Abstract
Background
To assess the relationship between postoperative implantable collamer lens (ICL) vault and lens height obtained from two different measurements.
Methods
A retrospective case series study enrolled eyes with horizontally implanted ICL. Crystal lens rise (CLR) and the distance between STS plane and anterior crystalline lens surface (STSL) were measured in the horizontal and vertical directions using ultrasound biomicroscopy (UBM). We compared the differences in the parameters measured in both horizontal and vertical directions. The participants were categorized into three groups according to ciliary sulcus width (CSW) which is defined as the distance between the posterior angle of the iris and the anterior angle of the ciliary process: narrow CSW group (NSG); medium CSW group (MSG); and wide CSW group (WSG). The correlations between CLR/STSL and vault were examined in each of the three groups. Biased correlation analysis was used further to contrast the correlation between CLR/STSL and vault.
Results
This retrospective study included 223 myopic eyes. Vertical STSL (VSTSL) and vertical CLR (VCLR) exhibited significantly greater values compared to their horizontal counterparts (both P < 0.05). None of the indicators were statistically different between the three groups. In both NSG and MSG, STSL/CLR correlated with vault, while in WSG, only STSL correlated with vault (r=-0.316, P = 0.013). In contrast to HCLR, the correlation between HSTSL and vault remained after controlling for HCLR (r=-0.162, P = 0.015).
Conclusions
STSL should deserve more attention in the preoperative evaluation of ICL compared to CLR especially when CSW is large.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Vault is a crucial indicator for assessing safety following implantable collamer lens (ICL) implantation. In general, an excessively low vault is associated with an increased incidence of anterior subcapsular cataracts [1], whereas an excessive vault is linked to an elevated risk of pigment dispersion and angle closure [2, 3], and the size of the ICL crystals chosen by the surgeon directly impacts vault. A study has shown that a thicker or more anteriorly positioned lens reduces vault [4]. For this reason, the researchers have used lens height which is defined as the relative height of the apex of the anterior surface of the lens from a given baseline to represent the effect of the lens on vault. However, there is no universally accepted definition of lens height. Two primary classifications: one is crystal lens rise (CLR) introduced by Baïkoff et al. [5] in 2006, and the other is the distance between STS plane and the anterior crystalline lens surface (STSL) proposed by Kojima et al. [6] in 2012. The two parameters show a negative correlation with vault [7, 8] and both are considered to be identified as significant independent variables in the ICL crystal size selection formula [9, 10]. Recently, Fan et al. [11] found that CLR differed horizontally and vertically (vertically greater than horizontally). To the best of our knowledge, no study has analyzed these two lens heights in detail to clarify whether this difference also exists in STSL and, more crucially, to clarify which parameter is of greater concern to the clinician in predicting postoperative vault.
This study utilized ultrasound biomicroscopy (UBM) to measure and analyze the distribution of two lens heights in both horizontal and vertical directions, investigating their relationships with other ocular parameters. Discussion of subgroups according to ciliary sulcus width (CSW) and biased correlation analysis were used further to contrast the correlation between CLR/STSL and vault.
Methods
Patients
This retrospective study included 223 eyes of 117 patients who underwent ICL implantation for myopic and astigmatism correction in the Eye Center of the Second Affiliated Hospital of Zhejiang University School of Medicine from September 2022 to February 2024. Inclusion criteria: age between 18 and 40 years, myopia stabilized for more than 2 years, anterior chamber depth (ACD) ≥ 2.8 mm, and implanted ICL lenses were required to be placed horizontally (rotated no more than 22.5° around the horizontal line [8]); exclusion criteria: patients with any eye disease. The study protocol was approved and the requirement to obtain informed written consent was waived by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. (NO: IR2023454). This study was performed in accordance with the tenets of the Declaration of Helsinki.
Examinations
All patients are required to undergo a comprehensive eye examination, including uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA), manifest and cycloplegic refraction, intraocular pressure (IOP) (non-contact tonometry, Canon, Japan), corneal endothelial cell density (ECD) (noncontact specular microscopy, SP-3000P, Topcon Corporation, Japan), scheimpflug tomography with Pentacam (Pentacam HR Oculus, Wetzlar, Germany) for ACD, horizontal white to white (HWTW), anterior chamber volume (ACV) and anterior chamber angle (ACA) measurement, IOL-Master 700 (Carl Zeiss Meditec, Jena, Germany) for lens thickness (LT) and axial length (AL), dilated fundus examination using a 90 D, anterior segment parameter measurements with UBM (Model SW-3200 L, Tianjin Suowei Electronic Technology Co, Ltd, Tianjin, China). The same examination and measurements are done by the same experienced physician.
Definition of UBM variables
UBM measurements were performed in a controlled lighting room (approximately 120 lx). The patient was asked to lie in the supine position, and an appropriately sized plastic eye cup filled with normal saline was placed in the conjunctival sac after topical anesthesia. To reduce the influence of accommodation, participants were then asked to keep their eyes fixed on the ceiling. The operator turned on the image acquisition mode and adjusted the ultrasound probe so that it was perpendicular to the center of the cornea. Cross-sectional scans were performed on the horizontal and vertical (90° and 180°) meridians in the state of non-ciliary muscle paralysis. Pictures showing the strongest reflections from the cornea, anterior lens capsule, and posterior lens capsule are considered eligible. The following indicators were repeated three times for each eye to ensure the accuracy of the results. (1) Distance of ciliary sulcus-to-sulcus (STS), the iris root attachment point distance. We refer to Chang et al. [12] for the measurement of STS. If the root of the iris is separated from the root of the anterior surface of the ciliary processes, STS is considered to be the distance between the basal ends of the ciliary sulcus on each side. (2) Distance of angle-to-angle (ATA), the distance between the two anterior chamber angle vertices in a line. (3) STSL, the distance between STS plane and the anterior crystalline lens surface; CLR, the distance between ATA plane and the anterior crystalline lens surface. The STSL/CLR value is defined as positive if the lens apex is located in front of the STS/ATA line. Conversely, the other one is negative. (4) CSW, the distance between the posterior angle of the iris and the anterior angle of the ciliary process [13, 14]. We used the magnification function provided by the UBM to observe the ciliary sulcus region of each image in detail. In our measurements, we found that CSW essentially reflects the positional relationship between the iris and the ciliary process, with two main scenarios: a relatively obvious space exists at the root of both; and only root contact or close contact between the two, in which case CSW is 0. If there is any doubt about CSW measurement of a particular image, we would choose another clear image to measure again or eliminate that eye. Finally, we calculate the average of CSW on both sides as CSW in that direction.
The above parameters are prefixed with “H” for horizontal direction and “V” for vertical direction. The same examination and measurements are done by the same experienced physician. All eyes were divided into three groups based on HCSW: narrow ciliary sulcus width group (NSG): HCSW ≤ 0.150 mm; medium ciliary sulcus width group (MSG): 0.150 mm < HCSW ≤ 0.250 mm; wide ciliary sulcus width group (WSG): HCSW > 0.250 mm. Parameters measured using UBM are shown in Fig. 1.
Parameters were determined on UBM images scanned horizontally and vertically over the full field of view centered on the pupil. A STS, the distance of ciliary sulcus-to-sulcus; ATA, the distance of angle-to-angle; STSL, the distance between STS plane and anterior crystalline lens surface; CLR, crystal lens rise. B CSW, ciliary sulcus width, calculate the average of the values on both sides, CSW = 0.30 mm in B
The appropriate ICL crystal size is selected based on STAAR online calculation and clinical experience, and all eye surgeries are performed by the same experienced surgeon. Recording of vault measured by a high-resolution anterior segment optical coherence tomography (AS-OCT, CASIA, Tomey Corporation, Aichi, Japan) at 1 month postoperatively.
Statistical analysis
All data were tested for normality using the Kolmogorov-Smirnov method. Where normal information was described as mean ± standard deviation, the differences between CSW subgroups were analyzed by one-way ANOVA, and each parameter’s variability in vertical and horizontal directions was analyzed by paired t-test. The skewed data were described as M (Q1, Q3), the differences between CSW subgroups were analyzed using the Kruskal-Wallis test followed by the Bonferroni post hoc test, and the variability of each parameter in vertical and horizontal directions was analyzed by the Wilcoxon signed-rank test. The chi-square test was used to compare the proportion of sex, and the ratio of ICL size among the three groups. Pearson or Spearman correlation coefficients were used to test the correlation between the parameters. The association between HCLR/HSTSL and vault was further explored by partial correlation analysis. All statistical analyses were performed using the R software (version 4.1.1), and a two-sided test of P < 0.050 was considered statistically significant.
Results
A total of 223 eyes of 117 patients aged 27.00 (23.00, 32.00) years were analyzed. For all eyes, the mean preoperative SE was − 9.06 ± 2.55 D, the mean AL was 27.13 ± 1.37 mm, and the mean vault at 1 month postoperatively was 590.51 ± 218.24 μm.
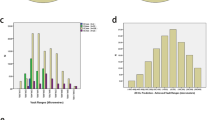
Non-uniform distribution of lens height horizontally and vertically
Table 1 provides the parameters of the UBM measurements, and there are statistical differences between STS, ATA, STSL, CLR, and CSW in the vertical direction and the corresponding values in the horizontal direction, which are overall greater vertically than horizontally. Notably, VSTSL > HSTSL in 190 eyes (85.2%); and VCLR > HCLR in 176 eyes (79.0%). Furthermore, the mean value of the difference between VSTSL and HSTSL (VSTSL - HSTSL) is 0.14 ± 0.15 mm with a maximum value of 0.60 mm; the mean value of the difference between VCLR and HCLR (VCLR - HCLR) is 0.10 ± 0.14 mm with a maximum value of 0.45 mm. Interestingly, the two maxima appear in the same eye. In general, (VSTSL - HSTSL) was larger than (VCLR - HCLR), with a mean difference of 0.03 ± 0.13 mm, which was statistically significant (p < 0.001). In 137 eyes (61.43%) of the observed eyes, (VSTSL - HSTSL) exceeded (VCLR - HCLR). Still, 77 eyes (34.53%) had a larger (VCLR - HCLR). The correlations between CLR/STSL and other parameters are shown in Fig. 2. STSL/CLR in both horizontal and vertical directions were positively correlated with age and LT (both P < 0.05), and negatively correlated with ACD, ACV, and ACA (all P < 0.05). A negative correlation was found between HCLR and AL (P = 0.005). While VCLR, HSTSL, and VSTSL were not significantly correlated with AL.
Correlation between CLR/STSL and other parameters. AL, axial length; LT, lens thickness; ACD, anterior chamber depth; ACV, anterior chamber volume; ACA, anterior chamber angle; HSTSL, horizontal STSL; VSTSL, vertical STSL; HCLR, horizontal CLR; VCLR, vertical CLR. * P < 0.05; ** P < 0.01; *** P < 0.001
Compare the predictive ability of CLR/STSL for vault
To make our conclusions more plausible, ICL lenses were requested to be implanted horizontally in all eyes in this study to explore the effect of HCSW on horizontal implantation. Table 2 provides preoperative demographic characteristics of the patients undergoing ICL implantation in different CSW groups. According to the mean HCSW value, the subjects were divided into three groups: 89 eyes in NSG, 73 eyes in MSG, and 61 eyes in WSG, and all the indicators listed in Table 2 were not statistically different between the three groups except for HCSW. Table 3 shows the correlation between the two lens heights and vault after grouping according to HCSW. Both HCLR and HSTSL were correlated with vault in all cases except in WSG where HCLR was not significantly correlated with vault. In NSG, both HCLR and HSTSL were moderately correlated with vault (r=-0.451, P < 0.001; r=-0.420, P < 0.001). The results of the biased correlation are displayed in Fig. 3. In contrast to HCLR, the correlation between HSTSL and vault remained after controlling for HCLR (r=-0.162, P = 0.015).
Discussion
The measurement of lens height in ICL is not standardized at now. To our knowledge, this is the first attempt to provide a detailed analysis of the disparities between CLR/STSL in horizontal and vertical orientations and evaluate the correlation between CLR/STSL and vault using two different methodologies. These will help clinicians increase their knowledge of CLR/STSL and guide ICL crystal size selection, thereby increasing the rate of ideal vault after surgery.
CLR can be measured directly by AS-OCT, while STSL is associated with the ciliary body, its measurement needs to be done with the help of a more penetrating UBM [15]. However, both CLR and STSL measurements in this study were performed in the UBM, and this choice was purposeful for several reasons: firstly CLR is more comparable to STSL when measured under the same conditions as it was found that light [7], and physiological conditioning [16, 17] affect the magnitude of CLR and STSL; secondly, the study by Bu et al. [18] clearly states that there is no significant difference between CLR measured by AS-OCT and UBM; and thirdly Ghoreishi et al. [19] also measured ATA and CLR using UBM.
The present study first observed that VCLR was greater than HCLR which is consistent with the findings of Fan et al. [11]. In addition, the same results, consistent with what we expected, were also seen in the STSL. Since the apex of the lens’s anterior surface is considered to be the same point in both horizontal and vertical images, this means that the two STS lines must be located in different coronal planes, in agreement with the results of the ATA [11]. For easier understanding, we plotted Fig. 4 to illustrate that HSTS is not on the same coronal plane as VSTS, and VSTS is closer to the posterior pole. What is noteworthy is that we noticed that overall (VSTSL - HSTSL) is larger than (VCLR - HCLR), which means that the height difference between VSTS and HSTS planes is larger than the height difference between VATA and HATA planes. This further highlights the distinction between the anterior and posterior chambers [20]. Based on the anatomy the main thing between the anterior chamber angle and the ciliary process is the iris and the ciliary sulcus; several studies have shown that there is no significant difference in the thickness of the iris root both horizontally and vertically [21, 22], so it is reasonable to suspect that it is the morphology of the ciliary sulcus that is responsible for this difference. Our study showed that VCSW is larger than HCSW, which somehow may explain the relationship between (VSTSL - HSTS) and (VCLR - HCLR). However, additional study is required.
Our study showed that both CLR/STSL were correlated with ACV, ACA, LT, and ACD, which is consistent with some studies that found that LT increases with age, which in turn leads to a shallowing of ACD, decrease of ACA, and decreasing of ACV [7, 23]. The results of such correlations are not uniform due to individual differences. Consistent with the study of Fan et al. [11], this study also found that only HCLR was negatively correlated with AL. We believe that the correlation between STSL and AL diminishes due to the influence of the ciliary sulcus morphology on STSL measurements.
Recently, more and more surgeons have realized that the morphology of the ciliary body plays a crucial role in vault. To date, there are fewer reports in the literature on CSW. Ye et al. [14] introduced CSW into ICL implantation in a study exploring ciliary sulcus morphology and ICL haptics location in eyes with the low vault. CSW and STS are both length parameters in the vicinity of the ciliary sulcus and are therefore equivalent in terms of measurement difficulty. The reliability and reproducibility of UBM have previously been considered to be poor, and it has been suggested that fixation of the examiner could effectively avoid such situations [24]. The UBM examination in this study was performed by the same examiner, and the CSW results of our measurements were consistent with Ye et al. [14] and Nils et al. [25]. Therefore, we consider the CSW results to be reliable in our study. Recently Li et al. [26] suggested that a standardized protocol can be effective in improving intra-examiner reliability and inter-examiner agreement, which may help to improve our examination process in the future. To better interpret the results of Table 3, it is essential to introduce some new measurement parameters. Vault can be disassembled by the concepts of the ICL arc (the difference in height between the highest point of the posterior surface of the ICL crystal and the lowest point of the ICL haptics) and the lens arc (the difference in height from the highest point of the anterior surface of the lens to the lowest point of the ICL haptics) proposed by Tan et al. [27]. Vault is to some extent the difference between the ICL arc and the lens arc. The ICL arc is the arch shape formed by the ICL in the eye which is mostly created by ciliary processes compressing the ICL haptics horizontally and the iris’ downward pressure on the ICL [12]. The accurate prediction of the lens arc as a percentage of the ICL arc is key to predicting postoperative vault, and STSL and CLR have been used as a proxy for the lens arc.
More and more studies are finding that ICL haptics are not always located in the ciliary sulcus and that numerous factors influence the location of the haptics. Roger et al. [28] examined 52 eyes with successful ICL implantation and found that in 81% (42 eyes) of cases, the ICL haptics were not in the ciliary sulcus on both the temporal and nasal sides. Dislocation of the ICL haptics results in changes in the ICL arc and the lens arc, causing the STSL/CLR to not accurately represent the lens arc and ultimately affecting the correlation of the STSL/CLR with vault [29]. Ye et al. [14] found that the incidence of the high vault is increased when CSW is narrow or even absent because at this time most of the ICL haptics are located in the ciliary sulcus with less possibility of sliding. Similar results were obtained by Chen et al. [30] and Peng et al. [13]. According to the findings, we think that in NSG and MSG, HSTSL can effectively indicate the ratio of the lens arc in the ICL arc due to the majority of ICL haptics being situated in the ciliary sulcus. In this situation, the correlation between HCLR and vault still exists, because HCLR, although not representative of the whole the lens arc, reflects the lens arc in a certain proportion. Therefore, we believe that because of the convenience of CLR measurements, CLR can temporarily replace STSL when CSW is small. On the other hand, in WSG, the ICL haptics are displaced to a higher extent or even inserted below the ciliary processes [14, 27, 31]. In addition, CLR is an ATA-based lens height that does not reflect the posterior chamber structure. The tenuous proportionality of CLR to the lens arc is difficult to maintain in WSG, and then it makes sense that the correlation between HCLR and vault disappears. On the contrary, because STSL takes into account the ciliary sulcus morphology, it reflects the lens arc more accurately than CLR, so the correlation with vault remains in WSG. When CSW exceeds 0.250 mm, CLR ceases to be a reliable predictor of postoperative vault, and STSL results become especially valuable for determining the crystal selection of ICL. In our study, the correlation coefficient between STSL and vault in NSG is for the largest of the three groups, and we suspect that there will be changes in other parameters during the process of CSW enlargement so that the position of the ICL haptics will be influenced by multiple factors. Our speculation is once again supported by the study of Ye et al. [14] who found that in addition to CSW, trabecular–ciliary angle (TCA), iris–ciliary angle (ICA), ciliary process length (CPL), and maximum ciliary body thickness (CBTmax) also correlated with ICL haptics location. In addition, the results with biased correlation indirectly suggest that the effect of CLR on vault may originate from STSL, which is exactly in line with the fact that compared to STSL, CLR represents only the tip of the iceberg of the lens arc. The question of the correlation between the two lens heights and vault comes down to the position of the ICL haptics affecting the lens arc, it is key to be able to accurately predict the position of the haptics.
With the development of science and the updating of equipment, AS-OCT is widely used in clinical practice because of the advantages of non-contact, patient compliance, and reliable results [18]. ANTERION as an advanced AS-OCT can perform wider and deeper scans, and Kim et al. [32] established the ICL vault prediction and ICL size model based on it. li et al. [33] studied the changes in the anterior segment of the eye caused by different luminance lights after ICL implantation using AS-OCT. However, AS-OCT has poor penetration compared to UBM. The posterior pigmented layer of the iris and sclera prevents the passage of infrared light from AS-OCT, rendering the ciliary body and suprachoroidal space invisible [34]. Qian et al. [35] in their study of inflammatory glaucoma found that UBM had a significant advantage over AS-OCT in visualizing the ciliary body and peripheral iris. Lincke et al. [36] found that ciliary body length (CBL) measured by AS-OCT was shortened by 2 mm compared to the true value, which they attributed to the ability of AS-OCT to poorly image posterior chamber structures. It can be seen that UBM is still superior to AS-OCT in ciliary imaging [15]. As AS-OCT has greater repeatability and accuracy, combining these two devices to study the structure of the anterior segment of the eye in the future will make the results more reliable.
The STAAR online calculation directs ICL sizing based on ACD and HWTW only, but more and more other relevant parameters are now being determined. CLR and STSL, in this study, are important components of the NK formula [37] and Reinstein’s formula [6]. Ando et al. [38] showed that the NK formula predicts vault significantly more than the actual value. Based on the results of our study, it is reasonable to suspect that CSW may have caused a bias in the NK formula and thus contributed to this result. Clarifying whether CSW affects the accuracy of ICL crystal size selection formulas (e.g., the NK formula) that include the independent variable CLR would further support our conclusions.
Our study had several limitations. Firstly, the accuracy of the relevant parameters obtained by UBM is affected by anthropogenic factors [39] and needs to be further validated. Second, only highly myopic populations in southern China were included. Due to the differences in ciliary body morphology between races [40] and the refractive status of populations in northern and southern China [41], the universality of our findings should be investigated. Thirdly, the relatively small sample size and short follow-up period of this study make it worthwhile to conduct large-sample, multicentre clinical trials in the future. Fourth, the mean AL in this study was approximately 27 mm, and whether this conclusion applies to all ranges of AL (especially AL > 28 mm [42]), needs to be further verified in future studies.
Conclusions
Our study suggests that more emphasis ought to be placed on STSL when determining ICL crystal size preoperatively because it more accurately reflects the lens arc than CLR; and STSL is the second parameter, after the CLR, that is not uniformly distributed horizontally and vertically. Clinicians should pay attention to these which may help to improve the optimal vault rate.
Data availability
All data used or analyzed during this study are available from the corresponding author upon reasonable request. Data is provided within the manuscript or supplementary information files.
Abbreviations
- ICL:
-
Implantable collamer lens
- CLR:
-
Crystal lens rise
- STSL:
-
The distance between STS plane and the anterior crystalline lens surface
- UBM:
-
Ultrasound biomicroscopy
- CSW:
-
Ciliary sulcus width
- ACD:
-
Anterior chamber depth
- UDVA:
-
Uncorrected distance visual acuity
- CDVA:
-
Corrected distance visual acuity
- IOP:
-
Intraocular pressure
- ECD:
-
Corneal endothelial cell density
- HWTW:
-
Horizontal white to white
- ACV:
-
Anterior chamber volume
- ACA:
-
Anterior chamber angle
- LT:
-
Lens thickness
- AL:
-
Axial length
- STS:
-
Distance of ciliary sulcus-to-sulcus
- ATA:
-
Distance of angle-to-angle
- H/V:
-
Horizontal/Vertical direction
- NSG:
-
Narrow ciliary sulcus width group
- MSG:
-
Medium ciliary sulcus width group
- WSG:
-
Wide ciliary sulcus width group
- AS-OCT:
-
Anterior segment optical coherence tomography
- VSTSL - HSTSL:
-
The difference between VSTSL and HSTSL
- VCLR - HCLR:
-
The difference between VCLR and HCLR
- The ICL arc:
-
The difference in height between the highest point of the posterior surface of the ICL crystal and the lowest point of the ICL haptics
- The lens arc:
-
The difference in height from the highest point of the anterior surface of the lens to the lowest point of the ICL haptics
- TCA:
-
Trabecular–ciliary angle
- ICA:
-
Iris–ciliary angle
- CPL:
-
Ciliary process length
- CBTmax:
-
Maximum ciliary body thickness
References
Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y. Posterior Chamber Phakic Intraocular Lens Implantation for the correction of myopia and myopic astigmatism: a retrospective 10-Year follow-up study. Am J Ophthalmol. 2019;206:1–10.
García-Feijoó J, Hernández-Matamoros JL, Castillo-Gómez A, Méndez-Hernández C, de la Casa JMM, Orte TM, et al. Secondary glaucoma and severe endothelial damage after silicone phakic posterior chamber intraocular lens implantation. J Cataract Refract Surg. 2004;30:1786–9.
Wei W, Yu X, Yang L, Xiong C, Zhang X. Diode laser transscleral cyclophotocoagulation causes intraocular collamer lens displacement in pseudophakic eye: a case report. BMC Ophthalmol. 2021;21:268.
Qi M-Y, Chen Q, Zeng Q-Y. The Effect of the Crystalline Lens on Central Vault after Implantable Collamer Lens Implantation. J Refract Surg. 2017;33:519–23.
Baïkoff G. Anterior segment OCT and phakic intraocular lenses: a perspective. J Cataract Refract Surg. 2006;32:1827–35.
Kojima T, Yokoyama S, Ito M, Horai R, Hara S, Nakamura T, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153:632–7. 637.e1.
Gonzalez-Lopez F, Bilbao-Calabuig R, Mompean B, Luezas J, Ortega-Usobiaga J, Druchkiv V. Determining the Potential Role of Crystalline Lens rise in vaulting in posterior Chamber Phakic Collamer Lens Surgery for correction of myopia. J Refract Surg. 2019;35:177–83.
Chang W, Niu L, Zhou X, Wang X, Yu Z, Qian Y. Risk factors Associated with Haptic Malposition in eyes implanted with implantable collamer lenses. J Cataract Refract Surg. 2023;50:276–82.
Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y. Implantable Collamer Lens sizing Method based on swept-source Anterior Segment Optical Coherence Tomography. Am J Ophthalmol. 2018;187:99–107.
Cui W, Wu X, Ren Q, Liu K, Kong F, Wu J. A new formula based on new parameters for predicting postoperative vault after posterior chamber intraocular lens implantation: a retrospective study. Quant Imaging Med Surg. 2023;13:5502–10.
Fan L, Chang Z, Xu Y, Yin X, Wang Z. The non-uniform distribution of Horizontal and Vertical Crystalline Lens rise using Optical Coherence Tomography. J Refract Surg. 2023;39:354–9.
Chang Y, Zhang L. Effect of posterior chamber structure on vault after implantable collamer lens implantation in phakic eye. Chin J Ocular Trauma Occup eye Disease. 2022;44:551–7.
Peng H, Wang F, Li JJ, Li JF, Shen XL, Liu GB, et al. [Mechanical analysis of the impact of the morphology of the iris and ciliary body on the central vault after posterior chamber phakic intraocular lens implantation]. Zhonghua Yan Ke Za Zhi. 2022;58:615–23.
Ye Y, Chen X, Yao H, Chen L, Yu N, Pei C, et al. Evaluation of ciliary body morphology and position of the implantable collamer lens in low-vault eyes using ultrasound biomicroscopy. J Cataract Refract Surg. 2023;49:1133–9.
Warjri GB, Senthil S. Imaging of the ciliary body: a major review. Semin Ophthalmol. 2022;37:711–23.
Yan P-S, Lin H-T, Wang Q-L, Zhang Z-P. Anterior segment variations with age and accommodation demonstrated by slit-lamp-adapted optical coherence tomography. Ophthalmology. 2010;117:2301–7.
Cheng M, Liu S, Chen X, Zhou X, Zhou X, Wang X. Pharmacological accommodative changes of the Anterior segment and its impact on the Vault in Implantable Collamer Lens Implantation. J Refract Surg. 2023;39:414–20.
Bu Q, Hu D, Zhu H, Jiang J, Su Y, Wu J, et al. Swept-source optical coherence tomography and ultrasound biomicroscopy study of anterior segment parameters in primary angle-closure glaucoma. Graefes Arch Clin Exp Ophthalmol. 2023;261:1651–8.
Ghoreishi M, Abdi-Shahshahani M, Peyman A, Pourazizi M. A model for predicting sulcus-to-sulcus diameter in posterior chamber phakic intraocular lens candidates: correlation between ocular biometric parameters. Int Ophthalmol. 2019;39:661–6.
X C. Effect of the difference between the White-to-White and Sulcus-to-Sulcus on Vault and the related factors after ICL implantation. Ophthalmol Therapy. 2021;10:947–55.
Garcia JPS, Spielberg L, Finger PT. High-frequency ultrasound measurements of the normal ciliary body and iris. Ophthalmic Surg Lasers Imaging. 2011;42:321–7.
Henzan IM, Tomidokoro A, Uejo C, Sakai H, Sawaguchi S, Iwase A, et al. Ultrasound biomicroscopic configurations of the anterior ocular segment in a population-based study the Kumejima Study. Ophthalmology. 2010;117:1720–8. 1728.e1.
Lei Q, Wang Y, Zhou H, Cao D, Hu J, Zhang W, et al. Anterior chamber parameters in cataract surgery candidates from middle China. Med (Baltim). 2022;101:e32211.
Yokoyama S, Kojima T, Horai R, Ito M, Nakamura T, Ichikawa K. Repeatability of the ciliary sulcus-to-sulcus diameter measurement using wide-scanning-field ultrasound biomicroscopy. J Cataract Refract Surg. 2011;37:1251–6.
Mungan N, Nischal KK, Héon E, MacKeen L, Balfe JW, Levin AV. Ultrasound biomicroscopy of the eye in cystinosis. Arch Ophthalmol. 2000;118:1329–33.
Li J, Drechsler J, Lin A, Widlus M, Qureshi A, Stoleru G, et al. Repeatability and Reliability of Quantified Ultrasound Biomicroscopy Image Analysis of the ciliary body at the pars Plicata. Ultrasound Med Biol. 2021;47:1949–56.
Tan W, Wang Z, Zeng Q, Lei X, Pan C, Shu B, et al. The influence of iris -ciliary angle (ICA) on the vault after implantation of V4c implantable collamer lens: a chain mediation model of ICL haptic related factors. BMC Ophthalmol. 2023;23:403.
Zaldivar R, Zaldivar R, Adamek P, Quintero G, Cerviño A. Descriptive analysis of footplate position after myopic implantable collamer Lens Implantation using a very high-frequency Ultrasound Robotic scanner. Clin Ophthalmol. 2022;16:3993–4001.
W T, Q C, Z RY. W, Q Z, X L, Characteristics and factors associated with the position of the haptic after ICL V4C implantation. J Cataract Refract Surg. 2023;49.
Chen Q, Tan W, Lei X, Pan C, Jin L, Zeng Q, et al. Clinical prediction of Excessive Vault after Implantable Collamer Lens Implantation using ciliary body morphology. J Refract Surg. 2020;36:380–7.
Petternel V, Köppl C-M, Dejaco-Ruhswurm I, Findl O, Skorpik C, Drexler W. Effect of accommodation and pupil size on the movement of a posterior chamber lens in the phakic eye. Ophthalmology. 2004;111:325–31.
Kim T, Kim SJ, Lee BY, Cho HJ, Sa BG, Ryu IH, et al. Development of an implantable collamer lens sizing model: a retrospective study using ANTERION swept-source optical coherence tomography and a literature review. BMC Ophthalmol. 2023;23:59.
Li X, Wang M, Dong W, Cai J. Anterior segment structure changes caused by different luminance light after implantable collamer lens surgery. BMC Ophthalmol. 2023;23:281.
Mansouri K, Sommerhalder J, Shaarawy T. Prospective comparison of ultrasound biomicroscopy and anterior segment optical coherence tomography for evaluation of anterior chamber dimensions in European eyes with primary angle closure. Eye (Lond). 2010;24:233–9.
Qian Y, Liu L, Shi Y, Wang M, Li M, Zou J. Assessment of Anterior Chamber by Ultrasound Biomicroscopy and Anterior Segment Optical Coherence Tomography in patients with inflammatory Glaucoma. J Int Med Res. 2019;47:5950–6.
Lincke J-B, Keller S, Amaral J, Zinkernagel MS, Schuerch K. Ciliary body length revisited by anterior segment optical coherence tomography: implications for safe access to the pars plana for intravitreal injections. Graefes Arch Clin Exp Ophthalmol. 2021;259:1435–41.
Nakamura T, Nishida T, Isogai N, Kojima T, Sugiyama Y, Yoshida Y. Evaluation of implantable collamer lens sizing developed by reviewing the horizontal compression-vault coefficient. J Cataract Refract Surg. 2023;49:525–30.
Ando W, Kamiya K, Hayakawa H, Takahashi M, Shoji N. Comparison of phakic intraocular Lens Vault using Conventional Nomogram and Prediction Formulas. J Clin Med. 2020;9:4090.
García-Feijoó J, Alfaro IJ, Cuiña-Sardiña R, Méndez-Hernandez C, Del Castillo JMB, García-Sánchez J. Ultrasound biomicroscopy examination of posterior chamber phakic intraocular lens position. Ophthalmology. 2003;110:163–72.
He N, Wu L, Qi M, He M, Lin S, Wang X et al. Comparison of ciliary body anatomy between American caucasians and ethnic Chinese using Ultrasound Biomicroscopy. Curr Eye Res. 2015;:1–7.
Leng L, Zhang J, Xie S, Ding W, Ji R, Tian Y, et al. Effect of Sunshine Duration on Myopia in Primary School students from Northern and Southern China. Int J Gen Med. 2021;14:4913–22.
Jin G, Liu Z, Wang L, Zhu Y, Luo L, Liu Y. Corneal biometric features and their Association with Axial length in high myopia. Am J Ophthalmol. 2022;238:45–51.
Acknowledgements
None.
Funding
The study was conducted by the Research and Development Plan of Zhejiang Science and Technology Department (NO.2023C03089) and Key Research and Development Projects of Zhejiang Science and Technology Plan (NO.2021C03103).
Author information
Authors and Affiliations
Contributions
YJN and TS were involved in the design and conduct of the study and were major contributors to writing the manuscript; HHJ and KLZ collected the data and helped in designing tables and figures; YD and YPW collected the data and provided statistical analysis; TS and PJQ critically revised the manuscript; PJQ and CYH offered financial and technical support; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved and the requirement to obtain informed written consent was waived by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. (NO: IR2023454). This study was performed in accordance with the tenets of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ni, Y., Wu, Y., Dong, Y. et al. Lens height paraments comparison according to ciliary sulcus width (CSW): a pilot study of the predictive role of CLR and STSL for vault after ICL implantation. BMC Ophthalmol 24, 355 (2024). https://doi.org/10.1186/s12886-024-03631-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03631-2