Abstract
Aim
Functional Management and Recovery is a standardized Psychoeducational Intervention, derived from “Integro”, an effective salutogenic-psychoeducational intervention for people in recovery journey, designed to improve recovery and functioning of individuals with psychotic disorders in Psychiatric Residential Facilities (PRFs). The aim of this study is to evaluate the primary and secondary outcomes of this intervention elaborated specifically for PRFs where evidence based structured interventions seem rare and desirable.
Methods
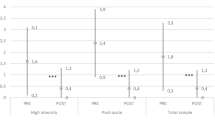
66 individuals with psychotic disorders were recruited in 9 PRFs dislocated in the North, Center and South Italy and 63 underwent a multicenter follow-up study with a two time-point evaluation (t0, pre-treatment and t1, 6 months; ). At each time point, social functioning was assessed as primary outcome by the Personal and Social Performance scale (PSP); furthermore, psychopathological status was assessed by Brief Psychiatric Rating Scale (BPRS), Recovery by Recovery Assessment Scale (RAS), Cognitive Functioning by Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), Stress management by Stress-Scale, Cognitive Flexibility by Modified Five-Point Test (M-FPT), Emotional Intelligence by Emotional Intelligence Index (EI-I), the PRF Atmosphere and the Opinion of users about the PFR by an ad hoc questionnaire. The Abilities Knowledge, the Utility and Pleasantness of sessions were measured by an ad hoc list of items.
Results
63 individuals out of 66, 52 (82,5%) affected by schizophrenia and 11 (17,5%) by bipolar I disorder with psychotic symptoms according to DSM-5-TR completed the study. At the end of the study, 43 (68,3%) were male, 57 (90.5%) were single, 5 (7.9%) engaged, 1 (1.6%) married; 45 (71.4%) unemployed. The total scores of PSP, RAS, BPRS, BANS, Stress management, Abilities Knowledge, Utility and Pleasantness of sessions showed a statistically significant improvement at t1 vs. t0. Two sub-scales out of 5 of M-FPT showed a statistically significant improvement. The Emotional Intelligence, the Unit Atmosphere and the Opinion of Users about PFR improved without statistical significance. Six months after the end of the follow-up study 22 individuals of the sample were dismissed with a very high turnover.
Conclusions
After a six-month follow-up (a short period of time), these results showed improvement in functioning, the primary outcome, as well as in the following secondary outcome variables: RAS, BPRS, BANS, Stress management, Abilities Knowledge, two sub-scales out of 5 of M-FPT, Utility and Pleasantness of sessions. Overall, a remarkable impact of psychoeducational structured intervention on the key Recovery variables is observed. Further studies are needed to address extent and duration of these improvements.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Psychiatric Residential Facilities (PRFs) play a relevant role in rehabilitation of individuals with Severe Mental Disorders and complex needs in Italy, covering 43.9% of the budget of a Mental Health Department [1]. A great number of beds in residential facilities has been reported in Italy since 2018 by Barbui et al. [2]; specifically, 46 per 100.000, surprisingly more than in England, where they are 10 per 100.000 (the 2 beds per 100.000 in English Psychiatric Hospitals do not compensate this difference). Nevertheless, PRFs have not received great attention in Italy, except for previous studies that thoroughly assessed the residential care system [3,4,5], and for few recent studies [6,7,8]. Despite several interventions, such as the Mental Health Budget, which was proposed by many regions and by the Government to overcome the residential approach [9], the beds raised from 46 in the 2018 [2] to 51.2 × 100.000 as recently reported [10]. The daily presence rates in PRFs in 2022 [1] were 10.919.751 for the 28.738 users (10.306 for the 27.813 in 2021; 11); the rate of accesses was 249 × 100.000 in 2022 (240 × 100.000 in 2021). Last year the Government entrusted a report about PRFs to the National Institute of Health [10]. In the introduction of this report, the length of stay of people admitted in PRFs is well underlined, so that PRFs often become “the house for life”! This is also the conclusion of the analytic investigation of Martinelli et al. [7]: “… the actual average length of stay was 2.9 years (SD 1.0), ranging from 2 to 6 years”.
Based on the Report of the National Institute of Health [10] and the results of Martinelli et al. [7], one critical point of this system of care is the lacking administration of evidence-based and recovery-oriented interventions. This may be true everywhere, as suggested by the conclusions of Killaspy et al. [12], underlining that discharge from PRFs is “facilitated by recovery-oriented practice that promotes service users’ activities and social skills”. This is a very important issue, but much more important, in our opinion, is the other conclusion by the same authors: “Further research is needed to identify effective interventions that enhance such practice to deliver these outcomes” [12]. In fact, in Italy there is a long tradition of providing a lot of activities in PRFs, as described in a recent survey [13]. For instance, cooking and gardening activities reached high percentages in all the facilities, respectively 55.6 and 55.2%, “due to the necessity to increase autonomy in patient’s everyday life”, followed by art therapies, representing 12.9% of the activities [13]. However, this tradition didn’t seem to bring a great contribution to reduce the length of stay in this kind of structures! Also, according to the conclusions of Killaspy et al. [12], we can note that only 13.8% of activities referred to evidence-based treatments, and that the percentage of evidence-based activities was similar among Italian facilities.
We believe that the under-provision of evidence-based treatments is a great issue; along with that, it is also important to consider what kind of treatment is really effective for people living in the PRFs. In our opinion, Killaspy et al. [12] hit the target in stating that research is needed for effective interventions that will improve good existing practice or activities to obtain better outcomes. Among other aims, an intervention must aim at reducing discrepancies of perceived needs between staff and users [8] as well as at better involving relatives in the process of care even if the user is admitted to PRFs, considering that involvement of relatives is about 50% [7]. Recovery-oriented interventions should feature the key-components for recovering, i.e. the effective evidence-based elements necessary to the recovery journey [14]. In addition to Killaspy et al. [12] statement and our previous considerations, the NICE Guidelines [15] ask “what structured group activities are effective at improving interpersonal functioning (social skills) for people with complex psychosis?” in the chapter “Recommendations for research”. In fact, the unique rehabilitative approach explicitly suggested by the Nice Guidelines is the Illness Management and Recovery (IMR; 17).
Bearing in mind all these aspects, a team specialized in providing effective psychoeducation interventions elaborated a new approach, specifically conceived for PRFs. This intervention is an adaptation to residential settings of an effective manualized psychoeducational and salutogenetic approach, named “InteGRO”, which was conceived to facilitate recovery in the community [17,18,19,20,21]. Whereas IMR (the manual most similar to InteGRO in several aspects, as described in Veltro et al.; 21) has a pathogenetic approach because of some components that refer to the nature of the disorder, InteGRO only concerns the improvement of abilities, including social cognition and mindfulness components. InteGRO is inspired to the principles of salutogenesis [22, 23], and to the aspect of “meaningfulness” above all, which we would like to pinpoint as the key element of recovery, as suggested with the locution “The sense of Meaning”, by Jaiswall et al. [14]. The intervention we propose shares with InteGRO the setting of pleasant and personal goals, communication skills, problem solving, emotional literacy, the principles of mindfulness and above all the salutogenic approach. This last-mentioned approach is important because it stresses the component of “meaningfulness” from the Antonovsky’s “triad” [22]. Furthermore positive psychology, which represents one of the basic foundations of the theory and practice of the salutogenesis, is also well considered. During the several meetings, individuals with mental disorders are guided to give meaning to the stressful events as challenges and, at same time, to see the experiences in a positive light. This action encourages them to commit and to adhere to the treatment in a satisfactory way. This intervention differs from “Integro” because it features a more intensive training (two meetings a week) on personal and social functioning, on reshaping negative thoughts and feelings in a positive way, on detection of early warning signs, on relaxation techniques and because it gives more importance to the other two components of the Antonovsky’s “triad”, that means “comprehensibility” and “manageability”. In addition, this intervention combines the traditional Social Skills Training aimed to the improvement of self-care or communication skills or problem-solving with the efforts to prompt life-style changes like diet, physical activity or relaxation self-training; this work is done by means of a specific schedule with the scores for the evaluation of progress, filled in during the group session. The intervention, which we called “Functional Management and Recovery (FMR)”, includes specific sessions with relatives and professionals of the facilities to share the work in progress. The stimulus to elaborate this intervention came from: (a) the lack of appropriate and specific interventions for PRFs as emerged by the Survey in Italy [13], as well as by the results of the contribution of Killaspy [12], also underlined by Nice Guidelines [15]; (b) the motivation and determination of many professionals trained in InteGRO in Italy to apply it also in the residential or semi-residential facilities, against the advice of the Authors. The last point is crucial, because we do not believe that an intervention, even if effective to facilitate recovery in the community, could be used in other settings, entirely or modified, simply based on “experience” or “knowledge” of some professionals. We believe that the appropriateness is a crucial aspect of a rehabilitation process. We had consistent feedback on this by the experience with a psychoeducational group intervention for acute inpatients [24], which some professionals tried to apply, unsuccessfully, in semi-residential facilities or low intensity residential settings. For all these reasons we elaborated this new approach, encouraged by the professionals of the Mental Health Department of Cuneo, who, enthusiastic of the previous InteGRO training, were interested in proving the effectiveness of this new intervention.
In this contribution we show the results of a multicenter study involving nine PRFs about the effectiveness at six months of the “FMR” intervention, with functioning as a primary outcome. Several other variables have been considered, concerning psychopathology, relapse, admission rates in psychiatric wards, discharge against the advice or shared with professionals, cognitive functions, including flexibility as a specific pattern, level of stress, settled personal goals and their achieving, atmosphere in the facilities.
Materials and methods
Study design
This is a multicenter observational study without a control group, with a 6 month follow-up, two time-point evaluation (t0 = pre-treatment; t1 = post-treatment, 6 months after the beginning of the treatment), carried out on personal and social functioning as the primary outcome; the study was conducted between 2022 and 2023 in individuals with DSM-5-TR [25] schizophrenia or bipolar I disorder with psychotic symptoms, enrolled in 9 intensive Psychiatric Residential Facilities (PRFs). There were no recruitment problems due to COVID-19 since the end of the pandemic state in Italy was decreed on April 1, 2022.
Sample and recruitment
Nine Italian PRFs, well-known to the Research Lead Unit of Cuneo for professional reasons, were selected and invited to take part in the study. In each of these PRFs, people with mental disorders who were clinically stable, without clinical worsening over the past 3 months, were invited to participate if they fulfilled the following inclusion criteria: (a) age between 18 and 55; (b) diagnosis of Schizophrenia or Bipolar disorder I with psychotic features according to the DSM-5-TR criteria; (c) a minimum of one year of duration of illness; (d) a minimum score on the Social and Personal Performance Scale of 35; (e) not Moderate, Severe or Profound Intellectual Developmental Disorder; (f) a minimum presence of 3 months in the PRF; (g) written informed consent to participate in the study and to be evaluated by means of interviews and questionnaires; (h) no current severe psychotic symptoms that could interfere with attention; (i) absence of use of drugs or intoxication by alcohol.
Individuals with mental disorders who agreed to participate in the study were consecutively allocated to the experimental group on the basis of their readiness to participate (up to 8); if the admitted eligible for the study were more than 8 they were allocated in a waiting list (up to 4 per center), receiving the intervention at the end of the study in case of positive results. The intervention was discontinued if the recruited individuals: (a) were unable to attend more than 4 sessions; or (b) were hospitalized for a period superior to one month or had 2 relapses or more during the study; or (c) withdrew their consent.

Description of the intervention
The experimental intervention is based on the psychoeducational and salutogenic intervention named “InteGRO”, developed by Veltro et al. [20] in order to facilitate recovery of people with severe psychiatric disorders. InteGRO has proved to be effective in several studies [21,22,23,24] for individuals with mental disorders who deliberately decide to undertake a recovery journey in the community, asking mental health service professionals to accompany them in this journey. InteGRO is based on four fundamental modules (definition of Pleasant and Life Goals, effective communication, emotional perception and problem-solving), each comprising different teaching units. For each unit a meeting is scheduled. There are also intermodular educational units to facilitate the acquisition of the skills of single modules. Emotional literacy, emotional perception, social cognition and problem solving are the most used training sessions of this approach. There are usually 36 weekly meetings, each one lasting 90 min; some of them are carried out twice a week to facilitate learning on the subject. InteGRO is a proactive and promotional intervention that focuses on the improvement of the abilities; there is no reference to symptoms, impairments or deficits. For the PRFs we re-elaborated InteGRO in order to intensify the work on personal and social functioning according to the main aim of promoting Recovery. In this way functioning became the most important aspect of the training. The FMR intervention involves 24 sessions, two per week (whereas InteGRO comprises 36 and 1 per week) with 3 meetings that require the presence of relatives and other professionals of the facility to inform them about the work in progress (units not present in InteGRO). For what concerns relatives, meetings are finalized to establish the possibility to do a family psychoeducation if this work has never been performed before, or how to proceed at home after discharge to help the person in achieving his/her goals. Training sessions not present in InteGRO are: (a) Early Warning Signs; (b) Structured Schedule to Help individuals with mental disorders to Plan Behavioural Changement; (c) Problem Solving training to facilitate the work on the Behavioural Changement Schedule (BCS); (d) 2 training sessions on the Albert Ellis’s ABC [26] model to help individuals reshape their negative thoughts and feelings in a positive way; (e) The modified Moritz Model [27] for empathy; (f) muscle relaxation training. The BCS represents the fundamental aspect of the work to improve functioning. This schedule contains the basic areas of functioning such as personal self-care, diet, sleep hygiene, motor activity, active mobility, relationships, hobbies and mastery. Each person with mental disorder would specify in two group sessions how he/she intends to work on each area and how to plan and to evaluate the progress in detail. All sessions of FMR and the BCS are illustrated in Appendix 1, 2 and 3. The intervention was carried out by mental health professionals who attended the training course. An ad-hoc manual was developed by the same team that developed InteGRO [20] in order to ensure treatment fidelity.
Training of mental health professionals in the intervention
The training intervention consisted of one residential meeting of 5 days, 8 h a day, carried out in a Residential Structure near Cuneo in order to: (a) inform professionals on the purposes and the methodology of the study; (b) train 2 professionals from each PRF in FMR; (c) train 2 researchers from each PRF on the assessment tools and test inter-rater reliability. In addition, we had five online supervision meetings, lasting 4 h; moreover, a regular phone and e-mail supervision was carried out. The mental health professionals who participated in the residential training were psychiatrists (10%), psychologists (23%), psycho-social rehabilitation technicians (10%), psychiatric nurses (21%), occupational therapists (8%), educators (23%), pedagogists (5%). All psychologists were trained in cognitive behavioral therapies. All psycho-social rehabilitation technicians were trained in Social Skills Training and psychoeducational intervention. All professionals had previously been fully trained in “InteGRO”.
Assessment instruments
The primary outcome of the study was the improvement of the personal and social functioning after the provision of the intervention at 6 months, assessed by the Personal and Social Performance Scale (PSPS; 29), derived from the version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS); compared to the SOFAS, the PSP has better face validity and psychometric properties. The PSPS evaluates personal and social functioning through a semi-structured interview and the information available from the acquaintances and health workers. There are four main areas: (1) socially useful activities (including working and studying); (2) personal and social relationships; (3) taking care of appearance and hygiene; (4) disturbing and aggressive behaviors. The total score ranges from 0 (worst possible functioning) to 100 (excellent functioning).
Other outcome measures were evaluated by means of:
-
The Recovery Assessment Scale (RAS; 30), one of the most used recovery measures in recovery-oriented practice evaluation for people with mental health conditions. Its psychometric properties have been extensively studied: it shows good reliability (i.e., internal consistency, test-retest reliability, interrater reliability), validity (i.e., consistent factor structures across different samples, expected associations with relevant constructs), and utility for intervention. It consists of five factors, corresponding to different features of the recovery processes: (1) personal confidence and hope; (2) willingness to ask for help; (3) goal and success orientation; (4) reliance on others; (5) no domination by symptoms.
-
The Italian version of Brief Psychiatric Rating Scale (BPRS; 31–33), a psychopathological hetero-evaluation scale consisting of 24 items. Each item is assessed on a Likert scale with 7 coding levels ranging from 1 (absent) to 7 (very severe). From a factorial analysis, five symptomatic clusters were identified: “disorganization” (range 4–28); “negative affectivity” (range 6–42); “positive symptoms” (range 4–28); “expanded affectivity” “negative symptoms” (range 3–21).
-
The Stress Scale [33], made up of 9 items taken from the well-known and widespread Goldberg tool for investigations in routine conditions, with a dichotomous yes-no (yes-score was considered equal 1, no-score was considered equal 2). The Cronbach’s alpha was evaluated at > .70 in all studies in which it was used. The test-retest reliability was assessed and met the criterion of > .70 in all cases. Two factor model best describes the scale: Perceived helplessness and Lack of self-efficacy.
-
The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS; 35): a brief, individually administered test measuring attention, language, visuospatial/constructional abilities, immediate and delayed memory. It consists of 12 subtests, which yield five Index scores and a Total Scale score. Stimuli are contained in a wire-bound, easel-type booklet, making the test easily portable. Clinical validity study of the RBANS suggests that it is sensitive both in terms of detecting and characterizing cognitive deficits.
-
The Modified Five-Point Test (M-FPT; 36) is a test for measuring non-verbal fluency (figurative) of executive functioning, linked to cognitive flexibility. The main aspects assessed are: cognitive flexibility, presence or absence of perseveration and strategic performance. Consequently, scores are of 3 types: (1) Unique Drawings (UDs), i.e. number of valid drawings not produced before; (2) Cumulative strategies (CSs) i.e. number of UDs produced with a particular strategy that can be either enumerating (CSse) or rotative (CSsr); (3) Error index (Errl), i.e. percentage of perseverative drawings or breaking of rules (errors) on the total number of drawings. The aim of the Italian validation study [35] was to collect normative data for a version of the Five-Point Test (M-FPT), which psychometric properties were well known from the original validation studies, administered to a sample of Italian healthy adults aged 16–60. The availability of these normative data allows one to assess individual’s performance with reference to cut-off scores.
-
The Emotional Intelligence Index (EI-I; 37) is a self-report questionnaire consisting of 15 items characterized by 5 factors as resulted by construct validity: intrapsychic, interpersonal, impulsivity, coping, self-efficacy with a total score ranging from 15 (absence) to 60 (the highest score). The cut-off for the presence of Emotional Intelligence is 22. The overall internal consistency of the Index assessed with Cronbach’s alpha was found to be 0.72. The concurrent validity was shown to be 0.74 (p < 0.01) with r²=0.55.
-
Psychiatric Residential Atmosphere Schedule (PRAS), is an ad hoc simple schedule adapted from the Ward Atmosphere for inpatients, which has shown good reproducibility results [37]: agreement exceeded 90% with a Cohen’s kappa > .70. It is filled twice a day (2 pm and 8 pm) by two professionals that work in the PRF in order to obtain a score about the atmosphere in the facility and also the presence of aggressive behavior. The score ranges from 1 (or white color) meaning no problem at all and also positive communication up to 5 (or red color), meaning that one or more individuals with mental disorders have destructive or violent or aggressive behavior. For each item well detailed scoring instructions are available.
-
The Patient Opinion about the PRF (POPReF), is an ad hoc list of items, adopted by the ABC questionnaire [38] that evaluates the opinion of people with mental disorders about the comfort in the facility, the availability and the kindness of professionals, the information provided about the illness, the drugs, the opinion about the quality of care and satisfaction about hospitality. The ABC questionnaire showed in the study of validation [38] good psychometric properties: test-retest (> .66); concurrent validity with the r’ Spearman correlation coefficients of 0.54 (p < .0001); internal consistency with the value of Cronbach’s alpha of 0.90; discriminant validity assessed by Kruskal-Wallis equal to 16.2 (p < .0001).
-
The Abilities Knowledge Schedule (AKS) is an ad hoc list of items that evaluate the Knowledge of ability to define goals (1 item, score 1 if the reply is good), communication skills (4 items, score 1 for each item if the replay was good) and problem solving (score one for each step if it has been considered in the solution of a problem) with scores ranging from 0 to 11. The score 6 is considered a good result.
-
Utility perception of the meeting was measured with a score ranging from 3 (Not at all) to 8 (very very much).
-
Pleasantness of the meeting was measured with a score ranging from 3 (Not at all) to 8 (very very much).
Statistical analysis
For all the variables with parametric distribution the average ± sd was calculated; for all variables with non-parametric distribution the median and range were calculated. The pre-post comparison of the variables with parametric distribution was performed by paired two-sample t-tests. For non-parametric distribution variables the Wilcoxon signed-rank test was performed. Pearson correlation coefficient or Spearman correlation coefficients were calculated for bivariate correlations between parametric and non-parametric variables, respectively. A forward stepwise linear regression was used to identify possible predictors of the primary outcome variable (PSP at t1) out of the psychopathological, recovery, Cognitive, Stress, Emotional Intelligence, Atmosphere, Opinion of users, Abilities Knowledge, Utility and Pleasantness variables. At each step, variables were chosen based on p-values (< 0.05). A similar forward stepwise linear regression analysis was carried on to identify possible predictors of Recovery as assessed by RAS at t1. The SPSS version 29.0.2.0 software for macOS (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp) was used for statistical analysis. All methods were carried out in accordance with relevant guidelines and regulations.
Human ethics and consent to participation declarations
Ethical approval of the experimental protocols
The study was conducted according to the Declaration of Helsinki. The protocol was submitted to and approved by the relevant ethical and review boards “Comitato Etico Interaziendale A. O. “Santa Croce e Carle di Cuneo AA.SS.LL. Cuneo 1, Cuneo 2, Asti, Via Monte Zovetto, 18–12100 CUNEO, reference “ASL CN1/PSICH. 4” (Report 75/22 of 27/04/2022; prot. n. of General Management Resolution Measure 01121153 of 09/09/2022). Prior to their participation in the study, all individuals were fully informed about the study scope, objectives, methodology, and components, and they provided written informed consent. They were also informed that their participation was voluntary and they could withdraw from the study at any time. Informed consent of the participants was obtained before the study.
Results
Recruitment process and attrition rate
All 9 centers contacted to participate to the study and run the intervention after training of mental health professionals. Each center was expected to recruit up to 8 individuals with mental disorders according to the criteria illustrated in the methodology. In 6 Centers the goal of 8 individuals recruited was achieved; in 3 centers there were 7 recruited people, for a total of 69. 3 people, 2 with schizophrenia and 1 with bipolar I disorder, refused to be evaluated and to participate before starting the study; the retention rate was 4.3%. The sample starting the study was 66 individuals. Other three left the study during the first month: one started to work, one left the PRF for another PRF and one left the PRF against the advice of clinicians. At the end of the study, total number of the sample was 63.
The socio‑demographic characteristics and diagnosis of the sample (Table 1)
The 66 individuals with mental disorders that started the study were: 46 (70%) male, 20 female (30%); 61 (92,4%) were single, 4 (6.1%) engaged; 1 (1.5%) married; 50 (76.7%) unemployed. 54 (81.8%) users were affected by schizophrenia, 12 (18,2%) by bipolar I disorder. At the end of the study, 43 (68,3%) were male, 57 (90.5%) were single, 5 (7.9%) engaged, 1 (1.6%) married; 45 (71.4%) unemployed. None of the study participants contracted COVID: mitigation recommendations were still in place inside the facilities and visitors were allowed to enter with a mask and with social distancing. No additional procedures were required for admissions and discharges due to Covid-19, except a swab upon admission.
The primary and secondary outcome of the sample and the statistical results (Table 2)
During the period of the 3 months before starting the study (T0) 5 admitted people (76%) had 5 admissions to hospital, 2 of them (40%) with a Compulsory Treatment Order (CTO). During the period of the 3 months before concluding the study (T1) 5 people had 5 admissions to hospital, 1 of them (20%) with a CTO.
During the six months after the t1 follow-up 22 (33,33%) people with mental disorders were discharged, 1 of them left the PRF against the advice of clinicians. At t0 2 individuals with mental disorders had a sheltered employment, while at t1 6 people did. At t0 there were no people with vocational training, whereas at t1 there was one.
PSP
At t0 the median was 52.50 (range = 35–65); at t1 it was 58.50; Wilcoxon signed-rank Test was significant (z = 4.653; p = .000).
The stepwise linear regression analysis was able to identify a significant final model (F(4,58) = 51.7; p < .001), which explained 76.6% of variance in PSP at t1. The model identified as predictors for PSP t1: the personal and social performance level at t0 (FPS t0: Beta = 0.711; t = 10.763; p < .001), item 22 “distractibility” from BPRS at t1 (Beta=-0.263; t=-4.220; p < .001), visuospatial and visuo-constructional abilities at RBANS (Beta = 0.181; t = 2.862; p = .006), number of voluntary admissions in a psychiatric ward during the year before the intervention (Beta=-0.150; t=-2.329; p = .023).
RAS
At t0 the average was 88.65 (sd: ±19.58); at t1 it was 94.84 (sd: ±22.32); Student’s t test was significant (T[62]=-3.086; p = .003). All subscale tests were significant. At subscale “Personal confidence and hope” at t0 the mean was 31.92 (sd: ±7.72), whereas at t1 it was 34.38 (sd: ±9.47); t[62]=-2.52; p = .014. At “No domination by symptoms” at t0 the mean was 9.57 (sd: ±3.28), at t1 it was 10.59 (sd: ±3.21); t[62]=-2.51; p = .015. At “Goal and success orientation” the median at t0 was 20.00 (range = 10–43), at t1 it was 20.50; Z = 3.58, p = .000. At “Reliance on others” the median at t0 was 14.00, at t1 it was 15.00; Z = 2.24; p = .025. At “Willingness to ask for help” at t0 the median was 12, at t1 was 12; Z = 2.33; p = .020.
The stepwise linear regression analysis was able to identify a significant final model (F(3,59) = 44.75; p < .001), which explained 67.9% of variance in RAS at t1. The model identified as predictors for RAS at t1: RAS level at t0 (Beta = 0.560; t = 7.275; p < .001); the emotional intelligence level (EI-I) at t1 (Beta = 0.349; t = 4.227; p < .001); the subjective experience of users in the PRF at t1(Beta = 0.177; t = 2.237; p = .029).
BPRS
At t0 the median was 43 (range = 28–82), at t1 was 39 [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]; Wilcoxon signed-rank Test was significant (Z=-4.87; p = .000).
RBANS
The total score median at t0 was 73 (range = 57–112), at t1 it was 74 (55–125); Wilcoxon signed-rank Test was significant (Z = 3.39; p = .001). Two subscales were significantly improved (“Immediate Memory” and “Delayed Memory”).
At subscale “Immediate Memory” the median at t0 was 75 (range = 40–126), at t1 it was 81 (40–129); Z = 2.92, p = .004. At “Delayed Memory” the median at T0 was 71.50 (range = 54–124), at T1 it was 75 (48–129); Z = 2.17, p = .030. At “Attention” the mean at t0 was 75.95 (sd: ±15.92), at t1 it was 77.87 (± 19.43); p = n.s. At “Language” the median at t0 was 77.50 (range = 61–102), at t1 it was 78 (62–115); p = n.s. At “Visuospatial/constructional abilities” the mean at t0 was 83.13 (sd: ±19.38) at t1 it was 86.48 (± 17.89); p = n.s.
STRESS scale
At t0 the median was 10.37 (range = 0–18), whereas at t1 it was 11 (0–18); Wilcoxon signed-rank Test was significant (Z=-2.84; p = .004).
M‑FPT
The UDs score showed a median at t0 of 0 (range = 0–3), whereas at t1 it was 1 (0–4); Wilcoxon signed-rank Test was significant (Z = 3.19; p = .001).
The ErrI score showed a median at t0 of 6.5 (range = 0–77), whereas at t1 it was 5 (0–50); p = n.s.
The Css score showed a median of 0 (range = 0–4) both at t0 and at t1; Wilcoxon signed-rank Test was significant (Z = 3.19; p = .046).
EI-I
At t0 the mean emotional intelligence was 41.51 (sd: ± 7.71), whereas at t1 it was 43.27 (± 8.08); p = n.s.
PRAS
The mean at t0 was 1.95 (sd: ± 0.79), whereas at t1 it was 2.01 (± 0.85); p = n.s.
POPReF
At t0 the mean was 62.98 (sd: ± 10.84), whereas at t1 it was 64.46 (± 10.39); p = n.s.
AKS
At t0 the median was 2.50 (range = 0–9), whereas at t1 it was 4.00 (0–11); Wilcoxon signed-rank Test was significant (Z = 4.79; p = .000).
Utility perception of the meeting
At t0 the mean was 6.0 (sd = ± 1.19), whereas at t1 it was 7.07 (sd = ± 1.40); Student’s t test was significant (T[62]=-4.07; p < .001)
Pleasantness of the meeting
At t0 the mean was 6.01 (sd = ± 1.25), whereas at t1 it was 6.85 (sd = ± 1.42); Student’s t test was significant (T[62]=-3.191; p = .001)
Discussion
To our knowledge, this is the first multicenter study testing the effectiveness of a psychoeducational recovery-oriented intervention, based on a salutogenic approach, with the explicit goal to improve personal and social functioning in the PRF. We observed a statistically significant improvement in the primary outcome (personal and social functioning) as well as in several secondary outcomes (Recovery; psychopathological status; Cognitive Functioning; stress management; Abilities Knowledge; Utility and Pleasantness of session). The Emotional Intelligence, the Unit Atmosphere and the Opinion of Users about PFR improved without statistical significance. Six months after the end of the follow-up study 22 individuals were dismissed with a very high turnover.
Most papers about PRFs are descriptive about the structures, the programs and the interventions or activities, often described, as if they were the same thing! Some papers explore the “quality” of the program [7] or the factors predicting discharge [39]. On the basis of the latest Italian survey [13], the evidence-based practice accounts for 13.8%, but as we wrote previously the question is: are the interventions usually applied in the community really effective in the PRF context, where social functioning and above all functional capacity are limited? In fact, the functioning capacity predicts the functioning of individuals with psychotic disorders as demonstrated by Galderisi et al. [40]. Nevertheless, the relevance of Cognitive Remedation generalizability to real-world functioning “should clearly be weighed against the context of care” as stated by Vita et al. [41]. For these reasons, our intervention, one of the first conceived on purpose to be appropriate for PRFs, seems interesting because the aim is to improve functioning in the PRF, where functioning in the real life is restricted. The only study that proposes the same type of intervention is Magliano et al. [42] called CIGI, “Combined Individual and Group Intervention”; the CIGI integrates the Vado Approach [43] with some parts (communication skills and problem solving) from the Falloon approach [44]. However, it does not appear comprehensive and its effectiveness on functioning seems discrete in the only study published [43].
The results of our study highlight a positive impact of the intervention on the majority of outcome indicators. Regarding the psychopathological component, it is worth recalling that the approach is not aimed at improving clinical symptoms, since pharmacological adherence is guaranteed 24/24 hours by professionals; the symptoms are stable and controlled by drugs. Nevertheless, in our study the post hoc comparison was significant, for BPRS total score at t1 vs. t0. Furthermore, the trend of clinical crises was better during the follow-up, as one CTO occurred compared with the two before the intervention; the same number of hospital admissions occurred. Some hospital admissions in the follow-up period could be explained by the potentially stressful intensity of this intervention (twice a week). Despite our beliefs, it has worked like a good investment in a longer period: in fact, we had a high percentage (33% of users) of discharged people at one year, whereas the PRF turnover in Italy is reported as not satisfactory [1].
The greatest impact of the intervention remains on personal and social functioning, the primary outcome, as predictable from the previous studies with the progenitor intervention “InteGRO” [18,19,20,21]. The variables predicting functioning at t1 are Social Functioning at t0, distractibility at t1, visuo-spatial abilities at t0, and admissions at t0. These results are very interesting, because in a complex network analysis on 921 individuals with psychotic disorders, Galderisi et al. [45] found that visuo-spatial learning and attention were directly connected with functional capacity. At the same time, it is not surprising that previous functioning is a predictive variable of the amelioration of personal and social functioning. For instance, social competence, more than social cognition, is directly linked to interpersonal functioning [40]. Based on these results, on data reported in specific literature and on the observations by the trainers of this intervention, the improvement on functioning may be due to:
-
a)
the work with the Behavioural Changement Schedule” (BCS) that commits the person to plan and evaluate the goals of changing in the most important components of personal and social functioning. Also prompting individuals to define Pleasant and Life Goals is probably linked to the improvement of functioning. This work is similar to the rehabilitation approach – effective and widespread in Italy - called “Vado” [46];
-
b)
the problem-solving training, the cognitive restructuring and the emotional literacy. The implementation of problem-solving strategies within psychoeducational interventions has an “impact on clinical and functional outcomes, by providing patients with long-lasting resources to manage daily life more effectively” [48]. In previous studies we discussed this and the relationship between cognitive functions, especially planning activity and Problem Solving [21], according to the theory about the Real World Problem Solving theory [21]. InteGRO and FMR dedicate many training sessions to emotional literacy and to recognizing the emotions on the other faces; in fact, the importance of emotional processing for social functioning in people with psychotic disorders has been well known for years [48]. Also in the more recent study, Galderisi at al. [45] pinpoint that the connection between emotion recognition and functional capacity highlights the role of social and emotional processing in general psychosocial functioning. According to Thaler et al. [49], people capable to comprehend social and emotional stimuli acquire better interpersonal skills needed for some functional capacity tasks (e.g. communication skills). On this basis, one could also consider the communication skills training, based on the emotional literacy as scheduled in FMR, boosting feedforward functioning;
-
c)
the salutogenic approach and the use of positive psychology. The high levels of positivity, which means to see life and experiences in a positive light, defined in the literature as ‘a quite pervasive mode of viewing and facing reality that affects the ways people evaluate their subjective experiences’ [50], was associated to better functioning [51]. Martinelli et al. [52] observed that people with a diagnosis of schizophrenia and higher “positivity” levels measured by an appropriate scale showed improved interaction skills, work abilities, and engagement in pleasant activities.
The improvement in functioning surely explains the high turnover as previously mentioned.
Functioning is a priority target in recovery-oriented interventions [53]. In fact, we observed good results in functioning as well as in Recovery assessment with a statistically significant improvement in RAS total score and in RAS subscale “Goal and success orientation”. These results should be considered very good if you look at the conclusion of a recent study about functioning in schizophrenia spectrum disorder (SSD): “Rehabilitative programmes implemented in RFs for people with SSD should be improved: many people who live there spend a significant amount of time doing nothing” [54]. The predictive variables for RAS at t1 were the RAS level at t0, the emotional intelligence index at t1 and the subjective experience of users in the PRF at t1. This confirms what has been reported in the specific literature of Recovery. In fact, seeing oneself as a person in recovery is a central part of the recovery process itself, associated with both better wellbeing and better recovery-outcome as conceptualized within the recovery model [55]. Simply, the journey of recovery is an on-going self-directed process which allows a person to have a better life despite the limitations posed by his/her condition. In that way the best possible condition of Recovery became itself a good predictor of recovery-outcome as if it were an ingredient of hope [56]. At the same time, it is interesting that emotional intelligence was a predictor of Recovery. Emotional intelligence means the Theory of mind, a field of knowledge partially explored in schizophrenia spectrum for what concerns functioning and recovery; nevertheless, very promising [57]. Our results could give a little contribution. The variable concerning the subjective experience about the structure, in term of good inter-relationship with others, confirms that a good environment facilitates the process of recovery. In fact, users’ experience of quality of interpersonal relationships is prospectively associated with recovery as well as good interpersonal relationships and interactions are central drivers of recovery in people with psychotic disorders [58]. In addition, we strongly believe that the BCS plays a relevant role in functioning, due to combining traditional aspects of behavioral rehabilitation, for instance on self-care or sleep-hygiene, with defining detailed goals of behavioral changes in lifestyle, such as diet, active mobility, mastery with relaxion-training or mindfulness or yoga or tai-chi. Working in groups encourages people and creates supportive pair-to-pair interactions to fill the schedule and to set realistic data to evaluate progress [59].
Another important improvement regards the level of stress. Managing stress is of crucial importance because it is a key variable of illness onset, relapse and recurrences as known for years [60, 61] and it has been recently well studied for peculiar aspects [62] as well as for identification of specific and effective interventions [63]. Since stress remains at high levels after the Covid-19 pandemic and lockdown [64], effective stress interventions, as considered in the FMR, are now and in the future of vital importance. Actually, at a population level, it is really pertinent to consider stress as a modern epidemic of human life [65]. We believe that also the mindfulness techniques as suggested by the recent scientific literature [66], used in our approach within the meetings of “calm your mind” and related homework, with also related booster sessions gave a great contribution to improve stress-management.
The good results in the cognitive flexibility are encouraging, since our intervention gave much importance to these cognitive deficits, prompting cognitive flexibility above all by the meetings of problem solving training and related homework. The cognitive flexibility, as known, is important “to appropriately adjust one’s behavior according to a changing environment” [67, 68] and is associated with resilience to negative life events and stress in adulthood [69]. However, despite its importance, a comparison of this variable is not possible because there are few data about the psychiatric rehabilitation in PRFs; nevertheless, Dajani et al. [67] stated that more studies about cognitive flexibility are required. The meetings on problem solving also had impact on the other executive functions. We observed an improvement trend in all cognitive variables even if only for immediate memory there was statistical significance. In our opinion, problem solving training works as an indirect and a global strategy of cognitive remedation. This fact could find some explanation in the recent pilot fMRI study of Alescio et al. [70]. They observed that “innovative thinking was influenced by reasoning, whereas it was influenced by cognitive flexibility following problem-solving training”. These findings highlight that an intervention based on problem solving “promotes innovative thinking by changing the way subjects recruit and use relevant cognitive processes. Modifications in the resting-state connectivity of attention, default mode and visual networks were observed in the problem-solving group”. After all this intervention, it is not sufficient to significantly improve cognitive function and specific programs are needed for this purpose, considering the role that cognitive functions play in improving social functioning [71] and Recovery Process [72], as we also wrote previously debating the role of problem-solving training.
The observed improvement of atmosphere inside the facility during the short follow-up period is also important, even if it does not reach statistically significant differences. As known, in psychiatry the Ward/Residential atmosphere or climate has been found associated with better outcomes and a better therapeutic alliance between the individuals with mental disorders and staff in several studies [24, 73]. Probably, also in this study the amelioration of atmosphere gave a contribution on the therapeutic alliance, since we had only 3 dropouts, in the first month, and 1 CTO.
We are not surprised by the improvement in the knowledge of abilities such as definition of goals, communication skills and problem-solving, because users had probably not carried out similar intervention before. However, the improvement of knowledge showed that the training worked very well.
Last, but not least: the improvement of Utility perception and Pleasantness of the sessions by participants, which represents a subjective feed-back for the intervention, mirroring the objective hard data of functioning improvement.
Conclusions
The purpose of this study was to assess improvements in functioning after an innovative, recovery-oriented program conceived for Psychiatric Residential Facilities; in fact, in these structures effective treatments seem to be rare and desirable. The strengths of this intervention is that is structured, manualized, and one of the first based on a psychoeducational and salutogenic approach for PRFs. In addition it can be integrated with similar approach, for instance the VADO approach in Italy and above all programs for cognitive remedation since its contain the approach based on problem solving that facilitate the improvement of cognitive functions. It may also be considered efficient, because of the limited number of sessions and the improvement consolidating over time, on the basis of good results we observed in this study. The limit of this program could concern the organizational problem of the structure (i.e., two meeting per week, a good coordination among the professionals that train the admitted and the staff of the PRF above all to sustain participant in pursuing their goals) and the lack of the involvement of relatives.
The strength of the study is the large number of variables explored, the methodology and that is a multicenter study in different geographics context. The limit is that is a not a randomized Study with the problem of the generalizability of the result. As a consequence, further studies, with randomized controlled design and with a longer follow up are needed to prove the efficacy of Functional Management and Recovery. We can then anticipate that a one-year multicenter controlled randomized study of a similar intervention has just finished with good results as observed by professionals; this intervention has been modified for the addition of the active group-resources to support functioning in real-life also in order to correct the lack of involvement of relatives.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available because individuals with mental disorders did not provide consent for their data to be shared with third parties. However, data may be available from the corresponding author upon reasonable request and with added patient consent for such data to be shared.
Abbreviations
- AKS:
-
Abilities Knowledge Schedule
- BCS:
-
Behavioural Changement Schedule
- BPRS:
-
Brief Psychiatric Rating Scale
- CTO:
-
Compulsory Treatment Order
- EI-I:
-
Emotional Intelligence Index
- FMR:
-
Functional Management and Recovery
- IMR:
-
Illness Management and Recovery
- M-FPT:
-
Modified Five-Point Test
- POPReF:
-
Patient Opinion about the PRF
- PRAS:
-
Psychiatric Residential Atmosphere Schedule
- PRFs:
-
Psychiatric Residential Facilities
- PSPS:
-
Personal and Social Performance Scale
- RAS:
-
Recovery Assessment Scale
- RBANS:
-
Repeatable Battery for the Assessment of Neuropsychological Status
References
Ministero Italiano della Salute. Rapporto salute mentale, Analisi dei dati del Sistema Informativo per la Salute Mentale (SISM), Anno 2022. Italy: Ministero Italiano della salute; 2023. https://www.salute.gov.it/imgs/C_17_pubblicazioni_3369_allegato.pdf.
Barbui C, Papola D, Saraceno B. Forty years without mental hospitals in Italy. Int J Mental Health Syst. 2018;12:43. https://doi.org/10.1186/s13033-018-0223-1.
de Girolamo G, Picardi A, Micciolo R, Falloon I, Fioritti A, Morosini, P for the Italian PROGRES Study Group. Residential care in Italy: a national survey of non-hospital facilities. Br J Psychiatry. 2002;181:220–5.
de Girolamo G, Picardi A, Santone G, Falloon I, Morosini P, Fioritti A, Micciolo, R for the PROGRES Group. The severely mentally ill in residential facilities: a national survey in Italy. Psychol Med. 2005;34:1–11.
Picardi A, Lega I, Candini V, Dagani J, Iozzino L, de Girolamo G. Monitoring and evaluating the Italian mental health system: the ‘Progetto Residenze’ study and beyond. J Nerv Mental Disease. 2014;202:451–9.
Martinelli A, Iozzino L, Ruggeri M, Marston L, Killaspy H. Mental health supported accommodation services in England and in Italy: a comparison. Soc Psychiatry Psychiatr Epidemiol. 2019;54(11):1419–27. https://doi.org/10.1007/s00127-019-01723-9. Epub 2019 May 4 PMID: 31055632.
Martinelli A, Killaspy H, Zarbo C, Agosta S, Casiraghi L, Zamparini M, Starace F, Rocchetti M, de Girolamo G, Ruggeri M, DIAPASON consortium. Quality of residential facilities in Italy: satisfaction and quality of life of residents with schizophrenia spectrum disorders. BMC Psychiatry. 2022;22(1):717. https://doi.org/10.1186/s12888-022-04344-w. PMID: 36397009; PMCID: PMC9672559.
Martinelli A, D’Addazio M, Zamparini M, Thornicroft G, Torino G, Zarbo C, Rocchetti M, Starace F, Casiraghi L, Ruggeri M, de Girolamo G. DiAPASon collaborators. Needs for care of residents with schizophrenia spectrum disorders and association with daily activities and mood monitored with experience sampling method: the DIAPASON study. Epidemiol Psychiatr Sci. 2023;32:e18. PMID: 37039434; PMCID: PMC10130736.
Repubblica Italiana. (2020). Legge n. 77 del 17 luglio 2020: Conversione in legge, con modificazioni, del decreto-legge 19 maggio 2020, n. 34, recante misure urgenti in materia di salute, sostegno al lavoro e all’economia, nonché di politiche sociali connesse all’emergenza epidemiologica da COVID-19. Gazzetta Ufficiale n. 180 del 18 luglio 2020. https://www.gazzettaufficiale.it/eli/gu/2020/07/18/180/so/25/sg/pdf
Scattoni ML. Residenzialità Psichiatrica: analisi e prospettive. Rapporti Istisan, Roma, 2023; 239. https://www.iss.it/-/rapporto-istisan-23/9-residenzialità-psichiatrica-analisi-e-prospettive
Ministero Italiano della Salute. Rapporto salute mentale, Analisi dei dati del Sistema Informativo per la Salute Mentale (SISM), Anno 2021. https://www.salute.gov.it/imgs/C_17_pubblicazioni_3369_allegato.pdf
Killaspy H, King M, Holloway F et al. The Rehabilitation Effectiveness for Activities for Life (REAL) study: a national programme of research into NHS inpatient mental health rehabilitation services across England. Southampton (UK): NIHR Journals Library; 2017. (Programme Grants for Applied Research, No. 5.7.) https://www.ncbi.nlm.nih.gov/books/NBK425139/https://doi.org/10.3310/pgfar05070
Viganò C, Ariu C, Barbieri D, Goffredi A, Ferrara L, Rea F, Barlati S, Vita A, SIRP Survey Group. Psychiatric rehabilitation patterns in Italy: results from the Italian society of Psychosocial Rehabilitation (SIRP) survey. Front Psychiatry. 2023;14:1130811. https://doi.org/10.3389/fpsyt.2023.1130811. PMID: 36911120; PMCID: PMC9992193.
Jaiswal A, Carmichael K, Gupta S, Siemens T, Crowley P, Carlsson A, Unsworth G, Landry T, Brown N. Essential elements that contribute to the recovery of persons with severe Mental illness: a systematic scoping study. Front Psychiatry. 2020;11:586230. https://doi.org/10.3389/fpsyt.2020.586230. PMID: 33329129; PMCID: PMC7710894.
National Institute for Health and Care Excellence. Rehabilitation for adults with complex psychosis: summary of NICE guidance. BMJ. 2020;372:7–10. https://www.nice.org.uk/guidance/ng181.
McGuire AB, Kukla M, Green A, Gilbride D, Mueser KT, Salyers MP. Illness management and recovery: a review of the literature. Psychiatr Serv. 2014;65(2):171–9. https://doi.org/10.1176/appi.ps.201200274. PMID: 24178191; PMCID: PMC4203303.
Veltro F, Vendittelli N, Pontarelli I, Pica A, Nicchiniello I. L’intervento Psicoeducativo Di Gruppo per Il Raggiungimento Di Obiettivi (Inte.G.R.O). Roma: Alpes; 2016.
Veltro F, Nicchiniello I, Pica A, et al. Description and impact of a structured psychoeducational and salutogenetic approach (Inte.G.R.O.) To support the recovery of people with severe mental disorders. Riv Psichiatr. 2018;53:205–13.
Veltro F, Latte G, Pica A, et al. Effectiveness of a new structured psychoeducational, salutogenetic based approach, in facilitating the recovery of people with severe mental disorders. Int J Ment Health Psychiatry. 2019;5:1–10.
Veltro F, Latte G, Pontarelli I, et al. Long term outcome study of a salutogenic psychoeducational recovery oriented intervention (Inte.G.R.O.) In severe mental illness patients. BMC Psychiatry. 2022;22:240.
Veltro F, Latte G, Pontarelli I, Pontarelli C, Nicchiniello I, Zappone L. Positive impact of InteGRO, a new salutogenic psychoeducational intervention, in managing covid-19 pandemic and lockdown aftermath. Riv Psichiatr. 2022;57(5):238–45. https://doi.org/10.1708/3893.38746. PMID: 36200466.
Antonovsky A. Health, stress and coping. San Francisco: Jossey-Bass; 1979.
Lindstrom B, Eriksson M. Salutogenesis. J Epidemiol Community Health. 2005;59:440–2. https://doi.org/10.1136/jech.2005.034777.
Gigantesco A, Pontarelli C, Veltro F, CBGI Italian Study Group. Psycho-educational group therapy in acute psychiatric units: creating a psychosocial culture. An update of spread and effectiveness of a psychosocial intervention in Italian psychiatric wards. Ann Ist Super Sanita. 2018;54(4):272–83. https://doi.org/10.4415/ANN_18_04_03. PMID: 30575563.
Diagnostic and Statistical Manual of Mental disorders, Fifth Edition, text revision. Washington DC Edition: American Psychiatric Association; 2022.
Ellis A. Rational psychotherapy and individual psychology. J Individual Psychol. 1957;13:38–44.
Moritz S, Menon M, Balzan R, Woodward TS. Metacognitive training for psychosis (MCT): past, present, and future. Eur Arch Psychiatry Clin Neurosci. 2023;273(4):811–7. https://doi.org/10.1007/s00406-022-01394-9. Epub 2022 Mar 25. PMID: 35338378; PMCID: PMC8956140.
Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV social and occupational functioning assessment scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 1995;101:323–9.
Corrigan PW, Salzer M, Ralph RO, Sangster Y, Keck L. Examining the factor structure of the recovery assessment scale. Schizophr Bull. 2004;30(4):1035–41. https://doi.org/10.1093/oxfordjournals.schbul.a007118. PMID: 15957202.
Morosini PL, Casacchia M. Traduzione italiana della brief Psychiatric Rating Scale, versione 4.0 ampliata (BPRS 4.0). Rivista Di Riabilitazione Psichiatrica E Psicosociale. 1995;3:199–228.
Roncone R, Ventura J, Impallomeni M, Falloon IRH, Morosini PL, Chiaravalle E, et al. Reliability of an Italian standardized and expanded brief psychiatric rating scale (BPRS 4.0) in raters with high vs. low clinical experience. Acta Psychiatr Scand. 1999;100:229–36. https://doi.org/10.1111/j.1600-0447.1999.tb10850.x.
Ventura J. Brief psychiatric rating scale-BPRS 4.0. In: Conti L, editor. Repertorio delle scale di valutazione in psichiatria, Tomo 1: 117 – 29. Firenze: Società Editrice Europea; 1999.
Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. 1979;9:139–45.
Randolph C, Tierney MC, Mohr E, Chase TN. The repeatable battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310–9. https://doi.org/10.1076/jcen.20.3.310.823.
Cattelani R, Dal Sasso F, Corsini D, Posteraro L. The modified five-point test: normative data for a sample of Italian healthy adults aged 16–60. Neurol Sci. 2011;32:595–601.
Veltro F, Ialenti V, Morales García MA, Gigantesco A. Indice di Intelligenza Emotiva: uno strumento per la valutazione di routine dei programmi di promozione della salute mentale nelle scuole [Emotional Intelligence Index: a tool for the routine assessment of mental health promotion programs in schools]. Riv Psichiatr. 2016;51(5):197–205. Italian. https://doi.org/10.1708/2476.25890. PMID: 27869906.
Veltro F, Chiarullo R, Leanza V, Di Padua P, Oricchio I, Addona F, Vendittelli N, di Giannantonio M. Descrizione dell’esperienza, dell’efficacia pratica e della diffusione dell’intervento cognitivo-comportamentale di gruppo nel Servizio Psichiatrico di Diagnosi e Cura di Psichiatria [A review of the experience, the effectiveness and the spread of behavioral-cognitive group intervention in psychiatric ward]. Riv Psichiatr. 2013;48(2):130-9. Italian. https://doi.org/10.1708/1272.14037. PMID: 23748723.
Veltro F, Morosini P, Gigantesco A, Casacchia M, Roncone R, Dell’acqua G, Chiaia E, Balbi A, De Stefani R, Cesari G. A new self-report questionnaire called ABC to evaluate in a clinical practice the aid perceived from services by relatives, needs and family burden of severe mental illness. Clin Pract Epidemiol Ment Health. 2007;3:15. https://doi.org/10.1186/1745-0179-3-15. PMID: 17877813; PMCID: PMC2031885.
Parker S, Arnautovska U, Siskind D, Dark F, McKeon G, Korman N, Harris M. Community-care unit model of residential mental health rehabilitation services in Queensland, Australia: predicting outcomes of consumers 1-year post discharge. Epidemiol Psychiatr Sci. 2020;29:e109. PMID: 32157987; PMCID: PMC7214525.
Galderisi S, Rossi A, Rocca P, Bertolino A, Mucci A, Bucci P, Rucci P, Gibertoni D, Aguglia E, Amore M, Bellomo A, Biondi M, Brugnoli R, Dell’Osso L, De Ronchi D, Di Emidio G, Di Giannantonio M, Fagiolini A, Marchesi C, Monteleone P, Oldani L, Pinna F, Roncone R, Sacchetti E, Santonastaso P, Siracusano A, Vita A, Zeppegno P, Maj M. Italian Network for Research on psychoses. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13(3):275–87. https://doi.org/10.1002/wps.20167. PMID: 25273301; PMCID: PMC4219069.
Vita A, Barlati S, Ceraso A, Nibbio G, Ariu C, Deste G, Wykes T, Effectiveness. Core elements, and moderators of response of cognitive remediation for Schizophrenia: a systematic review and Meta-analysis of Randomized clinical trials. JAMA Psychiatry. 2021;78(8):848–58. https://doi.org/10.1001/jamapsychiatry.2021.0620. PMID: 33877289; PMCID: PMC8058696.
Magliano L, Puviani M, Rega S, Marchesini N, Rossetti M, Starace F, Working Group. Feasibility and effectiveness of a combined individual and psychoeducational group intervention in psychiatric residential facilities: a controlled, non-randomized study. Psychiatry Res. 2016;235:19–28. Epub 2015 Dec 11. PMID: 26723137.
Vittorielli M, Pioli R, Brambilla L, Archiati L, Rossi G, Sleijpen C, Magliano L, Veltro F, Morosini P. Efficacia in riabilitazione psichiatrica dell’approccio VADO: uno studio controllato [Efficacy of the VADO approach in psychiatric rehabilitation: a controlled study]. Epidemiol Psichiatr Soc. 2003;12(1):43–52. Italian. https://doi.org/10.1017/s1121189x00006047. PMID: 12723391.
Falloon IR, Montero I, Sungur M, Mastroeni A, Malm U, Economou M, Grawe R, Harangozo J, Mizuno M, Murakami M, Hager B, Held T, Veltro F, Gedye R, OTP Collaborative Group. Implementation of evidence-based treatment for schizophrenic disorders: two-year outcome of an international field trial of optimal treatment. World Psychiatry. 2004;3(2):104–9. PMID: 16633471; PMCID: PMC1414683.
Galderisi S, Rucci P, Kirkpatrick B, Mucci A, Gibertoni D, Rocca P, Rossi A, Bertolino A, Strauss GP, Aguglia E, Bellomo A, Murri MB, Bucci P, Carpiniello B, Comparelli A, Cuomo A, De Berardis D, Dell’Osso L, Di Fabio F, Gelao B, Marchesi C, Monteleone P, Montemagni C, Orsenigo G, Pacitti F, Roncone R, Santonastaso P, Siracusano A, Vignapiano A, Vita A, Zeppegno P, Maj M, Italian Network for Research on Psychoses. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia: a network analysis. JAMA Psychiatry. 2018;75(4):396–404. https://doi.org/10.1001/jamapsychiatry.2017.4607. PMID: 29450447.
Gigantesco A, Vittorielli M, Pioli R, Falloon IR, Rossi G, Morosini P. The VADO approach in psychiatric rehabilitation: a randomized controlled trial. Psychiatr Serv. 2006;57(12):1778–83. https://doi.org/10.1176/ps.2006.57.12.1778. PMID: 17158494.
Rapado-Castro M, Moreno C, Ruíz-Sancho A, Camino F, Arango C, Mayoral M. Role of executive function in response to a problem solving based psychoeducational intervention in adolescents with psychosis: the PIENSA trial revisited. J Clin Med. 2019;82018. https://doi.org/10.3390/jcm81.
Hooker C, Park S. Emotion processing and its relationship to social functioning in schizophrenia patients. Psychiatry Res. 2002;112(1):41–50. https://doi.org/10.1016/s0165-1781(02)00177-4. PMID: 12379449.
Thaler NS, Sutton GP, Allen DN. Social cognition and functional capacity in bipolar disorder and schizophrenia. Psychiatry Res. 2014;220(1–2):309–14. PMCID: PMC5875306.
Caprara GV, Alessandri G, Eisenberg N, Kupfer A, Steca P, Caprara MG, Yamaguchi S, Fukuzawa A, Abela J. The positivity scale. Psychol Assess. 2012;24(3):701–12. https://doi.org/10.1037/a0026681. Epub 2012 Jan 16. PMID: 22250591.
Najas-Garcia A, Carmona VR, Gómez-Benito J. Trends in the study of motivation in Schizophrenia: a bibliometric analysis of six decades of Research (1956–2017). Front Psychol. 2018;9:63. https://doi.org/10.3389/fpsyg.2018.00063. PMID: 29515471; PMCID: PMC5826241.
Martinelli A, Moncalieri G, Zamparini M, Alessandri G, Vittorio Caprara G, Castelnuovo G, Rocchetti M, Starace F, Zarbo C, de Girolamo G. Positivity, daily time use, mood, and functioning in patients with schizophrenia spectrum disorders: results from the diapason multicentric study. Int J Soc Psychiatry. 2024;70(2):319–29. Epub 2023 Dec 6. PMID: 38054430; PMCID: PMC10913309.
Morin L, Franck N. Rehabilitation interventions to promote recovery from schizophrenia: a systematic review. Front Psychiatry. 2017;8:100. https://doi.org/10.3389/fpsyt.2017.00100.
Zarbo C, Rota M, Calza S, Crouter SE, Ekelund U, Barlati S, Bussi R, Clerici M, Placenti R, Paulillo G, Pogliaghi S, Rocchetti M, Ruggeri M, Starace F, Zanolini S, Zamparini M, de Girolamo G, DiAPAson Collaborators. Ecological monitoring of physical activity, emotions and daily life activities in schizophrenia: the DiAPAson study. BMJ Ment Health. 2023;26(1):e300836. https://doi.org/10.1136/bmjment-2023-300836. PMID: 37666578.
Cruwys T, Stewart B, Buckley L, Gumley J, Scholz B. The recovery model in chronic mental health: a community-based investigation of social identity processes. Psychiatry Res. 2020;291:113241. https://doi.org/10.1016/j.psychres.2020.113241. Epub 2020 Jun 16. PMID: 32590231.
Acharya T, Agius M. The importance of hope against other factors in the recovery of mental illness. Psychiatr Danub. 2017;29(Suppl 3):619–22. PMID: 28953841.
de Sales SC, Philippsen M, de Jesus LS, Carriello MA, Alvim PHP, Costa DFB, da Rosa LC, Hasse-Sousa M, Czepielewski LS, Massuda R. Social cognition and psychosocial functioning in schizophrenia and bipolar disorder: theory of mind as a key to understand schizophrenia dysfunction. Eur Neuropsychopharmacol. 2023;77:12–20. https://doi.org/10.1016/j.euroneuro.2023.08.483. Epub 2023 Sep 1 PMID: 37660439.
Linde J, Schmid MT, Ruud T, Skar-Fröding R, Biringer E. Social factors and recovery: a longitudinal study of patients with Psychosis in Mental Health Services. Community Ment Health J. 2023;59(2):294–305. https://doi.org/10.1007/s10597-022-01007-8. Epub 2022 Aug 17. Erratum in: Community Ment Health J. 2022;: PMID: 35976477; PMCID: PMC9859912.
Yalom ID, Leszcz M. The theory and practice of group psychotherapy. 5 ed. New York: Basic Books; 2005.
Papadimitriou G. The Biopsychosocial Model: 40 years of application in Psychiatry. Psychiatriki. 2017;28(2):107–110. Greek, Modern, English. https://doi.org/10.22365/jpsych.2017.282.107. PMID: 28686557.
Goh C, Agius M. The stress-vulnerability model how does stress impact on mental illness at the level of the brain and what are the consequences?. Psychiatr Danub. 2010;22(2):198–202. PMID: 20562747.
Kogler L, Regenbogen C, Müller VI, Kohn N, Schneider F, Gur RC, Derntl B. Cognitive stress regulation in Schizophrenia patients and healthy individuals: brain and Behavior. J Clin Med. 2023;12(7):2749. https://doi.org/10.3390/jcm12072749. PMID: 37048832; PMCID: PMC10095473.
Steffen PR. Using the Research Domain Criteria as a framework to integrate psychophysiological findings into stress management and psychotherapy interventions. Front Neuroergon. 2023;4:1245946. https://doi.org/10.3389/fnrgo.2023.1245946. PMID: 38234487; PMCID: PMC10790878.
American Psychological Association. (2023). Stress in America. Available online at: https://www.apa.org/news/press/releases/stress (accessed 24 June 2023).
Vodovotz Y, Arciero J, Verschure PFMJ, Katz DL. A multiscale inflammatory map: linking individual stress to societal dysfunction. Front Sci. 2024;1:1239462. https://doi.org/10.3389/fsci.2023.1239462.
Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;371:1–12. https://doi.org/10.1016/j.cpr.2015.01.006.
Dajani DR, Uddin LQ. Demystifying cognitive flexibility: implications for clinical and developmental neuroscience. Trends Neurosci. 2015;38(9):571–8. https://doi.org/10.1016/j.tins.2015.07.003. PMID: 26343956; PMCID: PMC5414037.
Armbruster DJN, et al. Prefrontal cortical mechanisms underlying individual differences in Cognitive Flexibility and Stability. J Cogn Neurosci. 2012;24:2385–99.
Genet JJ, Siemer M. Flexible control in processing affective and non-affective material predicts individual differences in trait resilience. Cogn Emot. 2011;25:380–8.
Alescio-Lautier B, Chambon C, Deshayes C, Anton JL, Escoffier G, Ferrer MH, Paban V. Problem-solving training modifies cognitive functioning and related functional connectivity in healthy adults. Neuropsychol Rehabil. 2023;33(1):103–38. Epub 2021 Oct 17. PMID: 34657550.
Mucci A, Galderisi S, Gibertoni D, et al. Factors Associated with Real-Life functioning in persons with Schizophrenia in a 4-Year follow-up study of the Italian Network for Research on psychoses. JAMA Psychiatry. 2021;78(5):550–9. https://doi.org/10.1001/jamapsychiatry.2020.4614. PMID: 33566071; PMCID: PMC7876615.
Vita A, Barlati S, Deste G, et al. Life engagement in people living with schizophrenia: predictors and correlates of patient life engagement in a large sample of people living in the community. Psychol Med. 2023;53(16):7943–52. Epub 2023 Jul 31. PMID: 37522514; PMCID: PMC10755242.
Papoulias C, Csipke E, Rose D, McKellar S, Wykes T. The psychiatric ward as a therapeutic space: systematic review. Br J Psychiatry. 2014;205(3):171–6. https://doi.org/10.1192/bjp.bp.114.144873. PMID: 25179622.
Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31–4. https://doi.org/10.4103/sja.SJA_543_18. PMID: 30930717; PMCID: PMC6398292.
Acknowledgements
We are grateful to patients that participated, to the professionals of PRFs, to the Interactive Cooperative that provide location for the training.
*FMR Working Group.
Dipartimento Salute Mentale di Salerno
Salerno, Italy
Gaetano Pinto, Pietro Giordano, Clementina Fontanella, Claudia Salernitano, Giulio Corrivetti.
Interactive Cooperativa
Torino, Italy
Matteo Tedde, Stefano Perello, Valentina Fonte, Assunta Bruno, Andrea Antonucci, Elena Bolognini, Monica Salbego, Marco Spadafora, Claudia Sasso, Andrea Bosonin, Maurizio Previtali, Maria Gloria Calì.
Dipartimento di Salute Mentale di Cuneo
Cuneo, Italy
Roberta Pellegrino.
Consorzio Utilità Sociale Molise-Puglia
Gambatesa (CB), Italy
Domenico Mucci, Iryna Skladanova, Giuseppe Di Ielsi, Stefania Rinaldi, Alessia Pozzuto, Antonio Barrea.
Cooperativa Nuove Prospettive
Busso (CB), Italy
Michele Biondi, Fabiana Priano, Battista Lorenzo.
STROBE guidelines
We followed the STROBE guidelines [74].
Informed consent for participation
Prior to their participation in the study, all individuals were fully informed about the study scope, objectives, methodology, and components, and they provided written informed consent. They were also informed that their participation was voluntary and they could withdraw from the study at any time. All participants provided written informed consent to participate in the study.
Funding
We received a contribution only for the publication of paper from “Cooperative Nuove Prospettive”. ID Grant: NP No 01/24.
Author information
Authors and Affiliations
Consortia
Contributions
FV conceived the study and wrote the first draft, GL performed statistical and co-wrote the first draft, CP contributed to the statistical analyses and co-wrote the first draft, MB conceived the study and provided feed-back, LS and GC were in charge of data collection and provided feed-back, IN and IP co-write the first draft, LZ provided feedback and participated for finalizing the manuscript, FMR-Working group provided feedback.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the Declaration of Helsinki. The protocol was submitted to and approved by the relevant ethical and review boards “Comitato Etico Interaziendale A. O. “Santa Croce e Carle di Cuneo AA.SS.LL. Cuneo 1, Cuneo 2, Asti, Via Monte Zovetto, 18–12100 CUNEO, reference “ASL CN1/PSICH. 4” (Report 75/22 of 27/04/2022; prot. n. of General Management Resolution Measure 01121153 of 09/09/2022). Prior to their participation in the study, all individuals were fully informed about the study scope, objectives, methodology, and components, and they provided written informed consent. They were also informed that their participation was voluntary and they could withdraw from the study at any time. The informed consent of the participants was obtained before the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Veltro, F., Latte, G., Pontarelli, C. et al. Functioning Management and Recovery, a psychoeducational intervention for psychiatric residential facilities: a multicenter follow-up study. BMC Psychiatry 24, 601 (2024). https://doi.org/10.1186/s12888-024-06033-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-06033-2