Abstract
Background
Preterm infants often require non-invasive breathing support while their lungs and control of respiration are still developing. Non-invasive neurally adjusted ventilatory assist (NIV-NAVA) is an emerging technology that allows infants to breathe spontaneously while receiving support breaths proportional to their effort. This study describes the first Australian Neonatal Intensive Care Unit (NICU) experience of NIV-NAVA.
Methods
Retrospective cohort study of infants admitted to a major tertiary NICU between October 2017 and April 2021 supported with NIV-NAVA. Infants were divided into three groups based on the indication to initiate NIV-NAVA (post-extubation; apnoea; escalation). Successful application of NIV-NAVA was based on the need for re-intubation within 48 h of application.
Results
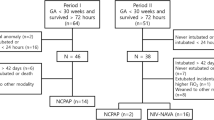
There were 169 NIV-NAVA episodes in 122 infants (82 post-extubation; 21 apnoea; 66 escalation). The median (range) gestational age at birth was 25 + 5 weeks (23 + 1 to 43 + 3 weeks) and median (range) birthweight was 963 g (365–4320 g). At NIV-NAVA application, mean (SD) age was 17 days (18.2), and median (range) weight was 850 g (501–4310 g). Infants did not require intubation within 48 h in 145/169 (85.2%) episodes [72/82 (87.8%) extubation; 21/21 (100%) apnoea; 52/66 (78.8%) escalation).
Conclusion
NIV-NAVA was successfully integrated for the three main indications (escalation; post-extubation; apnoea). Prospective clinical trials are still required to establish its effectiveness versus other modes of non-invasive support.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Advancing medical knowledge and improving technology over the past decades has seen consistent increases in survival rates for extreme preterm infants. Despite these improvements, there continues to be high rates of ventilator-associated complications with little reduction in rates of bronchopulmonary dysplasia (BPD). This has resulted an increased use of non-invasive ventilation (NIV), including more sophisticated methods of achieving patient-triggered ventilation [1, 2]. Systems that synchronise respiratory effort with lung inflation may help mitigate the long-term consequences of asynchrony including lung injury via volutrauma or hyperoxia [3]. Consequently, the use of NIV continues to increase, however, there are a paucity of data demonstrating clinical benefit [2, 4].
Neonatal non-invasive ventilation is used for a variety of indications which include respiratory failure, prevention of extubation failure and persistent, severe apnoea of prematurity [4,5,6,7]. Well-established non-invasive modes of respiratory support range from nasal continuous positive airway pressure (NCPAP), nasal intermittent positive pressure ventilation (NIPPV) and high-flow nasal cannula (HFNC). These all have varying volume and quality of supporting literature [4,5,6, 8]. Indeed, NCPAP, NIPPV and HFNC have respective benefits with regard to safety, efficacy, and ease of clinical use [1, 9]. However, there are limitations to these modalities particularly in terms of synchrony with infants breathing efforts for NIPPV and infants with absent or insufficient respiratory drive [4, 10, 11].
Neurally adjusted ventilatory assist (NAVA) differs from traditional ventilatory support, which adjusts ventilation according to pressure or flow changes, as NIV-NAVA delivers synchronised and scaled inspiratory support based upon the electrical diaphragmatic signal (Edi) activity [12, 13]. Minute sensors are embedded within standard feeding tubes to detect Edi [3, 12, 14]. This has no impact on feeding whilst monitoring the overall respiratory drive [15]. A computer algorithm analyses a filtered and amplified Edi signal to trigger the ventilation system. The system detects the start of a breath as it is being initiated in the diaphragm and provides synchronised support during inspiration. The level of support changes during inspiration in proportion to the detected Edi [13, 14]. Inspiratory support discontinues as the system detects the Edi signal decreasing to allow expiration. With adequate support, neural feedback mechanisms theoretically result in a decrease in respiratory drive with subsequent lower levels of inspiratory support [15]. However, this is not always seen in preterm infants due to immature neural feedback mechanisms [16].
The aim of this study was to evaluate our experience with NIV-NAVA by describing the intubation rate at 48 h following the initiation of NIV-NAVA for the following indications:
-
Post-extubation as a weaning mode from invasive ventilation.
-
As an escalation mode from NCPAP.
-
NCPAP therapy with a backup breath facility to treat apnoeas.
Methods
This was a retrospective cohort study conducted at the Royal Hospital for Women Neonatal Intensive Care Unit (NICU). Infants admitted to this unit between 4 October 2017 and 20 April 2021 who received NIV-NAVA during their admission were included in the study. Standard demographic maternal, perinatal, and neonatal data variables were extracted. Inclusion criteria included: inpatient, complete electronic medical records, indications for NIV-NAVA applications including post-extubation, escalation and apnoea (NIV-NAVA is not currently used as a primary mode of respiratory support in this unit). Exclusion criteria included: application of NIV-NAVA at another hospital or for other indications and if the patient had known congenital malformations of the lungs, airways or chest wall. All infants were managed using the Royal Hospital for Women’s, “NAVA (Neurally Adjusted Ventilatory Assist”, clinical guidelines (Appendix 1). Indications for the initiation of NIV-NAVA and typical settings for these indications can be found in the clinical guidelines.
The primary outcome was the need for intubation within 48 h of NIV-NAVA initiation. The decision for intubation was at the discretion of the treating neonatologist. Infants were stratified by indication and analysed in subgroups. We also investigated change in FiO2 and PCO2 when NIV-NAVA was used as an escalation mode. Infants may have required NIV-NAVA multiple times and subsequently appear across multiple indication groups or record more than one episode for the same indication.
The Respiratory Severity Score (RSS) was calculated prior to initiation of NIV-NAVA to indicate level of respiratory illness upon study entry point. This was calculated as either:
OR
MAP, mean arterial pressure; PIP, Peak inspiratory pressure in cm; PEEP, Positive end-expiration pressure in cm H2O; FiO2, fraction of inspired oxygen.
All statistical analyses were conducted using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., Armonk, NY: IBM Corp). Descriptive statistics were used to present the results of the study and summarised to the indication for NIV-NAVA. Data was inspected for normality before further analysis. Continuous demographic variables including the outcomes of FiO2 and pCO2 were summarised by mean and standard deviation if normally distributed and by median and range if not. Differences between initial and subsequent FiO2 and pCO2 were analysed by a paired samples test across all three indications. Statistical significance was set at p < 0.05.
The study was approved by the South Eastern Sydney Local Health District (Northern Sector) Human Research Ethics Committee (2020/ETH02488).
Results
122 infants were included in the study period; there were 169 episodes of NIV-NAVA use for the three different indications. The average age of the infants commencing NIV-NAVA therapy was 17.2 days with a median weight of 839 g. The median respiratory severity score was 2.6. The perinatal clinical characteristics of included infants is summarised in Table 1.
Of the infants requiring extubation from invasive ventilation, 72 (87.8%) did not require intubation after 48 h. 52 (78.8%) infants were successfully escalated from NCPAP to NIV-NAVA. 21 (100%) of those requiring NIV-NAVA for apnoea treatment were not intubated at 48 h. The overall rate of not requiring intubation following NIV-NAVA use was 145/169 (86%). There were 110 infants < 1000 g at the time of application of NIV-NAVA. 90/110 (82%) in this subgroup did not require intubation. The reason for intubation was not consistently reported but was usually for oxygenation and/or ventilation failure. There were no significant changes in mean FiO2 (33.8% before; 32.7% after [p = 0.353]) or pCO2 (49.4 mmHg before; 48.8 mmHg after [p = 0.547]) with application of NIV-NAVA in the escalation group. The clinical characteristics of the infants whilst on NIV-NAVA in addition to their prior ventilation modes is summarised in Table 2. There were no adverse events documented related to either the use of the NAVA catheter or the ventilation system.
Discussion
This retrospective cohort study describes the first experience of NIV-NAVA in an Australian NICU and represents the largest reported cohort of NIV-NAVA infants [9, 10, 16,17,18]. Within 48 h of application of NIV-NAVA for all indications, the majority of infants did not require intubation (86%). This is encouraging as these infants were at high risk of intubation, as evidenced by the cohort’s Respiratory Severity Scores (RSS) [19, 20]. The particularly high rate of success in infants with apnoeas highlights the effectiveness of the back-up support that is activated when the system detects an apnoeic episode. These results are consistent with other studies that have shown low intubation rates following the application of NIV-NAVA [21,22,23,24,25,26,27].
As a surrogate marker of respiratory status, we compared FiO2 and pCO2 before and after the application of NIV-NAVA in the escalation group and found no significant differences. Previous similar studies have shown that the application of NIV-NAVA in this setting either has no effect or improves these parameters [18, 22, 25, 28, 29]. The blood gases in this study were based on clinical need and were not timed. As a result, there was significant variability in the timing of FiO2 and pCO2 measurements both before and after the application of NIV-NAVA as well as the overall time between blood gases. In some circumstances, the two gases may not have been optimally timed to accurately capture the change in respiratory status [30, 31].
There are a number of important limitations to acknowledge in this study. Although it is reassuring that the rate of intubation in this cohort was low, there was no way of determining how many of these infants would have required intubation if alternative modes of non-invasive respiratory support were used. It was not possible to find a suitable control group of infants in whom NIV-NAVA was not used as the infants in this cohort were at significantly higher risk of needing intubation in which case their respiratory support was escalated to NIV-NAVA. They were also not representative of a typical cohort of infants requiring non-invasive respiratory support. The study is also inherently limited by its opportunistic nature, particularly with respect to finding objective measures of clinical change before and after the application of NIV-NAVA. While it is reassuring that infants in the escalation group had stable blood gas parameters, the lack of control in the timing of blood collection limits what we can conclude.
NCPAP has a well-established, evidenced-based role in the NICU environment and is the most widely used non-invasive mode of support for infants with respiratory distress. However, there are clinical circumstances where NCPAP alone does not provide adequate support and other forms of NIPPV may not be synchronised. NIV-NAVA has the theoretical advantages of optimising synchrony with breathing and providing support that is proportional to infants’ breathing efforts. Cohort studies such as this continue to show the stability that can be achieved with the application of NIV-NAVA in high-risk infants and adds to the growing body of evidence that supports its use in the NICU environment in selected clinical circumstances. Large, high-quality randomised trials are currently lacking but are essential to help further establish where NIV-NAVA fits into clinical practice [12, 32].
This study has shown that NIV-NAVA can be successfully integrated into the NICU environment for three main indications (escalation; post-extubation; apnoea). Although promising, it is important to note that prospective clinical trials are still required to establish the effectiveness of NIV-NAVA by comparing it to other modes of non-invasive support.
Data availability
The datasets used and analysed during the study are available from the corresponding author (Dr Tim Schindler) on reasonable request.
References
Kugelman A, editor. Controversies and update on non invasive ventilation in the NICU. Pediatr Pulmonol; 2017 2017.
Kugelman A, editor. Update on noninvasive ventilation in the NICU. Pediatr Pulmonol; 2019 2019.
Rossor TE, Hunt KA, Shetty S, Greenough A. Neurally adjusted ventilatory assist compared to other forms of triggered ventilation for neonatal respiratory support. Cochrane Database Syst Rev. 2017.
Boel L, Broad K, Chakraborty M. Non-invasive respiratory support in newborn infants. J Paediatr Child Health. 2018;28(1):6–12.
Lemyre B, Davis PG, De Paoli AG, Kirpalani H. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. 2017.
Lemyre B, Laughon M, Bose C, Davis PG. Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev. 2016.
Bancalari E, Claure N. The evidence for non-invasive ventilation in the preterm infant. Arch Dis Child Fetal Neonatal Ed. 2013;98(2):F98–102.
Abdel-Hady H, Shouman B, Nasef N. Weaning preterm infants from continuous positive airway pressure: evidence for best practice. World J Pediatr. 2015;11(3):212–8.
Shi Y, Muniraman H, Biniwale M, Ramanathan R. A review on non-invasive respiratory support for management of respiratory distress in extremely preterm infants. Front Pediatr. 2020;8:270.
Firestone K, Horany BA, de Leon-Belden L, Stein H. Nasal continuous positive airway pressure versus noninvasive NAVA in preterm neonates with apnea of prematurity: a pilot study with a novel approach. J Perinatol. 2020;40(8):1211–5.
Shehadeh AMH. Non-invasive respiratory support for preterm infants following extubation from mechanical ventilation. A narrative review and guideline suggestion. Pediatr Neonatol. 2020;61(2):142–7.
Goel D, Oei JL, Smyth J, Schindler T. Diaphragm-triggered non-invasive respiratory support in preterm infants. Cochrane Database Syst Rev. 2020(3).
Terzi N, Piquilloud L, Roze H, Mercat A, Lofaso F, Delisle S, et al. Clinical review: update on neurally adjusted ventilatory assist - report of a round-table conference. Crit Care. 2012;16(3):225.
Stein H, Beck J, Dunn M. Non-invasive ventilation with neurally adjusted ventilatory assist in newborns. Semin Fetal Neonatal Med. 2016;21(3):154–61.
Ververidis D, Van Gils M, Passath C, Takala J, Brander L. Identification of adequate neurally adjusted ventilatory assist (NAVA) during systematic increases in the NAVA level. IEEE Trans Biomed Eng. 2011;58(9):2598–606.
Beck J, Reilly M, Grasselli G, Qui H, Slutsky AS, Dunn MS, et al. Characterization of neural breathing pattern in spontaneously breathing preterm infants. Pediatr Res. 2011;70(6):607–13.
Martin RJ, Abu-Shaweesh JM. Control of breathing and neonatal apnea. Biol Neonate. 2005;87(4):288–95.
Colaizy TT, Kummet GJ, Kummet CM, Klein JM. Noninvasive neurally adjusted ventilatory assist in premature infants postextubation. Am J Perinatol. 2017;34(6):593–8.
Malkar MB, Gardner WP, Mandy GT, Stenger MR, Nelin LD, Shepherd EG, et al. Respiratory severity score on day of life 30 is predictive of mortality and the length of mechanical ventilation in premature infants with protracted ventilation. Pediatr Pulmonol. 2015;50(4):363–9.
Mhanna MJ, Iyer NP, Piraino S, Jain M. Respiratory severity score and extubation readiness in very low birth weight infants. Pediatr Neonatol. 2017;58(6):523–8.
García-Muñoz Rodrigo F, Rivero Rodriguez SM, Florido Rodríguez A, Martín Cruz FG. Galán Henríquez GM, Díaz Pulido R. Preliminary Experience with the Use of Neurally Adjusted Ventilatory Assist in the neonate. Arch Dis Child. 2014;99(Suppl 2):A496.
Lee BK, Shin SH, Jung YH, Kim EK, Kim HS. Comparison of NIV-NAVA and NCPAP in facilitating extubation for very preterm infants. BMC Pediatr. 2019;19(1):298.
Gibu CK, Cheng PY, Ward RJ, Castro B, Heldt GP. Feasibility and physiological effects of noninvasive neurally adjusted ventilatory assist in preterm infants. Pediatr Res. 2017;82(4):650–7.
Miyahara J, Sugiura H, Ohki S. The evaluation of the efficacy and safety of non-invasive neurally adjusted ventilatory assist in combination with intubation-surfactant-extubation technique for infants at 28 to 33 weeks of gestation with respiratory distress syndrome. SAGE Open Med. 2019;7:2050312119838417.
Parmer T, Smyth J, Bolisetty S, Lui K, Schindler T. Non-invasive neurally adjusted ventilatory assist (NAVA) in newborns: first Australian NICU experience. J Paediatr Child Health. 2017;53:87–8.
Rong X, Liang F, Li YJ, Liang H, Zhao XP, Zou HM, et al. Application of neurally adjusted ventilatory assist in premature neonates less than 1,500 grams with established or evolving bronchopulmonary dysplasia. Front Pediatr. 2020;8(110):110.
Makker K, Cortez J, Jha K, Shah S, Nandula P, Lowrie D, et al. Comparison of extubation success using noninvasive positive pressure ventilation (NIPPV) versus noninvasive neurally adjusted ventilatory assist (NI-NAVA). J Perinatol. 2020;40(8):1202–10.
Kallio M, Mahlman M, Koskela U, Aikio O, Suo-Palosaari M, Pokka T, et al. NIV NAVA versus nasal CPAP in premature infants: a randomized clinical trial. Neonatology. 2019;116(4):380–4.
Stein H, Howard D. Neurally adjusted ventilatory assist in neonates weighing < 1500 grams: a retrospective analysis. J Pediatr. 2012;160(5):786–9.
Shah SI, Aboudi D, La Gamma EF, Brumberg HL. Respiratory severity score greater than or equal to 2 at birth is associated with an increased risk of mortality in infants with birth weights less than or equal to 1250 g. Pediatr Pulmonol. 2020;55(12):3304–11.
Jung YH, Jang J, Kim H-S, Shin SH, Choi CW, Kim E-K et al. Respiratory severity score as a predictive factor for severe bronchopulmonary dysplasia or death in extremely preterm infants. BMC Pediatr. 2019;19(1).
Kacmarek RM, Villar J, Parrilla D, Alba F, Solano R, Liu S, et al. Neurally adjusted ventilatory assist in acute respiratory failure: a randomized controlled trial. Intensive Care Med. 2020;46(12):2327–37.
Acknowledgements
We acknowledge Dr Kylie-Ann Mallit for her support and expertise with statistical analysis. We also acknowledge the Bidjigal and Gadigal Peoples of the Eora Nation, whose land on which this research was conducted.
Funding
This research was investigator-initiated and did not require external funding.
Author information
Authors and Affiliations
Contributions
TS developed the original concept for the study. TP, JS, SB, and KL provided important intellectual input into the development of the study protocol. TS and TP performed a preliminary analysis to establish feasibility. JC was responsible for all data collection. JC performed statistical analysis with the assistance of Dr Kylie-Ann Mallit (acknowledgements). JC drafted the initial manuscript and all authors provided editorial input and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the South Eastern Sydney Local Health District (Northern Sector) Human Research Ethics Committee (2020/ETH02488) who deemed that individual consent was not required due to the nature of the study, being a retrospective study of de-identified data. All data was handled as per the New South Wales Information Privacy Commission Statutory Guidelines for Research and the study was conducted in accordance with applicable Privacy Acts and Regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cheng, J., Parmar, T., Smyth, J. et al. Non-invasive neurally adjusted ventilatory assist (NIV-NAVA) in the neonatal intensive care unit (NICU): an Australian NICU experience. BMC Pediatr 24, 514 (2024). https://doi.org/10.1186/s12887-024-04981-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04981-y