of exclusive breastfeeding practice in Indonesia: Analysis of Demographic and Health Surveys Program (DHS) 2017. Adv Heal Sci Res. 2020;30(Ichd):339–46.
Abas AH, Ahmed AT, Farah AE, Wedajo GT. Barriers to optimal maternal and child feeding practices in Pastoralist areas of Somali Region, Eastern Ethiopia: a qualitative study. Food Nutr Sci. 2020;11(06):540–61.
Tsegaye M, Ajema D, Shiferaw S, Yirgu R. Level of exclusive breastfeeding practice in remote and pastoralist community, Aysaita Woreda, Afar, Ethiopia. Int Breastfeed J. 2019;14(1):1–15.
Biza N, Mohammed H. Pastoralism and antenatal care service utilization in Dubti District, Afar, Ethiopia, 2015: a cross-sectional study. Pastoralism. 2016;6(1). https://doi.org/10.1186/s13570-016-0062-0.
Acknowledgements
The authors are grateful to Measure DHS, ICF International Rockville, Maryland, USA for allowing us to use the 2019 EDHS data.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
SS has conceived the study, analysed the data, interpreted the results, and drafted the manuscript while, YA, GG, TD and TA was equally involved in analysing the data and critically revised the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used secondary data from demographic and health survey data files. Initially, the MEASURE DHS team was formally requested to access the datasets by completing the online request form on their website (www.dhsprogram.com). Accordingly, permission to access the data and the letter of authorization was obtained from ICF international. Therefore, for this study consent to participate is not applicable. We kept all data confidential, and no effort was made to identify households or individuals. The Ethiopian Health Nutrition and Research Institute (EHNRI) Review Board and the National Research Ethics Review Committee (NRERC) at the Ministry of Science and Technology of Ethiopia, approved EMDHS 2019. The authors also confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sako, S., Gilano, G., Dileba, T. et al. Spatial distribution and determinants of exclusive breastfeeding practice among mothers of children under 24 months of age in Ethiopia: spatial and multilevel analysis. BMC Pregnancy Childbirth 24, 554 (2024). https://doi.org/10.1186/s12884-024-06755-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06755-x