Abstract
Background
Non-Hodgkin lymphoma (NHL) has been identified as a significant contributor to the cancer burden. This study investigates the incidence, mortality, and survival trends of NHL cancer in Brunei Darussalam from 2011 to 2020.
Methods
This is a registry-based retrospective study using de-identified data from the Brunei Darussalam Cancer Registry on patients diagnosed with NHL from 2011 to 2020 based on the ICD-10 codes C82-86. Statistical methods include descriptive statistics, age-specific and age-standardised incidence (ASIR) and mortality rates (ASMR), and joinpoint regression for trend analysis. Survival analysis was conducted using Kaplan-Meier plots, log-rank test, and Cox Proportional Hazards regression.
Results
From 2011 to 2020, 330 patients were diagnosed with NHL. The majority of patients were males (51.8%) and of Malay descent (82.7%). The age group most diagnosed was 55–74 years (42.3%), with a mean age at diagnosis being 55.1 years. The ASIRs were 12.12 for males and 10.39 per 100,000 for females; ASMRs were 6.11 for males and 4.76 per 100,000 for females. Diffuse large B-cell lymphoma was the most prevalent subtype, accounting for 39.1% of cases. The overall 5-year survival rate was 61.2%, with lower rates observed in older patients and those diagnosed at distant metastasis stage. Furthermore, older age and advanced stage diagnosis significantly increased mortality risk. NHL incidence and mortality rates in Brunei Darussalam remain stable over the period of 10 years, but highlights significant disparities in gender and age.
Conclusions
The findings emphasize the importance of early detection and tailored treatments, especially for high-risk groups, in managing NHL’s burden. These insights underline the need for focused healthcare strategies and continued research to address NHL’s challenges.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is the second leading cause of death globally, accounting for an estimated 9.7 million deaths in 2022 [1]. Among the various types of cancers, non-Hodgkin lymphoma (NHL) is a significant contributor to this burden, ranking between fifth and ninth in prevalence worldwide in 2020 [2]. NHL exhibits substantial variations in incidence, mortality, and survival rates across different regions. In 2022, approximately 553,010 newly diagnosed NHL cases and 250,475 NHL-related deaths were reported globally [1]. The highest incidence is seen across Europe, Northern America, and Australia/New Zealand. A rising trend in NHL incidence has been observed over the past decade, particularly in developed countries, older males, and younger population [3].
Brunei Darussalam, a country in Southeast Asia, with a population of approximately 445,400 people in 2022, has also seen an increase in NHL over the past few decades. The population consists of 52.8% males and 47.2% females, with Malay ethnicity (73.4%) making up the majority, followed by Chinese (9.5%), and other ethnicities (17.0%) [4]. Healthcare services at the primary healthcare clinics and tertiary specialist hospitals are available and provided free to citizens and permanent residents of the country [5]. Between 2011 and 2020, NHL ranked fifth in incidence among males and eighth among females in Brunei Darussalam [6].
Despite extensive studies on NHL, data from smaller nations, like Brunei Darussalam remain sparse, highlighting a critical gap in the global understanding of NHL [1, 7]. Therefore, understanding these epidemiological trends regionally is crucial for effective cancer control and management strategies. A recent study examined cancer incidence and mortality rates in Brunei Darussalam; however, it focused solely on incidence and mortality rates [6]. There have been no studies reporting on the survival trends of NHL in the region. Consequently, the epidemiology of NHL in Brunei Darussalam has not been comprehensively studied, underscoring a significant knowledge gap.
To address this gap, this study aims to provide the first comprehensive analysis of NHL in Brunei Darussalam, including not only incidence and mortality rates, but also survival trends from 2011 to 2020. This study will provide insights into the demographic and clinical characteristics of NHL patients, their association with survival outcomes, and identify areas for future research and intervention.
Materials and methods
This is a retrospective study based on population-based cancer registry. De-identified data were provided from the Brunei Darussalam Cancer Registry (BDCR) of patients diagnosed with non-Hodgkin lymphoma (NHL) from 1 January 2011 to 31 December 2020, based on the ICD-10 codes C82-C86. BDCR was established in 2001 to compile a comprehensive population-based cancer database of all diagnosed malignant cancers diagnosed in Brunei Darussalam. The collection of cancer data in Brunei Darussalam is an active process involving central pathology records, hospital department medical records, and the death registry, although cancer reporting to the BDCR is not mandated by law or regulations as a notifiable disease. However, medical and nursing professionals in hospitals, health centres, and clinics, are encouraged to report new cases to the BDCR using a standardised notification form. The introduction of the Brunei Healthcare Information Management System (BruHIMS) in 2013, a national electronic patient record system, has streamlined the process of data extraction and verification for malignant cancer cases [8]. This implementation has significantly improved the registry’s accuracy, timeliness, and comprehensiveness of cancer data.
The demographic and clinical variables collected and analysed include age at diagnosis, gender, ethnicity, district, date and stage of diagnosis, histology, date of last contact or death. Age at diagnosis was categorised into four groups: 0–34, 35–54, 55–74, and over 75 years old. The districts were divided into Brunei Muara, Tutong, Belait, and Temburong. Ethnicity was categorised as Malay, Chinese, or others. Cancer staging information presented in the BDCR was based on the Surveillance, Epidemiology, and the End result (SEER) summary staging which divides NHL spread from In-situ into localised (SEER Stage 1), regional (SEER Stages 2–5), distant metastasis (SEER Stages 6–7), and unknown (SEER Stage 9) [9].
The international classification of disease for oncology (ICD-O-3) histology code was used to classify different histological subtypes [10]. Histological subtypes were classified into 6 common groups, which are follicular lymphoma (9690, 9691, 9695, 9698), diffuse large B-cell lymphoma (DLBCL) (9680, 9688, 9735), Burkitt lymphoma, NOS (9687), T-cell non-Hodgkin lymphoma (9700, 9702, 9705, 9708, 9709, 9714, 9717, 9718, 9719, 9727, 9827, 9834, 9837), malignant lymphoma, NOS (9590, 9591, 9671) and other B-cell lymphomas (9670, 9673, 9679, 9684, 9689, 9699, 9728, 9833, 9836, 9940).
Study population
This study included only citizens and permanent residents of Brunei Darussalam. The population data used for analysis was obtained from the Department of Economic Planning and Statistics, based on official census information, which categorises the annual population into 5-year age group intervals. It should be noted that, our analysis excluded all patients diagnosed with In-situ carcinomas. All patients were followed up until the pre-specified ending time of 31st December 2021.
Statistical analysis
Descriptive statistics, including counts, percentages, mean, median, and standard deviation (SD) were used to illustrate the baseline characteristics of the patients. We performed calculation for incidence rates, mortality rates, age-specific rates, age-standardised rates using Microsoft Excel, and the data were then imported into R studio for further analyses and subsequent visualisation. Age-specific rates were calculated by dividing the number of newly diagnosed cases or deaths by the total population within a specific age group. Age-standardised incidence rates (ASIR) and age-standardised mortality rates (ASMR) were calculated as weighted averages of age-specific rates, considering the proportions of individual in specific age groups within a standard population [11].
To identify and quantify trends in NHL incidence and mortality, joinpoint regression analysis was employed to determine the best-fitting points where statistically significant changes occurred. We used the Joinpoint Regression Program, version 5.0.2, provided by the National Cancer Institute, to identify points where significant changes in the linear slope of the trend occured [12]. This approach fits the simplest model possible to the data and tests whether more complex models are necessary, i.e. whether a joinpoint, a point where the data trend changes direction or magnitude, is required. The model starts with the minimum number of joinpoints and tests whether additional joinpoints are statistically significant and should be added to the model. Joinpoint guidelines recommend a maximum of one joinpoint for studies with 7–11 data points, which was applied in our analysis [13]. The selection of the best-fitting model was based on the Bayesian Information Criterion (BIC). Incidence and mortality rates were age-standardised using the World Health Organization’s world standard population to account for differences in age distribution over time. The annual percent change (APC) for each segment between joinpoints was identified to quantify the rate of change over time. Additionally, the average annual percent change (AAPC) was calculated to summarise the overall trend for the entire study period with their corresponding 95% confidence intervals.
We examined the relationship between variables (gender, age, ethnicity, and stage of diagnosis) with histological subtypes among a sample of 330 individuals. Fishers’ exact test was used to determine if there is a statistically significant association between variables (gender, age, ethnicity, and stage of diagnosis) and the histological subtypes.
Overall survival was determined as the time from diagnosis to death from any cause or death from NHL. Patients who were lost to follow-up or were still alive after 31 December 2021, were right-censored in the analysis. Kaplan-Meier plots were used to plot survival curves, and the log-rank test was used to determine the difference in survival between groups. The overall 5-year survival rate was estimated using the Kaplan-Meier method. All statistical tests were two-sided, and we reported a 95% confidence interval (CI). Univariate and Multivariable Cox Proportional Hazards regression models were used to estimate the hazard rate, along with its 95% confidence interval. To control for potential confounding factors, we adjusted these models for several covariates such as age, ethnicity, district, gender, cancer stage, and histology. We calculated the scaled Schoenfeld’s residuals for each model. In addition, we visually examined plots of these scaled Schoenfeld’s residuals. The results of these checks did not indicate any violations of the proportional hazards assumption. P-value of less than 0.05 was considered statistically significant. Data analyses were carried out in R studio using various packages, including “ggplot2”, “dplyr”, “survival”, “survminer”, “KMsurv” and “cowplot”, with R version 4.2.2.
Ethical approval
This study was conducted in accordance with ethical principles and guidelines. Ethical approval was granted by the Medical and Health Research Ethics Committee of the Ministry of Health, Brunei Darussalam [Ref: MHREC/MOH/2022/1(1)]. This approval ensures that the research was conducted in accordance with ethical standards, including protection of participants rights, privacy, and confidentiality. Furthermore, ethical consideration was given throughout the study and the researchers ensured that the data collected was used only for the purpose of this study. Informed consent to participate was not required for this study as the data used were de-identified and no direct contact with participants was made. This waiver of consent was approved by the Medical and Health Research Ethics Committee in accordance with national regulations.
Results
Demographic and clinical characteristics of NHL patients
In the period from 2010 to 2020, a total of 330 patients were diagnosed with NHL. The years 2013 and 2020 saw the most diagnoses with 40 cases each, while the year 2012 recorded the fewest number of cases with 23 cases, as seen in Fig. 1. The mean age at diagnosis was 55.1 years (\(\:SD=19.1\)), with a median of 58.5 years. A total of 142 patients died during this period. The highest number of deaths was recorded in 2019 with 20 deaths, followed by 2015 with 18 deaths. The year 2012 recorded the least number of deaths with 7 deaths, while 2011 recorded a slightly higher count with 9 deaths.
The patients’ demographic characteristics are summarised in Table 1. There were 159 female patients (48.2%) and 171 male patients (51.8%). Most of the patients were of Malay descent (82.7%), followed by Chinese (13.0%), and the remaining 4.2% were classified as others. The age groups with the highest number of patients were 55 to 74 years old (42.3%), followed by 35 to 54 years old (27.6%), while the age groups with the fewest number of patients were 75 years and older (14.4%), followed by 0 to 34 years old (15.6%).Out of 330 cases, 126 cases had unknown stage (38.2%). Among the known stage cases, the majority were in the distant stage (30.9%), followed by regional (18.5%) and localised (12.4%) stages. The Brunei-Muara district had the highest number of cases (60.3%), followed by the Belait district (20.0%), the Tutong district (14.8%), and the Temburong district (3.0%). There were six cases (1.8%) where the district was not known. The most prevalent histological subtype was DLBCL (39.1%), ML, NOS was the next most common (36.1%), followed by OTHER B-CELL (8.8%) and T-CELL NHL (7.9%) subtypes. The least common were FL and BL, NOS which made up 3.9% and 4.2% of the total, respectively.
There were more deaths in males (53.5%) than females (46.5%). The highest number of deaths occurred in the age group of 55 to 74 years, accounting for 50.7% (72 deaths) of the total, followed by those 75 and above with 26.1% (37 deaths). Deaths among patients aged 35–54 were 16.2% (23 deaths) while the 0–34 age group recorded the fewest deaths at 7.0% (10 deaths). Geographically, the Brunei-Muara district had the highest mortality rate (56.3%), followed by the Belait district (24.6%), and the Tutong district (12.7%). The Temburong district reported the lowest number of deaths, accounting for only 2.1% (3 deaths). Malays accounted for the highest number of deaths (85.2%), followed by the Chinese (9.9%) and other ethnicities (4.9%). Most patients were in the distant-metastasis stage with 39.4% (56 deaths), followed by the regional stage at 19.0% (27 deaths), and the localised stage with 9.9% (14 deaths). For 31.7% (45 deaths), the disease stage was unknown. The majority of deaths were among patients with ML, NOS (50.7%), followed by those with DLBCL (33.8%), T-CELL NHL (5.6%), and OTHER B-CELL (4.9%). The least common were FL and BL, NOS accounting for 1.4% and 3.5% of the total deaths, respectively.
Histological classification
Table 2 presents the histopathological distribution of NHL by gender, age, ethnicity, and cancer stage. The majority of patients with each histological subtype were male, except for DLBCL. FL had the highest male percentage (84.6%), while DLBCL had the highest female percentage at (54.3%). For age at diagnosis, most FL (38.5%) and BL, NOS (35.7%) patients were in the age group of 35 to 54, whereas the majority of DLBCL (53.5%), Other B-Cell (41.4%), and ML, NOS (41.2%) patients were in the age group of 55 to 74. The highest proportion of T-cell NHL cases (42.3%) were in the youngest age group of 0 to 34 years. The least common age group for FL (7.7%), DLBCL (10.9%) and T-Cell NHL (11.5%) was 75 and above. In terms of ethnicity, the vast majority of patients across all histological subtypes were of Malay descent, with percentages ranging from 61.5% in FL to 88.5% in T-Cell NHL. Chinese ethnicity was second most common, with percentages ranging from 7.7% in T-Cell NHL to 30.8% in FL. Other ethnicities had the least representation across all histological subtypes. When analysing cancer stage at diagnosis, the majority of FL (38.5%) and ML, NOS (40.3%) patients were at the distant-metastasis stage. A significant proportion of DLBCL (47.3%), BL, NOS (71.4%), Other B-Cell (44.8%), and T-Cell NHL (50.0%) patients had an unknown stage. The localised stage was the least common across all histological subtypes, with the exception of T-Cell NHL (19.2%). The Fisher’s exact test revealed significant associations between histological subtype and both age (\(\:p<0.001\)) and cancer stage (\(\:p<0.001\)), suggesting that these variables are not independent of the histological subtype.
Incidence and mortality trends
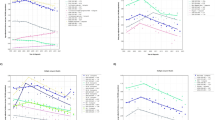
Figure 2a, b illustrate the trends of age-specific incidence and mortality rates among NHL-diagnosed patients across different age groups. For the age groups 0–34, 35–54, and 55–74, there were no notable trends in age-specific incidence and mortality rates from 2011 to 2020. However, the age group of 75 years and older exhibited varying trends, with the highest incidence rate occurring in 2011, followed by 2018, and the highest mortality rate occurring in 2019.
Figure 3a, b show that both ASIR and ASMR increased across age groups, with the highest rate observed in males aged 75 years and older, compared to females. The rates were equivalent in the remaining age groups.
The annual ASIR was 11.22 per 100,000, and the ASMR was 5.4 per 100,000 from 2011 to 2020. Meanwhile, the ASIRs for males and females were 12.12 and 10.39 per 100,000, respectively, while the ASMRs for males and females were 6.11 and 4.76 per 100,000, respectively. Over the years, ASIR and ASMR did not exhibit any increasing or decreasing trends, as the rates varied from year to year, as shown in Fig. 4a and b. However, ASIR appeared the highest in 2013 for both males and females, while the lowest were observed in 2016 and 2014 for males and females, respectively. Similarly, ASMR was highest in 2013 for males and 2018 for female patients. The lowest ASMR was observed in 2012 for female patients and 2018 for males.
Joinpoint regression analysis was conducted to identify changes in trends over time on annual cancer incidence and mortality over a 10-year period. No significant shifts were detected in the trends of cancer incidence rate and mortality rate during the 10-year period. A zero joinpoint was observed for the incidence trend in both males and females, suggesting a consistent linear trend throughout the study. Similarly, Joinpoint regression indicated a steady linear trend in mortality from 2011 to 2020. The average annual percentage change (AAPC) for incidence trends was − 1.3% (95% CI: -6.9, 5.1), -1.0% (95% CI: -11.8, 13.1) and − 1.5% (95% CI: -4.8, 2.1) for male, female, and both sexes, respectively (Table 3). The average annual percentage change (AAPC) for mortality trends was as follows: -1.5% (95% CI: -12.4, 11.4) for male, 4.5% (95% CI: -5.1, 18.5) for female, and − 6.1% (95% CI: -17.2, 5.4) for both sexes, respectively. The inclusion of zero within the confidence intervals indicated that the estimated AAPCs are not statistically significant at the 95% confidence level, suggesting no significant increase or decrease in the observed incidence and mortality rates over the study period.
Survival analysis
Survival analysis of patients diagnosed with NHL shows an overall survival rate of 71.6% (\(\:95\%\:CI:\text{66.4,76.2}\:\)) for 1-year, 62.6% (\(\:95\%\:CI:\text{56.9,67.7}\)) for 3-years, 61.2% (\(\:95\%\:CI:\:\text{55.5,66.5}\)) for 5-years, and 53.2% (95% CI:44.6,61.1) for 10-years (Fig. 5). No median survival time was observed in the overall survival of patients diagnosed with NHL. Table 4 provides a comprehensive summary of the survival data. Significant differences in the 5-year survival rate were observed across different age groups (\(\:p<0.001\)), and the stage of diagnosis (\(\:p=0.003\)) at the 5% level (Table 4). However, there were no significant differences in the survival rate based on gender (\(\:p=0.800\)), ethnicity (\(\:p=0.500\)), district (\(\:p=0.500\)), period of diagnosis (\(\:p=0.400\)), and histological subtype (\(\:p=0.100\)).
Patients diagnosed at a younger age demonstrated higher survival rates (Fig. 6; Table 4). Specifically, those diagnosed between 0 and 34 years exhibited higher survival rates compared to the older groups. As age at diagnosis increased, survival rates displayed a consistent decline. Notably, for patients diagnosed at 75 years and above, survival rates plummeted to 55.3%, 43.3%, and 37.1% at one, three, and five years respectively. Patients diagnosed at the distant-metastasis stage had the lowest survival rates, starting at 62.0% at 1-year and decreasing to 47.4% at both the 3- and 5-year marks (Fig. 7; Table 4). On the other hand, patients with localised stage had the highest survival rate, with a 1-year survival rate of 90.2%, which decreased to 82.7% at 3-years and further dropped to 77.4% at 5-years.
The hazard of death increases significantly with age (Table 5). In the multivariable analysis, patients aged 55–74 have an adjusted HR of 2.91 (\(\:p=0.003\)), while patients 75 years old and above have an adjusted HR of 4.48 (\(\:p<0.001\)) compared to the reference group (ages 0–34). The hazard is significantly higher for distant stage cancers with an adjusted HR of 2.96 (\(\:p=0.002\)) when compared to localised stages. The FL histology type was significantly associated with a lower hazard in univariate analysis (\(\:HR=0.14;\:p=0.049\)) when compared to ML, NOS, but this significance disappeared in the multivariable analysis (\(\:Adj\:HR=0.21;\:p=0.122\)). No significant difference in hazard was observed across the different districts, ethnicity, sex, and periods of diagnosis (\(\:p>0.05\)).
Discussion
The present study aimed to investigate the incidence, mortality, and survival trends of NHL patients in Brunei Darussalam over a 10-year period, from 2011 to 2020. NHL ranks among the top ten most prevalent cancers both in Brunei Darussalam and globally. Among ASEAN countries, Brunei Darussalam has the highest ASMR and the second highest ASIR, according to the WHO IARC GLOBOCAN 2022 estimates [14]. These statistics underscore the urgency and importance of effective management strategies for NHL in Brunei Darussalam. Our findings show that both the incidence and mortality rates of NHL remained relatively stable over this 10-year period, although peaks were observed in 2013 for incidence and in 2019 for mortality.
The joinpoint regression analysis conducted over this period suggested stable cancer incidence and mortality trends. We observed consistent age-adjusted incidence rates among both male and female patients, indicating a similar trend between genders. Possible contributors to the stability include improved access to healthcare and ongoing public health efforts. The stable trends observed in this study could provide a foundation for ongoing efforts to monitor and address the burden of cancer in the community. However, it is crucial to note that, despite this stability in Brunei Darussalam, projections indicate that there could be an estimated 779,000 new NHL cases worldwide by 2040 if the national rate remains unchanged [2].
Our study found that the age-standardised incidence rate (ASIR = 11.22 per 100,000) and the age-standardised mortality rate (ASMR = 5.40 per 100,000) for NHL in Brunei Darussalam are relatively higher than countries in the region such as China (ASIR = 5.0, ASMR = 2.3) in 2019 [15]. Lifestyle factors, environmental factors, and genetic predisposition could influence disease risk in Brunei compared to other parts of the world. Nevertheless, the mortality rate may be higher due to late diagnosis and inadequate treatment. The highest ASIRs were observed in North America in 2012 and in Australia in 2018, while the lowest ASIRs were reported in Central and South Asia in both 2012 and 2018 [16]. Another supporting study illustrated the highest incidence rates of NHL in Australia (ASIR = 12.5), New Zealand (ASIR = 12.5), Northern America (ASIR = 12.0), and Norther Europe (ASIR = 11.4) [17]. These observations demonstrate a significant prevalence of NHL in high-income countries. However, the highest incidence rate in high-income countries could be due to better early detection and reporting.
Our results also indicate significant variations in the incidence and mortality trends between age groups with the elderly population having higher ASIR and ASMR compared to the younger and middle-aged population. This finding is consistent with previous study which illustrated a significant increasing incidence rate among those over the age of 70. For instance, countries like China, USA, Republic of Korea, Israel, Germany, and the Netherlands had higher rates of incidence and mortality in the older population compared to the younger population [3, 16].
Moreover, DLBCL accounts for 39.1% of all cases recorded in Brunei Darussalam, making it the most common subtype. DLBCL was identified as the predominant histological subtype among NHL patients in Thailand, representing 58.1% of all subtypes studied [18]. Another similar research conducted in Bangladesh found that DLBCL accounted for 34% of all NHL cases [19]. These findings indicate the widespread prevalence of DLBCL across diverse populations, underscoring the need for further research to understand its epidemiology and clinical characteristics.
While gender disparities were evident among NHL subtypes, we found no significant association between histological subtype and gender. Nevertheless, the observation that DLBCL exhibits a higher percentage of female patients underscores the complexity of NHL subtypes and the potential for distinct biological underpinnings or unique risk factors associated with specific subtypes. A study conducted in Zambia observed similar results, whereby DLBCL affected more females than males, with a male to female ratio of 0.68 to 1 [20]. In contrast, a Swedish cohort study analysed more cases of DLBCL in males (55.8%) than females (44.2%), suggesting unclear reasons for sex differences in lymphoma incidence and mortality by subtypes [21]. However, many researchers have reported higher incidence in males than females in most histological subtypes, with few variations between males and females. Follicular lymphoma (FL) and Burkitt lymphoma (BL) were less common in Brunei Darussalam with only 3.9% and 4.2% of all cases respectively. It has been reported that FL is more prevalent in Western countries, while BL being more common in Africa [22]. These variations could potentially be attributed to differences in genetic factors and geographical locations.
In terms of age at diagnosis, some subtypes such as FL and BL, NOS, tend to affect younger individuals, primarily those aged 35 to 54, while others like DLBCL, Other B-Cell NHL, and ML, NOS, were more common among older individuals. Notably, T-cell NHL cases were more prevalent in the youngest age group, suggesting potential pediatric-specific factors in disease development. This is consistent with findings from 2016 suggesting that the prognosis for children and adolescents suffering from T-cell lymphoma is generally more unfavourable compared to younger children with other forms of NHL [23]. However, the prognosis varies with the type of T-cell lymphoma, such as peripheral T-cell lymphoma, which is rare among children and adolescents, may have a different outcome [24].
Additionally, the stage of cancer at diagnosis varies significantly among NHL subtypes, further emphasizing the complexity of this disease. Our study revealed a significant association between the stage at diagnosis and the various histological subtypes observed, suggesting potential implications for tailored treatment strategies and improved prognostic evaluation. The majority of cases in subtypes such as FL and ML, NOS, were diagnosed at the distant-metastasis stage. Patients diagnosed with advanced-stage disease often face different treatment approaches, prognosis, and overall management compared to those diagnosed at an earlier stage. This underscores the need for enhanced diagnostic strategies and awareness of the potential for aggressive NHL subtypes to present at an advanced stage, even when subtle symptoms may initially suggest otherwise.
The overall survival rates for NHL patients in Brunei were 71.6%, 62.6%, and 53.2% at 1-year, 5-years, and 10-years, respectively. These rates are comparable to those reported in the United States of America (USA) between 2000 and 2015, where the 1-year, 5-year and 10-year survival rates were 76%, 61% and 48%, respectively [25]. Another supporting study conducted in the USA and Europe reported an overall 5-year survival of 50–60% [26].
Age is found to be a significant predictor of survival in this study, with pronounced disparities observed across different age groups. Younger patients, especially those aged 0–34, showed higher survival rates. In contrast, patients diagnosed at 75 years and above had the lowest rates. This observation aligns with previous studies demonstrating a higher 5-year relative survival rate in younger age groups compared to older age groups during 2000–2018 in the USA [27]. The median age of diagnosis in Brunei is 58.5 years, while in Thailand it is 56 years [18]. The difference in median age of diagnosis could be due to various demographics, lifestyle, and risk factors that vary between the two countries. However, it is important to note that a comparison of median age of diagnosis alone does not provide a comprehensive understanding of the factors driving the difference in age distribution between the two countries; further research is necessary to identify the potential underlying factors.
The stage of diagnosis is also a significant factor for survival among NHL patients. Patients diagnosed at the distant-metastasis stage showed the lowest survival outcomes with a 5-year survival probability of 47.4%, while the survival probability for localised stage was 77.4%. This could be due to the spread of the cancer at a distant-metastasis stage making the treatment more challenging for patients diagnosed at an advanced stage. By contrast, a 5-year survival for stage I (localised stage) from 2010 to 2016 in US was 83.5%, while survival for stage IV (distant-metastasis stage) was 63.3%, which are higher when compared to Brunei Darussalam [28]. The reasons for these differences might include technological advancements in treatment methods, geographical location, genetic factors, and environmental exposures.
The hazard ratio (HR) indicated a significant association at the 5% level between distant-metastasis stage and increased risk of mortality (HR: 2.93), highlighting the critical impact of disease progression on patient survival. This is in line with findings that show stage IV patients (distant-metastasis stage) have a significantly higher risk of mortality compared to stage I patients (HR: 1.93) [25]. Additionally, our results showed an increased risk of mortality with advancing age, particularly in patients 75 years and older (HR: 4.16) compared to the 0–34 age group. Factors such as gender, ethnicity, district, and period of diagnosis were found not to impact survival.
This study has several strengths that contribute to the significance of the findings. The use of a population-based cancer registry provides a comprehensive and representative dataset, allowing for a detailed analysis of NHL trends in Brunei Darussalam. The long study period also enhances the ability to observe changes and trends over time. However, there are a few limitations to consider. While the improvement of the national cancer registries through adoption of the national electronic medical records system (BruHIMS) in 2013 and the cancer registration system (CanReg5) in 2016 have improved the accuracy of the registry database system, these changes have also introduced changes in the consistencies of the surveillance before and after the implementation. Additionally, the study did not investigate possible genetic, lifestyle, and environmental risk factors that may contribute to the differences between NHL subtypes. This information could provide a broader understanding of the disease’s prevalence and behaviour in various demographic groups. Furthermore, our study lacks information about the treatment that the NHL patients underwent, which is important to understand the impact of the disease and treatment efficacy [29]. Detailed treatment data, including the types and combination of therapies used, can provide insights into patient outcomes and help identify the most effective treatment strategies. Potential areas for improvement in future research include the incorporation of prospective data and the inclusion of genetic, lifestyle, and environmental factors to better understand their impact on NHL trends, and the collection of detailed treatment information to assess the effectiveness of different therapeutic approaches.
Conclusion
In conclusion, the study’s findings provide valuable insights into the incidence trends, mortality patterns, and survival rates of NHL in Brunei Darussalam from 2011 to 2020. While the incidence of NHL cases has remained relatively stable, it is crucial to acknowledge and address the significant burden of NHL on the healthcare system and the population in Brunei Darussalam compared to other regions. In light of these findings, there is a strong need to direct future strategies towards developing robust primary and secondary preventive measures targeting identified high-risk groups to mitigate risk factors, and investing in technologies and public health campaigns that prioritise screening and early detection. Early diagnosis not only offers better therapeutic outcomes but can significantly reduce the strain on healthcare resources and the burden on patients and communities.
Data availability
The data that supports the findings of this study are available from Ministry of Health Brunei Darussalam but restrictions apply to the availability of these data, and so are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of the Ministry of Health Brunei Darussalam.
Abbreviations
- APC:
-
Annual percentage change
- AAPC:
-
Average annual percentage change
- ASIR:
-
Age-standardised incidence rates
- ASMR:
-
Age-standardised mortality rates
- BDCR:
-
Brunei Darussalam Cancer Registry
- BL:
-
Burkitt lymphoma
- BruHIMS:
-
Brunei healthcare information management system
- CI:
-
Confidence interval
- DLBCL:
-
Diffuse large B-cell lymphoma
- FL:
-
Follicular lymphoma
- HR:
-
Hazard ratio
- NHL:
-
Non-Hodgkin lymphoma
- SD:
-
Standard deviation
- SEER:
-
Surveillance, epidemiology, and the end result
References
Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global Cancer statistics 2022: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. Cancer J Clin. 2022;74(3):229–63. https://doi.org/10.3322/caac.21834.
Sedeta E, Ilerhunmwuwa N, Wasifuddin M, Uche I, Hakobyan N, Perry J, et al. Epidemiology of Non-hodgkin Lymphoma: global patterns of incidence, mortality, and Trends. Blood. 2022;140(Supplement 1):5234–5. https://doi.org/10.1182/blood-2022-158830.
Huang J, Chan SC, Lok V, Zhang L, Lucero-Prisno DE, Xu W, et al. Global burden, risk factors, and trends of non-hodgkin lymphoma: a worldwide analysis of cancer registries. Cancer Med. 2024;13(5):e7056.
Department of Economic Planning and Statistics (DEPS) - Population. (n.d.). Retrieved June 22. 2023, from https://deps.mofe.gov.bn/SitePages/Population.aspx
Leong E, Ong SK, Jali F, Naing L. Incidence, mortality and survival analysis of epithelial ovarian cancer in Brunei Darussalam. Asian Pac J Cancer Prev. 2022;23(4):1415–23. https://doi.org/10.31557/APJCP.2022.23.4.1415.
Leong E, Ong SK, Si-Ramlee KA, Naing L. Cancer incidence and mortality in Brunei Darussalam, 2011 to 2020. BMC Cancer. 2023;23(1):466. https://doi.org/10.1186/s12885-023-10962-8.
Mafra A, Laversanne M, Gospodarowicz M, Klinger P, De Paula Silva N, Piñeros M, et al. Global patterns of non-hodgkin lymphoma in 2020. Int J Cancer. 2022;151(9):1474–81. https://doi.org/10.1002/ijc.34163.
Leong E, Madli F, Ong SK. Five-year survival rate of breast cancer patients in Brunei Darussalam. Brunei International Medical Journal. 2019; 15: 73–81. Retrieved from http://bimjonline.com/PDF/BIMJ2019;15/BIMJ2019;15-73-81/BIMJ2019;15-73-81.pdf
Young JL, Roffers SD, Ries LAG, Fritz AG, Hurlbut AA, editors. SEER Summary Staging Manual – 2000: Codes and Coding Instructions, National Cancer Institute, NIH Pub. No. 01-4969, Bethesda, MD. 2001.
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM et al. International classification of diseases for oncology (ICD-O), 3rd edition, First revision. 2013. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: A New WHO standard. Global Programme on Evidence Discussion Paper Series: No. 31. Geneva: World Health Organization; 2001.
Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3%3C335::aid-sim336%3E3.0.co;2-z.
US National Cancer Institute. Number of joinpoints. Retrieved June 30. 2024, from https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/number-of-joinpoints
World Health Organization. International Agency for Research on Cancer. CANCER TODAY. Retrieved July 1. 2024, from https://gco.iarc.who.int/today/en/dataviz/maps-heatmap?mode=population&zoom=4&cancers=34
Yao Y, Liu H, Zhao F, Zhang S, Liu X. Age-period-cohort analysis of gender differential trends in incidence and mortality of non-hodgkin lymphoma in China, 1990–2019. Front Oncol. 2022;12. https://doi.org/10.3389/fonc.2022.1056030.
Xu WF, Yang P, Wei ZW, Liu JS, Yan RL, Chen Q, et al. Correlation between the Human Development Index and the incidence and mortality of Non-hodgkin Lymphoma. Curr Med Sci. 2023;43:255–60. https://doi.org/10.1007/s11596-022-2682-5.
Chu Y, Liu Y, Fang X, Jiang Y, Ding M, Ge X, et al. Global burden, risk factors, and trends of Non-hodgkin Lymphoma in 2020 and projections to 2040: a Population-based study. Blood. 2022;140(Supplement 1):3844–5. https://doi.org/10.1182/blood-2022-168779.
Intragumtornchai T, Bunworasate U, Wudhikarn K, Lekhakula A, Julamanee J, Chansung K, et al. Non-hodgkin lymphoma in South East Asia: an analysis of the histopathology, clinical features, and survival from Thailand. Hematol Oncol. 2018;36(1):28–36. https://doi.org/10.1002/hon.2392.
Akhter A, Rahman M, Majid N, Shermin S, Saleheen M, Rajib R, et al. Histological subtypes of Non-hodgkin’s lymphoma in different age and sex groups. Bangladesh Med J. 2014;41(1):32–6. https://doi.org/10.3329/bmj.v41i1.18779.
Polepole P, Mudenda VC, Munsaka SM, Zhang L. Spectrum of lymphoma and non-hodgkin lymphomas subtypes in Zambia: a 3-year records review. J Health Popul Nutr. 2021;40(1):37. https://doi.org/10.1186/s41043-021-00261-y.
Radkiewicz C, Bruchfeld JB, Weibull CE, Jeppesen ML, Frederiksen H, Lambe M, et al. Sex differences in lymphoma incidence and mortality by subtype: a population-based study. Am J Hematol. 2022;98(1):23–30. https://doi.org/10.1002/ajh.26744.
Sapkota S, Shaikh H. Non-Hodgkin Lymphoma. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. https://pubmed.ncbi.nlm.nih.gov/32644754/
Sandlund JT, Martin MG. Non-hodgkin lymphoma across the pediatric and adolescent and young adult age spectrum. Hematol Am Soc Hematol Educ Program. 2016;1:589–97. https://doi.org/10.1182/asheducation-2016.1.589.
Mellgren K, Attarbaschi A, Abla O, Alexander S, Bomken S, Bubanska E, et al. Non-anaplastic peripheral T cell lymphoma in children and adolescents—an international review of 143 cases. Ann Hematol. 2016;95:1295–305. https://doi.org/10.1007/s00277-016-2722-y.
Singh V, Gor D, Gupta V, Jacob A, Du D, Eltoukhy H, et al. Epidemiology and determinants of survival for primary intestinal non-hodgkin lymphoma: a Population-based study. World J Oncol. 2022;13(4):159–71.https://doi.org/10.14740/wjon1504.
Trask PC, Mehta J, Abbe A, RuizSoto R. Epidemiology Projection trends for Non-hodgkin Lymphoma (NHL) and its subtypes in the United States (US) and Europe (EU). Blood. 2012;120(21):5074. https://doi.org/10.1182/blood.V120.21.5074.5074.
Xie S, Zhong Y, Feng A, Zheng S, Li Y, Zhou Y, et al. Analysis and prediction of relative survival trends in patients with non-hodgkin lymphoma in the United States using a model-based period analysis method. Front Oncol. 2022;12. https://doi.org/10.3389/fonc.2022.942122.
Thandra KC, Barsouk A, Saginala K, Padala S, Barsouk A, Rawla P. Epidemiology of Non-hodgkin’s lymphoma. Med Sci. 2021;9(1):5. https://doi.org/10.3390/medsci9010005.
Jolles S, Giralt S, Kerre T, Lazarus HM, Mustafa SS, Papanicolaou GA, et al. Secondary antibody deficiency in chronic lymphocytic leukemia and non-hodgkin lymphoma: recommendations from an international expert panel. Blood Rev. 2023;58:101020. https://doi.org/10.1016/j.blre.2022.101020.
Acknowledgements
The authors would like to thank the Brunei Darussalam Cancer Registry, Ministry of Health Brunei Darussalam for provision of de-identified data, Universiti of Brunei Darussalam for their support during the preparation of manuscript, and the Medical and Health Research Ethics Committee of Ministry of Health (MHREC) for ethics approval of this study.
Funding
The authors received no financial support for the research.
Author information
Authors and Affiliations
Contributions
MKM and EL designed the research; MKM and EL analyzed the data; SKO for data corroboration; MKM and EL wrote the paper, and MKM, EL, SKO and ZM critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was granted by the Medical and Health Research Ethics Committee of the Ministry of Health, Brunei Darussalam [Ref: MHREC/MOH/2022/1(1)]. This approval ensures that the research was conducted in accordance with ethical standards, including protection of participants rights, privacy, and confidentiality. Furthermore, ethical consideration was given throughout the study and the researchers ensured that the data collected was used only for the purpose of this study. Informed consent to participate was not required for this study as the data used were de-identified and no direct contact with participants was made. This waiver of consent was approved by the Medical and Health Research Ethics Committee in accordance with national regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mwalim, M.K., Leong, E., Ong, S.K. et al. Non-Hodgkin lymphoma incidence, mortality, and survival trends in Brunei Darussalam from 2011 to 2020. BMC Cancer 24, 994 (2024). https://doi.org/10.1186/s12885-024-12725-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12725-5