Abstract
Background
This study aims to investigate preoperative prognostic factors available for intrahepatic cholangiocarcinoma (ICC) patients and propose a new preoperative prognostic scoring system for ICC that combines CA19-9 and neutrophil/lymphocyte ratio (NLR).
Methods
In this retrospective analysis, 1728 patients diagnosed with ICC and undergoing curative liver resections were studied. This study employed univariate and multivariate Cox regression to find factors affecting recurrence and overall survival (OS), and furthermore assessed how preoperative models influenced tumor traits and postoperative recurrence.
Results
The results of the multivariate Cox regression analysis indicated that two preoperative variables, NLR and Ca19-9, were independent risk factors affecting postoperative recurrence and OS in ICC patients. Based on this data, assigning a score of 0 (NLR ≤ 2.4 and Ca19-9 ≤ 37U/ml) or 1 (NLR > 2.4 and Ca19-9 > 37U/ml) to these two factors, a preoperative prognostic score was derived. According to the scoring model, patients were divided into three groups: 0 points (low-risk group), 1 point (intermediate-risk group), and 2 points (high-risk group). The 5-year recurrence and OS rates for the three groups were 56.6%, 68.2%, 77.8%, and 56.8%, 40.6%, 27.6%, respectively, with all P values < 0.001. Furthermore, high-risk group patients were more prone to early recurrence (early recurrence rates for high-, intermediate-, and low-risk groups were 56.8%, 51.5%, and 37.1%, respectively, P < 0.001) and extrahepatic metastasis (extrahepatic metastasis rates for high-, intermediate-, and low-risk groups were 31.7%, 26.4%, and 15.4%, respectively, P < 0.001). In terms of tumor characteristics, high-risk group patients had larger tumor diameters and were more likely to experience microvascular invasion, lymph node metastasis, and perineural invasion.
Conclusions
The predictive capacity of postoperative recurrence and OS rates in ICC patients is effectively captured by the preoperative scoring system incorporating NLR and CA19-9 levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intrahepatic cholangiocarcinoma (ICC), making up 10%-20% of primary liver tumors, holds the second position after hepatocellular carcinoma(HCC) [1]. Characterized by a high degree of malignancy, ICC presents a grim prognosis, with its incidence and associated mortality rising globally each year. While surgical resection stands as the primary curative approach for ICC, the 5-year survival rate post-surgery remains modest, ranging from 22 to 40% [2, 3]. Therefore, establishing a preoperative scoring system to select suitable patients for surgical treatment to achieve maximum surgical benefits is crucial. Currently, some studies have analyzed factors affecting ICC prognosis, such as microvascular invasion, lymph node metastasis, tumor differentiation, etc [4,5,6]. However, most of these variables are postoperative variables and are not easily obtainable preoperatively, greatly compromising their guidance for surgical patient selection. Although there are preoperative prediction systems to guide surgical patient selection, these studies have included fewer patients and have not mentioned their impact on recurrence.
Tumors induce systemic inflammatory cytokines and mediators that can promote angiogenesis, DNA damage, and inhibit apoptosis of cancer cells, which are associated with poor prognosis in different cancers [7,8,9]. Before the tumor is diagnosed and treatment begins, the inflammatory response can be easily detected through peripheral blood tests. Different peripheral blood parameters, including neutrophil-to-lymphocyte ratio (NLR), derived NLR, platelet-to-lymphocyte ratio, and monocyte-to-lymphocyte ratio, have surfaced as markers of systemic inflammation. These parameters have demonstrated their predictive value in assessing the prognosis of diverse malignant tumors [10,11,12,13,14,15]. Although some studies have already linked elevated NLR with poorer prognosis in patients with ICC and HCC, few studies have discussed its correlation with the risk of postoperative recurrence in ICC patients following hepatectomy [16,17,18].
Several studies have shown that an increased preoperative NLR adversely affects the prognosis in patients with ICC. However, currently, there is still no research that incorporates preoperative NLR, which is relatively easy to obtain, into a scoring system for predicting long-term prognosis in ICC. In this study, we analyzed the independent risk factors affecting the prognosis of ICC and used this as the basis to establish a preoperative predictive model for long-term prognosis.
Methods
Patients selection
Consecutive patients who underwent curative intent liver resection for histologically confirmed ICC between January 2012 and December 2018 at the Eastern Hepatobiliary Surgery Hospital (Shanghai) had their data prospectively collected and subsequently reviewed in a retrospective manner. Approval for this study was obtained from the Institutional Ethics Committees of the hospital, and each patient provided informed consent for the use of their data in research. Inclusion criteria: (i)Patients underwent radical hepatectomy. (ii) Postoperative pathology confirmed ICC. (iii) No history of prior anticancer treatment or other malignancies. (iv) All participants must be aged 18 years or older, and their Performance Status (PS) should be ≤ 2 based on the Eastern Cooperative Oncology Group (ECOG) performance scale. (v) Comprehensive clinical and laboratory data, treatment modalities, outcomes, and follow-up data are required. Exclusion criteria were as follows: (i) patients with recurrent ICC; (ii) patients with combined HCC-cholangiocarcinoma; (iii) patients with microscopic positive margins; (iv)patients with perioperative death; (v) Participants with a history of prior anticancer therapy or other malignancies are excluded;. (vi) patients with clinical evidence of infection and autoimmune disease before operation; (vii) Participants with incomplete clinicopathological data or those lost to follow-up within 90 days after resection are excluded.
The following clinicopathological variables were reviewed for which included age, sex, BMI, HBV antigen, preoperative blood tests of liver function, prothrombin time (PT), α-fetoprotein (AFP), carcinoembryonic antigen (CEA) and carbohydrate antigen 19–9 (CA19-9). The tumor pathological data included the presence of multiple tumors or satellites, maximum tumor size, microvascular invasion (MVI), lymph node metastasis, perineural invasion. Cirrhosis was confirmed by histopathological examination. The operative variables included intraoperative blood transfusion, and type of liver resection. Major hepatectomy was characterized by the resection of 3 or more Couinaud segments, whereas minor hepatectomy involved the resection of 2 or fewer segments [19]. Regional lymph nodes were dissected for intraoperatively or preoperatively diagnosed ICC, as previously reported [20]. An R0 resection was defined as the complete removal of macroscopic nodules and the absence of microscopic disease at the surgical margin [21].
Postoperative follow-up
Patients underwent follow-up appointments every 2 months during the initial 6 months, and subsequently every 6 months following liver resection. The follow-ups included assessments of peripheral blood for tumor markers like AFP, ultrasonography, and enhanced CT or magnetic resonance imaging (MRI) of the abdomen.. The study endpoints included overall survival (OS) and time to recurrence (TTR). OS was calculated from the date of liver resection to either the date of death or the date of the last follow-up. TTR was calculated from the date of liver resection to the date of the first recurrence of intrahepatic cholangiocarcinoma or the date of the last follow-up. and the patterns of recurrence which included early or late recurrence (≤ or > 24 months post-treatment), type of recurrence (intra- and extrahepatic recurrences) [22].
Statistical analysis
Statistical analyses were conducted using R software, version 4.0.0 (http://www.r-project.org). Continuous variables with a normal distribution were reported as median (IQR: interquartile ranges). Categorical variables were expressed as number (n) and proportion (%). The two-tailed Student’s t-test was utilized to compare continuous variables when applicable; otherwise, the Mann–Whitney U test was employed. Categorical variables were compared using either the chi-square test or Fisher’s exact test, as deemed appropriate. The optimal cut-off for NLR to predict postoperative prognosis was determined using a time-dependent receiver operating characteristic (ROC) curve. The calculation of OS and TTR was performed using the Kaplan–Meier method, with the log-rank test employed for comparison. Univariate and multivariable Cox regression analyses were carried out to identify independent risk factors for both OS and TTR. Variables with a significance level of P < 0.05 in the univariable analysis were incorporated into the multivariable Cox regression model using forward stepwise variable selection. P-values were two-sided with values < 0.05 considered significant.
Results
Baseline characteristics and operative variables
Throughout the study duration, 2228 consecutive patients diagnosed with ICC underwent resection with curative intent. A total of 1728 (77.5%) ICC patients who satisfied the inclusion criteria were selected for further analysis (Fig. 1). Baseline characteristics was shown in Table 1. In the included 1728 ICC patients, there were 551 patients (31.9%) aged over 60, and 1154 patients (66.8%) were male. The optimal threshold for NLR predicting prognosis was established at 2.4 through the use of time-dependent ROC curves. Among them, 942 patients (54.1%) had NLR > 2.4, and 921 patients (53.3%) had CA19-9 > 37U/ml. There were 990 patients (57.3%) with tumor diameter > 5cm, 131 patients (7.6%) with multifocal tumors, 292 patients (16.9%) with lymph node metastasis, and 84 patients (4.9%) with perineural invasion. The median (range) follow-up time was 48.6 (1–109) months.
Preoperative NLR and CA19-9 were independent prognostic factor
Supplemental Table 1 displays the statistically significant factors in TTR and OS as identified by univariate analyses. We found that GGT > 64u/L, NLR > 2.4, CA19-9 > 37 U/ml, CEA > 5ng/L, AFP > 20ng/ml, tumor diameter > 5cm, multiple tumors, presence of MVI and lymph node metastasis were identified as factors significantly associated with TTR, and age > 60 year, HBsAg positive, ALB ≤ 35g/L, GGT > 64U/L, NLR > 2.4, CA19-9 > 37U/ml, CEA > 5ng/L, transfusion, tumor diameter > 5cm, presence of MVI and lymph node metastasis were identified as factors significantly associated with OS.
Multivariate analyses identified CA19-9 > 37U/ml, NLR > 2.4, tumor diameter > 5cm, presence of MVI and lymph node metastasis as independent predictors of TTR and OS (Table 2).
Preoperative prognostic score
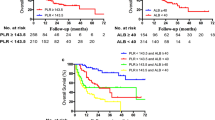
The results showed that ICC patients with NLR ≤ 2.4 compared to those with NLR > 2.4 had 1-, 3-, and 5-year recurrence rates and OS rates of 39.5%, 58.5%, 63.2% vs. 51.0%, 66.0%, 72.2%, and 82.1%, 57.9%, 49.5% vs. 70.0%, 44.4%, 33.0%, respectively, all with statistical differences (all P values < 0.001) (Fig. 2A and B). In ICC patients, those with CA19-9 levels ≤ 37 U/ml, when compared to those with CA19-9 levels > 37 U/ml, exhibited 1-, 3-, and 5-year recurrence rates and OS rates of 38.7%, 56.9%, 60.9% versus 52.0%, 67.9%, 74.9%, and 83.2%, 60.8%, 48.5% versus 68.7%, 41.0%, 33.2%, respectively. All these differences were statistically significant (all P values < 0.001) (Fig. 2C and D).
Based on the outcomes of the multivariate Cox regression analysis, a predictive model was formulated by integrating preoperative indicators CA19-9 and NLR. Assigning 0 points for CA19-9 ≤ 37 U/ml or NLR ≤ 2.4, and 1 point for CA19-9 > 37 U/ml or NLR > 2.4. Patients were stratified into low risk (0 points), intermediate risk (1 point), and high risk (2 points). The 1-, 3-, and 5-year recurrence rates for low-risk, intermediate-risk, and high-risk groups were 31.1%, 52.7%, 56.6% vs. 48.0%, 63.1%, 68.2% vs. 54.0%, 69.8%, and 77.8% (p < 0.001). The 1-, 3-, and 5-year OS rates were 90.7%, 67.8%, 56.8% vs. 73.9%, 50.2%, and 40.6% vs. 66.2%, 37.2%, 27.6% (p < 0.001) (Fig. 3A and B) The results indicate that the grouping can effectively predict the risk of postoperative recurrence and death in ICC patients undergoing curative resection.
Preoperative prognostic score association with recurrence patterns and tumors characteristics
Throughout the follow-up period, the occurrences of recurrence in the low-risk, medium-risk, and high-risk groups were 197 (47.5%), 440 (57.5%), and 337 (61.3%), respectively. The percentage of patients experiencing recurrence in the high-risk group was notably higher than that in the low-risk and medium-risk groups (P < 0.001). Early recurrence patients in the three groups were 154 (37.1%), 394 (51.5%), and 312 (56.8%), respectively, showing significant differences (P < 0.001). The number of extrahepatic metastasis in the low-risk, medium-risk, and high-risk groups were 64 (15.4%), 202 (26.4%), and 174 (31.7%), respectively. The research results indicate that with the increase in model scores, patients are more likely to experience extrahepatic metastasis (Table 3). We noted a significant positive correlation between a higher preoperative prognostic score and the following factors: tumor diameter > 5cm (p < 0.001), presence of MVI (p < 0.001), lymph node metastasis (p < 0.001), and perineural invasion (p = 0.046) (Table 4). Consequently, an elevated preoperative prognostic score could suggest an advanced stage of ICC, potentially elucidating the prognostic significance of this preoperative scoring system.
Discussion
ICC is a progressively prevalent and aggressive malignancy globally. Surgical resection remains the only curative approach for ICC [3]. Despite advancements in surgical techniques and perioperative care, the prognosis for patients with ICC remains grim [23]. In an endeavor to enhance patient outcomes, this study has devised a risk stratification tool. Utilizing preoperative indicators such as NLR and CA19-9, the prognostic model can identify patients who stand to benefit the most from resection. This model provides a convenient and effective means to guide clinical decisions for surgeons.
The predictive model based on NLR and CA19-9 demonstrates good predictive capabilities. According to the results of multifactor Cox regression analysis, preoperative indicators, NLR > 2.4 and CA19-9 > 37 U/ml are identified as independent risk factors influencing postoperative recurrence and OS in patients with ICC. With this classification, patients are stratified into low risk (0 points), moderate risk (1 point), and high risk (2 points) groups. The higher the risk, the more likely ICC patients are to experience recurrence, and the worse their overall postoperative survival. The 5-year recurrence and OS rates for the low-risk, moderate-risk, and high-risk groups are 56.6% vs. 68.2% vs. 77.8% and 56.8% vs. 40.6% vs. 27.6%, respectively. This model exhibits good discriminatory ability for the long-term prognosis of ICC patients after surgery. Moreover, NLR and CA19-9 indicators are clinically accessible and user-friendly.
The correlation between the NLR included in the model and OS has a biological basis [24, 25]. Neutrophilic granulocytes are the most common type of white blood cells and play a crucial role in the innate immune system [26, 27]. In the presence of malignancy, the number of neutrophils is upregulated, and neutrophil-mediated inflammation plays a significant role in tumorigenesis and tumor progression [28]. Although the impact of neutrophils is multifaceted and can either enhance or slow tumor growth, most published clinical studies support the notion that neutrophils promote cancer progression [29, 30]. Moreover, an increased number of neutrophils may inhibit the adaptive immune response, reducing the effectiveness of activated lymphocytes. As an indicator of this phenomenon, the NLR may be linked to unfavorable outcomes in various solid tumors. [31, 32] A high NLR may indicate intensified inflammatory reactions, compromised immune function, potentially leading to tumor spread and recurrence [7, 18, 24]. Our results are highly consistent with previous studies, confirming that a high NLR promotes postoperative recurrence and reduces OS in ICC patients, further substantiating the robust prognostic value of NLR in human malignancies.
CA19-9 stands out as the most frequently utilized prognostic tumor marker in ICC [33]. Even though it has not been formally incorporated into the eighth edition staging system of the American Joint Committee on Cancer, CA19-9 is recognized as a significant prognostic factor in the manual [34]. Additionally, the role of serum CA19-9 in increasing predictive performance has been observed in ICC staging systems [33]. In previous studies, CA19-9 has been repeatedly included in models predicting the postoperative prognosis of ICC patients and has achieved good predictive performance [33, 35, 36]. This study further validates that CA19-9 > 37 U/L is an independent risk factor influencing both tumor recurrence and OS in ICC patients.
This study reveals that ICC patients with higher scores based on the predictive model are more prone to early postoperative recurrence, and the biological characteristics of tumors are more invasive. This is manifested by larger tumor diameters, a higher proportion of MVI, lymph node metastasis, and surrounding nerve invasion. In the high-risk group, 145 cases (26.4%) of ICC patients were pathologically confirmed to have lymph node metastasis, and 100 cases (18.2%) showed MVI. In contrast, the low-risk group had only 42 cases (10.1%) with lymph node metastasis and 45 cases (10.9%) with MVI. Therefore, more aggressive surgical approaches may be necessary, including extended liver margins, anatomic hepatectomy, more thorough lymph node dissection, neoadjuvant therapy, or postoperative adjuvant anti-recurrence treatment. These aggressive surgical treatments have the potential to improve the prognosis for high-risk patients, and this study provides a basis for treatment decisions for such ICC patients.
The present study should be assessed in light of certain limitations. Primarily, similar to any retrospective analysis, selection bias might have impacted the decision of which patients were candidates for surgical resection. Patients with more aggressive oncologic features may be disproportionately under-represented because they were less likely to be offered surgery. Secondly, although a single-center study allows for standardization of surgical methods, it may not enhance the generalizability of our study results. Multicenter studies are needed to further validate the universality of the results. Third, while ROC curves are a widely accepted method in statistical analysis, they may indeed lack external validity when applied to different patient populations or settings. Last, the variables peripheral and hilar types of ICC were not included in this paper, which may affect the accuracy of the predictive model.
In conclusion, the model combining preoperative NLR and CA19-9 can more effectively predict postoperative recurrence and survival in ICC patients undergoing curative resection. Patients in the high-risk group exhibit more aggressive tumor biology. For high-risk ICC patients, adopting more aggressive treatment strategies may be necessary to achieve better long-term outcomes.
Conclusion
The predictive capacity of postoperative recurrence and OS rates in ICC patients is effectively captured by the preoperative scoring system incorporating NLR and CA19-9 levels.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICC:
-
Intrahepatic cholangiocarcinoma
- HCC:
-
Hepatocellular carcinoma
- NLR:
-
Neutrophil-to-lymphocyte ratio
- BMI:
-
Body Mass Index
- HBV:
-
Hepatitis B Virus
- PT:
-
Prothrombin time
- AFP:
-
α-Fetoprotein
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19–9
- MVI:
-
Microvascular Invasion
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- OS:
-
Overall survival
- TTR:
-
Time to recurrence
- TBIL:
-
Total bilirubin
- HBsAg:
-
Hepatitis B surface antigen
- ALB:
-
Albumin
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate aminotransferase
- GGT:
-
Gamma-glutamyl transferase
- PT:
-
Prothrombin time
- PLT:
-
Platelet
References
Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60(6):1268–89.
Moris D, Palta M, Kim C, Allen PJ, Morse MA, Lidsky ME. Advances in the treatment of intrahepatic cholangiocarcinoma: An overview of the current and future therapeutic landscape for clinicians. CA Cancer J Clin. 2023;73(2):198–222.
Ruff SM, Diaz DA, Pitter KL, Hartwell BC, Pawlik TM. Multidisciplinary management in the treatment of intrahepatic cholangiocarcinoma. CA Cancer J Clin. 2023;73(4):346–52.
Wang Y, Li J, Xia Y, Gong R, Wang K, Yan Z, Wan X, Liu G, Wu D, Shi L, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013;31(9):1188–95.
Zhou YW, Li QF, Chen YY, Wang K, Pu D, Chen XR, Li CH, Jiang L, Wang Y, Li Q, et al. Clinicopathologic features, treatment, survival, and prognostic factors of combined hepatocellular and cholangiocarcinoma: a nomogram development based on SEER database and validation in multicenter study. Eur J Surg Oncol. 2022;48(7):1559–66.
Shen H, Zhang S, Xia Y, Chen C, Huo L, Gan L, Li J, Wang K, Pawlik TM, Lau WY, et al. A Nomogram in predicting risks of intrahepatic cholangiocarcinoma after partial hepatectomy for hepatolithiasis. J Gastrointest Surg. 2021;25(9):2258–67.
Mano Y, Shirabe K, Yamashita Y, Harimoto N, Tsujita E, Takeishi K, Aishima S, Ikegami T, Yoshizumi T, Yamanaka T, et al. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg. 2013;258(2):301–5.
Sasaki M, Yoneda N, Kitamura S, Sato Y, Nakanuma Y. A serum amyloid A-positive hepatocellular neoplasm arising in alcoholic cirrhosis: a previously unrecognized type of inflammatory hepatocellular tumor. Modern Pathol. 2012;25(12):1584–93.
Wang X, Liu C, Chen J, Chen L, Ren X, Hou M, Cui X, Jiang Y, Liu E, Zong Y, et al. Single-cell dissection of remodeled inflammatory ecosystem in primary and metastatic gallbladder carcinoma. Cell discovery. 2022;8(1):101.
Shen X, Zhao H, Jin X, Chen J, Yu Z, Ramen K, Zheng X, Wu X, Shan Y, Bai J, et al. Development and validation of a machine learning-based nomogram for prediction of intrahepatic cholangiocarcinoma in patients with intrahepatic lithiasis. Hepatobiliary Surg Nutr. 2021;10(6):749–65.
Spolverato G, Maqsood H, Kim Y, Margonis G, Luo T, Ejaz A, Pawlik TM. Neutrophil-lymphocyte and platelet-lymphocyte ratio in patients after resection for hepato-pancreatico-biliary malignancies. J Surg Oncol. 2015;111(7):868–74.
Motomura T, Shirabe K, Mano Y, Muto J, Toshima T, Umemoto Y, Fukuhara T, Uchiyama H, Ikegami T, Yoshizumi T, et al. Neutrophil-lymphocyte ratio reflects hepatocellular carcinoma recurrence after liver transplantation via inflammatory microenvironment. J Hepatol. 2013;58(1):58–64.
Yugawa K, Itoh S, Yoshizumi T, Morinaga A, Iseda N, Toshima T, Harada N, Kohashi K, Oda Y, Mori M. Lymphocyte-C-reactive protein ratio as a prognostic marker associated with the tumor immune microenvironment in intrahepatic cholangiocarcinoma. Int J Clin Oncol. 2021;26(10):1901–10.
Iseda N, Itoh S, Toshida K, Nakayama Y, Ishikawa T, Tsutsui Y, Izumi T, Bekki Y, Yoshiya S, Toshima T, et al. Impact of albumin-lymphocyte-platelet-C-reactive protein index as a prognostic indicator of hepatocellular carcinoma after resection: Associated with nuclear factor erythroid 2-related factor 2. Hepatol Res. 2024;54(1):91–102.
Iseda N, Itoh S, Yoshizumi T, Tomiyama T, Morinaga A, Shimagaki T, Wang H, Kurihara T, Toshima T, Nagao Y, et al. Lymphocyte-to-C-reactive protein ratio as a prognostic factor for hepatocellular carcinoma. Int J Clin Oncol. 2021;26(10):1890–900.
Buettner S, Spolverato G, Kimbrough CW, Alexandrescu S, Marques HP, Lamelas J, Aldrighetti L, Gamblin TC, Maithel SK, Pulitano C, et al. The impact of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio among patients with intrahepatic cholangiocarcinoma. Surgery. 2018;164(3):411–8.
Liu L, Wang W, Zhang Y, Long J, Zhang Z, Li Q, Chen B, Li S, Hua Y, Shen S, et al. Declined preoperative aspartate aminotransferase to neutrophil ratio index predicts poor prognosis in patients with intrahepatic cholangiocarcinoma after hepatectomy. Cancer Res Treat. 2018;50(2):538–50.
Wang Y, Peng C, Cheng Z, Wang X, Wu L, Li J, Huang C, Guo Q, Cai H. The prognostic significance of preoperative neutrophil-lymphocyte ratio in patients with hepatocellular carcinoma receiving hepatectomy: a systematic review and meta-analysis. Int J Surg. 2018;55:73–80.
Torzilli G, McCormack L, Pawlik T. Parenchyma-sparing liver resections. Int J Surg. 2020;82s:192–7.
Lei Z, Xia Y, Si A, Wang K, Li J, Yan Z, Yang T, Wu D, Wan X, Zhou W, et al. Antiviral therapy improves survival in patients with HBV infection and intrahepatic cholangiocarcinoma undergoing liver resection. J Hepatol. 2018;68(4):655–62.
Spolverato G, Yakoob MY, Kim Y, Alexandrescu S, Marques HP, Lamelas J, Aldrighetti L, Gamblin TC, Maithel SK, Pulitano C, et al. The impact of surgical margin status on long-term outcome after resection for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2015;22(12):4020–8.
Yang P, Si A, Yang J, Cheng Z, Wang K, Li J, Xia Y, Zhang B, Pawlik TM, Lau WY, et al. A wide-margin liver resection improves long-term outcomes for patients with HBV-related hepatocellular carcinoma with microvascular invasion. Surgery. 2019;165(4):721–30.
European Association for the Study of the Liver. EASL-ILCA Clinical Practice Guidelines on the management of intrahepatic cholangiocarcinoma. J Hepatol. 2023;79(1):181–208.
Gomez D, Morris-Stiff G, Toogood GJ, Lodge JP, Prasad KR. Impact of systemic inflammation on outcome following resection for intrahepatic cholangiocarcinoma. J Surg Oncol. 2008;97(6):513–8.
Jansson H, Cornillet M, Björkström NK, Sturesson C, Sparrelid E. Prognostic value of preoperative inflammatory markers in resectable biliary tract cancer - validation and comparison of the Glasgow prognostic score and modified Glasgow prognostic score in a Western cohort. Eur J Surg Oncol. 2020;46(5):804–10.
Brandau S. The dichotomy of neutrophil granulocytes in cancer. Semin Cancer Biol. 2013;23(3):139–40.
Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13(3):159–75.
Mollinedo F. Neutrophil degranulation, plasticity, and cancer metastasis. Trends Immunol. 2019;40(3):228–42.
Giese MA, Hind LE, Huttenlocher A. Neutrophil plasticity in the tumor microenvironment. Blood. 2019;133(20):2159–67.
Felix K, Gaida MM. Neutrophil-derived proteases in the microenvironment of pancreatic cancer -active players in tumor progression. Int J Biol Sci. 2016;12(3):302–13.
Sheng Y, Peng W, Huang Y, Cheng L, Meng Y, Kwantwi LB, Yang J, Xu J, Xiao H, Kzhyshkowska J, et al. Tumor-activated neutrophils promote metastasis in breast cancer via the G-CSF-RLN2-MMP-9 axis. J Leukoc Biol. 2023;113(4):383–99.
Shan ZG, Chen J, Liu JS, Zhang JY, Wang TT, Teng YS, Mao FY, Cheng P, Zou QM, Zhou WY, et al. Activated neutrophils polarize protumorigenic interleukin-17A-producing T helper subsets through TNF-α-B7-H2-dependent pathway in human gastric cancer. Clin Transl Med. 2021;11(6):e484.
Moro A, Mehta R, Sahara K, Tsilimigras DI, Paredes AZ, Farooq A, Hyer JM, Endo I, Shen F, Guglielmi A, et al. The impact of preoperative CA19-9 and CEA on outcomes of patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2020;27(8):2888–901.
Lee JW, Lee JH, Park Y, Lee W, Kwon J, Song KB, Hwang DW, Kim SC. Prognostic predictability of American Joint Committee on Cancer 8th staging system for perihilar cholangiocarcinoma: limited improvement compared with the 7th Staging system. Cancer Res Treat. 2020;52(3):886–95.
He C, Zhang Y, Song Y, Wang J, Xing K, Lin X, Li S. Preoperative CEA levels are supplementary to CA19-9 levels in predicting prognosis in patients with resectable intrahepatic cholangiocarcinoma. J Cancer. 2018;9(17):3117–28.
Zhang J, Huang Q, Yang Y, Zhang J, Fang X, Yang Y, Liang H, Wang W, Wang Y. A novel prognostic system combining carbonic anhydrase II and preoperative CA19-9 for intrahepatic cholangiocarcinoma after curative resection. Cancer. 2023;129(7):1030–40.
Acknowledgements
We thank all patients and their families.
Funding
This work was not supported by grants.
Author information
Authors and Affiliations
Contributions
SB: Conceptualization; data curation; formal analysis; investigation; methodology; writing- original draft. XS: Data curation; resources. YD: Data curation; resources; methodology. HW: Data curation; resources. YX: Data curation; resources. JL: Data curation; resources. KW: writing-review and editing ,supervision. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Retrospective review and collection of patient data were approved by the Eastern Hepatobiliary Surgery Hospital ethics committee and each patient provided informed consent for the use of their data in research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bai, S., Shi, X., Dai, Y. et al. The preoperative scoring system combining neutrophil/lymphocyte ratio and CA19-9 predicts the long-term prognosis of intrahepatic cholangiocarcinoma patients undergoing curative liver resection. BMC Cancer 24, 1106 (2024). https://doi.org/10.1186/s12885-024-12819-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12819-0