Abstract
Background
This study aimed to observe corneal and retinal thicknesses at 5 years after femtosecond laser-assisted in situ keratomileusis (FS-LASIK) and small incision lenticule extraction (SMILE) for myopia, investigate the effect of epithelial remodeling on refractive status and visual quality, and compare retinal thicknesses among fundus tessellation grades.
Methods
Patients who received FS-LASIK or SMILE 5 years before were enrolled in this cross-sectional study. After 1:1 propensity score matching, each surgical group obtained 177 patients (177 eyes). Examinations including visual acuity, refraction, corneal and retinal thicknesses, corneal higher-order aberrations (HOAs), and fundus photography were performed in this visit at 5 years after surgery. The Quality of Vision (QoV) questionnaire was used to assess visual symptoms and overall satisfaction. Corneal and retinal thicknesses between groups were compared, contributing factors were analyzed, and correlations with postoperative refractive status, HOAs, QoV scores and overall satisfaction were evaluated.
Results
The discrepancy of epithelial thickness between central and pericentral zones in FS-LASIK group was larger than that in SMILE group, which was negatively correlated with postoperative spherical equivalent (SE), positively correlated with spherical aberration (all P < 0.05), but not correlated with QoV scores and overall satisfaction (all P > 0.05) in both surgical groups. There was no statistical difference in stromal thickness and total corneal thickness (all P > 0.05). Most annuluses of epithelial and stromal thicknesse were linearly related to preoperative SE (all P < 0.05). The macular thickness, ganglion cell complex thickness, and retinal nerve fiber layer thickness exhibited comparable values between two surgical groups and four fundus tessellation grades, with no significant association observed with postoperative SE (all P > 0.05).
Conclusion
The tendency that epithelial thickness in central zone was thicker than peripheral zone was more obvious at 5 years after FS-LASIK compared to SMILE. This uneven distribution of epithelial thickness might play a role in myopic regression and the changes in HOAs, especially in patients with high myopia, but it had little effect on patients’ subjective visual quality and satisfaction. Retinal thicknesses were not affected by these two surgical methods, and they did not appear to be the clinical indicators for myopic regression or fundus tessellation progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Femtosecond laser-assisted in situ keratomileusis (FS-LASIK) and small incision lenticule extraction (SMILE) have become the preferred surgical procedures for correcting myopia and myopic astigmatism [1]. FS-LASIK has been in clinical practice for years, and its efficacy and safety also have been confirmed [2]. SMILE, in which the intrastromal lenticule is removed through a small incision of 2 mm in length so the side effects associated with the flap creation could be avoided, [3] gains popularity progressively [4]. Corneal epithelium has a potential to compensate the change of surface or irregular of stroma by altering its thickness [5]. After FS–LASIK and SMILE such remodeling has been observed in short-term follow-up [6,7,8,9,10,11]. For the accuracy of myopic correction and the prevention of ectasia after surgery, precise prediction of stromal reduction is important. But previous studies have revealed the deviation between the amount of planed and achieved stroma reduction [12,13,14]. Thus, further studies with longer follow-up period are needed to describe the characteristics of epithelial and stromal distribution and analyze their influence. In addition, myopia with elongation of ocular axial length could bring a series of fundus changes, and the long-term safety of fundus after surgery is of concern.
This study aimed to observe epithelial and stromal thicknesses distribution at 5 years after these two different surgical methods by spectral domain optical coherence tomography (SD-OCT), explore their contributing factors, evaluate the effect of epithelial thickness on refractive status and visual quality, and compare retinal thicknesses among fundus tessellation grades.
Methods
This is a cross-sectional study. A visit at 5 years after surgery was conducted for patients who received FS-LASIK and SMILE for myopia and myopic astigmatism in Beijing Tongren Hospital from January 2015 to November 2017. The inclusion criteria were as follows: over 18 years of age at surgery; preoperative spherical equivalent (SE) ranged from − 12.00D to -1.00D; stable refraction (alternation of 1.00D or less) within 2 years; preoperative corrected distance visual acuity (CDVA) was 20/20 or better; stopped wearing corneal contact lens for 2 weeks, rigid contact lenses for 1 month and orthokeratology lens for more than 3 months. The exclusion criteria were as follows: presence or history of ocular and systemic diseases, or history of ocular surgery. All eligible patients participating in this study were divided into two surgical groups. According to preoperative SE, they were also separated into low-moderate myopia group (-6.00D < SE≤-1.00D) and high myopia group (SE≤-6.00D). And their age at surgery, gender, preoperative flattest keratometry (Kf) and steepest keratometry (Ks) measured by TMS-4 (Tomey Corporation, Nagoya, Japan), central corneal thickness measured by Lenstar LS 900 (Haag-Streit AG, Koeniz, Switzerland), and fundus examination using binocular indirect ophthalmoscopy were also consulted and recorded.
This study was approved by the Institutional Review Board of Beijing Tongren Hospital and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Surgical technique
Surgeries were performed by three experienced surgeons (FZ, CZ, YQ). In FS-LASIK VisuMax femtosecond laser system (Carl Zeiss Meditec AG, Jena, Germany) was used to create the corneal flap. The pulse energy was 130nJ. The intended flap thickness was 95–110 μm. The position of the hinge was set at the 12 o’clock. Lifting the flap, the VISX STAR S4 (VISX Inc, Santa Clara, California, America) excimer laser was used to perform stromal ablation, and the diameter of the optical zone was 6.0–6.5 mm. Then the flap was carefully repositioned over the stroma.
SMILE was performed using the VisuMax 500-kHz femtosecond laser system (Carl Zeiss Meditec AG, Jena, Germany). The pulse energy was 130nJ. The intended cap thickness was 110–130 μm and the diameter of the optical zone was 6.0–6.5 mm. A 2-mm incision was made at the position of 11 or 12 o’clock. When the upper and lower layers had been separated, the lenticule was removed through the incision.
Measurements
All patients received a complete clinical examination in this visit at 5 years after surgery, including uncorrected distance visual acuity (UDVA) and CDVA, noncontact tonometry, slit-lamp evaluation, manifest refraction. Refractive data of early postoperative period were lacked in our cross-sectional study, so basing on the target refraction of 0.00D, myopic regression was defined as UDVA of < 20/20 and postoperative SE value of <-0.50D.
The Quality of Vision (QoV) questionnaire was used to assess 10 visual symptoms including glare, halos, hazy vision, starbursts, blurred vision, double or multiple images, distortion, fluctuation in vision, focusing difficulties, and difficulty judging distance or depth perception. Each symptom has 3 rating scales: frequency (0 = never, 1 = occasionally, 2 = quite often, 3 = very often), severity (0 = not at all, 1 = mild, 2 = moderate, 3 = severe), and bothersome (0 = not at all, 1 = a little, 2 = quite, 3 = very) [15]. Patients were also asked about their overall satisfaction with the procedure (0 = very dissatisfied, 1 = dissatisfied, 2 = general, 3 = less satisfied, 4 = satisfied, 5 = very satisfied).
RTVue-100 (Optovue, Inc., Fremont, USA) was used to measure corneal and retinal thicknesses and performed by a single trained investigator (JL). “Pachymetry” scan mode was selected to measure epithelial, stromal, and total corneal thicknesses. The scan was triggered manually when both horizontal and vertical reflection stripes were simultaneously observed. Maps were divided into 17 sections: a central 2-mm diameter zone, 8 paracentral sections within an annulus between the 2- and 5- mm diameter rings, and 8 pericentral sections within an annulus between the 5- and 6- mm diameter rings. △ET-1, △ST-1 and △CT-1 were calculated as mean epithelial, stromal, and total corneal thicknesses in central zone minus that in paracentral zone respectively. And △ET-2, △ST-2 and △CT-2 represented the differences between central and pericentral zones. “Retina” scan mode was selected to measure the macular thickness. The scan was manually triggered after aligning the fovea. Macular thickness maps were divided into 9 sections: fovea representing the area within 1 mm diameter, 4 sections of parafovea within an annulus between the 1- and 3- mm diameter rings, 4 sections of perifovea within an annulus between the 3- and 5- mm diameter rings. “GCC” scan mode was selected to measure the ganglion cell complex thickness which contained internal limiting membrane to inner plexiform layer, centered 1 mm temporal to fovea and across 6-mm diameter area. Thicknesses in the superior and inferior zones were recorded. “ONH” scan mode was selected to measure the retinal nerve fiber layer thickness. Aligning the optic disc and the scan was triggered manually. The diameter of the scan was 3.4 mm. And the retinal nerve fiber layer map included temporal, superior, nasal, and inferior zones. Data of patients’ right eyes were selected for statistics.
Whole corneal higher-order aberrations (HOAs) of central 6-mm zone were obtained using Pentacam (Oculus, Wetzlar, Germany). Measurements were performed by a single trained investigator (JQ) under standard scotopic ambience light condition when pupil size was 6 mm. Zernike coefficients of vertical and horizontal coma, vertical and oblique trefoil, and spherical aberration, root mean square values of HOA (RMS. HOA) were automatically calculated by device’s software system.
Fundus images were collected by Daytona P200T (Optos, UK). Fundus tessellation was graded into four categories with the assistance of Early Treatment Diabetic Retinopathy Study (ETDRS) grid referring to previous study: grade 0 = without tessellation or no involvement of the outer circle, grade 1 = involvement of the outer circle, grade 2 = involvement of the middle circle, and grade 3 = involvement of the inner circle [16]. Two trained graders (DJ and ZY) completed grading independently in a masked manner. Final determination was made by the senior graders (ZY) if there was any disagreement with the grade.
Statistical analysis
SPSS (version 26; SPSS Inc., Chicago, IL, USA) was used for statistical analysis. A descriptive statistic was used to calculate the mean and standard deviations. The normality of all data samples was checked using the Kolmogorov-Smirnov test. Propensity score matching analysis was used to control age at surgery, gender, and preoperative SE between two surgical groups. The propensity score was estimated using logistical regression model without replacement. The matching algorithm was the nearest neighbor with a match ratio of 1:1 and a caliper value of 0.02. When comparing, Independent-samples t test and One-way analysis of variance (ANOVA) were used for normally distributed thicknesses, and Mann-Whitney U test for non-normally distributed QoV scores. Paired t-test was used to detect the asymmetry of cornea. Linear regression analysis was used to identify the contributing factors. The selection of Pearson or Spearman correlation analysis was also based on the normality of data, aiming to evaluate the correlations between thicknesses, visual quality, and myopic regression. A P value of less than 0.05 was considered significant.
Results
A total of 522 patients (522 eyes) completed postoperative OCT examination, comprising 339 patients (339 eyes) undergoing FS-LASIK and 183 patients (183 eyes) undergoing SMILE 5 years prior. After propensity score matching, 177 patients (177 eyes) in FS-LASIK group and 177 patients (177 eyes) in SMILE group were included in statistical analysis ultimately, and the baseline demographic and clinical characteristics were comparable between surgical groups (Table 1).
Corneal and retinal thickness profiles
The mean values of epithelial, stromal, and total corneal thicknesses at 5 years after surgery were shown in Fig. 1. In both groups epithelial thicknesses of the temporal and inferior sections were significantly thicker than nasal and superior sections (all P < 0.001), which was contrary to the stromal and total corneal thicknesses (all P < 0.001).
Epithelial, stromal, and total corneal thicknesses at 5 years after surgery. A, B = epithelial thickness; C, D = stromal thickness; E, F = total corneal thickness; FS-LASIK = femtosecond laser-assisted in situ keratomileusis; SMILE = small incision lenticule extraction; S = superior; I = inferior; T = temporal; N = nasal; *P < 0.05
The average macular thicknesses of two groups were shown in Fig. 2. 119 patients of FS-LASIK group and 175 patients of SMILE group completed ganglion cell complex and retinal nerve fiber layer thickness measurements. The ganglion cell complex and retinal nerve fiber layer thickness profiles were also shown in Fig. 2.
Macular, ganglion cell complex, and retinal nerve fiber layer thicknesses at 5 years after surgery. A, B = macular thickness, C, D = ganglion cell complex thickness; E, F = retinal nerve fiber layer thickness; FS-LASIK = femtosecond laser-assisted in situ keratomileusis; SMILE = small incision lenticule extraction; S = superior; I = inferior; T = temporal; N = nasal
Comparison of corneal and retinal thicknesses
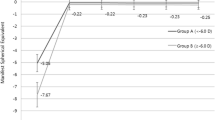
Except supratemporal and superior sections of paracentral zone, all other sections demonstrated significant variations of epithelial thickness (P of central zone, temporal, supratemporal, superior, supranasal and nasal sections of paracentral zone were 0.013, 0.013, 0.064, 0.128, 0.032, 0.003, other P < 0.001, Fig. 1). In FS-LASIK group epithelial thickness was thicker in the central and paracentral zones (P = 0.013, 0.001) and thinner in pericentral zone (P < 0.001) than that in SMILE group. And △ET-2 was statistically different between groups (P < 0.001, Table 2; Fig. 3). There was no statistical difference of stromal and total corneal thicknesses in all sections (all P > 0.05, Fig. 1), same as the mean stromal and total corneal thicknesses of 3 annuluses, △ST-1, △ST-2, △CT-1 and △CT-2 (all P > 0.05, Table 2; Fig. 3).
Comparison of epithelial, stromal, and total corneal thicknesses in two directions between surgical groups. A, B = epithelial thickness; C, D = stromal thickness; E, F = total corneal thickness; FS-LASIK = femtosecond laser-assisted in situ keratomileusis; SMILE = small incision lenticule extraction; Peri = pericentral; Para = paracentral; Cen = central; S = superior; I = inferior; T = temporal; N = nasal; *P < 0.05
There was no significant difference in macular thickness between surgical groups, so as the ganglion cell complex and retinal nerve fiber layer thicknesses (all P > 0,05). 63 fundus images were reviewed and graded. 19.05%, 15.87%, 30.16% and 34.92% of the eyes were classified into tessellation grade 0, 1, 2, and 3, respectively. No statistical difference in macular thickness, ganglion cell complex thickness and retinal nerve fiber layer thickness among fundus tessellation grades was observed (all P > 0.05).
Correlations between thicknesses and myopic regression
The median and interquartile range of postoperative UDVA and postoperative SE were − 0.10 (-0.10, 0.00) logMAR and 0.000D (0.000, 0.000) D in FS-LASIK group, -0.10 (-0.10, 0.00) logMAR and 0.000D (-0.468, 0.000) D in SMILE group. epithelial thickness in the central zone of FS-LASIK group and △ET-1 and △ET-2 of two groups were negatively correlated with SE postoperative (P = 0.023, 0.001, < 0.001, 0.008 and 0.036). In addition, epithelial thickness in the central zone was negatively correlated with SE postoperative in patients with high myopia after both surgeries (P = 0.021 and 0.029), but not in those with low-moderate myopia (P = 0.570 and 0.113, Table 3). Only a weak positive correlation between macular thickness in fovea and SE postoperative was found in SMILE group (P = 0.014, Additional file 1).
Myopic regression occurred in 15.25% of patients in FS-LASIK group and 12.99% in SMILE group. Epithelial thickness in central zone and △ET-1 of FS-LASIK group and △ET-2 of two groups were correlated with myopic regression (P = 0.035, 0.001, < 0.001and 0.016). In patients with high myopia, such correlations between △ET-1, △ET-2 and myopic regression were only found after FS-LASIK (P = 0.005 and 0.003, Table 3). There was no strong correlation between retinal thicknesses with myopic regression in neither group (P > 0.05, Additional file 1).
Correlation between epithelial thickness and visual quality
In FS-LASIK group, △ET-2 was positively correlated with RMS. HOA and spherical aberration (both P < 0.001), and negatively correlated with vertical trefoil (P = 0.025). But these correlations were not statistically significant in low-moderate myopia subgroup (all P > 0.05). In SMILE group, epithelial thickness in central zone and △ET-2 were positively correlated with RMS. HOA (P = 0.009 and 0.023) and spherical aberration (P = 0.023 and 0.014) in patients with low-moderate myopia. And in patients with high myopia these two parameters were positively correlated with vertical coma (P = 0.016 and 0.001, Table 4).
151 patients of FS-LASIK group and 142 patients of SMILE group completed the questionnaire. Main visual symptoms were fluctuation in vision (67.55%), glare (65.56%) and starbursts (58.28%) after FS-LASIK, and were glare (73.24%), fluctuation in vision (64.08%) and blurred vision (60.56%) after SMILE, though no significant variation in the scoring of individual symptom or the summary was found between two surgical methods even among patients with low-moderate or high myopia (all P > 0.05). Starbursts demonstrated correlations with pericentral epithelial thickness in FS-LASIK group (P = 0.011) and SMILE group (P = 0.036), but there was no relevance between total QoV scores, overall satisfaction and epithelial thickness (mean epithelial thickness of annuluses, △ET-1 and △ET-2) in two surgical groups or any diopter subgroups (all P > 0.05, Table 5).
Contributing factors of corneal and retinal thicknesses
Multiple linear regression analysis revealed that epithelial thickness would be thicker in central and paracentral zones with higher degree of myopia, so as △ET-1 and △ET-2 (all P < 0.05). Mean epithelial thickness of annuluses would be thicker in males (P < 0.05). Age at surgery and corneal curvature only influenced on a few parameters in two surgical groups (P < 0.05) (Additional file 2).
Stromal thickness would be thinner with higher degree of myopia (P < 0.05). △ST-2 would be larger in males after two surgical methods (both P < 0.05). All parameters of FS-LASIK group were affected by corneal curvature (P < 0.05). And all parameters in both groups were not associated with age at surgery (all P > 0.05) (Additional file 3).
In all enrolled patients, macular thickness in perifovea (P < 0.001), ganglion cell complex (P = 0.008, 0.010), and superior (P = 0.004), nasal, inferior retinal nerve fiber layer (both P < 0.001) were linearly positively correlated with SE preoperative.
Discussion
Using SD-OCT, our cross-sectional study revealed the distribution of epithelium at 5 years postoperatively. This is the longest visit from surgery as we know describing the differences of distribution patterns, and our result supported and complemented to the previous observation within 3 months postoperative [9]. Epithelial thickness increases greater after FS-LASIK than SMILE in the central 5-mm diameter zone, and less in 5–6 mm diameter zone. Reasons might account for this. These surgical methods have different effects on the stroma, and epithelial remodeling as the compensation is also affected. In FS-LASIK, the actual ablation at the paracentral zone might be deeper for compensation of the laser-induced spherical aberration, and the greatest epithelial thickening was observed in 3–4 mm diameter zones, [17] which was included in the paracentral zone of our study. Differently, optical zone transits smoothly from the center to the periphery in SMILE. Centrifugal increase after SMILE was presumed to be related to biomechanical change and central stroma remodeling [9]. Moreover, distinct distribution patterns of epithelial thickness between these two surgeries became evidence at 1 month postoperatively [9]. Then the remodeling was reported to continue for 1 to 3 months and tend to be stable up to 2 years after surgery [6, 7, 10]. Throughout this period, the discrepancy of thickening between surgeries in paracentral and periphery regions exists persistently despite not always reaching statistical significance [7, 9, 18, 19]. Therefore, we speculated that different distribution patterns of epithelium mainly develop in short term following surgery and persists up to 5 years. But further investigation is required to determine whether the noticeable variation of thickness results from the calculation of subtle thickening, since this study only included one visit at 5 years after surgery.
To verify the different distribution patterns of epithelial thickness and their impacts after two surgical methods, we analyzed that △ET-1 and △ET-2 were larger in FS-LASIK group, and the difference of △ET-2 was statistically significant. Central epithelium thickening greater than periphery can be regarded as a convex lens adding on the corneal surface, [20] and increasing epithelial thickness might induce myopization of its refractive power [19]. △ET-1 and △ET-2 of two groups were negatively correlated with SE postoperative in our study, which was similar to the results after LASIK and SMILE [10, 11]. △ET-1 of FS-LASIK group and △ET-2 of two groups were also correlated with myopic regression. However, when patients were grouped based on preoperative SE, significant correlations between these two parameters and myopic regression were found only in high myopia subgroup of FS-LASIK group. Hence, in order to ensure the long-term stability of refractive status, attention should be paid to the uneven distribution of epithelial thickness from the center to the periphery, especially in patients with high myopia and receiving FS-LASIK.
On the other hand, we investigated the correlations between epithelial thickness and objective and subjective visual quality. Previous studies have suggested that the inhomogeneity of epithelial thickness could elevate the HOAs of the anterior corneal surface, which could not be compensated by the posterior surface after surgery [21]. And variability of epithelial thickness has been proposed as an objective assessment for dry eye currently, with the latter being regarded as another important contributor to the increase of HOAs [22,23,24]. This study is the first to reveal different correlations between low-moderate and high myopia subgroups at 5 years after surgery. After FS-LASIK, corneal HOAs would be greater with higher degree of myopia, which could be explained by the increased risk of flap deflection and more laser-induced spherical aberration [25], and the compensatory response of epithelium would be greater simultaneously. Correspondingly, statistical correlations appeared only in high myopia subgroup but not in low-moderate subgroup in our study. In SMILE group, epithelial thickness was also associated with coma in patients with high myopia, for whom imbalanced healing caused by ablation decentration might be more obvious due to the lack of eye-tracking system [25]. When considering subjective visual quality, relevance was found solely in pericentral epithelial thickness and starburst which indicates the irregularity of cornea, rather than total QoV scores and overall satisfaction. And the main visual symptoms including fluctuation in vision, glare and starbursts after FS-LASIK, and glare, fluctuation in vision and blurred vision after SMILE, seemed to match to the aforementioned correlations with HOAs. Therefore, we emphasized the importance of monitoring of epithelial thickness and the use of drugs such as steroid and anti-glaucoma especially in the short term postoperative [20, 26, 27].
The remodeling induced by surgery did not alter the vertical distribution characteristic of epithelium at 5 years postoperatively [28]. The asymmetry might be related to the gravity-dependent flow of tear film and mechanical force exerted by eyelid when blinking [29]. Especially after FS-LASIK, the reducing of corneal sensitivity and lower blink rate increase the influence of incomplete blinks and result in epitheliopathy [30]. Although this change mostly occurred within 6 months after surgery, punctate stains were found in inferior area among a small number of patients complaining of dry eye in our study. The horizontal asymmetry was opposite to that in primary eyes, but consistent with other studies after surgery [6, 10]. Large curvature gradient change caused by astigmatism correction might be the reason.
Various studies have shown that epithelial remodeling is related to the attempted myopic correction [6, 8, 10, 17]. Moreover, △ET-1 and △ET-2 increased with higher degree of myopia in this long-term research. Regression analysis suggested the stability of epithelial thickness for young patients at 5 years after surgery. However, Luft et al. found that age diminished the effect of surgical refractive correction on epithelial remodeling [8]. The long-term consequence of this interaction require further studies with a wider range of age. In both groups male patients had thicker epithelial thickness. According to the previous research, gender would not increase the prediction of epithelium thickening [8], difference between gender was consistent with primary eyes, [28] and might result from the influence of gonadal hormones on ocular development [31]. Ks and Kf impacted on the mean epithelial thickness in pericentral zone in FS-LASIK group, and they were also negatively associated with △ET-1 and △ET-2 in SMILE group. It was reported that postoperative curvatures would change greater in patients with flatter corneas, which was ascribed to the less eyelid pressure [32].
In terms of stromal thickness, Luft et al. observed the increase of central stroma until the end of their 1-year observation [14]. Our study showed the long-term results without interference of measurement, including wound healing mediated by keratocyte in interface and short-term postoperative corneal edema. There were vertical and horizontal asymmetries of stromal thickness in both surgical groups. Surgeries preserved the distribution characteristics of primary eyes [33]. In current studies, when higher refractive error was corrected, the discrepancy between the planned and achieved lenticule thickness, or stromal reduction would be larger [12, 14]. Despite this mismatch, our study confirmed that residual stromal thickness was still linearly correlated to SE preoperative after these two surgical methods.
In this study there was no statistical difference of stromal thickness between groups. SMILE is considered to conduct more stromal ablation clinically. However, underestimation and overestimation of actual central stromal reduction after FS-LASIK and SMILE were reported in the follow-up of 6 months respectively [13]. For FS-LASIK, laser ablation increasing progressively with depth would cause over ablation. In SMILE, the anterior-most stomal lamellae with high cohesive tensile strength can be preserved better and the posterior stroma thickening might be the major contributor to the discrepancy [34,35,36]. Clinically, FS-LASIK is commonly recommended for patients with thin cornea or high myopia. We cannot completely attribute the result to over ablation and stromal remodeling. But the preoperative central corneal thickness was comparable between groups, so our 5-year stromal thickness results were still valuable for reference. Alio et al. demonstrated that as the level of ametropias was greater, the misestimation would be higher, and actual stromal thickness changes became equivalent, which proved the reliability of our study [12].
Macular thickness, ganglion cell complex and retinal nerve fiber layer thicknesses at 5 years postoperatively were not significantly different between two surgical groups, which was consistent with studies conducted in the short period after surgery [37, 38]. No maculopathy was found in all patients participating. Macular thickness in perifovea, ganglion cell complex thickness, and superior, nasal, inferior retinal nerve fiber layer thickness were positively correlated with SE preoperative, matching the retinal alterations in myopia [39,40,41]. On the basis of these linear relations, a greater myopic shift of refractive power was anticipated in association with thinner retinal thicknesses. However, only macular thickness in fovea of SMILE group was detected to have a weak correlation with SE postoperative in our study. Retinal thicknesses might not possess sufficient sensitivity to reflect the potential of myopic regression. The initial reduction in thicknesses primarily happened in the outer layer and petiphery region of the fovea, [42] which might be attributed to this observation. Besides, our results displayed no difference in macular thickness, ganglion cell complex thickness and retinal nerve fiber layer thickness among fundus tessellation grades. The previously constructed model of fundus tessellation progression excluded retinal nerve fiber layer from the independent variables, [43, 44] and the published literature of our research group had demonstrated that increased tessellation grades were associated with reduced contrast sensitivity 5 years after surgery, [45] which indicated that the change in retinal function might occur earlier than structure. It should be noted that postoperative aberration and changes of refractive properties will affect the measurement of retinal nerve fiber layer, [46] and tilted optic disc might cause the displacement of OCT scan circle and overestimation of temporal retinal nerve fiber layer [47]. Hence, further studies of retinal structure are needed to explore more feasible follow-up indicators for early warning of myopic regression and pathologic myopia.
There are limitations to our study. OCT was not a routine preoperative examination 5 years before in our hospital, so the baseline data of all patients were hard to be collected. Though the inherent defects of cross-sectional study could not be avoided, we focused on the characteristics of corneal and retinal thicknesses at 5 years after two surgeries. Considering the relatively large number of patients included in this study, we did not specify the size of the optical zone and the thickness of the corneal flap or cap. Studies in early period postoperative have shown that epithelium thickens greater with smaller the optical zone, [10, 26] and long-term study is still lacking. And the thickness of corneal flap or cap might be associated with the anterior surface curvature and biomechanics [48,49,50]. But the different distribution patterns of epithelial thickness in our study were similar to the observational research within 3 months postoperative, in which flap and cap thicknesses were set to 120 μm. The improved SD-OCT covering a 9-mm diameter range had already been applied in clinical research [6, 10]. However, the clinical significance of longer follow-up period beyond the 6-mm diameter range needs to be investigated further.
Conclusion
In summary, the tendency that epithelial thickness in central zone was thicker than peripheral zone was more obvious at 5 years after FS-LASIK compared to SMILE. This uneven distribution of epithelial thickness might play a role in myopic regression and the changes in HOAs, especially in patients with high myopia, but it had little effect on patients’ subjective visual quality. Moreover, stromal thickness was affected by over ablation and stromal remodeling respectively. And there were asymmetries of epithelial, stromal, and total corneal thicknesses after two surgeries. Attention should be paid to the corneal remodeling to ensure the accuracy and stability of surgery. Retinal thicknesses were not affected by these two surgeries, and they did not appear to be the clinical indicators for myopic regression or fundus tessellation progression.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- FS-LASIK:
-
Femtosecond laser-assisted in situ keratomileusis
- SMILE:
-
Small incision lenticule extraction
- OCT:
-
Optical coherence tomography
- △ET-1:
-
Difference of epithelial thickness between central and paracentral zones
- △ET-2:
-
Difference of epithelial thickness between central and pericentral zones
- △ST-1:
-
Difference of stromal thickness between central and paracentral zones
- △ST-2:
-
Difference of stromal thickness between central and pericentral zones
- △CT-1:
-
Difference of corneal thickness between central and paracentral zones
- △CT-2:
-
Difference of corneal thickness between central and pericentral zones
- SE:
-
Spherical equivalent
- UDVA:
-
Uncorrected distance visual acuity
- CDVA:
-
Corrected distance visual acuity
- HOAs:
-
Higher-order aberrations
- RMS.HOA:
-
Root mean square values of higher-order aberration
- QoV questionnaire:
-
Quality of Vision questionnaire
- Kf:
-
flattest keratometry
- Ks:
-
steepest keratometry
- CCT:
-
Central corneal thickness
References
Han T, Xu Y, Han X, Zeng L, Shang J, Chen X, Zhou X. Three-year outcomes of small incision lenticule extraction (SMILE) and femtosecond laser-assisted laser in situ keratomileusis (FS-LASIK) for myopia and myopic astigmatism. Br J Ophthalmol. 2019;103(4):565–8.
Wen D, McAlinden C, Flitcroft I, Tu R, Wang Q, Alió J, Marshall J, Huang Y, Song B, Hu L, et al. Postoperative efficacy, predictability, Safety, and visual quality of laser corneal refractive surgery: a Network Meta-analysis. Am J Ophthalmol. 2017;178:65–78.
Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95(3):335–9.
Blum M, Lauer AS, Kunert KS, Sekundo W. 10-Year results of small incision Lenticule extraction. J Refract Surg. 2019;35(10):618–23.
Reinstein DZ, Archer TJ, Gobbe M. Rate of change of curvature of the corneal stromal surface drives epithelial compensatory changes and remodeling. J Refract Surg. 2014;30(12):799–802.
Fan L, Xiong L, Zhang B, Wang Z. Longitudinal and Regional non-uniform remodeling of corneal epithelium after topography-guided FS-LASIK. J Refract Surg. 2019;35(2):88–95.
Kanellopoulos AJ. Comparison of corneal epithelial remodeling over 2 years in LASIK Versus SMILE: a Contralateral Eye Study. Cornea. 2019;38(3):290–6.
Luft N, Ring MH, Dirisamer M, Mursch-Edlmayr AS, Kreutzer TC, Pretzl J, Bolz M, Priglinger SG. Corneal epithelial Remodeling Induced by Small Incision Lenticule extraction (SMILE). Invest Ophthalmol Vis Sci. 2016;57(9):Oct176–83.
Ryu IH, Kim BJ, Lee JH, Kim SW. Comparison of corneal epithelial remodeling after Femtosecond Laser-assisted LASIK and small incision Lenticule extraction (SMILE). J Refract Surg. 2017;33(4):250–6.
Ye Y, Chen P, Yu N, Wan L, Lan M, Zheng H, Yu K. Evaluation of wide corneal epithelial remodeling after small incision Lenticule extraction (SMILE) with wide-field Optical Coherence Tomography. J Ophthalmol. 2022;2022:8764103.
Cho Y, Hieda O, Wakimasu K, Yamamura K, Yamasaki T, Nakamura Y, Sotozono C, Kinoshita S. Multiple Linear regression analysis of the impact of corneal epithelial thickness on refractive error Post corneal refractive surgery. Am J Ophthalmol. 2019;207:326–32.
Del Alió JL, Canto-Cerdan M, El Bahrawy M, Casanova L, García MJ, Cavas F, Alió JL. Corneal stromal thickness changes after myopic laser corneal refractive surgery. J Cataract Refract Surg. 2022;48(3):334–41.
Luo Y, He S, Chen P, Yao H, He A, Li Y, Qiu J, Lan M, Zhuang J, Yu K. Predictability of Central corneal stromal reduction after SMILE and FS-LASIK for high myopia correction: a prospective Randomized Contralateral Eye Study. J Refract Surg. 2022;38(2):90–7.
Luft N, Priglinger SG, Ring MH, Mayer WJ, Mursch-Edlmayr AS, Kreutzer TC, Bolz M, Dirisamer M. Stromal remodeling and lenticule thickness accuracy in small-incision lenticule extraction: one-year results. J Cataract Refract Surg. 2017;43(6):812–8.
McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–45.
Cheng T, Deng J, Xu X, Zhang B, Wang J, Xiong S, Du Y, Yu S, Gong W, Zhao H, et al. Prevalence of fundus tessellation and its associated factors in Chinese children and adolescents with high myopia. Acta Ophthalmol. 2021;99(8):e1524–33.
Tang M, Li Y, Huang D. Corneal epithelial remodeling after LASIK measured by Fourier-Domain Optical Coherence Tomography. J Ophthalmol. 2015;2015:860313.
Zhu M, Xin Y, Vinciguerra R, Wang Z, Warsame AM, Wang C, Zhu D, Qu Z, Wang P, Zheng X, et al. Corneal epithelial remodeling in a 6-Month follow-up period in myopic corneal refractive surgeries. J Refract surg. 2023;39(3):187–96.
Canto-Cerdan M, El Bahrawy M, Alió JL, Casanova L, García MJ, Al-Amri SA, J, Cavas F. Alió Del Barrio J L. Corneal epithelium thickness and refractive changes after myopic laser corneal refractive surgery. J Refract Surg. 2022;38(9):602–8.
Li H, Han Q, Zhang J, Shao T, Wang H, Long K. Role of corneal epithelial thickness during myopic regression in femtosecond laser-assisted in situ keratomileusis and transepithelial photorefractive keratectomy. BMC Ophthalmol. 2022;22(1):481.
Liu M, Jin C, Lu L, Yuan Y, Chen C, Zhao T, Ke B. The impact of corneal epithelial thickening and inhomogeneity on corneal aberrations after Small Incision Lenticule extraction. J Refract Surg. 2023;39(1):23–32.
Wang Y, Zhang X, Qian Y, Luo B, Li C, Yang X. Comparison of corneal epithelial remodeling after small incision lenticule extraction and femtosecond laser-assisted LASIK. Zhonghua Yan Ke Za Zhi. 2020(02): 93–102.
Kanellopoulos AJ. Incidence and management of symptomatic dry eye related to LASIK for myopia, with topical cyclosporine A. Clin Ophthalmol. 2019;13(null):545–52.
Kanellopoulos AJ, Asimellis G. In vivo 3-dimensional corneal epithelial thickness mapping as an indicator of dry eye: preliminary clinical assessment. Am j Ophthalmol. 2014;157(1):63–e682.
Zhou X, Qin B, Han T, Shang J, Chen Z, Zhao J, Yao P, Zhou X. Long-Term Observation of Higher-Order aberrations and microdistortions in Bowman’s Layer after Small Incision Lenticule extraction for the correcting myopia with Spherical Equivalent Higher Than – 9.0 diopters. Front Med (Lausanne). 2022;9:814810.
Ryu IH, Kim WK, Nam MS, Kim JK, Kim SW. Reduction of corneal epithelial thickness during medical treatment for myopic regression following FS-LASIK. BMC Ophthalmol. 2020;20(1):296.
Halkiadakis I, Vernikou A, Tzimis V, Markopoulos I, Popeskou K, Konstadinidou V. Assessment of corneal epithelium thickness in glaucomatous patients undergoing Medical Treatment. J Glaucoma. 2021;30(1):44–9.
Hashmani N, Hashmani S, Saad CM. Wide corneal epithelial mapping using an optical coherence tomography. Invest Ophthalmol Vis Sci. 2018;59(3):1652–8.
Du C, Wang J, Cui L, Shen M, Yuan Y. Vertical and horizontal corneal epithelial thickness profiles determined by Ultrahigh Resolution Optical Coherence Tomography. Cornea. 2012;31(9):1036–43.
McMonnies CW. How Blink anomalies can contribute to Post-LASIK neurotrophic epitheliopathy. Optom Vis Sci. 2015;92(9):e241–7.
Giuffrè G, Di Rosa L, Fiorino F, Bubella DM, Lodato G. Variations in central corneal thickness during the menstrual cycle in women. Cornea. 2007;26(2):144–6.
Lee S, Bae S, Jung M. Effect of preoperative keratometry on visual outcomes after small-incision lenticule extraction for myopia. Int Ophthalmol. 2022;42(6):1719–26.
Hashmani N, Hashmani M, Asghar N, Islam M, Hashmani S. Wide stromal mapping using an anterior segment Optical Coherence Tomography. Clin Ophthalmol. 2020;14:751–7.
Olsen MV, Lyngstadaas AV, Zhou W, Stojanovic A, Utheim TP, Wang X, Badian RA, Chen X. Temporal redistribution of cap and residual stromal thickness after SMILE. J Cataract Refract Surg. 2020;46(10):1331–8.
Liu S, Zhou X, Zhao Y. Comparison of predictability in Central corneal thickness reduction after SMILE and FS-LASIK for high myopia correction. Ophthalmol Ther. 2023;12(1):549–59.
Wu F, Yin H, Yang Y. Evaluation of the difference between predicted and measured central corneal thickness reduction after SMILE and Femtosecond Laser-assisted LASIK for myopia. Curr Eye Res. 2021;46(8):1089–95.
Chen M, Dai J, Gong L. Changes in Retinal vasculature and thickness after small incision Lenticule extraction with Optical Coherence Tomography Angiography. J Ophthalmol. 2019;2019:3693140.
Yu L, Wenli Y, Fengju Z. Effect of suction on the retina superficial vascular networks’s Flow density after SMILE and FS-LASIK in high myopia using Optical Coherence Tomography Angiography. Zhonghua Yan Shi Guang Xue Yu Shi Jue Ke Xue Za Zhi. 2019: 401–7.
Salehi MA, Nowroozi A, Gouravani M, Mohammadi S, Arevalo JF. Associations of refractive errors and retinal changes measured by optical coherence tomography: a systematic review and meta-analysis. Surv Ophthalmol. 2022;67(2):591–607.
Zhao Z, Zhou X, Jiang C, Sun X. Effects of myopia on different areas and layers of the macula: a Fourier-domain optical coherence tomography study of a Chinese cohort. BMC Ophthalmol. 2015;15:90.
Ucak T, Icel E, Yilmaz H, Karakurt Y, Tasli G, Ugurlu A, Bozkurt E. Alterations in optical coherence tomography angiography findings in patients with high myopia. Eye. 2020;34(6):1129–35.
Çitirik M, Yavuzer K, Bağci F. Assessment of changes in macular structural retinal layers in patients with pathological myopia. Turk j med sci. 2023;53(6):1807–16.
Yan YN, Wang YX, Yang Y, Xu L, Xu J, Wang Q, Yang X, Yang JY, Zhou WJ, Wei WB, Jonas JB. Long-term progression and risk factors of Fundus Tessellation in the Beijing Eye Study. Sci Rep. 2018;8(1):10625.
Shao L, Zhang QL, Long TF, Dong L, Zhang C, Da Zhou W, Wang YX, Wei WB. Quantitative Assessment of Fundus Tessellated Density and Associated Factors in Fundus images using Artificial Intelligence. Transl Vis Sci Technol. 2021;10(9):23.
Jiang D, Guo N, Lv X, Li Y, Han Y, Yuan M, Zhai C, Zhang W, Zhang F. Association between Fundus tessellation and contrast sensitivity in myopic eyes. Curr Eye Res. 2024;49(2):188–96.
Jiang Y, Wang Z, Li Y, Li Y, Lu TC. Retinal nerve Fibre Layer Thickness Change following Femtosecond Laser-assisted in situ Keratomileusis. Front Med (Lausanne). 2021;8:778666.
Shin HY, Park HY, Park CK. The effect of myopic optic disc tilt on measurement of spectral-domain optical coherence tomography parameters. Br J Ophthalmol. 2015;99(1):69–74.
Wu D, Liu C, Li B, Wang D, Fang X. Influence of Cap Thickness on corneal curvature and corneal biomechanics after SMILE: a prospective, Contralateral Eye Study. J Refract Surg. 2020;36(2):82–8.
Fang L, Wang Y, Yang R, Deng S, Deng J, Wan L. Effects of the LASIK flap thickness on corneal biomechanical behavior: a finite element analysis. BMC Ophthalmol. 2020;20(1):67.
Jun I, Kang DSY, Roberts CJ, Lee H, Jean SK, Kim EK, Seo KY, Kim TI. Comparison of clinical and biomechanical outcomes of small incision lenticule extraction with 120- and 140-µm Cap Thickness. Transl Vis Sci Technol. 2021;10(8):15.
Acknowledgements
The authors thank Professor Changbin Zhai and the colleagues from the Refractive Surgery Center, Beijing Tongren Eye Center of Beijing Tongren Hospital for supporting and assistance with collecting preoperative data and completing postoperative measurements.
Funding
This study was supported by Research and Transformation Application of Capital Clinical Diagnosis and Treatment Technology by Beijing Municipal Commission of Science and Technology (number Z201100005520043).
Author information
Authors and Affiliations
Contributions
FZ provided supervision and final approval, made critical revision of the manuscript and fund application, designed the research and conducted the surgeries. JL and JQ conducted the research, collected data, performed statistical analysis, and wrote the manuscript. XL and YX interpreted data and made revision of the manuscript. DJ and MY completed grading the fundus images. MS made revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in compliance with the Declaration of Helsinki and was approved by the ethics committee of Beijing Tongren Hospital affiliated to Capital Medical University. Informed consent was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, J., Qin, J., Lv, X. et al. Study of corneal and retinal thicknesses at five years after FS-LASIK and SMILE for myopia. BMC Ophthalmol 24, 396 (2024). https://doi.org/10.1186/s12886-024-03661-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03661-w