Abstract
Background:
The incidence of breast cancer (BC) in Thailand has been rising at an alarming rate. The annual incidence of BC in Thailand has doubled over a span of 15 years. A retrospective study was conducted with the primary objective of assessing and comparing survival rates of patients with BC, stratified by subtype of BC.
Methods:
A retrospective study was implemented for a cohort of women receiving a diagnosis of invasive BC with the objective of assessing and comparing their overall survival, stratified by BC subtype. Thai women receiving a diagnosis of their first primary invasive BC between January 2006 and December 2015 at Chiang Mai University Hospital were studied with 3,150 cases meeting the eligible criteria.
Results:
The median follow-up time was 4.9 years (Inter Quartile Range: 2.8–7.7). The most common diagnosed subtype was luminal B-like (n = 1,147, 36.4%). It was still the most prevalent subtype (35.8%) in women younger than 40 years and the 40–60 age-group, The proportion of patients with TNBC is the highest in women aged less than 40 years with 19.3% compared to the other age categories. Finally, among women older than 60 years, the proportion of each subtype was relatively uniform. Most women received a diagnosis of stage II disease. Triple negative subtype increased overall mortality in advanced staging (stages III and IV) (aHR:1.42, 95% CI: 0.96–2.11). The 5-year overall survival rate was found in luminal A-like at 82.8%, luminal B-like at 77.6%, HER-2 enriched at 66.4% and triple negative subtype at 64.2%.
Conclusion:
The histologic subtype, correlated with age and staging influenced the OS. Our results confirmed the association of triple negative BC with poor prognosis especially in advanced stage. The adjuvant medical treatment in our country could not be accessible in some group of patients, so the results of treatment and survival especially HER-2 enriched are lower than other countries without treatment barrier.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinical Practice Points
Currently, breast cancer systemic treatments using endocrine treatment, chemotherapy or targeted therapy depend on the patient’s clinical status and tumor characteristics but in some countries these patients did not achieve treatment goals due to public health service policy. Thus, real-world results especially overall survival may differ from standard publication results.
Introduction
Breast cancer (BC) is the most common female cancer and the leading cause of cancer mortality among Thai women and women worldwide. The incidence of BC in Thailand has been rising at an alarming rate. The annual incidence of BC in Thailand has doubled over a span of 15 years, from the age-standardized incidence rate (ASIR) of 17.8 per 100,000 in 1998 to 26.6 per 100,000 in 2012 [1]. The ASIR was 31.4 per 100,000 among Thai women based on data collected from 2013 to 2015 [2]. In northern Thailand, related published data showed that the ASIR of BC in a northern Thai population increased from an ASIR of 20.8 per 100,000 women-years from 1998 to 2002 to ASIR of 27.7 per 100,000 women-years from 2008 to 2012 while age-standardized mortality rates were stable around 5.0 per 100,000 women-years from 1998 to 2012 [3].
Women newly diagnosed with BC used clinical factors to determined prognosis, i.e., size and nodal status, but these did not serve as efficient predictors for the overall survival of Patients with BC because of the effectiveness of surgical and clinical interventions. Application of immunohistochemistry (IHC) in clinical settings permits subtyping BC, which can be used as another prognostic indicator [4]. Extensive studies have been conducted to estimate the overall survival of women by their BC subtype in Western countries [5,6,7,8,9]. Findings from these studies might be unapplicable to women from South East Asian (SEA) regions due to differences in healthcare infrastructure, personal and life-style habits or differences in genetic compositions of populations. We implemented a retrospective study of a cohort of women diagnosed with invasive BC, with the objective of assessing and comparing their overall survival, stratified by BC subtype.
Materials and methods
Setting
The Chiang Mai University (CMU) hospital system is a tertiary, 1,400-bed, teaching hospital serving six regions in northern Thailand. Annually, healthcare providers in the CMU hospital system provide health services to about 1,300,000 patients in outpatient and 48,000 i-inpatient departments. Since 2003, the hospital system has adopted a multidisciplinary BC treatment and management approach. The main objective has been to deliver the best healthcare services to patients with BC by providing consistent, continuous, coordinated and cost-effective care.
Description of the cohort
Members of the cohort included Thai women receiving a diagnosis of their first primary invasive BC between January 2006 and December 2015, inclusively. The initial year of entry in the cohort was restricted to January 1, 2006 due to changes in healthcare referral policies and practices at the CMU and its network hospitals. In 2006, we implemented the institutional policy of including the HER2 biomarker as a component of the diagnostic workup of women receiving a diagnosis of any stage of invasive BC. We restricted study eligibility to women with complete pathologic diagnostic information about the status of the Estrogen Receptor (ER), Progesterone Receptor (PR) and HER2 biomarker.
The study was approved by The Medical Ethics Committee of the Faculty of Medicine, Chiang Mai University (316/2016).
Data collection
Information on pathologic parameters (TNM staging, grade, ER, PR and HER2 status), date of surgery, considered as the date of initial diagnosis and age at the initial clinical presentation of the disease were retrieved from institutional tumor registry and validated against medical records. Additionally, information was retrieved regarding the type of surgery (lumpectomy vs. mastectomy) and adjuvant therapy by reviewing medical records. Patients’ vital status and dates of death were retrieved from databases at the Ministry of Interior, National Registration Department Vital Status.
Definition of subtype of breast cancer
We reviewed the pathological diagnostic data and categorized BC subtypes by expression status of ER, PR and HER2.The members of the cohort were grouped by their HR and HER2 status in Luminal A-like (ER+,PR + and HER2 negative), Luminal B-like (ER+,PR- and any HER2), HER2(ER-,PR- and HER2 positive) and triple negative(ER-,PR- and HER2 negative) groups.In this study, ER and PR + defined by positive more than 1% by IHC and HER2 positive defined by IHC 2 + and confirmed with fluorescence in situ hybridization (FISH) or IHC 3+.We used “luminal-like” because our hospital did not provide ki-67 pathologic assessment Table 1).
Statistical analysis
We applied descriptive statistics to summarize clinic-demographic and pathologic prognostic indictors of the members of our cohort. The variable age at initial clinical presentation of BC was categorized in (1) younger than 40 years of age; (2) 40 to 60 and (3) older than 60 years of age. The BC stages were classified as I, II, III or IV according to the American Joint Committee on Cancer (AJCC) 7th edition and overall grade as 1, 2 or 3. Chemotherapy and endocrine treatments were dichotomized as “Yes” or “No”. Women were classified by their BC subtype and differences in the distributions of clinicopathologic variables were assessed using parametric or nonparametric statistics as appropriate.
We applied Kaplan-Meier survival to assess the probability of 5-year survival by subtype of BC. For our study, we defined survival as the duration between the date of initial diagnosis and the date of death, documented in the medical records. All analyses were performed using STATA Software, Version 16 (Stata Corp, College Station, TX, USA) and hypothesis testing was two-sided with a 5% significance level.
Results
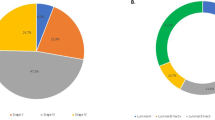
Of the 3,961 members of the cohort, 3,153 met the study eligibility criteria (Fig. 1). The median follow-up time was 4.9 years (Inter Quartile Range, IQR: 2.8–7.7). The distribution of clinicopathologic characteristics of members of the cohort at the initial clinical presentation of the disease is presented in Table 2. Overall, the most commonly diagnosed subtype was luminal B-like (n = 1,147, 36.4%) followed by luminal A-like (n = 910, 28.8%), HER2 enriched (n = 633, 20.0%) and Triple Negative (n = 463, 14.8%). However, after stratification of women by their age at the diagnosis of BC, the luminal B-like subtype was still the most prevalent in all age categories, 37.8% (131/346) among women younger than 40 years of age, 35.8% (765/2139) among the age group of 40 to 60 years and 17.81% (119/668) among women aged more than 60. The proportion of patients with TNBC is the highest in women aged less than 40 years with 19.3% (67/346) compared to the other age categories with 13.98% (299/2139) in women aged 40–60 and 14.52% (97/668) in women aged more than 60. Finally, among women older than 60 years, the proportion of women diagnosed with each subtype of BC was relatively uniform. (Table 2) Most women were diagnosed with TNM stage II, regardless of their BC subtypes; for women, diagnosed with either luminal A-like subtypes of BC, TNM stage I ranked the second highest prevalence, TNM stage I was the third most commonly diagnosed tumor stage. Information on the stage of BC was missing in the medical records of 352 women although histopathologic diagnostic data on subtype status were available and these women had completed their treatment at CMU Hospital.
Most of the patients were received chemotherapy (76.3%) and Adriamycin-based was the preferred regimen. Hormonal therapy was given to Hormone Receptor-Positive (ER + and/or PR+) patients in almost all cases (Table 3).
The triple-negative subtype increased overall mortality in advanced staging (stage III and IV) and (aHR:1.42, 95% CI: 0.96–2.11,p-value = 0.083) by multivariable cox regression analysis however tumor subtype did not affect the mortality in early-stage BC (stage I-II) (Table 4). The best 5-year OS rate was found in luminal A-like (82.8%), followed by luminal B-like (77.6%). HER-2 enriched and triple-negative subtype had an inferior survival rate. The lowest 5-year OS rate was found in the triple-negative subtype (64.2%) as shown in Fig. 2.
Discussion
Our study demonstrated the influences of subtype at diagnosis on the survival of Northern Thai BC patients. Most of our patients were luminal B-like. The second most common type was luminal A-like which also had the highest survival. Patients with triple-negative and HER-2 enriched had an increased adjust hazard risk of death compared to luminal-like subtypes. This result is consistent with other studies [5,6,7]. However, the triple negative subtype patients in this cohort did not increase the risk of death compared to luminal-like and HER2 enriched subtype that may be from most of the patients was found in the early-stage group. Chemotherapy was also given for HR+, HER2-subtypes patients in our study because of the other prognostic factors ex. histologic grade, presence of lymphovascular invasion, and nodal status were included for considering adjuvant treatment. Some hormonal receptor positive (HR+) Patients with BC in our study did not receive hormonal therapy and a few triple negative Patients with BC received hormonal therapy could not identified the reason from medical record. Those cases similar to ATLAS trial that enrolled women with HR- or unknow in study [10].
Most Thai patients were covered under the medical welfare scheme which can access public health services from public hospitals and private hospitals registered with The National Health Security Office (NHSO). This scheme of government universal coverage offers the three cornerstones of BC treatment: surgery, chemotherapy, and radiotherapy. However, NHSO restricts access to certain critical medical treatments such as novel chemotherapy or anti-hormonal therapy, and limited anti-HER2 treatment only in the adjuvant setting in nodal positive disease. National Comprehensive Cancer Network (NCCN) and some studies recommended adjuvant taxane-containing chemotherapy in patients who had axillary lymph node-positive, trastuzumab in HER2 positive [8,9,10,11] but the taxane-containing regimen has been approved for adjuvant treatment in node-positive BC and metastatic BC (MBC) since 2007, adjuvant trastuzumab was just approved in 2015 and eligible for BC patients who had node positive only in universal health coverage (UHC),Social security scheme(SSS) and Civil Servant Medical Benefit Scheme. and inflammatory BC and supraclavicular lymph node metastasis was not allowed to use adjuvant trastuzumab and Patients with MBC also could not access trastuzumab.
In this study cohort, HER-2 enriched group survival was 66.4% and shorter than the related published OS between 75 and 85% [5, 7, 11] because our patient was enrolled before the approval of adjuvant trastuzumab treatment which may have been the reason for an inferior outcome but similar results were found with other studies from Thailand [12, 13]. In our study, the result of luminal A-like 5-year OS was 83.4% in all stages which was less than in other studies [14,15,16]. Nonsteroidal aromatase inhibitor was approved to use in 2009. NSHO did not allow steroidal aromatase inhibitors, fulvestrant and CDK4/6 inhibitors for HR + and anti-HER2 for patients with metastatic BC. The further evaluation of treatment efficacy should compare between two periods of treatment “before and after” accessing adjuvant treatment.
Conclusion
Histological subtype correlated with age and staging affected to OS. Our results confirmed the association of triple-negative BC with poor prognosis especially in high grade tumors and advanced stage. The adjuvant medical treatment in our country could not be accessed by some groups of patients, so the results of treatment and survival especially HER-2 enriched appear inferior to those of other countries without treatment barrier.
Data availability
The datasets used or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- BC:
-
Breast cancer
- ASIR:
-
Age-standardized incidence rate
- HR:
-
Hormonal receptor
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- OS:
-
Overall survival
References
Cancer Incidence in Five Continents, CI5plus: IARC CancerBase No. 9 [Internet]. 2018. Available from: https://ci5.iarc.fr/Default.aspx.
Imsamran W, Pattatang A, Supattagorn P, Chiawiriyabunya I, Namthaisong K, Wongsena M, eaCiTVI. 2013–2015. Bangkok, 2018. Cancer in Thailand Bangkok2018.
Pongnikorn D, Daoprasert. K, Wongkaew B. Sangkam. S, Praditkay. M, R. M. Trends in Cancer Incidence and Mortality in Northern Thailand, 1993–2017. Lampang Cancer Hospital. 2020.
Wishart GC, Azzato EM, Greenberg DC, Rashbass J, Kearins O, Lawrence G, et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 2010;12(1):R1.
Haque R, Ahmed SA, Inzhakova G, Shi J, Avila C, Polikoff J, et al. Impact of breast cancer subtypes and treatment on survival: an analysis spanning two decades. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1848–55.
Hennigs A, Riedel F, Gondos A, Sinn P, Schirmacher P, Marmé F, et al. Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer. 2016;16(1):734.
Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in Breast Cancer Survival by Molecular Subtypes in the United States. Cancer Epidemiol Biomarkers Prev. 2018;27(6):619–26.
Mamounas EP, Bryant J, Lembersky B, Fehrenbacher L, Sedlacek SM, Fisher B, et al. Paclitaxel after doxorubicin plus cyclophosphamide as adjuvant chemotherapy for node-positive breast cancer: results from NSABP B-28. J Clin Oncol. 2005;23(16):3686–96.
Untch M, Gelber RD, Jackisch C, Procter M, Baselga J, Bell R, et al. Estimating the magnitude of trastuzumab effects within patient subgroups in the HERA trial. Ann Oncol. 2008;19(6):1090–6.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
Henderson IC, Berry DA, Demetri GD, Cirrincione CT, Goldstein LJ, Martino S, et al. Improved outcomes from adding sequential Paclitaxel but not from escalating Doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol. 2003;21(6):976–83.
Kongsiang A, Tangvoraphonkchai V, Jirapornkul C, Promthet S, Kamsa-Ard S, Suwanrungruang K. Survival time and molecular subtypes of breast cancer after radiotherapy in Thailand. Asian Pac J Cancer Prev. 2014;15(23):10505–8.
Virani S, Wetzel EC, Laohawiriyakamol S, Boonyaphiphat P, Geater A, Kleer CG, et al. Ethnic disparity in breast cancer survival in southern Thai women. Cancer Epidemiol. 2018;54:82–9.
Colleoni M, Sun Z, Price KN, Karlsson P, Forbes JF, Thurlimann B, et al. Annual Hazard Rates of Recurrence for Breast Cancer During 24 Years of Follow-Up: Results from the International Breast Cancer Study Group Trials I to V. J Clin Oncol. 2016;34(9):927–35.
Colzani E, Liljegren A, Johansson AL, Adolfsson J, Hellborg H, Hall PF, et al. Prognosis of patients with breast cancer: causes of death and effects of time since diagnosis, age, and tumor characteristics. J Clin Oncol. 2011;29(30):4014–21.
Zuo T, Zeng H, Li H, Liu S, Yang L, Xia C, et al. The influence of stage at diagnosis and molecular subtype on breast cancer patient survival: a hospital-based multi-center study. Chin J Cancer. 2017;36(1):84.
Acknowledgements
This research work was partially supported by the Faculty of Medicine, Chiang Mai University and Chiang Mai University.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
CD, PS, BC, PK, ET, SC, PM and IC performed experiments or analyzed the data. PK and PM contributed to literature search, data acquisition. CD and IC wrote the manuscript. All authors reviewed and edited the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University, Thailand (316/2016). All methods were performed according to the relevant guidelines and regulations. The data collection component of this project was waived the need of informed consent because data were collected from already existing databases and no study participants were contacted accepted by the Research Ethics Committee of Faculty of Medicine, Chiang Mai University.
Consent for publication
Consent for publication is not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ditsatham, C., Sripan, P., Chaiwun, B. et al. Breast Cancer Subtypes in Northern Thailand and Barriers to satisfactory survival outcomes. BMC Cancer 22, 1147 (2022). https://doi.org/10.1186/s12885-022-10196-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10196-0