Abstract
Background
The objective of this study was to compare HFNC therapy to noninvasive ventilation (NIV/BiPAP) in children with bronchiolitis who developed respiratory failure. We hypothesized that HFNC therapy would not be inferior to NIV.
Methods
This was a noninferiority open-label randomized single-center clinical trial conducted at a tertiary Brazilian hospital. Children under 2 years of age with no chronic conditions admitted for bronchiolitis that progressed to mild to moderate respiratory distress (Wood-Downes-Férres score < 8) were randomized to either the HFNC group or NIV (BiPAP) group through sealed envelopes. Vital signs, FiO2, Wood-Downes-Férres score and HFNC/NIV parameters were recorded up to 96 h after therapy initiation. Children who developed respiratory failure despite receiving initial therapy were intubated. Crossover was not allowed. The primary outcome analyzed was invasive mechanical ventilation requirement. The secondary outcomes were sedation usage, invasive mechanical ventilation duration, the PICU LOS, the hospital LOS, and mortality rate.
Results
A total of 126 patients were allocated to the NIV group (132 randomized and 6 excluded), and 126 were allocated to the HFNC group (136 randomized and 10 excluded). The median age was 2.5 (1–6) months in the NIV group and 3 (2–7) months in the HFNC group (p = 0,07). RSV was the most common virus isolated in both groups (72% vs. 71.4%, NIV and HFNC, respectively). Thirty-seven patients were intubated in the NIV group and 29 were intubated in the HFNC group (29% vs. 23%, p = 0.25). According to the Farrington-Manning test, with a noninferiority margin of 15%, the difference was 6.3% in favor of HFNC therapy (95% confidence interval: -4.5 to 17.1%, p < 0.0001). There was no significant difference in the PICU LOS or sedation duration. Sedation requirement, hospital LOS and invasive mechanical ventilation duration were lower in the HFNC group.
Conclusion
HFNC therapy is noninferior to NIV in infants admitted with mild to moderate respiratory distress caused by bronchiolitis that progresses to respiratory failure.
Trial registration numbers
U1111-1262-1740; RBR-104z966s. Registered 03/01/2023 (retrospectively registered). ReBEC: https://ensaiosclinicos.gov.br/rg/RBR-104z966s.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
High-flow nasal cannula (HFNC) therapy is an easy-to-apply supplemental oxygen therapy that provides a heated and humidified gas mixture through a nonocclusive interface. In addition to enabling the delivery of a high fraction of inspired oxygen (FiO2), this therapy provides a flow of oxygen that is greater than the patient’s peak inspiratory flow, potentially leading to low levels of positive alveolar opening pressure, decreasing inspiratory resistance, and reducing respiratory work by flushing the nasopharyngeal dead space [1,2,3,4,5].
HFNC therapy has been increasingly applied in the last two decades in both pediatric and adult populations, and it is currently a well-established therapy in the literature for patients who develop respiratory failure. However, there are still questions about the correct time to initiate HFNC therapy and how to escalate treatment in cases of therapy failure. In children, HFNC therapy was first introduced to treat preterm infants as an alternative to continuous positive airway pressure (CPAP) therapy. Over the years, the application of HFNC therapy has been widespread mainly in patients hospitalized for bronchiolitis [6,7,8,9].
Acute viral bronchiolitis is the most common lower respiratory disease and the primary reason for hospitalization among infants. According to a survey carried out in the United States (US) between 2010 and 2019, approximately 20% of hospitalized patients required intensive care, 4.9% required noninvasive mechanical ventilation (NIV), and 3.3% required invasive mechanical ventilation [10]. In a cross-sectional analysis of children admitted for bronchiolitis also performed in the US from 2000 to 2016, an increase in the hospitalization cost was observed—from $449 million to $734 million—after adjustment for inflation [11].
Among the few options for evidence-based supportive care available for patients with bronchiolitis, HFNC therapy has gained relevance mainly due to its easy application outside the pediatric intensive care unit (PICU), comfort, low sedation requirements, and tolerability. Recent studies have demonstrated that HFNC therapy is superior to low-flow oxygen therapy. However, to date, few randomized clinical trials evaluating the effectiveness of HFNC therapy versus NIV (CPAP and BiPAP – bilevel positive airway pressure), especially related to treatment failure and the need for invasive mechanical ventilation, have been published. Furthermore, most of these studies have some methodological limitations, such as the failure criteria not being well described, the lack of an established HFNC weaning protocol, the use of a small sample, the lack of clinical reassessment scores, the restricted populations analyzed, the inclusion of a small number of intubated patients, and the use of a short assessment period. All these biases could interfere with external validation of the use of HFNC therapy in the pediatric population [12,13,14,15,16,17,18].
Therefore, new studies are necessary to compare HFNC therapy to NIV (CPAP/BiPAP) for bronchiolitis, especially regarding treatment failure and the need for mechanical ventilation [6, 18].
The objective of this study was to compare HFNC therapy to NIV (BiPAP) in children with bronchiolitis who experienced mild to moderate respiratory distress and who required noninvasive respiratory support. We hypothesized that HFNC therapy would not be inferior to NIV (BiPAP).
Materials and methods
This noninferiority randomized single-center clinical trial was carried out between February 9, 2021, and May 3, 2023, in the emergency department and PICU of Hospital Municipal Infantil Menino Jesus (HMIMJ), São Paulo, Brazil. This 92-bed tertiary pediatric hospital comprises a 20-bed PICU with a monthly average admission rate of approximately 70 patients.
This study was approved by the Institutional Review Board (IRB) of the hospital (Hospital Municipal Infantil Menino Jesus Research Ethics Committee; approval number 39509820.0.0000.5639, 11/24/2020; trial registration number: U1111-1262-1740; RBR-104z966s, 03/01/2023). Although the clinical trial was submitted before patient randomization, its registration was approved later because some formatting and data adjustments were required. All methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent was obtained from a parent and/or legal guardian before the data were collected by the physician responsible for starting the protocol.
Patients admitted with a diagnosis of mild to moderate acute respiratory distress (Wood-Downes-Férres score < 8 points) caused by bronchiolitis were randomized into two groups using sealed envelopes (the HFNC or NIV groups) [19, 20]. Clinical physician and physiotherapist teams were responsible for identifying potentially eligible study participants. Patients who were admitted to the pediatric ward without respiratory distress but who later met these inclusion criteria were included in the study. Randomization could occur at admission or at any time during the hospital stay after respiratory failure was diagnosed. Each randomized patient received a kit of printed documents to be filled out: a form with vital signs, a form with ventilation scores and parameters, scales for bedside assessment and a consent form. After the protocol was completed, all records were gathered, and the data were transferred to a digital dataset. Each patient receiving NIV or HFNC therapy was transferred to the PICU depending on bed availability.
Local training for device usage and protocol application was carried out with physicians and physiotherapists before and during the research. Training efficacy evaluation was not performed.
The HFNC system used was an Airvo 2 (Fisher & Paykel), and the initial flow was 2 L/kg/min. The NIV system used was DX 3010/3020 (Dixtal). The initial inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP) values were defined according to the institutional protocol (BiPAP – bilevel positive air pressure: EPAP 4 to 6 cmH2O, IPAP 8 to 12 cmH2O) and adjustment through clinical evaluation. Frequency of rescue breathing, and asynchronies was not registered. In both groups, a binasal prong was used. FiO2 was titrated to maintain a peripheral oxygen saturation between 94 and 99%. All eligible patients who developed mild to moderate respiratory distress were connected to a nonrebreathing mask until randomization was performed and the device was properly installed.
The inclusion criteria were children under 2 years of age admitted for bronchiolitis that progressed to mild to moderate respiratory distress (WDF score < 8 points) during hospitalization. Bronchiolitis was clinically defined by upper respiratory tract (runny nose, sneezing) and lower respiratory tract (tachypnea, wheezing, coughing, crackling and use of accessory muscles) symptoms [21]. Blood laboratory investigations were not mandatory for this trial.
The exclusion criteria were severe respiratory distress (WDF score ≥ 8 points), gestational age less than 35 weeks, bronchopulmonary dysplasia, cyanotic congenital heart disease or hemodynamic repercussion, liver disease, neuromuscular disease, or tracheostomy. Infants with a positive viral panel result for SARS-CoV-2, those whose parents refused to participate in this study and those with missing fulfilled forms were also excluded.
Vital signs, WDF score, peripheral oxygen saturation (SpO2), and FiO2 were recorded at 0 h, 2 h, 6 h, 12 h, 24 h, 48 h, 72 h and 96 h after HFNC therapy or NIV therapy initiation. The variables assessed included age, weight, sex, comorbidities, previous respiratory hospitalization, the Pediatric Index of Mortality – version 2 (PIM 2) score, viral panel results, the need for antibiotics, nasal septum injury status, sedative usage, HFNC/NIV duration, invasive mechanical ventilation duration, PICU length of stay (LOS), the hospital LOS, and the mortality rate [22,23,24].
The Comfort behavior scale (Comfort-B) and Richmond Agitation-Sedation Scale (RASS) were standardized scales for sedative adjustments. The drugs administered for this purpose were dexmedetomidine, ketamine, lorazepam, methadone, and clonidine [25, 26]. The Fischer scale was applied daily to evaluate nasal septum injuries [27].
Early enteral feeding initiation was recommended and depended on the clinician’s judgment. Oral food (liquid or solid) intake was permitted in the HFNC group, particularly during treatment weaning, and its initiation was allowed depending on respiratory distress status. For patients on NIV, an enteral diet was mandatorily provided through nasogastric or orogastric tubes.
Viral panel analysis was carried out through quantitative reverse transcription polymerase chain reaction (RT‒qPCR) in partnership with the Institute of Biomedical Sciences II at the University of São Paulo. The samples were collected during emergency department or PICU admission, and the following viruses were detected: respiratory syncytial virus, human metapneumovirus, influenza virus (IA and IB), parainfluenza virus 1, 2, 3 and 4, seasonal coronaviruses (types OC43, HKU1, NL63 and 229E), human adenovirus, human enterovirus, human rhinovirus, SARS-CoV-2 and human bocavirus.
The criteria for indicating HFNC/NIV therapy failure and the need for mechanical ventilation were signs of severe respiratory distress (WDF score of 8 to 14 points), a respiratory rate > 60 bpm (in children up to 1 year old) or > 40 bpm (in children aged 1 to 2 years), or a heart rate > 160 bpm. For this study, crossover was not allowed, and patients who experienced therapy failure were intubated. Although the intervention could not be masked, all the investigators remained unaware of the partial results. For patients who experienced respiratory improvement, an HFNC weaning protocol was administered according to the institutional protocol. NIV weaning was carried out according to daily reassessments and clinical judgment.
The primary outcome was the need for invasive mechanical ventilation. The secondary outcomes analyzed were sedation usage, invasive mechanical ventilation duration, the PICU LOS, the hospital LOS, and the mortality rate.
The hospital’s epidemiological data and the reasons for hospitalization classified by the International Classification of Diseases (ICD-10 J21 – acute bronchiolitis) recorded at admission were retrospectively collected from the patients’ electronic medical records. The purpose was to determine the fraction of study participants, the primary reason for intensive care and the need for invasive mechanical ventilation. Data on the enteral feeding duration and antibiotic administration were also obtained retrospectively.
Statistical analysis
This was an open-label and randomized study. Randomization was carried out using sealed envelopes. The sample size was calculated based on a pilot study carried out in Brazil. Considering the success rate, 252 patients (126 in each group) were needed to exclude a difference of more than 15% with a certainty of 80% in favor of the CPAP group [28]. To determine noninferiority, the Farrington-Manning test was applied to calculate the difference in success rates with a 95% confidence interval for the primary outcome. The Farrington-Manning method for rate differences tests the null hypothesis of H0: p1−p2=δ. The rejection of the null hypothesis allows the conclusion that the rate of success in group one is at least the rate of success in group two plus the delta value [29]. We established a delta value of 15%, which is arbitrary but has been used in the literature [12]. To compare distributions between groups, the Wilcoxon/Mann‒Whitney test was used, and the chi‒square test was used to compare frequencies between groups. The cumulative probabilities of “surviving” without the need for intubation over the time of observation were compared using the log rank test. To compare repeated measurements, we used the Friedman test, with post hoc analysis by the Wilcoxon paired test (signed rank), with Bonferroni correction. The magnitude of the effect of HFNC therapy and NIV on vital parameters was assessed using Cohen’s “d” test (Cohen’s d). The interpretation of Cohen’s d is as follows: small effect (d: 0.2 - <0.5), moderate effect (d = 0.5 - <0.8) and large effect (d ≥ 0.8) [30]. The statistical analyses were performed using R: A language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria) [31].
The interrater reliability of the WDF score was not evaluated. The standard method was applied for missing data, which is the analysis of complete cases not using any replacement or imputation technique [32]. The percentages of missing data for each period were as follows: 0 h (0), 2 h (0.5%), 6 h (0.4%), 12 h (1.2%), 24 h (0.9%), 48 h (0.4%), 72 h (0.8%) and 96 h (0). Missing data occurred as a result of incomplete forms. The CONSORT guidelines for reporting randomized trials in journals and abstracts were applied for text structuring [33, 34].
Results
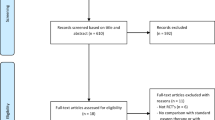
A total of 132 patients were randomized to the NIV group, and 136 patients were randomized to the HFNC group. Of these, six patients were excluded from the NIV group, and 10 were excluded from the HFNC group, totaling 126 patients in the NIV group and 126 patients in the HFNC group. The reasons for exclusion were failure to fully comply with the protocol, a diagnosis of heart disease with hemodynamic repercussions during hospitalization, external transfer, a lack of written informed consent, and a positive viral panel result for SARS-CoV-2. Figure 1 shows the study flowchart for the period between February 2021 and May 2023.
During this period, 1007 patients were admitted to the hospital for bronchiolitis. Of these patients, 649 (64%) were transferred to the PICU, and 146 (22%) required invasive mechanical ventilation. For the analyzed patients, nine (7%) patients in the HFNC group and three (2%) patients in the NIV group were weaned from respiratory support in the emergency room and were not transferred to the PICU. One patient from the NIV group and three patients from the HFNC group were transferred to another hospital after protocol finalization (respiratory failure and invasive mechanical ventilation requirement). Their collected data were used only for the primary outcome analysis.
The demographic data and other relevant characteristics are described in Table 1.
Thirty-seven patients in the NIV group were intubated (29%), and 29 patients in the HFNC group were intubated (23%, p = 0.25). According to the Farrington-Manning test, within the noninferiority margin of 15%, the difference was 6.3% in favor of HFNC therapy (95% confidence interval: -4.5 to 17.1%, p < 0.0001). Most of the intubations occurred within the first 24 h after starting NIV or HFNC therapy: 62% in the NIV group and 72% in the HFNC group. According to the log rank test, the cumulative probabilities of intubation were similar during the observation period (p = 0.33). The device settings along the time points are shown in Fig. 2.
The mean values of the devices used for NIV and HFNC therapy. The p values refer to observed differences between FiO2 utilized in the NIV and HFNC groups at the time points (hours). IPAP: Inspiratory positive airway pressure; EPAP: Expiratory positive airway pressure. FiO2: Fraction of inspired oxygen
Both NIV and HFNC therapy promoted a reduction in heart and respiratory rates and, consequently, in the WDF score. For the consecutive heart rate measurements in the NIV group, the Friedman p value was < 0.0001. The most pronounced effect on the reduction in the heart rate was observed when comparing the 12-h measurement with the measurement at the beginning of therapy: Cohen’s d was estimated to be -1,1 (95% CI -1.38 to -0.82; large effect). The p value obtained by the Wilcoxon paired test was < 0.0001. In the HFNC group, a greater effect was also observed when comparing the heart rate at 12-h with the initial heart rate: Cohen’s d was − 0.86 (95% CI -1.14 to -0.58 - large effect; p < 0.0001).
The reduction in the respiratory rate in the NIV group was also significant (p < 0.0001). A larger effect was estimated when comparing the 24-h measurement and the initial measurement. Cohen’s d was − 1.04 (95% CI -1.36 to -0.73 - large effect; p < 0.0001). In the HFNC group, the most pronounced effect was observed when comparing the 72-h measurement with the initial measurement: Cohen’s d was − 1.1 (95% CI -1.44 to -0.75 - large effect; p < 0.0001).
The WDF score decreased markedly in the NIV group during the first two hours of therapy: Cohen’s d was − 0.84 (95% CI -1.1 to -0.57 – large effect; p < 0.0001). Comparing the 48-h measurements with the initial measurements, Cohen’s d was − 2.27 (95% CI -2.7 to -1.8 – large effect, p < 0.0001). In the HFNC group, Cohen’s d was estimated to be -0.72 for the first two hours (-0.99 to – 0.47 – medium effect; p < 0.0001). A larger effect was observed when comparing the 72-h and initial measurements (Cohen’s d -2.15, 95% CI -2.6 to -1.74, p < 0.0001).
The pulse oximetry saturation/fraction of inspired oxygen ratio (SpO2/FiO2) increased slowly in both groups. The Friedman p value was < 0.0001 for all measurements. The effect in the first two hours was negligible for the NIV and HFNC groups. In the NIV group, a greater effect was observed when comparing the 72-h measurement and the initial measurement (Cohen’s d 1.7; 95% CI 1.15–2.2 – large effect, p < 0.0001). In the HFNC group, the most pronounced effect was also observed when comparing the initial and 72-hour measurements; Cohen’s d was estimated to be 1.54 (95% CI 1.17–1.91, large effect, p < 0.0001). These measurements and effects are illustrated in Fig. 3.
There were no patients with nasal pressure injuries in the HFNC group. In the NIV group, 11 patients presented with nasal trauma (Fischer stage 1 or 2).
Discussion
In our study, we analyzed young and eutrophic infants who were admitted for bronchiolitis, the vast majority of whom were admitted during their first wheezing episode and had respiratory syncytial virus isolated from a viral panel. This population portrays classic bronchiolitis without risk factors, such as prematurity and cardiopathies [10, 11, 35].
Although the therapy duration was significantly longer in the HFNC group [77.5 (46.5–108) versus 48 (24–78) hours, p = 0,0003], this finding does not seem to have influenced the PICU LOS or hospital LOS. We could not assess if the establishment of a HFNC weaning protocol directly impacted the longer duration of therapy.
In our study, although the sedation duration was similar between the groups, the percentage of patients who required pharmacological measures was significantly greater in the NIV group [121 (96%) versus 54 (42,8%) patients, p < 0.001]. Moreover, children receiving NIV had a greater incidence of nasal injury. There are few studies comparing HFNC therapy and NIV that have used the need for sedation as an outcome. In a review published in 2015 by Hutchings et al., despite not finding an objective difference in patient comfort, nasal injury was significantly greater in the NIV group. Furthermore, for parents, HFNC therapy seems to increase the possibility of parent contact and interactions with children during treatment. In a study evaluating clinical practices related to HFNC therapy, only 6.5% of Brazilian pediatric intensivists affirmed that they frequently use sedatives for patients receiving HFNC therapy. Comfort and synchrony play a role in the NIV success rate, especially in the pediatric population, considering the particularities in children’s airway anatomy. At our institution, neurally adjusted ventilatory assistance (NAVA) was not available for this purpose. Furthermore, bronchiolitis, a lower respiratory tract disease characterized by a mixed pattern of restriction and obstruction, adequate air entry, may be further impaired in nonsedated and asynchronous patients [9, 36,37,38].
The enteral feeding duration was longer in the HFNC group than in the NIV group [3 (2–4) versus 4 (2–5) days, p = 0,012]. Although both groups demonstrated clinical improvement over time (considering vital signs and WDF score), this assessment was only carried out in the first 96 h of protocol initiation. After this period, we cannot assume whether the longer time in HFNC therapy may have impacted the longer time of enteral tube use. In addition, there were no well-defined protocol for starting or discontinuing enteral feeding.
The need for antibiotics was greater in the NIV group than in the HFNC group [62 (49%) versus 49 (38%) patients, p < 0.001]. Although these data alone are not objective, previous studies have demonstrated that bacterial coinfection and antibiotic therapy use are related to PICU admission and the need for mechanical ventilation in children with severe bronchiolitis. There are few publications evaluating the use of antibiotics and clinical outcomes in patients admitted for bronchiolitis who receive HFNC therapy. In these patients, antibiotic therapy does not seem to increase the need for mechanical ventilation. However, the analyses were heterogeneous and had many limitations. New studies with high-quality evidence are needed to evaluate this association. Patients on mechanical ventilation are prone to ventilator-associated pneumonia (VAP), one of the most common healthcare-associated infections in the PICU. Nevertheless, in our results ventilator-associated pneumonia (VAP) does not appear to be an influencing factor in this higher ATB requirement since the VAP incidence in both groups was similar [7, 39,40,41,42].
Another interesting finding was the persistently higher FiO2 demand in the NIV group to maintain an SpO2 between 94 and 99%. In our hospital, the use of nasal prongs in infants is the standard interface applied. One possibility for this occurrence is air leak pressure due to the use of prongs instead of masks, which can lead to alveolar opening impairment. Furthermore, agitation and NIV asynchrony could contribute to higher FiO2 values. We cannot assume that lower target SpO2 levels could influence this difference. Currently, lower SpO2 thresholds are considered safe for some specific populations. However, for critical bronchiolitis patients who progress to respiratory failure, a well-established SpO2 threshold has not yet been defined [6, 21, 43, 44].
All four clinical markers evaluated (heart rate, respiratory rate, WDF score and SpO2/FiO2) demonstrated significant variations in both groups throughout the period analyzed. Among these markers, the WDF score showed the earliest variation (2 h after protocol initiation), followed by the heart rate and respiratory rate. The SpO2/FiO2 ratio exhibited the slowest variation. The WDF score was developed in the 1970s to evaluate asthma status and began to be applied in cases of bronchiolitis. According to our analysis, WDF score improvement seemed to occur earlier than did the other variables analyzed. This may have been because the isolated analyses of the heart rate, the respiratory rate and SpO2/FiO2 are nonspecific and can suffer some interference from a series of factors, such as fever, the use of sedatives (such as dexmedetomidine), crying and sepsis [19, 20]. Respiratory failure is classically classified into hypoxemic (tipe 1) or hypercapnic failure (tipe 2). For this definition, arterial blood gas sample may be required and could be a challenge, considering children’s anatomy and the risk of respiratory deterioration in case of agitation during the procedure. Thence, in pediatric clinical practice, the standardization of non-invasive scores with high predictive value for respiratory failure has been encouraged by current guidelines to make continuous patient assessment more objective. There are several scores published in the literature that are applied to this aim. However, few of these methods have been widely validated. In a systematic review that evaluated 32 scales for assessing bronchiolitis severity, WDF score was among the 6 considered the best available instrument. For this classification the following criteria were accounted: instrument’s items origin, assessment by the instrument’s items of endorsement frequency, reliability, validity, usability, and responsiveness. In a recent prospective observational study comparing 9 severity scales for bronchiolitis, WDF was one of them applied. The authors did not find a significant accuracy difference between them for access bronchiolitis severity respiratory status. Furthermore, in our research, we also pondered the fact that this scale was familiar to some professionals prior to protocol initiation [7, 45,46,47].
The PICU LOS was similar between the groups. However, the hospital LOS and duration of mechanical ventilation were shorter in the HFNC group. Some factors may have contributed to a longer hospital stay in the NIV group: absence of a specific weaning protocol, greater use of sedation and consequently increased risk of withdrawal and delirium syndrome and, although not significant, the mean duration of mechanical ventilation in patients who failed NIV was slightly higher, which may have contributed to a longer hospital stay. The degree of respiratory distress at the beginning of the protocol was similar between groups and does not appear to have influenced the outcome.
According to our protocol, all patients who received HFNC therapy or NIV were transferred to the PICU. Only a small percentage of patients completed the protocol in the emergency room while a PICU bed was not available. In some centers, HFNC therapy has been administered in emergency and pediatric wards. Nonetheless, in our study, PICU requirements could not be compared.
Another important question concerns the cost of hospitalization. Since our internal electronic system did not allow the individualization of all expenses per patient, it was not possible to carry out this analysis between groups. However, because we observed a shorter hospital LOS, less sedative administration, a lower rate of nasal injury, and a shorter duration of mechanical ventilation in the HFNC group, we may infer that these findings could contribute to reducing patient-related costs.
Finally, in our analysis, we were able to conclude that HFNC therapy is no less effective than NIV in mild or moderate bronchiolitis. To our knowledge, most of the published observational studies, clinical trials and meta-analyses of HFNC therapy and NIV (CPAP/BiPAP) have compared the superiority of one therapy over the other; the results are divergent or inconclusive, and the studies have several limitations [14,15,16, 18, 48, 49]. However, it is worth noting that the nonsignificance in traditional testing does not support the nondifference conclusion. For this purpose, noninferiority studies and, more specifically, equivalence trials should be performed. Nonetheless, to carry out equivalence studies, the necessary sample size is generally large, which can limit and extend the research. In this way, noninferiority trials have gained relevance by contributing to the understanding of comparative analysis. Furthermore, it is important to highlight that once noninferiority is significantly demonstrated, the secondary outcomes and benefits of HFNC therapy, such as better tolerability, less sedative usage, and easier handling and application outside the PICU ward, gain more relevance [50].
In a recent review published about HFNC therapy for bronchiolitis, the authors concluded that more studies comparing HFNC therapy and NIV are necessary. The Pediatric Acute Lung Injury Consensus Conference (PALICC-2) also recommends further studies to elucidate the importance of HFNC therapy in the management of respiratory distress syndrome in children. It is notable to reinforce that our results were found in patients with mild to moderate respiratory distress. Those patients who presented with severe bronchiolitis and evidence of acute respiratory distress syndrome (ARDS) could initially benefit from end-expiratory pressure (EPAP) and were excluded from randomization. Despite that consideration, we assume that our results can contribute to the understanding of therapy adjustment in cases of bronchiolitis that progress to respiratory failure [6, 18].
This study has several limitations: it was carried out in a single center and had a small sample size. It was not possible to blind patients or researchers. The hospital is primarily a teaching institution with 24-h resident coverage led by staff in the emergency department and PICU. The initiation of HFNC/NIV therapy was determined by clinicians, and children who were admitted for severe respiratory distress were not randomized. Only failure criteria were established. There was no specific protocol for NIV weaning, only for HFNC weaning. NIV asynchrony was not evaluated and might have influenced sedation requirement as well as the respiratory failure rate. Furthermore, crossover was not allowed, and no other ventilatory therapy support was provided (e.g., NIV in the case of HFNC therapy failure) before intubation. Extubation failure was not evaluated. Several risk factors for intubation and ICU admission (blood gas analysis, radiological changes, vasoactive drugs, bacterial coinfection, and fluid overload) were not evaluated. In addition, this research was initiated during the coronavirus disease 2019 pandemic, a period in which viral circulation and clinical presentation changed. Therefore, it is not possible to say thus far whether these findings will be only isolated points or trends. We cannot assess the cost-effectiveness of both modalities of respiratory support. Usually, HFNC therapy itself is more expensive than NIV, which may impair its application, especially in low-income countries [38, 51, 52].
Nevertheless, the population analyzed reflects the majority of patients treated in clinical practice—infants under 2 years old admitted to emergency and PICU departments with no comorbidities and a positive panel result for respiratory syncytial virus—which makes its external validation possible. In addition, the rate of therapy failure and need for invasive mechanical ventilation were similar to those in previous publications. Considering state-of-the-art HFNC therapy for bronchiolitis, our study can clarify its clinical applicability in the pediatric population [48].
Conclusion
HFNC therapy is noninferior to NIV in infants admitted for bronchiolitis in mild to moderate respiratory distress. This therapy could also contribute to a shorter duration of mechanical ventilation, a shorter hospital LOS, and a reduced need for sedatives.
Data availability
Santos, ACEZ (Forthcoming 2024). “Comparison between high-flow nasal cannula (HFNC) therapy and noninvasive ventilation (NIV) in children with acute respiratory failure by bronchiolitis: Dataset from a randomized controlled trial” [Dataset]. Dryad. https://doi.org/10.5061/dryad.4xgxd25jh [53]
Abbreviations
- BiPAP:
-
Bilevel positive airway pressure
- CI:
-
Confidence interval
- Comfort-B:
-
Comfort behavior scale
- CPAP:
-
Continuous positive airway pressure
- EPAP:
-
Expiratory positive airway pressure
- FiO2 :
-
Fraction of inspired oxygen
- HFNC:
-
High-flow nasal cannula
- HMIMJ:
-
Hospital Municipal Infantil Menino Jesus
- ICD:
-
International classification of diseases
- IPAP:
-
Inspiratory positive airway pressure
- IRB:
-
Institutional review board
- LOS:
-
Length of stay
- MV:
-
Mechanical ventilation
- NAVA:
-
Neurally adjusted ventilatory assistance
- NIV:
-
Noninvasive mechanical ventilation
- PALICC:
-
Pediatric Acute Lung Injury Consensus Conference
- PICU:
-
Pediatric intensive care unit
- PIM:
-
Pediatric index of mortality
- RASS:
-
Richmond agitation-sedation scale
- ROX:
-
Respiratory oxygenation
- RT-qPCR:
-
Quantitative reverse transcription polymerase chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SpO2 :
-
Peripheral oxygen saturation
- US:
-
United States
- VAP:
-
Ventilator-associated pneumonia
- WDF:
-
Wood-Downes-Férres score
References
Slain KN, Shein SL, Rotta AT. The use of high-flow nasal cannula in the pediatric emergency department. J Pediatr (Rio J). 2017. https://doi.org/10.1016/j.jped.2017.06.006.
Hough JL, Pham TM, Schibler A. Physiologic effect of high-flow nasal cannula in infants with bronchiolitis. Pediatr Crit Care Med. 2014. https://doi.org/10.1097/PCC.0000000000000112.
Pham TM, O’Malley L, Mayfield S, Martin S, Schibler A. The effect of high flow nasal cannula therapy on the work of breathing in infants with bronchiolitis. Pediatr Pulmonol. 2015. https://doi.org/10.1002/ppul.23060.
Guglielmo RD, Hotz JC, Ross PA, Deakers TW, Diep JEL, Newth CJL, et al. High-flow nasal cannula reduces effort of breathing but not consistently via positive end-expiratory pressure. Chest. 2022. https://doi.org/10.1016/j.chest.2022.03.008.
Rotta AT, Rehder KJ. Toward elucidating the mechanism of action of high-flow nasal cannula support in children. Chest. 2022. https://doi.org/10.1016/j.chest.2022.04.010.
Carroll CL, Napolitano N, Pons-Òdena M, Iyer NP, Korang SK, Essouri S et al. Noninvasive respiratory support for pediatric acute respiratory distress syndrome: from the Second Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2023; https://doi.org/10.1097/PCC.0000000000003165
Milési C, Baudin F, Durand P, Emeriaud G, Essouri S, Pouyau R, et al. Clinical practice guidelines: management of severe bronchiolitis in infants under 12 months old admitted to a pediatric critical care unit. Intensive Care Med. 2023. https://doi.org/10.1007/s00134-022-06918-4.
National Institute for Health and Care Excellence. Bronchiolitis in children: diagnosis and management. 2021. https://www.nice.org.uk/guidance/ng9/chapter/1-Recommendations. Accessed 25 Mar 2024.
Mikalsen IB, Davis P, Øymar K. High flow nasal cannula in children: a literature review. Scand J Trauma Resusc Emerg Med. 2016. https://doi.org/10.1186/s13049-016-0278-4.
Pelletier JH, Au AK, Fuhrman D, Clark RSB, Horvat C. Trends in bronchiolitis ICU admissions and ventilation practices: 2010–2019. Pediatrics. 2021. https://doi.org/10.1542/peds.2020-039115.
Fujiogi M, Goto T, Yasunaga H, Fujishiro J, Mansbach JM, Camargo CA, et al. Trends in bronchiolitis hospitalizations in the United States: 2000–2016. Pediatrics. 2019. https://doi.org/10.1542/peds.2019-2614.
Milési C, Essouri S, Pouyau R, Liet JM, Afanetti M, Portefaix A, et al. High flow nasal cannula (HFNC) versus nasal continuous positive airway pressure (nCPAP) for the initial respiratory management of acute viral bronchiolitis in young infants: a multicenter randomized controlled trial (TRAMONTANE study). Intensive Care Med. 2017. https://doi.org/10.1007/s00134-016-4617-8.
Franklin D, Babl FE, Schlapbach LJ, Oakley E, Craig S, Neutze J, et al. A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med. 2018. https://doi.org/10.1056/NEJMoa1714855.
Zhong Z, Zhao L, Zhao Y, Xia S. Comparison of high flow nasal cannula and non-invasive positive pressure ventilation in children with bronchiolitis: a meta-analysis of randomized controlled trials. Front Pediatr. 2022. https://doi.org/10.3389/fped.2022.947667.
Lin J, Zhang Y, Xiong L, Liu S, Gong C, Dai J. High-flow nasal cannula therapy for children with bronchiolitis: a systematic review and meta-analysis. Arch Dis Child. 2019. https://doi.org/10.1136/archdischild-2018-315846.
Vahlkvist S, Jürgensen L, la Cour A, Markoew S, Petersen TH, Kofoed PE. High flow nasal cannula and continuous positive airway pressure therapy in treatment of viral bronchiolitis: a randomized clinical trial. Eur J Pediatr. 2020. https://doi.org/10.1007/s00431-019-03533-2.
Dafydd C, Saunders BJ, Kotecha SJ, Edwards MO. Efficacy and safety of high flow nasal oxygen for children with bronchiolitis: systematic review and meta-analysis. BMJ Open Respir Res. 2021. https://doi.org/10.1136/bmjresp-2020-000844.
Armarego M, Forde H, Wills K, Beggs SA. High-flow nasal cannula therapy for infants with bronchiolitis. Cochrane Database Syst Rev. 2024. https://doi.org/10.1002/14651858.CD009609.pub3.
Wood DW, Downes JJ, Lecks HI. A clinical scoring system for the diagnosis of respiratory failure. Preliminary report on childhood status asthmaticus. Am J Dis Child. 1972. https://doi.org/10.1001/archpedi.1972.02110090097011.
Rivas-Juesas C, Rius Peris JM, García AL, Madramany AA, Peris MG, Álvarez LV, et al. A comparison of two clinical scores for bronchiolitis. A multicentre and prospective study conducted in hospitalised infants. Allergol Immunopathol (Madr). 2018. https://doi.org/10.1016/j.aller.2017.01.012.
Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014. https://doi.org/10.1542/peds.2014-2742.
Roca O, Messika J, Caralt B, García-de-Acilu M, Sztrymf B, Ricard JD, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016. https://doi.org/10.1016/j.jcrc.2016.05.022.
Roca O, Caralt B, Messika J, Samper M, Sztrymf B, Hernández G, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019. https://doi.org/10.1164/rccm.201803-0589OC.
Slater A, Shann F, Pearson G, Group PIoMPS. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003. https://doi.org/10.1007/s00134-002-1601-2.
Ista E, van Dijk M, Tibboel D, de Hoog M. Assessment of sedation levels in pediatric intensive care patients can be improved by using the COMFORT behavior scale. Pediatr Crit Care Med. 2005. https://doi.org/10.1097/01.PCC.0000149318.40279.1A.
Kerson AG, DeMaria R, Mauer E, Joyce C, Gerber LM, Greenwald BM, et al. Validity of the Richmond agitation-sedation scale (RASS) in critically ill children. J Intensive Care. 2016. https://doi.org/10.1186/s40560-016-0189-5.
Fischer C, Bertelle V, Hohlfeld J, Forcada-Guex M, Stadelmann-Diaw C, Tolsa JF. Nasal trauma due to continuous positive airway pressure in neonates. Arch Dis Child Fetal Neonatal Ed. 2010. https://doi.org/10.1136/adc.2009.179416.
Cesar RG, Bispo BRP, Felix PHCA, Modolo MCC, Souza AAF, Horigoshi NK, et al. High-flow nasal cannula versus continuous positive airway pressure in critical bronchiolitis: a Randomized Controlled Pilot. J Pediatr Intensive Care. 2020. https://doi.org/10.1055/s-0040-1709656.
Farrington CP, Manning G. Test statistics and sample size formulae for comparative binomial trials with null hypothesis of non-zero risk difference or non-unity relative risk. Stat Med. 1990. https://doi.org/10.1002/sim.4780091208.
Tomczak ATE. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. 2014;1:19–25.
R Foundation for Statistical Computing. 2020. https://www.r-project.org/about.html. Accessed 20 Jul 2020.
Karahalios A, Baglietto L, Carlin JB, English DR, Simpson JA. A review of the reporting and handling of missing data in cohort studies with repeated assessment of exposure measures. BMC Med Res Methodol. 2012. https://doi.org/10.1186/1471-2288-12-96.
Hopewell S, Clarke M, Moher D, Wager E, Middleton P, Altman DG, et al. CONSORT for reporting randomised trials in journal and conference abstracts. Lancet. 2008. https://doi.org/10.1016/S0140-6736(07)61835-2.
Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010. https://doi.org/10.1136/bmj.c332.
Sociedade Brasileira de Pediatria. Diretrizes para o manejo da infecção causada pelo vírus sincicial respiratório (VRS). 2017. http://www.sbp.com.br/fileadmin/user_upload/Diretrizes_manejo_infeccao_causada_VSR2017.pdf. Accessed 18 Nov 2020.
Cammarota G, Simonte R, De Robertis E. Comfort during non-invasive ventilation. Front Med (Lausanne). 2022. https://doi.org/10.3389/fmed.2022.874250.
Colleti Júnior J, Kawaguchi A, Araujo OR, Garros D. Clinical practices related to high-flow nasal cannulas in pediatric critical care in Brazil compared to other countries: a Brazilian survey. Rev Bras Ter Intensiva. 2021. https://doi.org/10.5935/0103-507X.20210055.
De Luca D, Pezza L, Vivalda L, Di Nardo M, Lepainteur M, Baraldi E, et al. Critical care of severe bronchiolitis during shortage of ICU resources. EClinicalMedicine. 2024. https://doi.org/10.1016/j.eclinm.2024.102450.
Marlow RK, Brouillette S, Williams V, Lenihan A, Nemec N, Lukowski JD, et al. Risk factors associated with mechanical ventilation in critical bronchiolitis. Child (Basel). 2021. https://doi.org/10.3390/children8111035.
Guitart C, Alejandre C, Bobillo-Perez S, Girona-Alarcon M, Sole-Ribalta A, Cambra FJ, et al. Risk factors and incidence of invasive bacterial infection in severe bronchiolitis: the RICOIB prospective study. BMC Pediatr. 2022. https://doi.org/10.1186/s12887-022-03206-4.
Lewis L, Fernandes R, Kapitein B, Davies J, Holden J, Messahel S, et al. Predicting failure of high flow nasal cannula in bronchiolitis: a systematic review. Eur Respir J. 2019. https://doi.org/10.1183/13993003.congress-2019.PA1005.
Antalová N, Klučka J, Říhová M, Poláčková S, Pokorná A, Štourač P. Ventilator-associated pneumonia prevention in pediatric patients: narrative review. Child (Basel). 2022. https://doi.org/10.3390/children9101540.
Shein SL, Karsies T. Conservative versus liberal oxygenation targets for children admitted to PICU. Lancet. 2024. https://doi.org/10.1016/S0140-6736(23)02301-2.
Peters MJ, Gould DW, Ray S, Thomas K, Chang I, Orzol M, et al. Conservative versus liberal oxygenation targets in critically ill children (Oxy-PICU): a UK Multicentre, open, parallel-group, randomised clinical trial. Lancet. 2024. https://doi.org/10.1016/S0140-6736(23)01968-2.
Caballero MT, Polack FP, Stein RT. Viral bronchiolitis in young infants: new perspectives for management and treatment. J Pediatr (Rio J). 2017. https://doi.org/10.1016/j.jped.2017.07.003.
Granda E, Urbano M, Andrés P, Corchete M, Cano A, Velasco R. Comparison of severity scales for acute bronchiolitis in real clinical practice. Eur J Pediatr. 2023. https://doi.org/10.1007/s00431-023-04840-5.
Rodriguez-Martinez CE, Sossa-Briceño MP, Nino G. Systematic review of instruments aimed at evaluating the severity of bronchiolitis. Paediatr Respir Rev. 2018. https://doi.org/10.1016/j.prrv.2016.12.006.
Clayton JA, McKee B, Slain KN, Rotta AT, Shein SL. Outcomes of children with bronchiolitis treated with high-flow nasal cannula or noninvasive positive pressure ventilation. Pediatr Crit Care Med. 2019. https://doi.org/10.1097/PCC.0000000000001798.
Borgi A, Louati A, Ghali N, Hajji A, Ayari A, Bouziri A, et al. High flow nasal cannula therapy versus continuous positive airway pressure and nasal positive pressure ventilation in infants with severe bronchiolitis: a randomized controlled trial. Pan Afr Med J. 2021. https://doi.org/10.11604/pamj.2021.40.133.30350.
Pinto VF. Non-inferiority clinical trials: concepts and issues. J Vasc Bras. 2010;9:145–51.
Rodríguez-Fernández R, González-Martínez F, Perez-Moreno J, González-Sánchez MI, de la Mata Navazo S, Del Toledo B, et al. Clinical phenotype of respiratory syncytial virus bronchiolitis before and during the coronavirus disease 2019 pandemic. Am J Perinatol. 2024. https://doi.org/10.1055/s-0042-1759602.
Bottau P, Liotti L, Laderchi E, Palpacelli A, Calamelli E, Colombo C, et al. Something is changing in viral infant bronchiolitis approach. Front Pediatr. 2022. https://doi.org/10.3389/fped.2022.865977.
Santos ACEZ. Forthcoming (2024). Comparison between high-flow nasal cannula (HFNC) therapy and noninvasive ventilation (NIV) in children with acute respiratory failure by bronchiolitis: Dataset from a randomized controlled trial [Dataset]. Dryad. https://doi.org/10.5061/dryad.4xgxd25jh
Funding
Fisher & Paykel provided the materials and equipment. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
ACEZS was the principal and corresponding author and contributed to the design, analysis, interpretation of data and drafted the submitted version. CMC, AGDL, GCF, AKAE, and DBLO contributed to the acquisition data. ORA contributed to the analysis and interpretation of data. WBC contributed to the design, analysis, and interpretation of data. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent was obtained from a parent and/or legal guardian. This study was approved by the Institutional Review Board (IRB) of the hospital (Hospital Municipal Infantil Menino Jesus Research Ethics Committee; approval number 39509820.0.0000.5639, 11/24/2020).
Consent for publication
Written informed consent was obtained from a parent and/or legal guardian before the data were collected by the physician responsible for starting the protocol.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Santos, A.C.E., Caiado, C.M., Lopes, A.G. et al. “Comparison between high-flow nasal cannula (HFNC) therapy and noninvasive ventilation (NIV) in children with acute respiratory failure by bronchiolitis: a randomized controlled trial”. BMC Pediatr 24, 595 (2024). https://doi.org/10.1186/s12887-024-05058-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05058-6