Abstract
Background
Nonresectable gastric cancer develops rapidly; thus, monitoring disease progression especially in patients receiving nivolumab as late-line therapy is important. Biomarkers may facilitate the evaluation of nivolumab treatment response. Herein, we assessed the utility of serum-based inflammatory indicators for evaluating tumor response to nivolumab.
Methods
This multicenter retrospective cohort study included 111 patients treated with nivolumab monotherapy for nonresectable advanced or recurrent gastric cancer from October 2017 to October 2021. We measured changes in the C-reactive protein (CRP)-to-albumin ratio (CAR), platelet-to-lymphocyte ratio (PLR), and neutrophil-to-lymphocyte ratio (NLR) in serum from baseline to after the fourth administration of nivolumab. Furthermore, we calculated the area under the receiver operating characteristic curves (AUC ROCs) for CAR, PLR, and NLR to identify the optimal cutoff values for treatment response. We also investigated the relationship between clinicopathologic factors and disease control (complete response, partial response, and stable disease) using the chi-squared test.
Results
The overall response rate (complete and partial response) was 11.7%, and the disease control rate was 44.1%. The median overall survival (OS) was 14.0 (95% CI 10.7‒19.2) months, and the median progression-free survival (PFS) was 4.1 (95% CI 3.0‒5.9) months. The AUC ROCs for CAR, PLR, and NLR before nivolumab monotherapy for patients with progressive disease (PD) were 0.574 (95% CI, 0.461‒0.687), 0.528 (95% CI, 0.418‒0.637), and 0.511 (95% CI, 0.401‒0.620), respectively. The values for changes in CAR, PLR, and NLR were 0.766 (95% CI, 0.666‒0.865), 0.707 (95% CI, 0.607‒0.807), and 0.660 (95% CI 0.556‒0.765), respectively. The cutoff values for the treatment response were 3.0, 1.3, and 1.4 for CAR, PLR, and NLR, respectively. The PFS and OS were significantly longer when the treatment response values for changes in CAR, PLR, and NLR were below these cutoff values (CAR: OS, p < 0.0001 and PFS, p < 0.0001; PLR: OS, p = 0.0289 and PFS, p = 0.0302; and NLR: OS, p = 0.0077 and PFS, p = 0.0044).
Conclusions
Measurement of the changes in CAR, PLR, and NLR could provide a simple, prompt, noninvasive method to evaluate response to nivolumab monotherapy.
Trial registration
This study is registered with number K2023006.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Gastric cancer is the fifth most common cancer worldwide and accounted for approximately 1.1 million (5.6%) of all new cancer cases in 2020. It has the fourth greatest cancer-related death rate, with 769,000 (7.7%) deaths estimated in the same year worldwide [1]. Various chemotherapeutic treatment regimens have been effective in randomized trials and has improved the prognosis for patients with advanced gastric cancer [2,3,4,5,6,7]. Nivolumab and other monoclonal antibodies against human programmed death receptor-1 (PD-1) have demonstrated clinical efficacy in advanced nonresectable and recurrent gastric cancers [8,9,10]. A phase 3 clinical trial, ATTRACTION-2, demonstrated that nivolumab monotherapy provides benefit to patients with advanced gastric or gastroesophageal junction cancers who had previously received at least two chemotherapy regimens [8]. Furthermore, the phase 3 ATTRACTION-4 and CHECKMATE 649 studies demonstrated the efficacy and safety of nivolumab plus chemotherapy with platinum-containing drugs, such as fluoropyrimidines, in previously untreated patients with human epidermal growth factor receptor 2 (HER2)-negative advanced gastric or gastroesophageal junction cancers [9, 10]. A systematic review and meta-analysis showed that subsequent chemotherapy after first- and second-line chemotherapies improved post-progression survival and overall survival (OS) in patients with advanced gastric cancer [11].
Gastric cancers develop faster than many other gastrointestinal cancers; therefore, it is important to detect disease progression to change the chemotherapy regimen as soon as possible [9, 12]. However, in advanced gastric cancer, peritoneal metastasis is common and renders accurate evaluation of disease progression difficult [13]. Furthermore, compared with conventional cytotoxic agents, pseudoprogression is infrequently observed with nivolumab treatment [14]. Therefore, it is urgently needed to develop promising, simple, and effective biomarkers that can be used to evaluate treatment response.
Inflammation and tumorigenesis are closely and intrinsically connected [15]. Several studies reported that serum-based inflammatory indicators, such as C-reactive protein (CRP)-to-albumin ratio (CAR), platelet-to-lymphocyte ratio (PLR), and neutrophil-to-lymphocyte ratio (NLR) are significantly negatively related to the prognosis of various cancers including advanced gastric cancer [16,17,18]. These inflammatory indicators are easy to measure in outpatient settings, economical, less invasive, and have a simple calculation method.
Tumor progression causes systemic inflammation and impaired nutritional status in patients in various cancers [19]. Therefore, we focused on the changes in these serum-based inflammatory indicators to detect tumor progression earlier. We hypothesized that measurement of the change in CAR, PLR, and NLR would differentiate progression from no or pseudoprogression in patients with advanced gastric cancer treated with nivolumab monotherapy.
Methods
Study design and patients
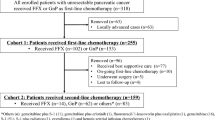
We conducted a multicenter retrospective cohort study at Fujita Health University Hospital, Keiyu Hospital, and Fujita Health University Okazaki Medical Center in Japan. Eligible patients had nonresectable advanced or recurrent gastric cancer and received nivolumab monotherapy as third-line or later therapy from October 2017 to October 2021. The inclusion criteria were histologically proven adenocarcinoma according to the Lauren classification, age of ≥ 20 years, receipt of four or more courses of nivolumab during the study period, and absence of obvious temporary infection and other synchronous or metachronous malignancy within 5 years after the start of nivolumab treatment. Finally, 111 patients were included in this study (Fig. 1).
Treatment
The patients received intravenous nivolumab at a dose of 3 or 240 mg/body every 2 weeks or 480 mg/body every 4 weeks. All patients received nivolumab within 2 weeks after the failure of the previous chemotherapy. Medical interviews, physical examinations, and blood tests were conducted at every administration of nivolumab. Tumor progression response was assessed every 6‒8 weeks using computed tomography (CT) or magnetic resonance imaging according to the Response Evaluation Criteria in Solid Tumors guidelines version 1.1 [20]. Response was classified as complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD).
Adverse events were assessed according to the Common Terminology Criteria for Adverse Events version 5.0. Treatment was continued until PD, onset of severe adverse events requiring permanent discontinuation of nivolumab, or patients’ refusal to continue treatment. The follow-up period ended in January 2022. All patient data were collected from the medical records of each institution.
Data collection and measurement of CAR, PLR, and NLR
We measured albumin, CRP and total peripheral blood lymphocyte, and neutrophil and platelet counts in the serum. CAR was defined as the CRP level divided by the total albumin level; PLR, the platelet count divided by the lymphocyte count; and NLR, the neutrophil count divided by the lymphocyte count. Changes in the ratios for all biomarkers were calculated by directly dividing the values before the first administration by those after the fourth administration. Ascites was assessed via CT and graded as follows: 0, no ascites in all slices; grade 1, ascites detected only in the upper or lower abdominal cavity; grade 2, ascites detected in both the upper and lower abdominal cavities; and grade 3, ascites extending continuously from the pelvic cavity to the upper abdominal cavity [21].
The HER2 status was confirmed via immunohistochemistry and/or fluorescence in situ hybridization.
Statistical analysis
Receiver operating characteristic (ROC) curves were constructed, and the areas under the curves (AUCs) for the change in CAR, PLR, and NLR from before nivolumab administration to after the fourth nivolumab administration were calculated to evaluate the optimal cutoff values for the treatment response. The relationships between clinicopathologic characteristics and disease control (defined as CR, PR, and SD) were analyzed using the chi-squared test.
OS was measured from the date of the first nivolumab administration to that of the last follow-up or the end of the follow-up period, whichever occurred first. Progression-free survival (PFS) was measured from the date of first nivolumab administration to that of death or progression. The OS and PFS were estimated using the Kaplan‒Meier method and were compared using the log-rank test. We considered p < 0.05 to indicate statistical significance. All statistical analyses were conducted using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [22].
Results
Patient demographics
Overall, 111 patients were enrolled in this study. All patients had not received immune checkpoint inhibitors before receiving nivolumab. The clinicopathologic features of the patients are presented in Table 1. The median age of the patients was 69 (range 36–90) years, and 81.9% were male. The median length of follow-up was 334 (range, 78–1656) days for all patients. Histology revealed intestinal tumors in 68 patients (61.3%) and diffuse-type tumors in 42 patients (37.8%). Primary-site resection was performed in 52 patients (46.8%). The tumors were HER2-positive in 16 patients (14.4%). In total, 57 patients (51.4%) experienced immune-related adverse events of any grade.
Tumor response
The best overall response was PD in 62 patients and SD in 36 patients (Table 2). The overall response rate was 11.7% (13 of 111 patients), and the disease control rate was 44.1% (49 of 111).
Survival
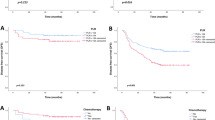
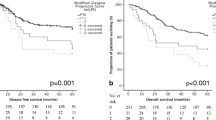
The median OS and median PFS for all patients were 14.0 (95% CI 10.7–19.2) months and 4.1 (95% CI 3.0–5.9) months, respectively (Fig. 2). The OS in the PD group was significantly poorer than that in the disease control group (p < 0.0001; Fig. 3).
ROC curve analyses
The AUC ROC values for CAR, PLR, and NLR before nivolumab administration were 0.574 (95% CI, 0.461‒0.687), 0.528 (95% CI, 0.418‒0.637), and 0.511 (95% CI, 0.401‒0.620), respectively. The values for the change in CAR, PLR, and NLR were 0.766 (95% CI, 0.666‒0.865), 0.707 (95% CI, 0.607‒0.807), and 0.660 (95% CI 0.556‒0.765), respectively (Fig. 4). The optimum cutoff values for the change in CAR, PLR, and NLR to discriminate between PD and non-PD were 3.0, 1.3, and 1.4, respectively. With these values, the sensitivity and specificity were 95.3% and 47.9%, 78.0% and 59.6%, and 70.0% and 56.1% for the CAR, PLR, and NLR changes, respectively.
ROC curves for distinguishing patients with PD and those with non-PD based on inflammatory indicators such as CAR-pre (a), PLR-pre (b), NLR-pre (c), CAR change (d), PLR change (d), PLR change (e) and NLR change (f). ROC curves: receiver operating characteristic curves PD: progressive disease, CAR-pre: CRP-to-albumin ratio right before treatment, CRP: C-reactive protein, PLR-pre: platelet-to-lymphocyte ratio before treatment, NLR-pre: neutrophil-to-lymphocyte ratio before treatment, CAR change: CAR after the fourth administration of nivolumab (CAR-4th ) divided by CAR-pre, PLR change: PLR after the fourth administration of nivolumab (PLR-4th ) divided by PLR-pre, NLR change: NLR after the fourth administration of nivolumab (NLR-4th ) divided by NLR-pre
Relationships between clinicopathologic characteristics and disease control
No significant correlation was observed between disease control and any clinicopathologic characteristics other than changes in CAR, PLR, and NLR (Table 3). We consistently found that the PFS and OS were significantly longer when the values for the change in CAR, PLR, and NLR were below the cutoff values for the treatment response (Fig. 5).
Progression-free survival and overall survival according to inflammatory indicators. Kaplan-Meier curves of progression-free survival rates of patients with a cutoff of change in CAR at 3 (a), change in PLR at 1.3 (b), change in NLR at 1.5 (c), and overall survival rates with a cutoff of change in CAR at 3 (d), change in PLR at 1.5 (e), and overall survival rates with a cutoff of change in NLR at 3 (f). CAR: CRP-to-albumin ratio, CRP: C-reactive protein, PLR: platelet-to-lymphocyte ratio, NLR: neutrophil-to-lymphocyte ratio, CAR change: CAR after the fourth administration of nivolumab divided by CAR before nivolumab administration, PLR change: PLR after the fourth administration of nivolumab divided by PLR before, nivolumab administration, NLR change: NLR after the fourth administration of nivolumab divided by NLR before nivolumab administration
Discussion
In this study, we found that the changes in the serum-based inflammatory biomarkers CAR, PLR, and NLR could help differentiate between PD and non-PD in patients with unresectable advanced or recurrent gastric cancer receiving nivolumab monotherapy as third-line or later treatment. The AUC ROC analysis revealed cutoff values that were significantly associated with disease control and prognosis.
Gastric cancer is an aggressive disease, but the use of chemotherapy after disease progression can improve prognosis in patients with advanced tumors [11]. In our study, the median OS (14.0 months) was longer than that reported by the ATTRACTION-2 trial (5.26 months) [8]. This discrepancy may be due to the differences in ethnicity in the study sample but also the frequent transition to other subsequent chemotherapy following nivolumab.
To avoid delays in changing treatment and improve survival outcomes, early detection of PD and prompt intervention are crucial [11]. This proactive approach allows for timely modifications to therapeutic strategies, which can significantly enhance the overall prognosis. However, diagnosing PD is particularly challenging in advanced gastric cancer due to the frequent occurrence of peritoneal metastases, which is difficult to evaluate with imaging modalities.
The difficulty in diagnosing PD arises from the subtle and often asymptomatic characteristic of peritoneal metastases. Standard imaging modalities and traditional biomarkers might not always provide clear indications of PD, leading to potential delays in treatment adjustments. Consequently, there is an urgent need for more reliable and easily detectable biomarkers that can signal the presence of PD at an earlier stage.
To the best of our knowledge, this is the first study to reveal the usefulness of changes in CAR, PLR, and NLR as potential biomarkers for PD in advanced gastric cancer patients.
High CAR is used as an indicator of malnutrition [23], and several studies have demonstrated that nutritional management improves prognosis in various cancers [24, 25]. In our study, however, no relationship was observed between disease control and pre-treatment serum albumin levels or body mass index. In addition, although patients who underwent gastrectomy are prone to malnutrition, the presence or absence of gastrectomy also did not correlate with the efficacy of nivolumab. Similarly, CAR, NLR, and PLR before treatment were unrelated to disease control. Only the “changes” in these serum-based inflammatory indicators were correlated with disease control. We presumed that this is because tumor progression causes systemic inflammation and impaired nutritional status in patients with gastric cancer. For example, the increase in CAR may result from the production of cytokines, such as interleukin-6 and tumor necrosis factor alpha, by gastric cancer [26]. Thus, we think that CAR change alone was not a reason for but a result of disease control.
During the study period (i.e., 2017–2021), Japanese gastric cancer treatment guidelines recommended nivolumab or irinotecan monotherapy for third- or later-line treatment of advanced gastric cancer. At present, based on the findings of the ATTRACTION-4 and CHECKMATE 649 studies, nivolumab plus chemotherapy with platinum-containing drugs and fluoropyrimidines is widely used as first-line treatment for HER2-negative advanced gastric or gastroesophageal junction cancer [9, 10]. However, grade 3‒5 drug-related adverse events occurred more frequently with nivolumab plus chemotherapy than with placebo plus chemotherapy. Thus, chemotherapy alone is favored as first-line treatment in vulnerable patients. For such patients, nivolumab monotherapy is generally reserved for late-line treatment. Furthermore, for patients who achieve disease control with nivolumab plus chemotherapy but suffer from peripheral neuropathy induced by oxaliplatin, nivolumab plus fluoropyrimidines therapy or nivolumab monotherapy will be used as maintenance treatment. Thus, biomarkers for PD detection remain important. However, PLR and NLR may be influenced by thrombocytopenia and neutropenia induced by the cytotoxic effect of combined chemotherapies.
Microsatellite instability (MSI)-high and high combined positive score (CPS) have been reported as efficacy predictors in patients with unresectable advanced or recurrent gastric cancer receiving nivolumab monotherapy. [27, 28] Patients in the MSI-high group had better PFS, and response rates were significantly higher in patients with CPS ≥ 5. However, in this study, determination of serum-based inflammatory indicators such as CAR, PLR, and NLR changes required performing blood test after four cycles of nivolumab. Therefore, they are considered useful biomarkers for assessing nivolumab treatment response rather than predicting treatment effect.
This study has several limitations. First, we did not investigate PD-L1 CPS or MSI. It has been reported that patients with gastric cancer who have high CPS (≥ 5) and MSI-high and who are treated with nivolumab plus chemotherapy have better prognosis than those with low CPS or MSI-low [10]. Second, the number of regimens before and after nivolumab administration was not standardized. However, most patients (89.2%) received nivolumab monotherapy as third-line treatment according to the recommendations of Japanese gastric cancer treatment guidelines (5th edition). Third, cases in which nivolumab treatment was discontinued after three or fewer courses were due to reasons such as severe adverse events, disease progression, and exacerbation of comorbidities. This result in the exclusion of some PD cases. Forth, this was a retrospective study; therefore, there were various sources of bias. A large-scale prospective study involving measurement of CPS and MSI is required.
Conclusions
The measurement of changes in CAR, PLR, and NLR appears to be a simple, prompt, noninvasive method to evaluate response to nivolumab monotherapy in patients with recurrent or unresectable advanced gastric cancer.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Areas Under the Curves
- CR:
-
Complete Response
- CT:
-
Computed Tomography
- OS:
-
Overall Survival
- PFS:
-
Progression-Free Survival
- PR:
-
Partial Response
- SD:
-
Stable Disease
- MSI:
-
Microsatellite Instability
- CPS:
-
Combined Positive Score
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–21. https://doi.org/10.1016/S1470-2045(08)70035-4.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–97. https://doi.org/10.1016/S0140-6736(10)61121-X.
Wilke H, Muro K, Van Cutsem E, Oh SC, Bodoky G, Shimada Y, et al. Ramucirumab plus Paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014;15:1224–35. https://doi.org/10.1016/S1470-2045(14)70420-6.
Shitara K, Doi T, Dvorkin M, Mansoor W, Arkenau HT, Prokharau A, et al. Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19:1437–48. https://doi.org/10.1016/S1470-2045(18)30739-3.
Shitara K, Bang YJ, Iwasa S, Sugimoto N, Ryu MH, Sakai D, et al. Trastuzumab Deruxtecan in previously treated HER2-positive gastric cancer. N Engl J Med. 2020;382:2419–30. https://doi.org/10.1056/nejmoa2004413.
Thuss-patience PC, Kretzschmar A, Bichev D, Deist T, Hinke A, Breithaupt K, et al. Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer - a randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur J Cancer. 2011;47:2306–14. https://doi.org/10.1016/j.ejca.2011.06.002.
Kang Y, Boku N, Satoh T, Ryu M, Chao Y, Kato K, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:2461–71. https://doi.org/10.1016/S0140-6736(17)31827-5.
Kang Y, Chen L, Ryu M, Oh D, Oh SC, Chung HC, et al. Nivolumab plus chemotherapy versus placebo plus chemotherapy in patients with HER2-negative, untreated, unresectable advanced or recurrent gastric or gastro-oesophageal junction cancer (ATTRACTION-4): a randomised, multicentre, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2022;23:234–47. https://doi.org/10.1016/S1470-2045(21)00692-6.
Shen L. First-line nivolumab plus chemotherapy versus chemotherapy as first-line treatment for advanced gastric cancer/gastroesophageal junction cancer/oesophageal adenocarcinoma (CheckMate 649): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2021;398:27–40. https://doi.org/10.1016/S0140-6736(21)00797-2.Nivolumab.
Iizumi S, Takashima A, Sakamaki K, Morita S, Boku N. Survival impact of post-progression chemotherapy in advanced gastric cancer: systematic review and meta-analysis. Cancer Chemother Pharmacol. 2018;81:981–9. https://doi.org/10.1007/s00280-018-3569-9.
Cremolini C, Antoniotti C, Rossini D, Lonardi S, Loupakis F, Pietrantonio F, et al. Upfront FOLFOXIRI plus bevacizumab and reintroduction after progression versus mFOLFOX6 plus bevacizumab followed by FOLFIRI plus Bevacizumab in the treatment of patients with metastatic colorectal cancer (TRIBE2): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 2020;21:497–507. https://doi.org/10.1016/S1470-2045(19)30862-9.
Sirody J, Kaji AH, Hari DM, Chen KT. Patterns of gastric cancer metastasis in the United States. Am J Surg. 2022;224:445–8. https://doi.org/10.1016/j.amjsurg.2022.01.024.
Chiou VL, Burotto M. Pseudoprogression and immune-related response in solid tumors. J Clin Oncol. 2015;33:3541–3.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(10). https://doi.org/10.1016/S1470-2045(14)70263-3.
Toyokawa T, Muguruma K, Yoshii M, Tamura T, Sakurai K, Kubo N, et al. Clinical significance of prognostic inflammation-based and/or nutritional markers in patients with stage III gastric cancer. BMC Cancer. 2020;20:517. https://doi.org/10.1186/s12885-020-07010-0.
Yang X, Song X, Zhang L, Wu C. Prognostic role of the pretreatment C-reactive protein/albumin ratio in gastric cancer: a systematic review and meta-analysis. Med (Baltim). 2020;99:e19362. https://doi.org/10.1097/MD.0000000000019362.
Hirahara T, Arigami T, Yanagita S, Matsushita D, Uchikado Y, Kita Y, et al. Combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with advanced gastric cancer. BMC Cancer. 2019;8(1):672.
Dolan RD, McSorley ST, Park JH, Watt DG, Roxburgh CS, Horgan PG, McMillan DC. The prognostic value of systemic inflammation in patients undergoing surgery for colon cancer: comparison of composite ratios and cumulative scores. Br J Cancer. 2018;119:40–51. https://doi.org/10.1038/s41416-018-0095-9.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer Version 1. 2009;45:228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Honda M, Kawamura H, Kobayashi H, Takiguchi K, Muto A, Yamazaki S, et al. An ascites grading system for predicting the prognosis of gastric cancer with peritoneum dissemination. Ann Gastroenterol Surg. 2020;4:660–6. https://doi.org/10.1002/ags3.12386.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
Blomberg J, Lagergren P, Martin L, Mattsson F, Lagergren J. Albumin and C-reactive protein levels predict short-term mortality after percutaneous endoscopic gastrostomy in a prospective cohort study. Gastrointest Endosc. 2011;73:29–36. https://doi.org/10.1016/j.gie.2010.09.012.
Müller-richter U, Betz C, Hartmann S, Brands RC. Nutrition management for head and neck cancer patients improves clinical outcome and survival. Nutr Res. 2017;48:1–8. https://doi.org/10.1016/j.nutres.2017.08.007.
Gustafsson UO, Oppelstrup H, Thorell A, Nygren J, Ljungqvist O. Adherence to the ERAS protocol is associated with 5-year survival after colorectal cancer surgery: a retrospective cohort study. World J Surg. 2016;40:1741–7. https://doi.org/10.1007/s00268-016-3460-y.
Porporato PE. Understanding cachexia as a cancer metabolism syndrome. Oncogenesis. 2016;5:e200. https://doi.org/10.1038/oncsis.2016.3.
Hung-Yuan Y, Chung-Pin L, Yi-Hsiang H, Shao-Jung H, Yen-Po W, Yun-Cheng H et al. Microsatellite instability, Epstein–Barr virus, and programmed cell death ligand 1 as predictive markers for immunotherapy in gastric cancer. Cancers. 2022; 3;14(1):218. https://doi.org/10.3390/cancers14010218
Takaomi H, Yukinori K, Ryohei K, Takeshi O, Jin M, Kazumasa F, et al. Multicentre biomarker cohort study on the efficacy of nivolumab treatment for gastric cancer. BJC. 2020;123:965–72. https://doi.org/10.1038/s41416-020-0975-7.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English Language review.
Funding
The authors received no financial support for this study.
Author information
Authors and Affiliations
Contributions
MI, TN, and HM participated in the conception of the study, data collection, and analyses. MI and TN drafted the manuscript. HM, KM, KS, AS, SA, MN, TT, KK, SS, IU and KS participated in the data collection and analyses. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Board of Fujita Health University Hospital (approval #K2023006) and conducted in accordance with the principles of the Declaration of Helsinki and Ethical Guidelines for Medical and Health Research Involving Human Subjects.
Consent to participate
An opt-out approach was adopted for informed consent, which was approved by the ethics board.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Inukai, M., Nishi, T., Matsuoka, H. et al. Measurement of changes in serum-based inflammatory indicators to monitor response to nivolumab monotherapy in advanced gastric cancer: a multicenter retrospective study. BMC Cancer 24, 1121 (2024). https://doi.org/10.1186/s12885-024-12813-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12813-6