Abstract
Background
Long non-coding RNAs (lncRNAs) play an important role in angiogenesis, immune response, inflammatory response and tumor development and metastasis. m6 A (N6—methyladenosine) is one of the most common RNA modifications in eukaryotes. The aim of our research was to investigate the potential prognostic value of m6A-related lncRNAs in ovarian cancer (OC).
Methods
The data we need for our research was downloaded from the Cancer Genome Atlas (TCGA) and the Gene Expression Omnibus (GEO) database. Pearson correlation analysis between 21 m6A regulators and lncRNAs was performed to identify m6A-related lncRNAs. Univariate Cox regression analysis was implemented to screen for lncRNAs with prognostic value. A least absolute shrinkage and selection operator (LASSO) Cox regression and multivariate Cox regression analyses was used to further reduct the lncRNAs with prognostic value and construct a m6A-related lncRNAs signature for predicting the prognosis of OC patients.
Results
Two hundred seventy-five m6A-related lncRNAs were obtained using pearson correlation analysis. 29 m6A-related lncRNAs with prognostic value was selected through univariate Cox regression analysis. Then, a seven m6A-related lncRNAs signature was identified by LASSO Cox regression. Each patient obtained a riskscore through multivariate Cox regression analyses and the patients were classified into high-and low-risk group using the median riskscore as a cutoff. Kaplan–Meier curve revealed that the patients in high-risk group have poor outcome. The receiver operating characteristic curve revealed that the predictive potential of the m6A-related lncRNAs signature for OC was powerful. The predictive potential of the m6A-related lncRNAs signature was successfully validated in the GSE9891, GSE26193 datasets and our clinical specimens. Multivariate analyses suggested that the m6A-related lncRNAs signature was an independent prognostic factor for OC patients. Moreover, a nomogram based on the expression level of the seven m6A-related lncRNAs was established to predict survival rate of patients with OC. Finally, a competing endogenous RNA (ceRNA) network associated with the seven m6A-related lncRNAs was constructed to understand the possible mechanisms of the m6A-related lncRNAs involed in the progression of OC.
Conclusions
In conclusion, our research revealed that the m6A-related lncRNAs may affect the prognosis of OC patients and identified a seven m6A-related lncRNAs signature to predict the prognosis of OC patients.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Background
Ovarian cancer (OC) is a common malignant tumor in gynecology. More than 70% of OC patients are diagnosed in advanced stages due to the lack of symptoms and effective screening methods in early stages [1]. Tumor cell reduction plus platinum-based chemotherapy has become the standard model for initial treatment of OC [2]. However, nearly 80% of OC patients still relapse in about three years [3]. Therefore, it is is urgent to identify new prognostic markers and therapeutic targets to promote the prognosis of OC.
At present, more than 100 RNA modification methods have been confirmed, among which m6A methylation is the most widely studied one [4]. The m6A methylation is mainly accomplished by three enzymes, including methyltransferase, demethylase and methylation recognition enzyme [5]. Recent research have shown that m6A methylation is closely related to the occurrence and development of a variety of tumors including OC. Lili Hao et al. reported that the up-regulated ALKBH5 promote the epithelial-to-mesenchymal transition (EMT) and worse outcome of uveal melanoma by inducing m6A methylation of FOXM1 [6]. Haocheng Wang et al. revealed that overexpression level of YTHDF1 was associated with the poor outcome of cervical cancer. The knockdown of YTHDF1 will inhibit the proliferation, invasion and metastasis of cervical cancer cells [7]. Le Tao et al. indicated that FTO is involved in tumorigenesis and prognosis of bladder cancer by regulating the MALAT/miR-384/MAL2 axis [8]. FTO inhibits the self-renewing of OC stem cells and the occurrence of OC by enhancing the second messenger 3', 5'-cyclic adenosine monophosphate (cAMP) signaling [9].
Long non-coding RNAs (lncRNAs) are a class of nucleotide transcripts over 200 nt in length. Studies have shown that lncRNA can regulate physiological processes such as cell differentiation, immune response and apoptosis. LncRNAs plays an important role in the occurrence and development of a variety of metabolic diseases and cancers [10]. Yanrong Lv et al. found that LncRNA TDRG1 promotes the proliferation, invasion and metastasis of breast cancer cells through miR-214-5p/CLIC4 axis [11]. The up-regulated expression level of TOPORS-AS1 inhibited the proliferation and aggressive behaviors of OC cells by disrupting the Wnt/β-catenin signaling and associated with the favorable outcome of OC patients [12]. In addition, it has been reported that several lncrnas regulate the occurrence and development of cancer through m6A modification. For example, overexpressed LINC00857 regulates the expression of E2F3 by binding to Mir-150-5p, ultimately promoting the tumogenesis and poor outcome of pancreatic cancer [13]. LNC942 promotes breast cancer cell proliferation and progression by modulating METTL14-mediated M 6A methylation [14]. LncRNA LINRIS was upregulated in colorectal cancer tissues and associated with the poor overall survival and aerobic glycolysis of colorectal cancer patients by stabilizing IGF2BP2 [15]. LncRNA GAS5-AS1 has been identified as a promoter of ALKBH5-dependent m6A demethylation in cervical cancer, thereby inhibiting the proliferation, migration and invasion of cervical cancer cells [16]. However, the potential mechanisms of m6A modifications involved in the lncRNA-dependent OC occurrence and development remains unclear. Thus, it is significant to investigate the potential mechanisms of m6A modifications of lncRNAs participated in OC.
In the current research, we identified and verified a seven m6A-related prognostic lncRNAs signature for predicting the prognosis of OC based on the data obtained from the Cancer Genome Atlas (TCGA) and the Gene Expression Omnibus (GEO) database. Each patient obtained a riskscore and the patients were classified into high-and low-risk group using the median value. The patients in low-risk group were associated with favorable prognosis. The receiver operating characteristic (ROC) curve revealed that the predictive potential of the m6A-related lncRNAs signature for OC was powerful. The predictive potential of the m6A-related lncRNAs signature was successfully validated in the GSE9891, GSE26193 datasets and 60 clinical specimens. A nomogram was constructed based on the expression level of the seven m6A-related lncRNAs to predict the survival rate of OC patients. Finally, a ceRNA network related to the seven m6A-related lncRNAs was established.
Materials and methods
Data acquisition
The training cohort, TCGA-OV dataset containing 379 patients were downloaded from the Genomic Data Commons Data Portal (https://portal.gdc.cancer.gov/). The validation cohort, GSE9891 [20] and GSE26193 [21] dataset including 285 and 107 patients respectively were acquired from Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/). Perl software was used for data integration and extraction of lncRNAs expression data and corresponding clinical data.
Specimen collection
A total of 60 OC samples were collected at ShengJing Hospital of China Medical University (Shenyang, China) from January to December 2015. Clinical information of the OC samples is presented in Supplementary Table 1. The inclusion criterion of the samples was as follows: (1) High-grade serous OC diagnosed by postoperative pathology; (2) All patients underwent surgical treatment, and the lesion tissue was retained during the operation; (3) Complete prognostic information was available (4) Informed and consented participants in this study. The exclusion criteria of the samples was as follows: (1) Patients with cognitive dysfunction and autoimmune system diseases; (2) The patient had received hormonal or chemoradiotherapy prior to tissue collection; (3) Complicated with mental abnormalities, tumors in other parts or severe liver and kidney function abnormalities. This study was approved by the ethics committee of the ShengJing Hospital of China Medical University, and informed consent was obtained from all patients. In addition, all methods were executed in accordance with relevant guidelines and regulations.
Identification of the m6A-related lncRNAs
The 21 m6A regulators including 8 writers (METTL3, ZC3H13, METTL14, RBM15B, CBLL1, WTAP, RBM15, and KIAA1429), 2 erasers (FTO and ALKBH5), and 11 readers (YTHDC1, YTHDC2, ELAVL1, YTHDF1, LRPPRC, YTHDF2, FMR1, YTHDF3, HNRNPC, HNRNPA2B1, and IGF2BP1) were extracted from the TCGA-OV dataset [22]. Pearson correlation analysis was performed to calculate the correlation coefficient between 21 m6A regulators and lncRNAs. LncRNAs meet the screening criteria p < 0.001 and |R|> 0.4 were considered as m6A-related lncRNAs [23]. A lncRNAs- m6A regulators network was constructed and visualized by cytoscope software. Finally, function enrichment analysis was used to explore the functions of the m6A regulators in the network involed in OC through GenCLiP310 online website (http://ci.smu.edu.cn/genclip3/analysis.php) [24].
Construction of the m6A-related lncRNAs prognostic signature
The m6A-related lncRNAs were fitted into univariate Cox regression analysis to obtain the m6A-related lncRNAs with prognostic value according to p < 0.05. A least absolute shrinkage and selection operator (LASSO) Cox regression and forward stepwise method was conducted to further narrow the prognostic related lncRNAs. Multivariate Cox regression analysis was implemented to calculate the regression coefficients of the selected m6A-related lncRNAs. Each patient acquired a riskscore according to the formula:
Risk score = ∑Coefi * xi (Coefi represents the regression coefficient, xi represents the expression level of m6A-related lncRNAs).
Real-time qPCR
Total RNA of OC samples was extracted using TriZol Reagent (Takara, Japan). cDNA synthesis was carried out using the AMV reverse transcriptase reagent box (Takara, Japan). Real-time PCR was performed using a 2 × SYBR Green PCR Master Mix. Next, the 2-ΔΔCt method was used to calculate the relative gene expression with GAPDH serving as an internal reference. The sequences of primers used for RT-qPCR are presented in Supplementary Table 2.
Evaluation and validation of the m6A-related lncRNAs prognostic signature
Patients were divided into high- and low- risk groups based on the median riskscore. Kaplan–Meier (K-M) method was used to compare the differences in prognosis between groups. The receiver-operating characteristics (ROC) curve was performed to evaluate the effectiveness of the m6A-related lncRNAs prognostic signature and the area under the curve (AUC) was calculated. We then validated the results in GSE9891 and GSE26193 dataset. Finally, multivariate Cox regression analysis was used to investigate whether the riskscore was independent of the clinicopathological parameters as an independent prognostic factor in OC patients.
Construction of the nomogram model
To predict the survival rate of the OC patients, a nomogram model was conducted based on the expression level of the m6A-related lncRNAs prognostic signature using the “rms”package in R software. Calibration curves at 1-,3-,5- year were drawn to assess the consistency between actual and predicted survival rates [25].
Construction of the ceRNA network related to the m6A-related lncRNAs prognostic signature
CeRNA network plays an important role in the occurrence and progression of ovarian cancer. We constructed a ceRNA network related to the m6A-related lncRNAs prognostic signature and the corresponding m6A regulators. Firstly, we obtained the miRNAs interacted with the m6A-related lncRNAs prognostic signature from the miRDB online website (http://mirdb.org/custom.html) [26]. We then acquired the possible miRNAs interacted with the m6A regulators from miRWalk online website (http://mirwalk.umm.uni-heidelberg.de/) [27]. After intersecting the predicted miRNAs, a lncRNAs—miRNAs—mRNAs ceRNA network was conducted and visualized by cytoscope software.
Results
Construction of the seven m6A-related lncRNAs prognostic signature
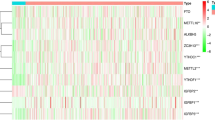
We obtained 275 m6A-related lncRNAs based on the pearson correlation analysis between the 21 m6A regulators and lncRNAs (Table1). 275 lncRNAs- 12 m6A regulators network was constructed and visualized by cytoscope software (Fig. 1). The 12 m6A regulators in the network was fitted into the GenCLiP310 online website to explore the function involed in OC. The results indicated that the 12 m6A regulators involved in OC progression through post-transcriptional modification of RNA (Fig. 2). 29 m6A-related lncRNAs with prognostic value for OC patients selected from the 275 m6A-related lncRNAs using univariate Cox regression analysis (Table 2, p < 0.05). The expression level of 29 m6A-related lncRNAs and corresponding overall survival, survival status of patients were substituted into Lasso regression analysis to select and shrink the variables.Ten m6A-related lncRNAs prognostic signature (AC004816.1, AC013270.1, AL138820.1, AC008669.1, AC010336.1, AC097376.3, AC130710.1, ACAP2-IT1, AL138820.1 and CACNA1G-AS1) was selected according to the optimal λ value of tenfold cross-validation (Fig. 3A and B). Forward stepwise method was conducted to further narrow the prognostic related lncRNAs. A seven m6A-related lncRNAs prognostic signature (AC008669.1, AC010336.1, AC097376.3, AC130710.1, ACAP2-IT1, AL138820.1 and CACNA1G-AS1) was obtained. Multivariate Cox regression analysis was implemented to calculate the regression coefficients of the seven m6A-related lncRNAs prognostic signature (Table 3). Each patient acquired a riskscore according to the formula: riskscore = 9.84E-06* exp AC008669.1 -7.82E-05 * exp AC010336.1 -1.56E-05* exp AC097376.3 -4.26E-05* exp AC130710.1 + 3.19E-05* exp ACAP2-IT1 + 0.00011047* exp AL138820.1 + 5.74E-05 * exp CACNA1G-AS1.
Identification of a seven m6A-related lncRNAs prognostic signature. A LASSO coefficient profiles of the 29 m6A-related lncRNAs. B The penalization coefficient λ in the LASSO model was tuned using tenfold cross-validation and the minimum criterion. AUC metrics (y-axis) were plotted against log(λ) (bottom x-axis). The top x-axis indicates the number of predictors for the given log (λ). For the optimal λ, ten m6A-related lncRNAs with non-zero coefficient were selected. C K-M survival curve showed survival analysis of the seven m6A-related lncRNAs prognostic signature in TCGA-OV dataset. D ROC curve analysis of the seven m6A-related lncRNAs prognostic signature in TCGA-OV dataset
Evaluation and validation of the seven m6A-related lncRNAs prognostic signature
Patients were divided into high- and low- risk groups based on the median riskscore. K-M curve indicated that the patients in high-risk group have poor prognosis cpmpared with the patients in low- risk group (Fig. 3C, p = 4.493e-08). The ability of the seven m6A-related lncRNAs prognostic signature to predict patient outcome was evaluated by a ROC curve, and the AUC value was 0.735 (Fig. 3D). To verify the the seven m6A-related lncRNAs prognostic signature established in TCGA database, the riskscore of patients in GSE9891, GSE26193 dataset as well as 60 clinical specimens was calculated based on the seven m6A-related lncRNAs. The patients were divided into high- and low- risk group according to the median riskscore. Similar to the results obtained in the TCGA database, patients in the high-risk group had a shorter overall survival compared to patients in the low-risk group (Fig. 4A, C and E). The ROC curve was drawn in GSE9891, GSE26193 dataset as well as 60 clinical specimens, the AUC value was 0.873, 0.784 and 0.818, respectively (Fig. 4B, D and F).
Evaluation of the seven m6A-related lncRNAs prognostic signature in GSE9891 and GSE26193 dataset. A K-M survival curve showed survival analysis of the m6A-related lncRNAs prognostic signature in GSE9891 dataset. B ROC curve analysis of the m6A-related lncRNAs prognostic signature in GSE9891 dataset. C K-M survival curve showed survival analysis of m6A-related lncRNAs prognostic signature in GSE26193 dataset. D ROC curve analysis of the m6A-related lncRNAs prognostic signature in GSE26193 dataset. E The K-M survival curve showed survival analysis of m6A-related lncRNAs prognostic signature in in our clinical specimens. F ROC curve analysis of of the m6A-related lncRNAs prognostic signature in our clinical specimens
Independent prognostic value of the seven m6A-related lncRNAs prognostic signature
Univariate and multivariate Cox regression analyses were performed in the TCGA-OV dataset to determine whether riskscore was an independent prognostic factor for OC patients. Univariate Cox regression analyses indicated that the riskscore was significant associated with the prognosis of OC patients (HR = 1.167, 95%CI = 1.111 ~ 1.226, P < 0. 001, Fig. 5A). Multivariate Cox regression analyses revealed that riskscore remains a significant prognostic factor after controlling for other confounders (HR = 1.571, 95%CI = 1.080 ~ 2.288, P = 0. 018, Fig. 5B), demonstrating that riskscore could be used as an independent prognostic factor of OC patients. The ROC curve showed that the prognostic ability of the riskscore was higher than the other clinical factors (Fig. 5C).
Construction of the nomogram model based on the seven m6A-related lncRNAs prognostic signature
A nomogram model was conducted based on the expression level of m6A-related lncRNAs prognostic signature to predict the survival rates of OC patients at 1, 3, 5 years (Fig. 6A). The calibration curve at 1, 3, 5 years revealed that the actual and predicted survival rates was highly consistent, suggesting that the predictive performance of the nomogram model was power ((Fig. 6B, C and D).
Construction of the ceRNA network related to the seven m6A-related lncRNAs prognostic signature
A ceRNA network was constructed based on the seven m6A-related lncRNAs prognostic signature and the corresponding eighteen m6A regulators (Table 4). We obtained the microRNA (miRNA) interacted with the seven m6A-related lncRNAs from miRDB online website. Then, the miRNA interacted with the eighteen m6A regulators was obtained from miRWalk online website. After intersecting the predicted miRNAs, a ceRNA network including seven m6A-related lncRNAs, eighteen m6A regulators and two hundred miRNAs was obtained and visualized by cytoscope software (Fig. 7).
Discussion
TCGA-OV dataset including 379 OC patients was used as training dataset to identify the prognostic significance of m6A-related lncRNAs in OC. 29 m6A-related lncRNAs with prognostic value were selected and seven of them were used to conduct a m6A-related lncRNAs prognostic signature for predicting the prognosis of OC patients. The patients in TCGA-OV dataset were divided into high- and low- risk groups based on the median riskscore, and the patients in high- risk group have poor outcome. Multivariate Cox regression analyses revealed that the riskscore was an independent prognostic factor for OC patients. We then conducted a nomogram based on the expression level of the seven m6A-related lncRNAs prognostic signature to predict the survival rate of the OC patients. Finally, a ceRNA network including seven m6A-related lncRNAs, eighteen m6A regulators and two hundred miRNAs was acquired to investigate the potential mechanisms of the m6A-related lncRNAs involed in OC. Reviewing previous studies, we found an article consistent with the purpose of our analysis [17]. Jianfeng Zheng etc. randomly divided the TCGA-OV dataset into training or validation dataset at a ratio of 3:7. In our study, TCGA-OV dataset was used as the training dataset, while GSE9891 GSE26193 dataset as well as 60 clinical specimens were used as the validation dataset. Jianfeng Zheng etc. selected 129 m6A-related lncRNAs based on the screening criteria p < 0.01 and |R|> 0.4, while our study aquired 275 m6A-related lncRNAs according to the screening criteria p < 0.001 and |R|> 0.4. Jianfeng Zheng etc. conduct a four m6A-related lncRNAs prognostic signature (AC010894.3, ACAP2-IT1, CACNA1G-AS1 and UBA6-AS1) for predicting the prognosis of OC patients based on the training dataset, while we built a m6A-related lncRNAs prognostic signature containg seven lncRNAs. ACAP2-IT1 and CACNA1G-AS1 was included in the m6A-related lncRNAs prognostic signature of two analyses. Jianfeng Zheng etc. found that the prognostic signature was confirmed to show completely opposite prognostic value in training dataset and validation dataset, while our prognostic signature was successfully confirmed in the validation dataset. Jianfeng Zheng etc. Superior to our analysis is that they further analyzed the differences of immune cell infiltration and chemotherapy drugs between high-and low- risk groups as well as the effect of CACNA1G-AS1 on ovarian cancer cell proliferation. The reason for some differences in the results between the two studies maybe that the sample size of the training dataset and screening criteria for m6A-related lncRNAs were different.
Numerous studies have shown that m6A regulators might play an important role in the malignant progression of cancers. Positively controlled by METTL3, LINC00958 promotes the tumorigenesis for breast cancer by regulating the miR-378a-3p/YY1 axis [18]. Jie Shen et al. reported that YTHDF2 promotes the proliferation of endometrioid endometrial carcinoma by increasing the degradation of lncRNA FENDRR [19]. Xiangrui Meng et al. have shown that m6A mediated overexpression of LINC00857 promotes the progression and tumorigenesis of pancreatic cancer through the regulation of miR—150–5 p/E2F3 axis [13]. LncRNA MALAT1 acts a oncogenic role in thyroid cancer by regulating the miR-204/IGF2BP2/m6A-MYC axis [20]. We can see that m6A regulators and lncRNAs can promote the progression of cancer through interaction from the above literature review. However, the potential mechanisms of m6A regulators involved in the lncRNAs-dependent OC pathogenesis remains unclear. In our study, we explored the potential interaction between the m6A regulators and lncRNAs through the construction of the ceRNA network, but more experimental studies are still needed to verify our conjecture in the future.
A seven m6A-related lncRNAs prognostic signature (AC008669.1, AC010336.1, AC097376.3, AC130710.1, ACAP2-IT1, AL138820.1 and CACNA1G-AS1) was conducted for predicting the prognosis of OC. Among them, AC008669.1, ACAP2-IT1, AL138820.1 and CACNA1G-AS1 was associated with poor prognosis of OC, while AC010336.1, AC097376.3 and AC130710.1 was protective factor for the prognosis of OC. CaCNA1G-AS1 has been reported to be associated with the malignant progression of liver cancer, rectal cancer, and non-small cell lung cancer [21,22,23]. In addition, other six m6A-related lncRNAs have not been reported yet. This demonstrates the novelty of our study and encourages us to continue to validate our findings in vitro and in vivo.
This study had some limitations. Firstly, we could not determine whether the seven selected m6A-related lncRNAs prognostic markers would be suitable for measuring in blood samples due to the sample tissues came from decidual tissue rather than blood. Secondly, ceRNA network of our research are only predictions and need to be verified by basic science and clinical studies. Finally, the number of OC samples in TCGA and GEO databased were limited, we need verify our research results using more other datasets.
Conclusions
In conclusion, our research identified a seven m6A-related lncRNAs prognostic signature as a independent prognostic factors to predict the prognosis of OC. The seven m6A-related lncRNAs prognostic signature might act as prognostic markers and new therapeutic targets of OC.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the TCGA (https://portal.gdc.cancer.gov/) and GEO (https://www.ncbi.nlm.nih.gov/) repository.
Abbreviations
- lncRNAs:
-
Long non-coding RNAs
- OC:
-
Ovarian cancer
- TCGA:
-
The Cancer Genome Atlas
- GEO:
-
Gene Expression Omnibus
- LASSO:
-
Least absolute shrinkage and selection operator
- EMT:
-
Epithelial-to-mesenchymal transition
- cAMP:
-
Cyclic adenosine monophosphate
- K-M:
-
Kaplan–Meier
- ROC:
-
Receiver-operating characteristics
- AUC:
-
Area under the curve
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
Wang D, Zhang G, Peng C, Shi Y, Shi X. Choosing the right timing for interval debulking surgery and perioperative chemotherapy may improve the prognosis of advanced epithelial ovarian cancer: a retrospective study. J Ovarian Res. 2021;14(1):49.
Yang J, Ma J, Jin Y, Cheng S, Huang S, Zhang N, Wang Y. Development and validation for prognostic nomogram of epithelial ovarian cancer recurrence based on circulating tumor cells and epithelial-mesenchymal transition. Sci Rep. 2021;11(1):6540.
Ping XL, Sun BF, Wang L, Xiao W, Yang X, Wang WJ, Adhikari S, Shi Y, Lv Y, Chen YS, et al. Mammalian WTAP is a regulatory subunit of the RNA N6-methyladenosine methyltransferase. Cell Res. 2014;24(2):177–89.
Yang Y, Hsu PJ, Chen YS, Yang YG. Dynamic transcriptomic m(6)A decoration: writers, erasers, readers and functions in RNA metabolism. Cell Res. 2018;28(6):616–24.
Hao L, Yin J, Yang H, Li C, Zhu L, Liu L, Zhong J. ALKBH5-mediated m(6)A demethylation of FOXM1 mRNA promotes progression of uveal melanoma. Aging (Albany NY). 2021;13(3):4045–62.
Wang H, Luo Q, Kang J, Wei Q, Yang Y, Yang D, Liu X, Liu T, Yi P. YTHDF1 Aggravates the Progression of Cervical Cancer Through m(6)A-Mediated Up-Regulation of RANBP2. Front Oncol. 2021;11: 650383.
Tao L, Mu X, Chen H, Jin D, Zhang R, Zhao Y, Fan J, Cao M, Zhou Z. FTO modifies the m6A level of MALAT and promotes bladder cancer progression. Clin Transl Med. 2021;11(2): e310.
Huang H, Wang Y, Kandpal M, Zhao G, Cardenas H, Ji Y, Chaparala A, Tanner EJ, Chen J, Davuluri RV, et al. FTO-Dependent N (6)-Methyladenosine Modifications Inhibit Ovarian Cancer Stem Cell Self-Renewal by Blocking cAMP Signaling. Cancer Res. 2020;80(16):3200–14.
Mercer TR, Dinger ME, Mattick JS. Long non-coding RNAs: insights into functions. Nat Rev Genet. 2009;10(3):155–9.
Lv Y, Dong K, Gao H. Long non-coding RNA TDRG1 facilitates cell proliferation, migration and invasion in breast cancer via targeting miR-214-5p/CLIC4 axis. Cancer Biol Ther. 2021;22(3):248–56.
Fu Y, Katsaros D, Biglia N, Wang Z, Pagano I, Tius M, Tiirikainen M, Rosser C, Yang H, Yu H. Vitamin D receptor upregulates lncRNA TOPORS-AS1 which inhibits the Wnt/β-catenin pathway and associates with favorable prognosis of ovarian cancer. Sci Rep. 2021;11(1):7484.
Meng X, Deng Y, He S, Niu L, Zhu H. m(6)A-Mediated Upregulation of LINC00857 Promotes Pancreatic Cancer Tumorigenesis by Regulating the miR-150-5p/E2F3 Axis. Front Oncol. 2021;11: 629947.
Sun T, Wu Z, Wang X, Wang Y, Hu X, Qin W, Lu S, Xu D, Wu Y, Chen Q, et al. LNC942 promoting METTL14-mediated m(6)A methylation in breast cancer cell proliferation and progression. Oncogene. 2020;39(31):5358–72.
Wang Y, Lu JH, Wu QN, Jin Y, Wang DS, Chen YX, Liu J, Luo XJ, Meng Q, Pu HY, et al. LncRNA LINRIS stabilizes IGF2BP2 and promotes the aerobic glycolysis in colorectal cancer. Mol Cancer. 2019;18(1):174.
Wang X, Zhang J, Wang Y. Long noncoding RNA GAS5-AS1 suppresses growth and metastasis of cervical cancer by increasing GAS5 stability. Am J Transl Res. 2019;11(8):4909–21.
Zheng J, Guo J, Cao B, Zhou Y, Tong J. Identification and validation of lncRNAs involved in m6A regulation for patients with ovarian cancer. Cancer Cell Int. 2021;21(1):363.
Rong D, Dong Q, Qu H, Deng X, Gao F, Li Q, Sun P. m(6)A-induced LINC00958 promotes breast cancer tumorigenesis via the miR-378a-3p/YY1 axis. Cell Death Discov. 2021;7(1):27.
Shen J, Feng XP, Hu RB, Wang H, Wang YL, Qian JH, Zhou YX. N-methyladenosine reader YTHDF2-mediated long noncoding RNA FENDRR degradation promotes cell proliferation in endometrioid endometrial carcinoma. Lab Invest. 2021;101(6):775–84.
Ye M, Dong S, Hou H, Zhang T, Shen M. Oncogenic Role of Long Noncoding RNAMALAT1 in Thyroid Cancer Progression through Regulation of the miR-204/IGF2BP2/m6A-MYC Signaling. Mol Ther Nucleic Acids. 2021;23:1–12.
Wei LJ, Bai DM, Wang ZY, Liu BC. Upregulated lncRNA CACNA1G-AS1 aggravates the progression of colorectal cancer by downregulating p53. Eur Rev Med Pharmacol Sci. 2020;24(1):130–6.
Yang J, Li C, Li H. E C: LncRNA CACNA1G-AS1 facilitates hepatocellular carcinoma progression through the miR-2392/C1orf61 pathway. J Cell Physiol. 2019;234(10):18415–22.
Yu PF, Kang AR, Jing LJ, Wang YM. Long non-coding RNA CACNA1G-AS1 promotes cell migration, invasion and epithelial-mesenchymal transition by HNRNPA2B1 in non-small cell lung cancer. Eur Rev Med Pharmacol Sci. 2018;22(4):993–1002.
Ye G, Guo L, Xing Y, Sun W, Yuan M. Identification of prognostic biomarkers of prostate cancer with long non-coding RNA-mediated competitive endogenous RNA network. Exp Ther Med. 2019;17(4):3035–40.
Fu Y, Bao Q, Liu Z, He G, Wen J, Liu Q, Xu Y, Jin Z, Zhang W. Development and Validation of a Hypoxia-Associated Prognostic Signature Related to Osteosarcoma Metastasis and Immune Infiltration. Front Cell Dev Biol. 2021;9:633607.
Wong N, Wang X. miRDB: an online resource for microRNA target prediction and functional annotations. Nucleic Acids Res. 2015;43(Database issue):D146–52.
Xiu D, Liu L, Cheng M, Sun X, Ma X. Knockdown of lncRNA TUG1 Enhances Radiosensitivity of Prostate Cancer via the TUG1/miR-139-5p/SMC1A Axis. Onco Targets Ther. 2020;13:2319–31.
Acknowledgements
We thank the authors who provided the TCGAand GEOpublic datasets.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Hui Qu, Yang Song conceived and designed the study. Hui Qu, Yang Song developed the methodology. Hui Qu, Yang Song analyzed and interpreted the data. wrote, reviewed, and/or revised the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the ShengJing Hospital of China Medical University, and informed consent was obtained from all patients. In addition, all methods were executed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, Y., Qu, H. Identification and validation of a seven m6A-related lncRNAs signature predicting prognosis of ovarian cancer. BMC Cancer 22, 633 (2022). https://doi.org/10.1186/s12885-022-09591-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09591-4