Abstract
Background
Lung cancer is the most commonly diagnosed cancer and the leading cause of cancer-related death in men in Algeria. Little is known about the characteristics of lung cancer in Algeria. This study aimed to determine the clinicopathological characteristics and prognosis of non–small cell lung cancer (NSCLC) patients in Algeria.
Methods
This retrospective study was performed on 269 pathologically confirmed cases of NSCLC at the Benbadis University Hospital of Constantine (2015–2023). Of these, 95 patients were included in the survival analysis. The clinicopathological and outcome data were investigated based on the patients’ medical records.
Results
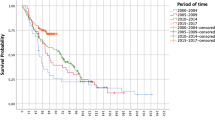
This study showed male predominance with sex ratio of 5.7, with a mean age of 61.8 years. Histologically, 67.3% of cases had adenocarcinoma (ADC) and 22.7% squamous cell carcinoma (SCC). ADC and SCC occurred more frequently in female (p = 0.02) and male (p = 0.003) patients, respectively. Smoking was estimated at 82.2% in men. Over 28% were non-smokers, of which 50.7% were women, and presented at younger age (p = 0.04). Most of our patients (75.5%) have an advanced stage at diagnosis. Around 70% of patients underwent chemotherapy (CT) as first-line treatment, with medians diagnostic and treatment delays of 4 and 1 months, respectively. The median overall survival (mOS) was estimated at 10.3 and 6.7 months in I-III and IV stages, respectively. Other factors that negatively impact OS were age > 65 years (p = 0.01), and the presence of symptoms (p = 0.005) and comorbidity (p = 0.004) in stage IV, and delayed treatment (p = 0.03) and receiving CT alone (p = 0.03) in stages I-III cases. Medians progression free survival (mPFS) in stage IV, III, and II patients were 4.1, 5.2, and 8.3 months, respectively, and negatively affected by the comorbidity (stage IV, p = 0.03) and receiving CT alone (stages II-III, p = 0.03).
Conclusions
NSCLC presents at an early age and advanced stage in Algerian patients. ADC is the most frequent histological subtype and smoking remains the most important risk factor in men. Furthermore, the prognostic factors affecting survival are stage, age, comorbidity, symptoms, and treatment. Thus, tobacco control, early detection program, and access to novel therapies may be the best strategies to reduce NSCLC morbidity and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Lung cancer is the second most commonly diagnosed cancer and the leading cause of cancer-related death in 2020, representing 11.4% cancers diagnosed and 18% deaths of total cases. In men, lung cancer is the leading cause of cancer morbidity (14.3%) and mortality (21.5%), whereas, in women, it ranks third for incidence (8.4%) and second for mortality (13.7%) [1]. Lung cancer remains the most commonly diagnosed cancer among men in North-West Africa or the Maghreb region, including Algeria, Morocco, Tunisia, and Libya, posing a real public health problem. In Algeria, the overall lung cancer incidence rates in 2018 and 2020 have been estimated to be 1.3 and 1.4 cases per 100,000 people, respectively. It is the most common cancer among men, which accounts for about 15.2% of total cases of male cancers, and the third in both sexes. Lung cancer is the leading cause of cancer-associated death, for all ages, responsible for more than 4,300 deaths representing 13.2% of cases [2].
Lung cancer is likely to continue as a major health problem well through the first half of this century with the increasing global trends in its incidence and mortality [3]. The overall survival rate for lung cancer patients is still poor and depends mainly on the stage of disease. Patients diagnosed with localized disease, NSCLC type, have the best 5-year survival rate [4]. However, the survival of advanced NSCLC has relatively improved in recent years by therapeutic advances [5]. Tobacco smoking is the major risk factor in the development of lung cancer. Other risk factors thought to contribute to lung cancer risk, implicating occupational exposures, air pollution, pulmonary conditions, dietary factors, and genetic susceptibility [6]. Disparities in lung cancer incidence, mortality, and survival have been reported by gender and geographical differences. Besides, the observed epidemiological variations are influenced by histological and molecular characteristics [3]. Over the past years, changes have been remarked on in some epidemiological factors such as gender, smoking, and histology [7].
There is limited published data associated with lung cancer reported from Algeria. This study aimed to investigate the clinicopathological and prognosis aspects of patients with NSCLC in the Eastern region of Algeria, based on a referral hospital record, which might reflect a national landscape and could lead to better recognition of this type of cancer in the North African population.
Methods
Patients
We retrospectively reviewed the clinical and pathological data of 269 patients with primary NSCLC diagnosed and/or treated at the Benbadis University Hospital of Constantine (UHC) for 8 years, between February 2015 and March 2023. Of these, 95 patients who underwent CT and/or radiotherapy (RT) were included in the survival analysis. Most patients admitted to the Benbadis UHC came mainly from the eastern regions of Algeria.
Diagnostic and staging were determined on the basis of imaging and anatomopathological testing. Patients underwent chest X-ray and computed axial tomography (CAT), abdominal (CAT or ultrasound), and brain (CAT or magnetic resonance imaging) imaging. Positron emission tomography-CAT was also performed for a proportion of patients. The tissue biopsy was obtained via either bronchoscopy, CAT-guided biopsy, or surgical lung biopsy, and thoracentesis for pleural fluid. Samples were subjected to histopathological (H&E staining) and immunohistochemical (Cytokeatins, TFF1, p40/63 markers) examination. The histopathological classification was confirmed on the basis of the WHO classification of lung tumors (2015). Furthermore, patients were staged according to the 8th edition of the American Joint Committee on Cancer (AJCC) TNM system.
Data collection
The data of NSCLC patients were obtained from the patients’ medical records, at the departments of Anatomical Pathology, Thoracic Surgery, Pneumology, and Medical Oncology. The data collected comprised demographic characteristics and clinicopathological features of patients, including gender, age, smoking status, histological type, stages of the disease, treatment approach, and follow-up times.
Diagnostic delay was measured from first symptom onset to formal diagnosis, and treatment delay from diagnosis to the date of the first consultation in the center. The OS and PFS were defined as the interval from the date of diagnosis and the date of the first treatment to the date of the last follow-up or untill December 31, 2022.
Statistical analysis
The data were constructed and sorted with Excel (Microsoft Office, 2019). Quantitative and qualitative variables were represented with means/medians and percentages, respectively. The differences between groups were assessed using Chi-squared or Fisher test for categorical variables and Mann–Whitney test for continuous variables. Two-sided p values of < 0.05 were considered statistically significant. GraphPad Prism version 7.05 (GraphPad Software, San Diego, CA) was used for statistical analysis.
Results
Clinicopathological characteristics of patients
The main clinicopathological characteristics of the patients included in this study are presented in Table 1. A total of 269 cases of NSCLC primary lung cancer were included, of which 229 (85.1%) were men and 40 (14.9%) women, with a sex ratio male-to-female (M/F) of 5.7. The mean age of patients at the time of presentation was 61.8 years. The age group range from 50 to 69 years represented 63,9% of cases, while about 12% with an age fewer than 50 years.
In terms of smoking history, 178 (66.2%) were smokers, including ex-smokers, and 77 (28.6%) were non-smokers. Taking into account that only one (2.5%) woman patient was a smoker and unavailable data for 14 (5.2%) patients, the rate of smoking was estimated at 82.2% in male patients. Non-smokers tend to present at a younger age compared to smokers (mean: 59.6 vs. 62.8 years ; 44.4% ≤50 vs. 28.1% >50 years, p = 0.04). Also, 50.7% of non-smoker patients were women. On the other hand, of 106 patients with data of occupational exposure, the history of profession-related to increased risk of NSCLC was observed in 24 (22.67%) male patients, the most frequent were the professional driver (8.5%).
The data for symptoms and comorbidity were available for 238 (88.5%) cases. The frequent symptoms at diagnosis were cough (31.9%), thoracic pain (23.1%), dyspnea (21.4%), hemoptysis (8.4%), and non-respiratory symptoms (16%). Regarding comorbidity, 19 (11.4%) patients had a comorbid pulmonary disease, including mainly chronic obstructive pulmonary disease (COPD) and tuberculosis, while 75 (31.5%) cases had chronic diseases, the most common were hypertension (18.1%) and diabetes (13.4%).
The study subjects had the following histological distribution: 181 (67.3%) ADC, 61 (22.7%) SCC, and 27 (10%) other types [Large cell carcinoma (LCC), Adenosquamous carcinoma (ADC-SCC), not otherwise specified (NOS), carcinoid]. A significant association was found between the histological type and gender, in which a high rate of ADC was found in women in comparison to men (82.5% vs. 64.6%, p = 0.02) and SCC in men in comparison to women (25.8% vs. 5%, p = 0.003). Also, there was an association between the histological type and smoking statute, but not statistically significant, ADC was more frequent in non-smokers (76.6% vs. 65.7%, p = 0.08) and SCC in smokers (24% vs. 14.3%, p = 0.08) (Tables 2 and 3). Furthermore, 106 (39.4%) cases had moderately or poorly differentiated tumor while 53 (19.7%) had well differentiated.
Regarding the clinical stage of the disease and treatment approach, 149 (55.4%) cases were at the metastatic disease (stage IV) and 102 (38%) were in non-metastatic stages (stages I-III). Over 75% of patients presented with advanced stages (stage III/IV). The major distant metastatic sites were bone (23%) and brain (12.6%), followed by liver (7.1%) and adrenal gland (3%). These results reflected the received treatment, around 70% of cases undergoing chemotherapy as a first-line treatment, while 16.5% and 13.6% of patients were treated with radiotherapy and surgery, respectively. On the other hand, among patients with metastatic stage, 17 (11.4%) cases benefited from epidermal growth factor receptor (EGFR) mutation testing, of which 6 (35.3%) had positive EGFR mutation. Furthermore, of the 165 patients with data regarding symptoms, the medians of the diagnostic and treatment delay were 4 months (IQR 2–6 months) and 31 days (IQR 14–71 days), respectively.
Prognostic factors
As reported in Tables 4 and 5, various clinicopathological variables were evaluated on a group of treated patients to determine potential prognostic factors for survival. The mOS was estimated at 10.3 months and 6.7 months in non-metastatic and metastatic disease, respectively (p = 0.03). The univariate analysis revealed that a shorter mOS was significantly associated with advanced stage [T4 stage, N2-3 stage, clinical stage IV, two or more sites of metastasis (p < 0.05)], age at diagnosis ≥ 65 years (p = 0.01), and the presence of symptoms (p = 0.005) and comorbidity (p = 0.004) in stage IV, and the treatment delay > 2 months (p = 0.018) and receiving CT alone (p = 0.025) in stage I-III cases. According to this analysis, OS was not influenced by other variables including gender, smoking status, histological type, tumor grade, and diagnostic delay. Furthermore, the mPFS was estimated at 4.1 months in metastatic stage and significantly associated with the presence of comorbidity (p = 0.03), while it was at 5.5 months in non-metastatic stages (Table 6), of which 5.2 months in stage III (p = 0.32) and 8.3 months in stage II (p = 0.07). A shorter mPFS was also significantly associated with receiving CT alone in non-metastatic stages (p = 0.04). Moreover, 50% (6/12) of stage II and merely 25% (5/20) of stage III cases were treated with CT and/or RT.
Discussion
To the best of our knowledge, this is the first study to investigate the clinicopathological and prognosis features of NSCLC in Algeria. The present study is a retrospective investigation of NSCLC in a public referral hospital in Constantine, an Eastern Province of Algeria. The analysis of the collected data allowed us to evaluate some clinicopathological characteristics and prognostic factors of this type of cancer in Algeria.
In our cohort, NSCLC showed a male predominance with a sex ratio (M/F) of 5.7. Comparable results were reported from studies in Algeria [8,9,10,11], Tunisia, and Morocco [12,13,14,15,16,17], with a sex ratio (M/F) varying between 6 and 13.2. In the same line, according to global estimates based on Globocan 2020, the sex ratio (M/F) varies widely across regions, ranging from 1.2 in Northern America to 5.6 in Northern Africa [1]. The low incidence of NSCLC in women in the region of North Africa largely reflects differences in tobacco consumption which represents about 2-5.6% among women versus 27–55% among men [18]. Besides, women have less access to professions with high occupational exposure to pulmonary carcinogens [11].
We found that NSCLC mainly affects patients older than 50 years at the moment of diagnosis, with a mean age of 61.8 years, which is similar to that reported in other Algerian studies [8,9,10,11]. These findings are also close to those found in studies carried out in Maghreb countries [12,13,14,15, 17, 19]. NSCLC is often considered a disease in elderly patients with a median age at diagnosis of 70 years old [20]. The young age observed in NSCLC patients in Northern Africa may be explained by the fact that our population is younger compared to other populations, in particular in Europe and North America [21].
Our findings indicate that the male smoking rate was over 82%. This rate is close to the previous Algerian study conducted by Kefti et al [11]., while other studies in the Maghreb region have reported higher rates varying between 90% and 94%. Concerning female smoking, one patient (2.5%) in our study was a smoker; similar findings were obtained in studies conducted in our region with rates of 0–4% [8, 10, 13,14,15]. Although tobacco smoking remains the most important risk factor in men, about 10–25% of lung cancer patients report no history of regular smoking [22]. In our study, we found a high prevalence (28.6%) of non-smokers, and this non-smoking-related NSCLC was associated with younger age, women and ADC subtype. As reported in literature, neversmokers with NSCLC present distinct clinicopathological characteristics and different patterns of molecular alterations. Never-smoker patients are more likely to be female and have ADC [23]. Shan et al. found that non-smoker with lung ADC showed a younger age [24]. This should increase our interest to understanding the biological and clinical features of this subset of patients.
Other risk factors such as occupational exposure, air pollution, respiratory diseases, and genetic susceptibility, may be related to an increased risk of lung cancer [6]. In terms of respiratory comorbidities, they represent 11.4% among our patients, the most common were COPD and tuberculosis, whereas hypertension and diabetes were the most common chronic diseases. These comorbidities may be an important prognostic factor in treatment choice [25]. Additionally, according to the study by Kefti et al., approximately 50% of Algerian patients with lung cancer had occupational exposure to a carcinogen in their workplace, such as diesel exhaust gases, silica, PAHs, welding fumes, and asbestos [11]. Taking into account that data in our study was not readily available for all patients, the history of occupational exposure was observed in 22.6%, mostly related to professional drivers. As demonstrated in a meta-analysis by Tsoi et al., there is an 18% excess risk of lung cancer linked to professional drivers, potentially exposed to diesel exhaust [26]. Thus, it is needed to research potential non-tobacco-related risk factors in NSCLC.
Regarding lung cancer incidence by histological subtypes, our findings indicate that ADC was the most common subtype, followed by SCC. Recent studies from the region of Maghreb have reported similar proportions of ADC compared with SCC [10, 11, 13,14,15]. Although comparable to previous studies in our region, the SCC subtype predominantly occurred [8, 12]. Indeed, the rates of ADC increased over time and surpassed SCC as the most frequent lung cancer subtype. Moreover, there are disparities in the distribution of histological subtypes according to gender and smoking status. Contrary to the SCC, which is more associated with tobacco smoking, ADC is seen with a higher incidence among women and neversmokers [27]. Although ADC is most commonly found in women and non-smokers in our study, men smokers also showed a high proportion of ADC. It has been suggested that cigarette filter ventilation has contributed to the rise in ADC among smokers [28].
Lung cancer patients are more likely to have advanced disease upon diagnosis. In the same line, most patients in our serie presented with advanced disease. Furthermore, the extra-thoracic metastatic sites are frequently seen in the order of bone, brain, and liver. Our findings are close to those reported in the literature, but hepatic metastases were less frequent [29]. The delayed diagnosis of lung cancer is relatively attributed to the lack of validated screening tools and non-specific symptoms [3]. However, evidence from several cohort studies indicated that low-dose CAT screening allows for the early detection of lung cancer in high-risk patients [1]. On the other hand, promoting awareness of lung cancer symptoms may lead to improved clinical outcomes. In our study, the dominant symptoms that prompted consultation were mainly cough and chest pain, followed by dyspnea and hemoptysis, which are consistent with reported in previous large-scale studies [30, 31]. In terms of delays in the diagnosis and treatment of our patient, contrary to a reasonable time of treatment delay, the diagnostic delay seems excessive in comparison to the recommendation by professional organizations (2–4 weeks) [32]. Our findings are comparable with those in Western Algeria and Morocco, with median times of 83 days and 75 days, respectively [33, 34]. Thus, our patients experience substantial delays from the onset of symptoms to treatment initiation. Future efforts should focus on developing efficient strategies for early detection, based on improving lung cancer diagnosis intervals accompanied by implementing a screening program.
The survival rate of NSCLC depends mainly on the stage of disease. Patients with advanced NSCLC usually have a poor prognosis [4]. In our study, the mOS was estimated at 10.3 and 6.7 months in non-metastatic and metastatic stages, respectively. These findings are generally consistent with data of NSCLC patients received CT and CRT [35]. We found that the advanced stage was associated with a poor prognosis, especially having T4, N2-3, or metastatic stage, particularly with two or more distant metastases. Furthermore, older age (≥ 65 years) and the presence of symptoms and comorbidity were associated with a poor prognosis in patients with metastatic disease. This is in line with the results of a regional study in Tunisian patients with advanced NSCLC, which reported a mOS of 6 months, and the stage, performance status, comorbid conditions, delay of management, and treatment were identified as prognostic factors [36]. The age and comorbidity have been reported yet as independent prognostic factors in lung cancer [37]. Besides, asymptomatic lung cancer patients at diagnosis exhibit a better prognosis. This underlines the importance of an early diagnosis [38]. On the other hand, our data showed that delayed treatment and receiving CT alone were associated with a poor prognosis in patients with non-metastatic disease. These results were consistent with previous findings showing that patients with stages I-III NSCLC who received delayed treatment had a higher risk of mortality [39, 40].
Furthermore, we found that mPFS in patients with stage IV, III, and II were 4.1, 5.2, and 8.3 months, respectively. The PFS was also negatively affected by the presence of comorbidity and receiving CT alone. These findings are under the expected range according to mOS, though a shorter mPFS in patients with stage III. Besides the stage of disease, the presence and severity of comorbid conditions along with age and performance status appear to be important determinants of PFS in NSCLC. The age and presence of comorbidity could have a significant impact on treatment decisions [41]. In patients with early-stage NSCLC, in addition to the impact of comorbidities on the qualification for surgical treatment, they contribute to increased postoperative complications [42, 43]. Multiple comorbidities also have a negative impact on elderly NSCLC patients with III and IV stages treated with CT or CRT [44, 45]. Additionally, PFS may vary depending on the specific treatment regimens and patient characteristics involved in each study. A multicenter retrospective study by Jazieh et al., from 19 low-to-middle-income countries, reported that surgery plus CT and concurrent CRT (cCRT) as initial therapy predicted better mPFS in patients with stage III NSCLC compared to other different treatment regimens [46]. In the same line, Sakin et al. showed that performance status and CRT are the most important factors affecting PFS in elderly patients with inoperable stage III NSCLC, and the best survival was achieved in patients treated with cCRT [47]. Moreover, Flörsch et al. found that patients with inoperable stage III NSCLC treated (post cCRT) according to a multimodal treatment depending on the treatment time and pattern, demonstrated improved survival regardless of immunotherapy use. However, the implementation of immunotherapy has further enhanced patient outcomes [48]. This highlights the importance of timely initiation of specific therapy, along with treatment of comorbidity, to improve the outcome of NSCLC patients. Thus, we suggest further optimization strategies in the management of our NSCLC patients, taking into consideration these different factors.
As expected, our outcome is lower than the medians survival achieved with the use of novel therapies. Though the recent progress in targeted therapy and immunotherapy have changed the landscape for the treatment of advanced NSCLC, access to certain therapeutic modalities among the countries in the region is still limited [18]. Besides, EGFR and PDL1 have been proved as predictive biomarkers in advanced NSCLC for tyrosine kinase and PD1/PDL1 inhibitors, respectively [49, 50]. In conjunction with the predominance of ADC histological type in the current study, high rates of EGFR mutation and PDL1 overexpression (approximativly 40%) were observed in our patients with NSCLC, in particular in those with ADC [51, 52]. This suggests that a large number of Algerian patients with NSCLC are likely candidates for EGFR-targeted therapy and PD1/PDL1 immunotherapy. However, the rate of EGFR testing was admittedly low in this cohort of patients, even among patients with metastatic ADC. This may be explained by the socioeconomic status of our patients since there is limited access to diagnostic settings for molecular testing in public hospitals and anticancer centers. On the other hand, immunotherapy is much more likely to be accessed since PDL1 expression could be routinely assessed by immunohistochemistry. Thus, the establishment of precision medicine treatments at our anticancer centers is likely to improve survival outcomes.
Our study presents some limitations as being a single-center evaluation and based on retrospectively reviewed medical records. There was a proportion of cases without information for some parameters. Besides, the lack of molecular testing of some important markers (EGFR, ALK, ROS1) and PDL1 have not routinely introduced with the immunohistochemical report until most recently. Despite the limitations, our results could be an update on the clinicopathological and prognosis features of NSCLC in our population and help to conduct future research studies, particularly prospective investigations of the influence of novel therapies (targeted and immuno-therapies) and clinical parameters on NSCLC patients' survival.
Conclusion
In this Algerian cohort of patients with NSCLC, the majority of cases were male and diagnosed with advanced disease. The age at diagnosis was relatively younger and ADC was the predominant histological subtype. Tobacco smoking was the most important risk factor in men. On the contrary, neversmokers patients were more likely to be young and female. Furthermore, the prognostic factors affecting survival are stage, age at diagnosis, comorbidity, symptoms, and treatment. Therefore, we suggest that primary prevention, based mainly on tobacco control and early detection through screening program, and access to targeted therapy and immunotherapy may be the best strategies to reduce lung cancer morbidity and mortality. Future efforts should focus on identifying biological differences and potential etiological risk factors to improve NSCLC management in our population.
Data availability
All analyzed data are included in this published article. Data available upon reasonable request to the corresponding author.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries CA. Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660
World Health Organization International, Agency for Research on Cancer. GLOBOCAN 2020: estimated cancer incidence, mortality, and prevalence worldwide in 2020. http://globocan.iarc.fr/Pages/fact_sheets_cancer
Cheng T, Cramb TY, Baade SM, Youlden PD, Nwogu DR, Reid C ME. The international epidemiology of lung cancer: latest trends, disparities, and tumor characteristics. J Thorac Oncol. 2016;11(10):1653–71. https://doi.org/10.1016/j.jtho.2016.05.021
Barta JA, Powell CA, Wisnivesky JP. Global epidemiology of lung cancer. Ann Glob Health. 2019;22;85(1):8. https://doi.org/10.5334/aogh.2419
Howlader N, Forjaz G, Mooradian MJ, Meza R, Kong CY, Cronin KA, et al. The effect of advances in lung-cancer treatment on population mortality. N Engl J Med. 2020;13(7):640–9. https://doi.org/10.1056/NEJMoa1916623
Malhotra J, Malvezzi M, Negri E, La Vecchia C, Boffetta P. Risk factors for lung cancer worldwide. Eur Respir J. 2016;48(3):889–902. https://doi.org/10.1183/13993003.00359-2016
Schabath MB, Cote ML. Cancer progress and priorities: lung cancer. Cancer Epidemiol Biomarkers Prev. 2019;28(10):1563–79. https://doi.org/10.1158/1055-9965.EPI-19-0221
Harir N, Zeggai S, Maalem A. Epidemiological and pathological profile of lung cancer in West Algeria: about 772 cases. J Afr Cancer. 2015;7:22–6. https://doi.org/10.1007/s12558-014-0336-7
Hamdi Cherif M, Kara L, Atoui S, Boudefar F. Données épidémiologiques du cancer dans l’Est et le sud-est Algérien, 2014–2017. Algerian J Health Sci. 2020;2(S2):S14–31.
Bounedjar A, Benkali R, Badoui L, Abada M, Moumeni A, Marouani A, et al. Incidence of lung cancer in males and females in Algeria: the lung cancer registry in Algeria (LuCaReAl). Cancer Epidemiol. 2020;12:69:101799. https://doi.org/10.1016/j.canep.2020.101799
Ketfi A, Zanoun N, Laouedj I, Gharnaout M, Fraga S. Cancer bronchique Primitif et risques professionnels dans une population Nord-Africaine [Primary lung cancer and occupational exposure in a north African population]. Pan Afr Med J. 2020;5:37:120. https://doi.org/10.11604/pamj.2020.37.120.21755. French.
Missaoui N, Hmissa S, Landolsi H, Korbi S, Joma W, Anjorin A, et al. Lung cancer in central Tunisia: epidemiology and clinicopathological features. Asian Pac J Cancer Prev. 2011;12(9):2305–9. PMID: 22296375.
Ben Amar J, Ben Safta B, Zaibi H, Dhahri B, Baccar MA, Azzabi S. Facteurs pronostiques Du cancer Bronchique non à petites cellules localement avancé et métastatique. Tunis Med. 2016;94:5. https://doi.org/10.1016/j.pneumo.2017.05.002
Harizi C, Bellali H, Hchaichi A, Hamzaoui A, Chahed K. Estimation Du coût de la prise en charge Du cancer broncho-pulmonaire en tunisie. East Mediterr Health J. 2018;24(10):988–93. https://doi.org/10.26719/2018.24.10.988
Belmokhtar KY, Tajir M, Boulouiz R, Bennani A, Brahmi SA, Alloubi I, et al. Cancer Du Poumon Au Maroc Oriental: où en sommes-nous? [Lung cancer in Eastern Morocco: where do we stand?]. Pan Afr Med J. 2019;34:177. https://doi.org/10.11604/pamj.2019.34.177.19934
Lachgar A, Tazi MA, Afif M, Er-Raki A, Kebdani T, Benjaafar N. Lung cancer: incidence and survival in Rabat, Morocco. Rev Epidemiol Sante Publique. 2016;64(6):391–5. https://doi.org/10.1016/j.respe.2016.02.012
Oukabli M, Rharrassi I, Damiri A, et al. Cancers bronchopulmonaires: étude Clinique et anatomopathologique. À propos de 163 cas. J Afr Cancer. 2011;3:29–35. https://doi.org/10.1007/s12558-010-0130-4
Jazieh AR, Algwaiz G, Errihani H, Elghissassi I, Mula-Hussain L, Bawazir AA, Gaafar R. Lung cancer in the Middle East and north Africa region. J Thorac Oncol. 2019;14(11):1884–91. https://doi.org/10.1016/j.jtho.2019.02.016
Tazi MA, Er-Raki A, Benjaafar N. Cancer incidence in Rabat, Morocco: 2006–2008. Ecancermedicalscience. 2013;8;7:338. https://doi.org/10.3332/ecancer.2013.338
Galvez-Nino M, Ruiz R, Pinto JA, Roque K, Mantilla R, Raez LE, et al. Lung cancer in the young. Lung. 2020;198(1):195–200. https://doi.org/10.1007/s00408-019-00294-5
Ritchie H, Roser M. (2019) Age structure. Published online at OurWorldInData.org. Retrieved from: https://ourworldindata.org/age-structure
Zhang T, Joubert P, Ansari-Pour N, Zhao W, Hoang PH, et al. Genomic and evolutionary classification of lung cancer in never smokers. Nat Genet. 2021;53(9):1348–59. https://doi.org/10.1038/s41588-021-00920-0
Dias M, Linhas R, Campainha S, Conde S, Barroso A. Lung cancer in never smokers - what are the differences? Acta Oncol. 2017;56(7):931–5. https://doi.org/10.1080/0284186X.2017.1287944
Shan L, Zhang L, Zhu X, Wang Z, Fang S, Lin J. et al. Chinese never smokers with adenocarcinoma of the lung are younger and have fewer lymph node metastases than smokers. Respir Res. 2022;29;23(1):293. https://doi.org/10.1186/s12931-022-02199-z
Tsoi CT, Tse LA. Professional drivers and lung cancer: a systematic review and meta-analysis. Occup Environ Med. 2012;69(11):831–6. https://doi.org/10.1136/oemed-2012-100666
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, WHO Panel. The 2015 World Health Organization classification of lung tumors. J Thorac Oncol. 2015;10(9):1243–60. https://doi.org/10.1097/JTO.0000000000000630
Song MA, Benowitz NL, Berman M, Brasky TM, Cummings KM, Hatsukami DK et al. Cigarette filter ventilation and its relationship to increasing rates of lung adenocarcinoma. J Natl Cancer Inst. 2017;1;109(12):djx075. https://doi.org/10.1093/jnci/djx075
Li J, Zhu H, Sun L, Xu W, Wang X. Prognostic value of site-specific metastases in lung cancer: a population-based study. J Cancer. 2019;2;10(14):3079–3086. https://doi.org/10.7150/jca.30463
Athey VL, Walters SJ, Rogers TK. Symptoms at lung cancer diagnosis are associated with major differences in prognosis. Thorax. 2018;73(12):1177–81. https://doi.org/10.1136/thoraxjnl-2018-211596
Xing PY, Zhu YX, Wang L, Hui ZG, Liu SM, Ren JS, LuCCRES Group, et al. What are the clinical symptoms and physical signs for non-small cell lung cancer before diagnosis is made? A nation-wide multicenter 10-year retrospective study in China. Cancer Med. 2019;8(8):4055–69. https://doi.org/10.1002/cam4.2256
Canadian Strategy for Cancer Control. (2001) www.hc-sc.gc.ca/hppb/cscc/work_reports.html
Hanna SJ, Muneer A, Khalil KH. The 2-week wait for suspected cancer: time for a rethink? Int J Clin Pract. 2005;59(11):1334–9. https://doi.org/10.1111/j.1368-5031.2005.00687.x
Bourkadi D, Sahraoui K, Zaoui A, Bouchareb A, Bouzidi EE, Bennani MA. Délais De prise en charge Du cancer bronchopulmonaire primitif, expérience Du service de pneumologie B, CHU d’Oran. Rev Mal Respir. 2018;35. Supplement, A221. https://doi.org/10.1016/j.rmr.2017.10.509
Erefai O, Soulaymani A, Mokhtari A, Obtel M, Hami H. Diagnostic delay in lung cancer in Morocco: a 4-year retrospective study. Clin Epidemiol Global Health. 2022;16:101105. https://doi.org/10.1016/j.cegh.2022.101105
PDQ Adult Treatment Editorial Board. Non-small cell lung cancer treatment (PDQ): Health Professional Version. 2023 Feb 17. In: PDQ Cancer Information Summaries. Bethesda (MD): National Cancer Institute (US); 2002. PMID: 26389304.
Kwas H, Guermazi E, Khattab A, Hrizi C, Zendah I, Ghédira H. Facteurs pronostiques du cancer bronchique non à petites cellules Au Stade avancé [Prognostic factors of advanced stage non-small-cell lung cancer]. Rev Pneumol Clin. 2017;73(4):180–7. https://doi.org/10.1016/j.pneumo.2017.05.002. French.
Islam KM, Jiang X, Anggondowati T, Lin G, Ganti AK. Comorbidity and survival in lung cancer patients. Cancer Epidemiol Biomarkers Prev. 2015;24(7):1079–85. https://doi.org/10.1158/1055-9965
Polanco D, Pinilla L, Gracia-Lavedan E, Mas A, Bertran S, Fierro G, Seminario A, Gómez S, Barbé F. Prognostic value of symptoms at lung cancer diagnosis: a three-year observational study. J Thorac Dis. 2021;13(3):1485–94. https://doi.org/10.21037/jtd-20-3075
Abrao FC, de Abreu IRLB, Rocha RO, Munhoz FD, Rodrigues JHG, Batista BN. Interaction between treatment delivery delay and stage on the mortality from non-small cell lung cancer. J Thorac Dis. 2018;10(5):2813–9. https://doi.org/10.21037/jtd.2018.05.22
Tsai CH, Kung PT, Kuo WY, Tsai WC. Effect of time interval from diagnosis to treatment for non-small cell lung cancer on survival: a national cohort study in Taiwan. BMJ Open. 2020;22;10(4):e034351. https://doi.org/10.1136/bmjopen-2019-034351
Asmis TR, Ding K, Seymour L, Shepherd FA, Leighl NB, Winton TL, National Cancer Institute of Canada Clinical Trials Group. (2008). Age and comorbidity as independent prognostic factors in the treatment of non small-cell lung cancer: a review of National Cancer Institute of Canada Clinical Trials Group trials. J Clin Oncol. 2008;26(1):54–9. https://doi.org/10.1200/JCO.2007.12.8322
Lembicz M, Gabryel P, Brajer-Luftmann B, Dyszkiewicz W, Batura-Gabryel H. Comorbidities with non-small cell lung cancer: is there an interdisciplinary consensus needed to qualify patients for surgical treatment? Ann Thorac Med. 2018;13(2):101–7. https://doi.org/10.4103/atm.ATM_274_17
Pezzuto A, Trabalza Marinucci B, Ricci A, Ciccozzi M, Tonini G, D’Ascanio M, Guerrieri G, Chianese M, Castelli S, Rendina EA. Predictors of respiratory failure after thoracic surgery: a retrospective cohort study with comparison between lobar and sub-lobar resection. J Int Med Res. 2022;50(6):3000605221094531. https://doi.org/10.1177/03000605221094531
Lee JH, Wu HG, Kim HJ, Kim DW, Lee SH, Kim TM, Kim YW, Heo DS. Influence of comorbidities on the efficacy of radiotherapy with or without chemotherapy in elderly stage III non-small cell lung cancer patients. Cancer Res Treat. 2012;44(4):242–50. https://doi.org/10.4143/crt.2012.44.4.242
Blanco JA, Toste IS, Alvarez RF, Cuadrado GR, Gonzalvez AM, Martín IJ. Age, comorbidity, treatment decision and prognosis in lung cancer. Age Ageing. 2008;37(6):715–8. https://doi.org/10.1093/ageing/afn226
Jazieh AR, Onal HC, Tan DSW, Soo RA, Prabhash K, Kumar A, Huggenberger R, Robb S, Cho BC. Real-world treatment patterns and clinical outcomes in patients with stage III NSCLC: results of KINDLE, a multicountry observational study. J Thorac Oncol. 2021;16(10):1733–44. https://doi.org/10.1016/j.jtho.2021.05.003
Sakin A, Sahin S, Atci MM, Sakin A, Yasar N, Geredeli C, et al. The effect of different treatment modalities on survival in elderly patients with locally advanced non-small cell lung cancer. Pulmonology. 2021;27(1):26–34. https://doi.org/10.1016/j.pulmoe.2019.11.007
Flörsch B, Taugner J, Käsmann L, Kenndoff S, Guggenberger J, Tufman A, et al. Treatment patterns and prognosis of patients with inoperable stage III NSCLC after completion of concurrent chemoradiotherapy ± immune checkpoint inhibition: a decade-long single-center historical analysis. J Cancer Res Clin Oncol. 2023;149(7):3267–76. https://doi.org/10.1007/s00432-022-04174-z
Levy MA, Lovly CM, Pao W. Translating genomic information into clinical medicine: lung cancer as a paradigm. Genome Res. 2012;22(11):2101–8. https://doi.org/10.1101/gr.131128.111
Niu M, Yi M, Li N, et al. Predictive biomarkers of anti-PD-1/PD-L1 therapy in NSCLC. Exp Hematol Oncol. 2021;10:18. https://doi.org/10.1186/s40164-021-00211-8
Lahmadi M, Beddar L, Rouibah AL, Boumegoura A, Boufendi H, Temim A et al. Analysis of EGFR mutation status in Algerian patients with non-small cell lung cancer. Asian Pac J Cancer Prev. 2021;1;22(4):1063–1068. https://doi.org/10.31557/APJCP.2021.22.4.1063
Jazieh AR, Bounedjar A, Bamefleh H, Alfayea T, Almaghraby HQ, Belarabi A, et al. Expression of immune response markers in Arab patients with lung cancer. JCO Glob Oncol. 2020;6:1218–24. https://doi.org/10.1200/GO.20.00107
Acknowledgements
Not applicable.
Funding
No funds, grants, or other support were received.
Author information
Authors and Affiliations
Contributions
M.L. wrote the main manuscript. M.L., L.B., and S.K. contributed to conception and design of the study. M.L., L.B., T.M., N.L., and T.F. contributed to the data interpretation and collection. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and our national legislation on medical research ethics. For this retrospective study, consent to participate was not required according to the ethical standards of the national regulations and the ethics committee CCE (Comité Consultatif d’Éthique) of the Biotechnology Research Center that approved this study (No. 02/C.B.Rt/202).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lahmadi, M., Beddar, L., Ketit, S. et al. Clinicopathological characteristics and prognosis of non-small cell lung cancer in Algeria: a single-center retrospective study. BMC Cancer 24, 946 (2024). https://doi.org/10.1186/s12885-024-12709-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12709-5