Abstract
Background
Human amniotic membrane (AM) transplantation has been applied to treat ocular surface diseases, including corneal trauma. The focus of much deliberation is to balance the mechanical strength of the amniotic membrane, its resistance to biodegradation, and its therapeutic efficacy. It is commonly observed that the crosslinked human decellularized amniotic membranes lose the functional human amniotic epithelial cells (hAECs), which play a key role in curing the injured tissues.
Methods and results
In this study, we crosslinked human decellularized amniotic membranes (dAM) with genipin and re-planted the hAECs onto the genipin crosslinked AM. The properties of the AM were evaluated based on optical clarity, biodegradation, cytotoxicity, and ultrastructure. The crosslinked AM maintained its transparency. The color of crosslinked AM deepened with increasing concentrations of genipin. And the extracts from low concentrations of genipin crosslinked AM had no toxic effect on human corneal epithelial cells (HCECs), while high concentrations of genipin exhibited cytotoxicity. The microscopic observation and H&E staining revealed that 2 mg/mL genipin-crosslinked dAM (2 mg/mL cl-dAM) was more favorable for the attachment, migration, and proliferation of hAECs. Moreover, the results of the CCK-8 assay and the transwell assay further indicated that the living hAECs’ tissue-engineered amniotic membranes could facilitate the proliferation and migration of human corneal stromal cells (HCSCs) in vitro.
Conclusions
In conclusion, the cl-dAM with living hAECs demonstrates superior biostability and holds significant promise as a material for ocular surface tissue repair in clinical applications.
Similar content being viewed by others
Introduction
The ocular surface system, mainly including the conjunctiva and cornea, is functional to guarantee the stability of the refractive surface of the eye. Any component dysfunction or impairment can lead to whole-system secondary dysfunction and severe ocular surface disease [1, 2]. Conditions such as chemical and thermal burns, ocular cicatricial pemphigoid, Stevens-Johnson syndrome, and other similar diseases pose significant treatment challenges for ophthalmologists globally. The concept of ocular surface reconstruction with biomaterial for tissue engineering has been generally accepted by ophthalmologists [3].
The amniotic membrane, the innermost layer of the placenta, has a translucent appearance and is consists of a monolayer of amniotic epithelial cells, a thick basement membrane, and an avascular stroma [4, 5]. Over the past two decades, the amniotic membrane has become a common graft for ocular surface reconstruction due to its ability to reduce inflammation and scarring, as well as promote epithelialization. Furthermore, the amniotic membrane is widely available and easily obtainable [6,7,8]. However, some underlying shortcomings of currently available amniotic membrane products include the tendency to curl and tear, difficulties in intraoperative handling and suturing, and rapid degradation that may necessitate re-transplantation [9,10,11]. Treating amniotic membranes with crosslinking agents can enhance the mechanical strength and biological stability of the grafts. Genipin, an agent extracted from Gardenia jasminoides fruit, is a newly discovered crosslinker [12]. Compared to crosslinking agents such as formaldehyde and glutaraldehyde, genipin offers higher biocompatibility, lower cytotoxicity to cells, and improved mechanical strength and degradation properties for biological materials [13, 14]. Previous research has shown that the genipin-crosslinked AM has excellent biostability and biocompatibility, making it suitable for various tissue engineering applications [15]. However, the crosslinking process leads to a loss of function in human amniotic epithelial cells (hAECs).
HAECs originate from the epiblast and possess the proliferative and differentiation properties of embryonic stem cells. The capacity of amniotic epithelial cells to modulate or even suppress both innate and acquired immunity makes them a practical resource for inducing tolerance in both autoimmune and transplantation models [16]. Intravenous administration of hAECs did not cause a hemolytic reaction, toxicity, allergic reactions, or tumorigenicity, indicating their systemic safety [17]. Recently, hAECs have been widely used in regenerative medicine, including treatment for lung injury [18], liver injury [19], skin wound healing [20], and ocular surface restoration [21], due to their anti-inflammatory, anti-fibrotic, tissue regeneration, and immunomodulatory properties. In our previous study, hAEC not only facilitate re-epithelialization of the cornea after alkali burns but also reduce scar formation and promote the restoration of corneal tissue transparency [22]. The amniotic membrane graft that was employed in ocular surface treatment lack functional hAECs, which to some extent limits the therapeutic effect of the amniotic membrane.
In this study, we aimed to crosslink human decellularized amniotic membranes (dAM) with genipin to enhance their mechanical strength, optical clarity, anti-degradation properties, and reduce cytotoxicity. Then hAECs were seeded onto genipin crosslinked dAM to construct a functional living-hAEC tissue-engineered amniotic membrane, potentially offering a more effective treatment for ocular surface diseases.
Materials and methods
Human ethics
After written informed consent was obtained from every placental donor, amniotic membranes were collected from term healthy placentas of women according to the guidelines and approval of the the Human Research Ethics Committee of the School of Medicine at Tongji University (Approval No. 2021tjdx053). A total of five placental donors participated in this study.
Decellularization of human amniotic membrane
The amniotic membrane on the surface of the placenta was stripped aseptically and washed with phosphate-buffered saline (PBS, B548117, Sangon Biotech, China) containing 10% penicillin and streptomycin (10378016, Thermo Fisher Scientific, USA) at least 3 times to remove blood stains and impurities. The amniotic membrane was then cut into pieces approximately 5 cm × 5 cm in size and incubated with 0.25% Trypsin-EDTA (25200072, Thermo Fisher Scientific, USA) at 37 °C for 15 min. Then the hAECs were gently scraped from the surface of the amnion with a cell scraper without destroying the structure of the underlying amniotic tissue. The decellularized amniotic membrane (dAM) was then rinsed several times with PBS to remove residual chemicals. To ensure complete decellularization of dAM, we stained the AM samples with DAPI for residual cell nucleus inspection. The dAM was then stored in DMEM medium (D6046, Sigma, Germany) mixed with glycerol (A100854, Sangon Biotech, China) at a ratio of 1:1 (vol/vol) and stored at -80 °C.
Cell culture
To isolate and culture hAECs, the previous steps are the same as for dAM preparation. The dissociated hAECs were collected by centrifugation at 1500 rpm for 10 min and cultured in DMEM/F12 medium (11330032, Thermo Fisher Scientific, USA) containing 10% fetal bovine serum (FBS, FSP500, ExCell Bio, China), 10 ng/ml human recombinant epidermal growth factor (EGF, PHG0311, Thermo Fisher Scientific, USA), 5 µM SB431542 (301836-41-9, Selleck, China), and 1% penicillin and streptomycin at 37 °C with 5% CO2. The culture medium was changed every two days.
Human corneal epithelial cell (HCEC) and Human corneal stromal cell (HCSC) (kind gifts from professor Qingjun Zhou (Shandong Eye Institute, China)) were cultured in DMEM/F12 medium (11330032, Thermo Fisher Scientific, USA) containing 10% FBS in an incubator at 37 °C with 5% CO2.
Immunofluorescence assay
The expression of proteins in hAECs was detected by immunofluorescence. The cultured hAECs were seeded on a 24-well plate and cultured for 24 h. The cells were fixed with 4% paraformaldehyde (PFA; E672002-0500, Sangon Biotech, China) for 5 min, then permeabilized with 0.3% TritonX-100 (A600198, Sangon Biotech, China) /PBS for 5 min, and blocked with 3% bovine serum albumin (BSA, A600332, Sangon Biotech, China) /PBS for 1 h at room temperature (RT). The cells were stained with primary antibodies (mouse anti-Cytokeratin19, mouse anti-E-cadherin, and mouse anti-SSEA4) at 4 °C overnight and then incubated with Alexa-Fluor 488 conjugated anti-mouse or Alexa-Fluor 555 conjugated anti-mouse secondary antibodies for 1 h at RT. The cell nuclei were stained with DAPI. The images were captured by a fluorescence microscope (IX73, Olympus, Japan). Cells not stained with the primary antibody were considered negative controls.
Genipin crosslinked amniotic membrane
Decellularized amniotic membrane (dAM) was crosslinked with 2 mg/mL, 4 mg/mL, or 8 mg/mL genipin (6902-77-8, LinChuan ZhiXin Biotechnology, China) in PBS solution. In brief, dAM was immersed in different genipin solutions (2 mg/mL, 4 mg/mL, or 8 mg/mL) for 24 h at 37 °C. After 24 h, the genipin-crosslinked dAM was rinsed with PBS and stored in DMEM medium mixed with glycerol at a ratio of 1:1 (vol/vol) at -80 °C. Before use, all crosslinked materials should be thoroughly rinsed with PBS to eliminate any residual crosslinking agent.
Five different groups were involved in this study: native amniotic membrane (nAM), decellularized amniotic membrane (dAM), 2 mg/mL genipin-crosslinked decellularized amniotic membrane (2 mg/mL cl-dAM), 4 mg/mL genipin-crosslinked decellularized amniotic membrane (4 mg/mL cl-dAM), and 8 mg/mL genipin-crosslinked decellularized amniotic membrane (8 mg/mL cl-dAM). The 2 mg/mL cl-dAM, 4 mg/mL cl-dAM, and 8 mg/mL cl-dAM were respectively referred to as the genipin low, genipin medium, and genipin high groups.
Measurement of optical clarity
The amniotic membrane of each group was laid flat on a cell culture dish, and then the dish was placed on a piece of paper with a square pattern to observe the clarity of the amniotic membrane of each group separately. The general appearance of the AM was captured with a digital camera (Olympus, Japan).
In vitro biodegradation experiment
The biostability of amniotic membrane before and after crosslinking with genipin was examined using an in vitro enzymatic degradation assay [23]. Collagenase type I (17018029, Thermo Fisher Scientific, USA) was applied to examine the anti-biodegradation abilities of the amniotic membrane in all groups. All the amniotic membranes (n = 3) were cut into 1 cm × 1 cm pieces and then incubated with 2 mL of 0.1 mg/mL of collagenase I at 37 °C. The degradations of the AM were observed at 0, 24, and 120 h with a microscope (SZX10, Olympus, Japan).
Surface morphology and ultrastructure analysis
The surface morphology and ultrastructure of nAM, dAM, and cl-dAM were characterized with a S-3400 N scanning electron microscope (SEM) (HITACHI, Japan). The samples of each group were initially fixed with 2.5% glutaraldehyde solution overnight at 4 °C and then washed three times with ddH2O and frozen overnight at -20 °C. The samples were dried in a freeze dryer (ALPHA 1–2 LD plus, Christ, Germany) for 3 h and then sputter-coated with gold, followed by SEM observation.
Cytotoxicity assessment of genipin crosslinked amniotic membranes
The CCK-8 assay was performed to assess the cytotoxicity of the extracts of genipin-crosslinked amniotic membranes on cells. Cut each group of amniotic membrane into 3 cm × 3 cm pieces and place them flat in 6-cm cell culture dishes. Add 3 mL of culture medium DMEM/F-12 containing 1% penicillin and streptomycin to each group and extract them for 48 h at 37 °C as the extraction solution.
The cultured cells were seeded on a 96-well plate at a density of 5 × 103 cells per well and cultured for 24 h. The culture medium was replaced by DMEM/F-12 medium containing 1% FBS only as a control, and the same medium contained amniotic membrane extracts from each group. After cells were incubated with or without amniotic membrane extracts for 24 h and 72 h, the medium was aspirated, and then freshly prepared CCK-8 (TargetMol, USA) culture medium was added to each well according to the manufacturer’s instructions. Cell viability was measured as the absorbance at 450 nm with a microplate reader (iMark™ Microplate Absorbance Reader, BioRad, USA) as in our previous report [24].
Re-plant hAECs on the genipin-crosslinked amniotic membrane
The dAM (control group) or 2 mg/mL cl-dAM was trimmed into a 25 mm diameter circle and then placed into 24-well culture plates. hAECs at passage 2 were seeded at a density of 5 × 105 cells (200 µL cell suspension) per well onto the dAM or 2 mg/mL cl-dAM and cultured in hAECs medium in an incubator at 37 °C with 5% CO2.
After 12 h of incubation, 500 µL of hAECs medium was added, and the incubation was continued for another 24 h before changing the culture medium. Then the cultural medium changed every day. The attachment, proliferation, and migration of hAECs on the amniotic membrane were monitored by microscopy (CKX41, Olympus, Japan).
Hematoxylin and eosin (H&E) staining
After 4 days of culture, cl-dAM with living-hAECs was collected for H&E staining. Amniotic membrane samples were fixed with 4% paraformaldehyde (PFA, E672002-0500, Sangen Biotech, China) for 24 h and then embedded in paraffin and cut into 3-µm-thick sections. As previously described, hematoxylin and eosin (H&E) staining was used to analyze the morphology of the amniotic membrane [25].
Transwell migration assay
Polycarbonate transwell inserts of 8 μm pore diameter (3422, Corning Incorporated, USA) were used to determine the vertical migration of HCSCs. In a 24-well culture plate, 500 µL of DMEM/F-12 medium without FBS was added to the lower chamber. Then the cl-dAM or the hAECs-cl-dAM was placed into the 24-well culture plate. Cultured HCSCs were resuspended in serum-free cell culture media, and 200 µL of cell solution (5 × 104 cells) was seeded into the upper transwell insert membrane. Cells were incubated for 24 h and stained with 0.5% crystal violet (Yeasen, China). Images of migrating cells in the lower compartment of the inserts were visualized and photographed by microscopy (CKX41, Olympus, Japan).
Statistical analysis
For all quantitative data, the mean ± SEM was expressed. The data were evaluated and presented with GraphPad Prism 9.5 (GraphPad Software, USA). The statistical comparison was evaluated with one-way ANOVA. P < 0.05 was deemed statistically significant. In the graphs, asterisks are displayed to indicate the statistical significance of the values. *: P < 0.05; **: P < 0.01; ***: P < 0.001.
Results
Decellularization of human amniotic membrane
Neatly arranged amniotic epithelial cells were visibly observed in the superficial layer of the native amniotic membrane (nAM) (Fig. 1A). The collagen fiber structures could be seen when the amniotic epithelial cells were completely removed with the above mentioned protocol (Fig. 1B). The DAPI stained nuclei showed that nAM contained a high number of hAECs (Fig. 1C). Conversely, the complete decellularization of the amniotic membrane was verified by the non-availability of the DAPI-stained nucleus on the decellularized amniotic membrane (dAM) (Fig. 1D). These results showed the successful preparation of a completely decellularized amniotic membrane.
Decellularization of amniotic membrane and isolation of hAECs. (A) hAEC morphology on native amniotic membrane (nAM). (B) The appearance of the amniotic membrane (AM) following the removal of hAECs. (C) The cell nuclei of hAECs were stained with DAPI. (D) The cell nucleus-stained dAM showed complete removal of hAECs. (A-D) Scale bar: 100 μm. (E) Cell morphology of hAECs cultured in AEC culture medium at passage 2. Scale bar: 200 μm. (F) Immunofluorescence staining revealed the specific markers CK19, E-cadherin, and SSEA-4 in cultured hAECs. Scale bar: 100 μm. Abbreviations: hAECs: human Amniotic Epithelial Cells; nAM: native amniotic membrane; dAM: decellularized amniotic membrane
Isolation and identification of hAECs
In this study, human amniotic epithelial cells (hAECs) isolated from the human amniotic membrane can be cultured to a confluent and tightly connected monolayer cell with hAEC medium (Fig. 1E). The cultured hAECs expressed hAEC-specific markers, including CK19, E-cadherin, and SSEA-4 (Fig. 1F), as determined by the immunofluorescence assay. With morphology and protein identification, hAECs were isolated and stably expanded in vitro.
Application of genipin to crosslink decellularized amniotic membrane
Freshly separated nAM and dAM show white lamellae against a black background (Fig. 2A). The genipin-crosslinked amniotic membrane had a light blue appearance. And its color gradually deepens as the concentration of genipin increases (Fig. 2B).
Appearance and optical clarity of amniotic membrane. (A) Appearance of native and decellularized amniotic membrane. (B) Appearance of genipin-crosslinked amniotic membrane. (C-D) Comparison of optical clarity of different amniotic membrane groups. Abbreviations: nAM: native amniotic membrane; dAM: decellularized amniotic membrane; cl-dAM: genipin-crosslinked decellularized amniotic membrane
However, crosslinking with genipin had no significant effect on the transparency of the amniotic membranes. As shown in Fig. 2C-D, the optical clarity of the amniotic membrane in the 2 mg/mL cl-dAM, 4 mg/mL cl-dAM, and 8 mg/mL cl-dAM was between the nAM and dAM. In addition, among the genipin-crosslinked amniotic membranes, the 8 mg/mL cl-dAM showed a slightly lower clarity as a result of a higher blue tint compared to the 2 mg/mL cl-dAM. Thus, dAM crosslinked with 2 mg/mL genipin did not affect the transparency of the amniotic membrane.
Crosslinked dAM can resist biodegradation
Anti-biodegradation is an important consideration for the transplantation and application of amniotic membrane on the ocular surface. We further observe and record the physical appearance of the amniotic membrane prior to immersion in 0.1 mg/mL of collagenase I at 37 °C. The dAM was wholly degraded after 24 h. Only a small amount of debris was seen in the nAM after 5 days of collagenase digestion. The 2 mg/mL cl-dAM, 4 mg/mL cl-dAM, and 8 mg/mL cl-dAM still maintained a physically intact structure. No significant difference was seen in the 2 mg/mL cl-dAM compared with the 4 mg/mL cl-dAM and 8 mg/mL cl-dAM (Fig. 3A). Since the decellularization process damages the amniotic membrane to some extent, dAM was rapidly degraded, while genipin effectively increased the biostability of dAM. It is evident that crosslinked dAM with 2 mg/mL genipin can be sufficiently resistant to biodegradation.
The characteristics study of genipin crosslinked amniotic membrane. (A) The anti-biodegradation ability of the amniotic membrane with or without crosslinking was determined by digestion with type I collagenase. (B) The CCK-8 assay detected the cytotoxic effects of the extracts of genipin crosslinked amniotic membranes on HCECs for 24 h and 72 h. (C) The amniotic membranes were analyzed by SEM (1000 × and 10,000 × magnification) to analyze the changes in ultrastructure. Data are presented as mean ± SEM (n = 3). *: P < 0.05; **: P < 0.01; ***: P < 0.001. Abbreviations: nAM: native amniotic membrane; dAM: decellularized amniotic membrane; cl-dAM: genipin-crosslinked decellularized amniotic membrane
Furthermore, we performed the CCK-8 assay to determine the cytotoxicity of genipin-crosslinked dAM in vitro using HCEC. Compared with the control group, the extracts from the nAM, dAM, and 2 mg/mL cl-dAM promoted HCECs proliferation but did not appear to cause cytotoxicity. The extracts from the 4 mg/mL cl-dAM had neither toxic nor proliferative effects, while the extracts from the 8 mg/mL cl-dAM showed cytotoxicity effects (Fig. 3B). These results show that 2 mg/mL cl-dAM and 4 mg/mL cl-dAM are the safe concentrations to crosslink the amniotic membrane, and 2 mg/mL cl-dAM is better.
Surface ultrastructure of amniotic membrane
Next, we performed SEM to analyze the surface morphology and ultrastructure of AM. At 1000 × magnification, the surface of nAM was covered by tightly arranged amniotic epithelial cells so that the morphology and arrangement of the underlying AM fibers could not be observed. After complete decellularization of hAECs, it was observed that the surface of the amniotic membrane was rough and fibrillar, and the fibers were interconnected to form pores of different sizes. However, the surface of genipin-crosslinked amniotic membrane (cl-dAM) was smoother compared to dAM (Fig. 3C). At 10,000 × magnification, we can observe a thickening of the fibers and an increase in the space between the fibers in the cl-dAM compared to dAM.
Construct of living cell tissue-engineered amniotic membrane
hAECs are reported to secrete growth factors and exosomes to promote tissue repair. Re-planting the functional hAECs onto the genipin-crosslinked amniotic membrane can improve the clinical outcome of the tissue-engineered amniotic membrane. After hAECs were cultured for 24 h, attached cells were observed on the dAM and 2 mg/mL cl-dAM, with more attached cells on the 2 mg/mL cl-dAM (Fig. 4A). Continuously maintaining for another 72 h, the attached hAECs could proliferate and spread on the amniotic membrane. hAECs grown on 2 mg/mL cl-dAM were more neatly arranged, with clearer cell borders and fewer vacuolated cells compared to the dAM group. We further employ H&E staining of the amniotic membrane to demonstrate the attachment and proliferation of hAECs on dAM and 2 mg/mL cl-dAM (Fig. 4B and E). This result indicated that hAECs were able to re-plant onto the dAM, and crosslinking the dAM with 2 mg/mL genipin solution facilitated the proliferation and spread of hAECs on the amniotic membrane.
Re-plant crosslinked amniotic membrane with living hAECs. (A) hAECs attachment and proliferation on the dAM and the 2 mg/mL cl-dAM. (B-E) H&E staining of amniotic membrane sections from nAM(B), dAM(C), hAECs-containing dAM(D), and hAECs-containing 2 mg/mL cl-dAM (E). Scale bar: 200 μm. Abbreviations: nAM: native amniotic membrane; dAM: decellularized amniotic membrane; cl-dAM: genipin-crosslinked decellularized amniotic membrane
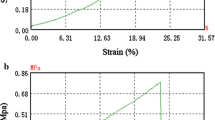
The facilitation effect of tissue-engineered amniotic membrane on HCSCs
In most cases, the proliferation and migration of corneal epithelial cells are prominent, but how to promote the proliferation and migration of corneal stromal cells is not yet clear. We further determined the effect of the living hAEC tissue-engineered amniotic membrane on the function of HCSCs. The CCK-8 assay and transwell assay revealed that the living hAEC tissue-engineered amniotic membrane significantly promoted the proliferation and migration of HCSCs. First, we culture cl-dAM and hAECs-dAM extracts with HCSCs. The extracts of hAECs-cl-dAM significantly promote cell proliferation with the CCK-8 assay (P < 0.01) (Fig. 5A). Studies have shown that CSCs begin to migrate to the damaged area within 24 h, accompanied by cell morphology changes [26]. We placed the cl-dAM or hAECs-cl-dAM in the bottom and the HCSCs in the upper compartment of the transwell insert as shown in Fig. 5B. After treating HCSCs with living-hAECs tissue-engineered amniotic membrane for 24 h, more crystal violet-stained cells were visualized on the lower surface of the transwell insert (Fig. 5C). The migrated cell numbers were subject to statistical analysis, and the results were statistically significant (Fig. 5D). These results further indicated that living hAECs crosslinked AM could facilitate the migration of HCSCs in vitro, which is very significant for accelerating tissue repair after ocular surface injury.
The facilitation effect of tissue-engineered amniotic membrane on the migration of HCSCs. (A) Cell viability of HCSCs co-cultured with cl-dAM or hAECs-cl-dAM extracts. (B) HCSC migration pattern diagram using cl-dAM or hAECs-cl-dAM co-culture. (C) Representative images of migrated cells with crystal violet staining in the transwell assay for 24 h. Scale bar: 200 μm. (D) Histogram representation of the number of migrated cells in the transwell assay. Data are presented as mean ± SEM (n = 3). ***: P < 0.001
Discussion
The human amniotic membrane (AM) contains various types of collagen and is recognized as an exceptional collagen-based biomaterials [27]. Collagen-based implants are frequently crosslinked to enhance their strength and elasticity, as well as to resist their premature degradation in the host system [28]. Our findings demonstrated that the dAM crosslinked with genipin was more resistant to enzymatic biodegradation than the nAM and dAM. Previous studies have shown both genipin and genipin crosslinked scaffolds can promote cell proliferation and differentiation [29, 30]. But there is a dose-dependent crosslinking effect and cytotoxicity of genipin [31, 32]. Genipin is known to react spontaneously with amino acids or proteins, resulting in the formation of blue pigments, and it is frequently employed in the food industry to manufacture food dyes [32]. The genipin crosslinked AM displayed a light blue appearance, and its color deepened with increasing concentrations of genipin. In addition, the microscopic observation and H&E staining results showed that, compared with the decellularized amniotic membrane, the 2 mg/mL cl-dAM was more favorable for attachment, migration, and proliferation of hAECs. We considered the optimal genipin concentration (2 mg/mL) was suitable for the construction of living-hAECs tissue-engineered AM with better optical clarity, anti-biodegradation properties, and lower cytotoxicity.
In this study, extracts from both native AM and living-hAECs tissue-engineered AM significantly promote the proliferation of target cells, including HCECs and HCSCs. Additionally, the hAECs were enabled to attach, migrate, and proliferate on 2 mg/mL cl-dAM very well. The paracrine effects of hAECs have been reported to contain growth factors, inflammatory regulators, and exosomes to intervene in the excessive epithelial-mesenchymal transition and regenerate the injured tissues [33, 34]. Corneal stromal cells (CSCs) are considered the primary cell type for repairing tissue in the process of corneal wound healing. Cell migration of the remaining stroma contributes to corneal stromal reformation through secreting growth factors and extracellular matrix [35]. Our results showed that living hAECs crosslinked-AM could facilitate the migration of HCSCs in vitro. Therefore, re-planting the hAECs onto the crosslinked AM could enhance the outcome of the application of crosslinked AM.
The theoretical advantages of using living hAECs crosslinked-AM in tissue engineering and regenerative medicine are multifaceted. On one hand, the benefits stem from the enhanced biocompatibility, structural integrity, and mechanical properties imparted by genipin crosslinking. On the other hand, the presence of hAECs can promote tissue regeneration and repair because of the well-known regenerative properties of these cells.
To summarize, we propose that hAECs be re-planted onto tissue-engineering biomaterials to improve clinical outcomes. The integration of functional stem cells and biomaterials is widely accepted. Although we modified the crosslinked AM, the re-planted hAECs are also suitable for other biomaterials. Future studies will be focused on assessing the capability of living-hAECs tissue-engineered AM to repair ocular surface lesions in animal models.
Conclusion
Compared to nAM and dAM, 2 mg/mL cl-dAM demonstrates superior biostability and biocompatibility. With the attachment, proliferation, and migration of hAECs on 2 mg/mL cl-dAM, living-hAECs tissue-engineered AM was successfully constructed. This living-hAECs tissue-engineered amniotic membrane presents a promising candidate for tissue repair, including the ocular surface.
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information.
Abbreviations
- AM:
-
amniotic membrane
- nAM:
-
native amniotic membrane
- dAM:
-
decellularized amniotic membrane
- cl-dAM:
-
genipin-crosslinked decellularized amniotic membrane
- hAEC:
-
human amniotic epithelial cell
- hCEC:
-
human corneal epithelial cell
- hCSC:
-
human corneal stromal cell
- PBS:
-
phosphate-buffered saline
- PFA:
-
paraformaldehyde
- SEM:
-
scanning electron microscope
References
Zhou H, Lu Q, Guo Q, Chae J, Fan X, Elisseeff JH, Grant MP. Vitrified collagen based conjunctival equivalent for ocular surface reconstruction. Biomaterials. 2014;35(26):7398–406.
Gipson IK. The ocular surface: the challenge to enable and protect vision: the Friedenwald lecture. Investig Ophthalmol Vis Sci. 2007;48(10):4391–8.
Nakamura T, Inatomi T, Sotozono C, Koizumi N, Kinoshita S. Ocular surface reconstruction using stem cell and tissue engineering. Prog Retin Eye Res. 2016;51:187–207.
McLaren J, Malak TM, Bell SC. Structural characteristics of term human fetal membranes prior to labour: identification of an area of altered morphology overlying the cervix. Hum Reprod. 1999;14(1):237–41.
Ma KN, Thanos A, Chodosh J, Shah AS, Mantagos IS. A novel technique for amniotic membrane transplantation in patients with acute Stevens-Johnson syndrome. Ocul Surf. 2016;14(1):31–6.
Le Q, Deng SX. The application of human amniotic membrane in the surgical management of limbal stem cell deficiency. Ocul Surf. 2019;17(2):221–9.
Riau AK, Beuerman RW, Lim LS, Mehta JS. Preservation, sterilization and de-epithelialization of human amniotic membrane for use in ocular surface reconstruction. Biomaterials. 2010;31(2):216–25.
Jie J, Yang J, He H, et al. Tissue remodeling after ocular surface reconstruction with denuded amniotic membrane. Sci Rep. 2018;8(1):6400.
Asl NS, Nejat F, Mohammadi P, Nekoukar A, Hesam S, Ebrahimi M, Jadidi K. Amniotic membrane extract eye drop promotes limbal stem cell proliferation and corneal epithelium healing. Cell J (Yakhteh). 2019;20(4):459.
Guo Q, Hao J, Yang Q, Guan L, Ouyang S, Wang J. A comparison of the effectiveness between amniotic membrane homogenate and transplanted amniotic membrane in healing corneal damage in a rabbit model. Acta Ophthalmol. 2011;89(4):e315–9.
Zhou Z, Long D, Hsu CC, et al. Nanofiber-reinforced decellularized amniotic membrane improves limbal stem cell transplantation in a rabbit model of corneal epithelial defect. Acta Biomater. 2019;97:310–20.
Yoo JS, Kim YJ, Kim SH, Choi SH. Study on genipin: a new alternative natural crosslinking agent for fixing heterograft tissue. Korean J Thorac Cardiovasc Surg. 2011;44(3):197.
Wang Z, Liu H, Luo W, et al. Regeneration of skeletal system with genipin crosslinked biomaterials. J Tissue Eng. 2020;11:2041731420974861.
Nair M, Johal RK, Hamaia SW, Best SM, Cameron RE. Tunable bioactivity and mechanics of collagen-based tissue engineering constructs: a comparison of EDC-NHS, genipin and TG2 crosslinkers. Biomaterials. 2020;254:120109.
Gobinathan S, Zainol SS, Azizi SF, et al. Decellularization and genipin crosslinking of amniotic membrane suitable for tissue engineering applications. J Biomater Sci Polym Ed. 2018;29(17):2051–67.
Wassmer CH, Berishvili E. Immunomodulatory properties of amniotic membrane derivatives and their potential in regenerative medicine. Curr Diab Rep. 2020;20:1–10.
Yang P, Yuan W, Liu J, et al. Biological characterization of human amniotic epithelial cells in a serum-free system and their safety evaluation. Acta Pharmacol Sin. 2018;39(8):1305–16.
Hodges RJ, Lim R, Jenkin G, Wallace EM. (2012). Amnion epithelial cells as a candidate therapy for acute and chronic lung injury. Stem cells international, 2012.
Andrewartha N, Yeoh G. (2019). Human amnion epithelial cell therapy for chronic liver disease. Stem Cells International, 2019, p. 8106482, 2019, https://doi.org/10.1155/2019/8106482
Zhao B, Liu JQ, Zheng Z, et al. Human amniotic epithelial stem cells promote wound healing by facilitating migration and proliferation of keratinocytes via ERK, JNK and AKT signaling pathways. Cell Tissue Res. 2016;365:85–99.
Parmar DN, Alizadeh H, Awwad ST, et al. Ocular surface restoration using non-surgical transplantation of tissue-cultured human amniotic epithelial cells. Am J Ophthalmol. 2006;141(2):299–307.
Hu S, Wang Z, Jin C, et al. Human amniotic epithelial cell-derived extracellular vesicles provide an extracellular matrix-based microenvironment for corneal injury repair. J Tissue Eng. 2022;13:20417314221122123.
Bi L, Cao Z, Hu Y, et al. Effects of different cross-linking conditions on the properties of genipin-cross-linked chitosan/collagen scaffolds for cartilage tissue engineering. J Mater Science: Mater Med. 2011;22:51–62.
Jin C, Ou Q, Chen J, et al. Chaperone-mediated autophagy plays an important role in regulating retinal progenitor cell homeostasis. Stem Cell Res Ther. 2022;13(1):1–14.
Jin J, Ou Q, Wang Z, et al. BMSC-derived extracellular vesicles intervened the pathogenic changes of scleroderma in mice through miRNAs. Stem Cell Res Ther. 2021;12(1):327.
Fini ME, Stramer BM. How the cornea heals: cornea-specific repair mechanisms affecting surgical outcomes. Cornea. 2005;24(8):S2–11.
Jirsova K, Jones GL. Amniotic membrane in ophthalmology: properties, preparation, storage and indications for grafting—a review. Cell Tissue Banking. 2017;18:193–204.
Gu L, Shan T, Ma YX, Tay FR, Niu L. Novel biomedical applications of crosslinked collagen. Trends Biotechnol. 2019;37(5):464–91.
Frohbergh ME, Katsman A, Botta GP, Lazarovici P, Schauer CL, Wegst UG, Lelkes PI. Electrospun hydroxyapatite-containing chitosan nanofibers crosslinked with genipin for bone tissue engineering. Biomaterials. 2012;33(36):9167–78.
Kwon YS, Lim ES, Kim HM, Hwang YC, Lee KW, Min KS. Genipin, a cross-linking agent, promotes odontogenic differentiation of human dental pulp cells. J Endod. 2015;41(4):501–7.
Fessel G, Cadby J, Wunderli S, van Weeren R, Snedeker JG. Dose-and time-dependent effects of genipin crosslinking on cell viability and tissue mechanics–toward clinical application for tendon repair. Acta Biomater. 2014;10(5):1897–906.
Sung HW, Chang Y, Liang IL, Chang WH, Chen YC. Fixation of biological tissues with a naturally occurring crosslinking agent: fixation rate and effects of pH, temperature, and initial fixative concentration. J Biomed Mater Res. 2000;52(1):77–87.
Fathi I, Miki T. Human amniotic epithelial cells Secretome: components, Bioactivity, and challenges. Front Med. 2022;8:763141.
Zhang Q, Lai D. Application of human amniotic epithelial cells in regenerative medicine: a systematic review. Stem Cell Res Ther. 2020;11(1):1–16.
Chen TC, Tsai TY, Chang SW. Molecular mechanism of fluoroquinolones modulation on corneal fibroblast motility. Exp Eye Res. 2016;145:10–6.
Acknowledgements
We acknowledge Professor Qingjun Zhou (Shandong Eye Institute, China) for the kind gifts of human corneal epithelial cell line and human corneal stromal cell line.
Funding
This paper was supported by the National Natural Science Foundation of China (82271108).
Author information
Authors and Affiliations
Contributions
SH and QO conceived and designed the experiments, performed the experiments, analyzed the data, and wrote the paper. QO and G-T X contributed to designing the experiment, financial support, manuscript writing, and final approval of the manuscript. CJ, JJ, and YL contributed to reagents/materials/analysis tools. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
After written informed consent was obtained from every placental donor, amniotic membranes were collected from term healthy placentas of women according to the guidelines and approval of the Human Research Ethics Committee of the School of Medicine of Tongji University (Approval No.2021TJDX053). All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hu, S., Chen, J., Jin, J. et al. Construction of living-cell tissue engineered amniotic membrane for ocular surface disease. BMC Ophthalmol 24, 409 (2024). https://doi.org/10.1186/s12886-024-03680-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03680-7